Notes - Medical treatment of Minors
1/58
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
59 Terms
Arguments for leaving minors consent to medical treatment
Ethical arguments for and against respecting autonomy of young person/minor
Should be treated with dignity and have their decisions respected
Ensures compliance
Better recovery
Encourages trust
Issues that arise with minors being able to consent
Immaturity: Different understanding between ages 13 and 17
Incomplete understanding of death: Might have never had to deal with death yet
Increase of conflict with parents
Failure to protect them from burdens of adulthood
UN Convention on the Rights of the Child Article 12
States that children capable of forming their own views have the right to express those views freely in all matters affecting them.
Minors included in this.

Non-Fatal Offences Against the Person Act 1997
S.23(1) The consent of a minor who has attained the age of 16 years to any surgical, medical or dental treatment which, in the absence of consent, would constitute a trespass to his or her person, shall be as effective as it would be if he or she were of full age; and where a minor has by virtue of this section given an effective consent to any treatment it shall not be necessary to obtain any consent for it from his or her parent or guardian.
(2) In this section “surgical, medical or dental treatment” includes any procedure undertaken for the purposes of diagnosis, and this section applies to any procedure (including, in particular, the administration of an anaesthetic) which is ancillary to any treatment as it applies to that treatment.

s 8(1) of the Family Law Reform Act 1969 (ENGLAND)
gives a minor aged over 16 years powers to consent to medical and surgical treatment equivalent to those of an adult. It is silent in respect of minors under the age of 16.
![<p><span style="color: red"><strong><em>Gillick v West Norfolk and Wisbech AHA</em> [1986] AC 112</strong></span></p>](https://knowt-user-attachments.s3.amazonaws.com/bc0fa8a7-09f2-46c3-be57-4114bd961ac8.jpg)
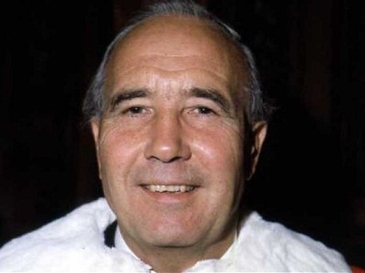
Gillick v West Norfolk and Wisbech AHA [1986] AC 112
UK Dept. of Health issued guidance allowing doctors to prescribe contraception to girls under 16 without parental consent if it protected the girl from harm, despite encouraging parental involvement.
Plaintiff: Mrs. Gillick, a mother, sought assurance that her daughters wouldn’t receive contraceptives without her consent. The Health Authority refused.
Legal Action: Mrs. Gillick claimed this guidance breached her parental rights.
Outcome: House of Lords (3:2 majority) ruled in favor of the Health Authority.
Significance:
Established that parental rights are not absolute and decrease with a child's maturity.
Confirmed that doctors can treat minors under 16 if they possess sufficient understanding of the treatment's nature and consequences.
Comparable Law: S.8 Family Law Reform Act 1969 in the UK, similar to Irish section 23(1).

Lord Scarman's 'Gillick Competency' Test
The benchmark for assessing if a minor under 16 can independently consent to medical treatment.
Key Principle = A minor's right to consent begins when they have "sufficient understanding and intelligence" to fully comprehend the proposed treatment.
‘Gillick competency’ criteria
Understanding of the medical advice and its implications.
Sufficient maturity to grasp all aspects involved, including emotional and long-term consequences.
Gillick context of contraceptive advice for young girls
Lord Scarman noted the necessity of considering moral and family dynamics, emotional impacts, and health risks.
Interpretation = This standard is so rigorous that it could challenge the understanding level of many adults
Lord Frasers view on minor consent
argued that there is no legal distinction between consent for medical treatment and contraceptive advice for minors.
Rejecting Ms. Gillick’s argument, he implied that prohibiting under-16s from consenting to any medical treatment would be "surprising" and "absurd."
“Provided the patient... is capable of understanding what is proposed... I see no good reason for holding that he or she lacks the capacity to express them validly and effectively.”
The Fraser Guidelines
Established criteria for doctors to give contraceptive advice to minors without involving parents.
Doctor must be satisfied:
The girl understands the advice.
Parental consent or knowledge cannot be persuaded.
She is likely to engage in sexual intercourse with or without contraceptives.
Her physical or mental health could suffer without treatment.
Providing advice or treatment is in her best interests.
Gillick Dissenting opinions:
Brandon and Templeman LJJ dissented.
Templeman LJ believed parents should make decisions for minors lacking competence and opposed granting doctors the discretion to provide contraception without parental knowledge. Argued it could undermine parental authority and potentially harm the minor by encouraging sexual activity. Parents finding this out would harm family doctor relationships. Doctors should not prescribe contraceptives based solely on clinical judgment or best interest because they lack family dynamic understanding.
![<p><span style="color: red"><strong><em>Axon v Secretary of State for Health</em></strong></span><span style="color: red"><strong> [2006] EWHC 37</strong></span></p>](https://knowt-user-attachments.s3.amazonaws.com/836499d8-457e-4a1a-a6e6-3b9b7bb287fa.png)
Axon v Secretary of State for Health [2006] EWHC 37
Mother claimed Department of Health guidance allowing minors under 16 confidentiality on reproductive advice was unlawful, breaching her Art. 8 rights.
Court Held:
Guidance on Abortion: Acknowledged as more serious due to its irreversible nature, potential risks, and moral implications.
—> however…
Gillick Precedent: Court upheld that no exception to confidentiality for minors was permissible, maintaining the duty of confidence.
Minor confidentiality promotes access to care and autonomy, outweighing parents rights
Art. 8 Analysis:
Silber J affirmed that a young person’s autonomy takes precedence over parental rights when they possess sufficient understanding and intelligence.
Parental rights to notification depend on the minor’s age, maturity, and willingness to share.

NHS Trust v ABC (2014)
Involved the question of whether a 13-year-old had capacity to decide whether to continue or terminate her pregnancy.
Court took an unambiguous stance to a finding of Gillick competence as the end of the matter, permitting the girl to make a determinative choice.

Bell & A v Tavistock & Portman NHS Foundation Trust
Judicial review of NHS protocols for prescribing puberty-blockers (PBs) to minors under 18 with gender dysphoria.
First claimant was Ms. Bell who detransitioned but got PBs at 16, and a mother who was concerned her child would be referred to GIDS.
Claimants' Argument: Minors under 18 lack the competence to give informed consent due to complex, insufficiently explained long-term impacts of PBs.

High Court Findings: Bell & A v Tavistock & Portman NHS Foundation Trust
Understanding the long-term implications of PBs requires significant maturity.
Eight Essential Factors: Young people must: grasp immediate effects, long-term progression to cross-sex hormones, surgery implications, fertility loss, sexual function, relationship impacts, unknown consequences, and uncertain evidence.
Age Rulings:
Under 13: Highly unlikely to have capacity.
14-15: Doubtful capacity.
16-17: Statutory presumption of capacity to consent to medical treatment
Held: Given the innovative and experimental nature of PBs and their significant long-term impacts, clinicians may need to seek court authorisation before starting treatment in cases involving minors.

Criticisms & Implications: Bell & A v Tavistock & Portman NHS Foundation Trust
The requirement for deep understanding suggests potential court involvement before treatment is administered.
Criticism:
Moreton's View: High thresholds for understanding complex, long term treatment implications move beyond the original Gillick standard, which focused on basic comprehension.
Autonomy Concerns: has been criticised as overly cautious and not in line with modern healthcare principles, which emphasise patient rights and involvement.
Concerns raised:
The expectation for a 13-year-old to understand fertility and long-term life impacts is seen as unreasonable, particularly when certain related treatments aren't accessible until they are older.
Departure from the autonomy-focused principles of Gillick.

AB & CD v Tavistock & Portman NHS Foundation Trust & Ors.
AB (parent of a 15-year-old trans daughter) sought a declaration regarding her legal ability to consent to the administration of puberty blockers (PBs) on behalf of her daughter, who was affected by the previous ruling in Bell.
Legal Issues and Findings by the Court: AB & CD v Tavistock & Portman NHS Foundation Trust & Ors
Issue: Parental Consent: Whether parents retain a concurrent right to consent alongside a Gillick competent child?
Held: Parents retain a right to consent when a competent child declines or does not object, or is unconscious.
Issue: Special Category of Treatment: Whether PBs require a unique application to the court due to their nature.
Court Approval for PB? = While some cases require court approval (e.g., clinical disagreements, alternative treatments), there is no blanket requirement for PBs as a special category.

Critiques: AB & CD v Tavistock & Portman NHS Foundation Trust & Ors
Moreton believes this ruling mainly benefits children with supportive parents and fails to uphold the rights of competent children to consent to necessary medical treatments, potentially limiting the scope of Gillick.
![<p><span style="color: red"><strong><em>Bell</em></strong></span>: <span style="color: red">Court of Appeal Ruling [2021] EWCA Civ 1363.</span></p>](https://knowt-user-attachments.s3.amazonaws.com/65e942c8-10d2-420e-adb3-2f48eb9e36b6.jpg)
Bell: Court of Appeal Ruling [2021] EWCA Civ 1363.
The Court reversed the High Court’s declarations in Bell, stating they were not appropriate for judicial review and emphasising that the High Court could not generalise about the competence of minors to consent to puberty blockers.
High Court Critique:
The Court of Appeal found that the High Court improperly restricted the Gillick test by imposing age criteria and requiring court applications for consent to PBs, which was not appropriate for general guidance.
The Court stressed that clinicians must use their judgment in assessing a young person's ability to consent, recognising the complexities involved in cases of transgender minors.
Informed Consent Factors for Puberty Blockers
Includes understanding immediate consequences, paths to future treatments, and implications of irreversible decisions.
![<p><span style="color: red"><strong><em>Re E (a minor) (wardship: medical treatment) </em>[1993]</strong></span></p>](https://knowt-user-attachments.s3.amazonaws.com/33dfa44b-ee88-4102-ac59-2f4c5965a5ef.png)
Re E (a minor) (wardship: medical treatment) [1993]
15 years and 10 month old Jehovah Witness boy suffering from leukaemia
Refused life saving blood transfusion with 80-90% remission
Parents supported his decision and gave consent for alternative drug treatment with lower success rate.
Hospital sought wardship to override the refusal
Court held:
E was intelligent but did not comprehend the distress and pain of dying
Not Gillick competent
Ruled in favour of transfusion under welfare concerns
Even if he was Gillick competent decision would have been overridden on welfare basis.
Ward J ‘ court must protect him from him and his parents’
Mature Minor
A young person who has the capacity to make decisions regarding their own medical treatment.
Judicial Review
The process by which a court reviews the legality of a decision or action taken by a public authority.
![<p><span style="color: red"><strong><em>Re S (a minor) (medical treatment) </em>[1994]</strong></span></p>](https://knowt-user-attachments.s3.amazonaws.com/f69bccfe-e72e-4b0e-bd42-c67b4101ed95.webp)
Re S (a minor) (medical treatment) [1994]
15 and a half years old girl stopped attending her blood transfusions and became disillusioned with the treatment
Mother had converted to Jehovah Witness at 10
Local authority sought court intervention for her to receive treatment
High Court:
S’s decision was recent, driven by disillusioned with and heavily influenced by mothers beliefs
She lacked full understanding of the consequences of refusing treatment as she thought God would save her. and was found not to be Gilick competent
Johnson J: her decision did not carry weight without greater understanding of her death’s manner, pain and distress
Court overrode her decision
Re E and Re S: Contrast
E =
Deeper religious conviction
Better grasp of the consequences of his refusal and death
Views shaped by life long religious teachings
S =
hoped for some miracle cure
doubted the doctors diagnosis
newly influenced by mothers conversion
Both minors refuses were overruled with court focusing on their age and welfare over evolving autonomy or individual maturity.
Critique: Re E and Re S
“Ignore the development of the individual and flies in the face of evolving autonomy. Rationality appears to be acquired on 18th birthday”
E died 2 years after transfusion and raised questions aroundnwhetehr the court prolonger his life meaningfully to imposed distressing unwanted treatment
![<p><span style="color: red"><strong><em>Re L (Medical Treatment: Gilick Competency)</em> [1998]</strong></span></p>](https://knowt-user-attachments.s3.amazonaws.com/a3c1619b-2248-426a-90d8-b7ffc328eb5c.jpg)
Re L (Medical Treatment: Gilick Competency) [1998]
14 year old Jehovah Witness with severe burns refused medical treatment
Had previously signed and renewed directive refusing blood transfusion based on her faith
Required life saving treatment to survive and without transfusion would develop gangrene leading to a ‘horrible death’
Described as religious, mature and intelligent with a supportive family that would accept her even if she got the treatment.
Court:
Authorised blood transfusion, overriding L’s refusal
Considered her rigid and unquestioning faith as immaturity and her sheltered upbringing
She could not fully understand her decision as she hadn’t been given full details of her likely death at her family’s request
Not Gilick competent as she did not understand the consequences of her decision
Critiques: Re L [1998]
Her beliefs appeared to lack the same validity as an adults
May be asked why her beliefs were not repsected in the same way as adults even though she was competent and not under any coercion.
She was not deliberately told about her condition and so could not increase her understanding and therefore could not make a valid consent of refusal.

AC v Manitoba (2009)
Canadian case
14 year old Jehovah Witness refused blood transfusion
Under Manitoba law, minors under 16 are not permitted to have full autonomy in medical decisions
Court:
Ordered transfusion in the best interests of minor
Supreme Court:
Upheld this and emphasised laws balance between respecting personal rights and protecting vulnerable children
Introduced a sliding scale of scrutiny
![<p><span style="color: red"><strong><em>Re R (a minor) (wardship, consent to medical treatment) </em>[1991]</strong></span></p>](https://knowt-user-attachments.s3.amazonaws.com/e4a2cf6e-bd07-4d42-bd19-7d2a48597031.png)
Re R (a minor) (wardship, consent to medical treatment) [1991]
15 year old placed in children's home following a violent altercation with her father.
Mental health deteriorated significantly leading to hallucinations, suicidal threats and erratic, aggressive behaviour.
Local authority secured order to place R in psychiatric unit.
Condition was unstable but during lucid period she objected to anti-psychotics understanding their nature and effects.
Unit could not provide care without medicating her against her will so sought wardship.
Court:
Not found to be Gillick Competent as wardship is based solely on best interests of the child
Even if she was her refusal could be overridden by court or those with parental rights.
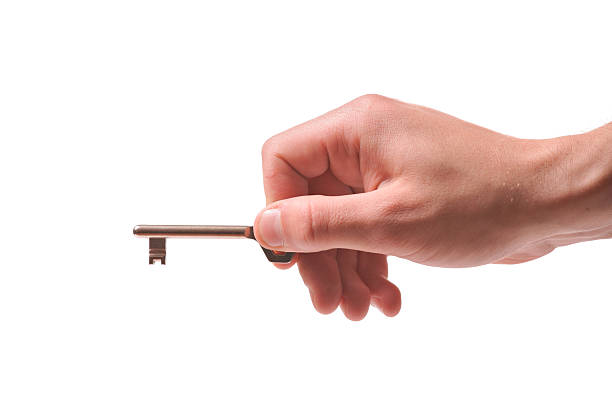
Re R: KEYHOLDER ANAOLOGY
Donaldson J in Re R:
Both minor and those with parental responsibilities hold keys to consent
Each party can authorise treatment but refusal by one does not veto consent given by the other
Parental rights do NOT terminate when child is competent as this would cause ‘intolerable dilemma’ for doctors treating minors who refuse care”
Re R: Farquharson
Highlighted R’s fluctuating capacity due to her illness which rendered her Gilick difficult to apply
Whether court approached question from competence and welfare the result would be the same.
![<p><span style="color: red"><strong><em>South Glamorgan County Council v. W and B</em> [1993]</strong></span></p>](https://knowt-user-attachments.s3.amazonaws.com/17fdba7d-33e2-4645-a5d8-bfbc449fdfa6.undefined)
South Glamorgan County Council v. W and B [1993]
15 year old girl experiences severe psychiatric issues after her parents divorce.
Lived reclusively in fathers home, refusing school and social interaction
Behaviour became abusive and she threatened harm if her demands were not met
Father refused removal of girl so local authority sought court approval under Children’s Act 1989, citing probable harm if intervention was denied.
Court
Granted permission to remove her for assessment and treatment
Rejected argument that A’s statutory right to refuse treatment precluded its jurisdiction, affirming the HC’s inherent jurisdiction over children’s welfare.
A’s wishes were considered but her welfare was paramount
Critiques: South Glamorgan County Council v. W and B
undermined A’s statutory right suggesting where courts exercise jurisdiction minors cannot rely on legal protections
Highlights a tension between respecting minors autonomy and overriding their rights in the name of welfare.
![<p><span style="color: red"><strong><em>Re W (a minor) (Medical Treatment: Courts Jurisdiction) </em>[1992]</strong></span></p>](https://knowt-user-attachments.s3.amazonaws.com/85111925-e834-482a-b62a-5dbf13b8e14b.jpg)
Re W (a minor) (Medical Treatment: Courts Jurisdiction) [1992]
16 year old with anorexia required nosgastric feeding at a specialised unit and refused
Local authority worried that her condition would get worse and she would begin to refuse all treatments so they sought permission to transfer her to another unit and treat her without consent under courts inherent jurisdiction.
Court of Appeal:
Granted application affirming that a competent minor does not hold an absolute veto over medical treatment
Donaldson clarified that Gilick refers to consent but not the power to refuse if another parent/authority consented
ruled anorexia as a condition that could impair the ability to make informed decisions, justifying intervention to save W’s life

Re W: FLAK JACKET ANAOLOGY
Donaldson went back on his key holder analogy in Re. R ‘because keys can lock as well as unlock’ to replace it with the flak jacket analogy that he preferred.
emphasised legal protection for doctors against liability
Critiques: Re W
Criticised for flak jacket analogy seeming to place more emphasis on doctors from litigation than on patient autonomy.
''get a signature on consent form and proceed to do what they think is best’
courts seem sincere with autonomy but is argued they are reluctant to make this a legal principle
Welfare > Self determination
![<p><span style="color: red"><strong><em>Re K, W and H (Minors)</em> [1993]</strong></span></p>](https://knowt-user-attachments.s3.amazonaws.com/c9816521-025e-4c1e-b974-f46dc63949c5.webp)
Re K, W and H (Minors) [1993]
3 adolescents (2 = 15yrs, 1 = nearly 15) girls in a. secure psychiatric unit refused emergency medication after behavioural issues escalated
Hospital sought court approval to override refusals and administer treatment
Court:
Held none of them were Gilick competent but even if they were their refusals could be overwritten as their parents had provided consent to treatment
Thorpe J: affirmed consent from parental authority was enough to authorised treatment and said application was unnecessary as parental consent = legal protection.
Critiques: Re K, W and H (Minors)
Denied minors a way to object paternalistic approach to psychiatric care
Flak jacket reiterated - focusing on shielding doctors from liability over respecting minors autonomy.

Re C (Detention Medical Treatment)
16 year old with anorexia from a dysfunctional family with a history of sexual abuse
Discharged from ED clinic and health rapidly declined
She was erratic and suicidal, her weight dropped dangerously
Clinic sought authorisation to detain her and enforce a referring program but said they treatment would only succeed if she remained in care.
Court
Authorised detention under their inherent jurisdiction, finding it in her best interests
Not Gilick competent as illness impaired her ability to evaluate the risks and benefits of treatment
Detention was needed as essential part of treatment but force feeding was not permitted.
![<p><span style="color: red"><strong><em>Re M (Child: Refusal of Medical Treatment)</em> [1999]</strong></span></p>](https://knowt-user-attachments.s3.amazonaws.com/923edcda-f7cd-45dc-aa48-5a2977ec5808.webp)
Re M (Child: Refusal of Medical Treatment) [1999]
15 years and a half girl with heart failure refused a transplant
Did not want lifelong medication/another persons heart
She did not want to die but was overwhelmed by her decision
Court:
Authorised transplant sedate M’s refuse as the certainty of death outweighed the risks of treatment
M deemed to be incompetent to decide due to her emotional state
Johnson J: consent could have came from her, her mother or the court.
![<p><span style="color: red"><strong><em>University Hospital Plymouth NHS Trust v. B (a minor) [</em>2019]</strong></span></p>](https://knowt-user-attachments.s3.amazonaws.com/61454ae3-d95e-45fa-b25d-a55be037f75f.webp)
University Hospital Plymouth NHS Trust v. B (a minor) [2019]
16 year old with type 1 diabetes
No evidence that she lacked capacity, had a good knowledge of her condition and the risk of death for not taking insulin.
Condition got worse and consented to being admitted to hospital but refused insulin saying she wished to die
Doctors and family feared for her life
Court:
Overrode refusal on her best interests
McDonald J: Presumption in preserving life unless pain and suffering outweighed the benefits
A minor refusal is not binding e.g another with capacity (e.g parent/court) consent to the treatment.
![<p><span style="color: red"><strong><em>An NHS Trust v. X</em> [2021]</strong></span></p>](https://knowt-user-attachments.s3.amazonaws.com/d532125c-0ff8-4ffa-bbe7-37efbdb091cf.webp)
An NHS Trust v. X [2021]
nearly 16 Jehovahs Witness with severe sickle cell syndrome refused blood transfusion, despite urgent medical needs.
Court:
Munby J upheld the principle that minors lack an absolute right to refuse treatment even if Gillick competent.
Declined a rolling 2 year order for blood transfusions but reiterated courts ability to override refusals to prevent serious harm/death
Acknowledged societal/legal changes like HRA but did not displace the authority of Re R or Re W on overriding competent minors refusals.

ECHR Article 8
The article that protects the right to respect for private and family life, often involved in cases concerning parental rights.
Capacity Assessment
The evaluation of a person's ability to understand and decide on their medical care.
Informed Refusal
The patient's right to refuse treatment after being fully informed of the consequences.
HSE National Consent Policy
Guide for healthcare professionals in Ireland
Recognises sufficient consent by 16-17year olds for treatment except under Mental Health Act 2001.
Reinforces LRC 2009 observation that criminal act is in practice applied as if it was civil re trespass to the person.
Differentiates between consent vs. refusal
Refusal = can be overturned by court if deemed contrary to minors best interests

LRC 2011: Children and the Law: Medical Treatment - Recommendations
Consent and refusal should not be treated differently but considerations need to be taken into account where life-sustaining treatment is refused.
Advocate for legislation presuming minors aged 16-17 have capacity to both consent to and refuse treatment
Suggested a non-prescriptive framework for under 16s, using factors like maturity, understanding of consequences and stability of beliefs to assess capacity
Sliding scale similar to Gilick and Manitoba.
Under 16s should involve parent of guardians.
Recommended mandatory HC involvement in cases of life-sustaining treatment refusals.
Does not extend to Mental Health.

General Scheme of the Mental Health (Amendment) Bill 2021
proposes that children aged 16 and over will be able to consent to, refuse, admission and treatment in an approved inpatient facility - lining up with UN Convention on Person with Disabilities
Ombudsman is concerned that this proposed legislation makes no provision for consent by children under 16, having regard to their age and evolving capacity.
![<p><span style="color: red"><strong><em>HSE v JM and RP </em>[2013]</strong></span></p>](https://knowt-user-attachments.s3.amazonaws.com/d23f6c69-f933-4284-aa37-0683d912d05e.undefined)
HSE v JM and RP [2013]
15 years 11 month old with bipolar refused blood tests for the medication she was in
Assessed as mature but impaired by her condition as she was a suicide risk
Court:
Birmingham J held she lacked capacity to refuse treatment due to her impaired judgment.
Even though she was not protected by statute under s.23 to refuse this wasn’t to mean she should not be treated with respect.
No principle laid down that 15year olds lack capacity.
Did not comment on whether Gilick was applicable in Ireland
Even if Gillick was applicable in Ireland, she would not be competent as per Re R and decision could be overridden by court or wardship.
Highlighted distinction between consenting and refusing treatment
Refusing = greater scrutiny then life or welfare is at risk
Reiterated ‘central role of parents’ in determining best interests, particularly for medical decisions

Mental Health Act 2001
Minors (under 18) are defined as individuals under 18 years old.
Involuntary Admission: Can be done if the minor meets criteria, with parental consent required for those under 16.
Parental Involvement: Parents or guardians must be involved in decisions for minors under 16.
Consent to Treatment: The Act does not explicitly address minors' consent; parental consent is typically needed.
Best Interests: If a minor refuses treatment, courts may intervene based on the best interests principle.
XY, a minor suing by her Guardian ad Litem Raymond McEvoy v. HSE
Later hearing of JM case
Minor challenged the constitutionality of her detention under the Mental Health Act 2001 and the forceable administration of her treatment
Court
Birmingham J upheld the constitutionality of s.25 of MHA emphasising that parents authority ordinarily governs medical decisions for children.
Differentiated Gilick being about contraceptive advice and consent and refusing psych treatment that was aimed at suicide prevention not the same.
![<p><span style="color: red"><strong><em>McKay v. Information Commissioner </em>[2006]</strong></span></p>](https://knowt-user-attachments.s3.amazonaws.com/0e7a07cd-f191-401e-845e-94bc8c826867.jpg)
McKay v. Information Commissioner [2006]
Nearly 18 year old opposed fathered access to her hospital records when she was admitted
Claimed he had abused her and when she was in hospital cited emotional harm and lack of any relationship with him
She was supported by her joint guardian
Hospital refused to give records to father and he appealed
Fathers appeal was unsuccessful - no evidence of benefit to the girl if records were released
Court:
Denham J acknowledged family had special rights under Constitution
Exceptional circumstances that medical info not given to parent/guardian
Test = parents presumed to have right to access unless this presumptions is displaced by evidence that it would not be in the childs best interest
Delay in proceedings meant girl was nearly 18 and Denham said he views were very relevant here
Sent back to FOI Commissioner
Regarded her age and maturity so presumption was rebutted.
Art. 42A of the Constitution
emphasises the child’s best interests as paramount, allowing the State to intervene in exceptional circumstances.
![<p><span style="color: red"><strong><em>Temple Street v. D and Anor </em>[2011]</strong></span></p>](https://knowt-user-attachments.s3.amazonaws.com/a3281808-9dbe-4343-8b00-26b84bd421ab.jpg)
Temple Street v. D and Anor [2011]
Baby needed blood transfusion but parents refused as they were JW
Court granted a declaration and found administering blood transfusion was necessary and urgent and all other options were exhausted
Considered the constitutional rights of the parents to raise their baby in the religion they wished but that the State has a duty to protect the child.

North Western Health Board v. HW and CW
Parental refusal to PKU screening test was upheld because the scenario was not life-threatening
Mills & Mulligan in Medical Law in Ireland
suggest that following XY, “while Irish law may be willing to recognise that a minor under the age of 16 could have the capacity to consent, it does not mean that that minor will be the sole decision-making agent in relation to his or her care”
“it seems arguable that the courts would recognise a qualified right to consent in the case of mature under-16s.