Chapter 4: Mechanical Ventilation Part 1
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
57 Terms
What is mechanical ventilation?
use of an external device/machine that either breathes for the patient OR helps the patient breathe on his/her own
a _____ is, “a device that delivers air into the lungs through a tube placed within the windpipe”
Delivers O2, removes CO2
What’s a ventilator?
device for moving air
can be complex computerized; or, a simple bag mask
Ventilation → air exchange
Respiration → gas exchange
Perfusion → oxygen actually reaching the blood
What’s a respirator?
device for filtering air
What are indications for mechanical ventilation?
failure of the respiratory system
failed/weak respiratory muscles → alveolar hypoventilation
absent brainstem respiratory drive → central alveolar hypoventilation
hypoventilation → inadequate ventilation
over time → affects gas exchange at the level of the alveoli
hypoxemia
hypoxia
What is hypoventilation?
theoretical: deviation from the usual state of ventilatory control resulting in decreased minute ventilation relative to metabolic requirements
operational: PaCO2 EXCEEDS normal upper limit (45mmHg)
(Terms - Arterial Blood Gasses [ABGs]) SaO2/SpO2 - Oxygen Saturation:
extent to which the hemoglobin is saturated w/ oxygen
(Terms - Arterial Blood Gasses [ABGs]) What is FIO2?
Fraction of Inspired Oxygen
Room air FIO2 = ~21%
(Terms - Arterial Blood Gasses [ABGs]) What is the difference between PAO2 & PaO2?
PAO2 → the force necessary to move oxygen from the air into the blood
PaO2 amount of O2 in the blood
80-100 mm Hg
(Terms - Arterial Blood Gasses [ABGs]) What is the difference between PACO2 & PaCO2?
PACO2 → the force necessary to move CO2 from the blood & into the air
PaCO2 → amount of CO2 in the blood
35-45 mm Hg (millimeters of mercury)
(ABGs - Acidosis vs Alkalosis) What is normal blood pH?
7.34-7.45
(Homeostasis) Which systems work together to keep the body in homeostasis?
respiratory & renal system
(Homeostasis) What does acute (uncompensated) impaired breathing impact?
→ Renal system (healthy) will compensate
→ Need ventilation/respiration support
(Homeostasis) What does acute (uncompensated) impaired kidney function impact?
Respiratory system (healthy) will compensate
May need ventilation/respiration support
May need dialysis
(Homeostasis) What does chronic (compensated) breathing and/or kidney function impact?
the body does its best to keep in homeostasis w/ either or both ventilation/respiratory support & renal support (dialysis)
If unable →
Hypoxemia
Hypoxia
What is hypoxemia?
decreased oxygen in the blood
What is hypoxia?
decreased oxygen in the tissue
How do you treat hypoxia?
Deliver more oxygen by increasing FIO2 & using nasal cannula (40% is common)
Apply (Extrinsic) PEEP “Positive End-Expiratory Pressure”
Needs mechanical ventilation to get more PEEP
What is hypercapnia?
Too much CO2 in the blood
it’s bc ur hypoventilating from kidney → ur not urinating
What is Positive End-Expiratory Pressure (PEEP)?
the amount of pressure needed to maintain air in the lungs after exhalation (at the “end” of exhalation).
healthy systems have a little bit of natural or “physiologic” PEEP
impaired systems may need to have external PEEP added
PEEP - Extrinsic maintains airway pressure above atmospheric pressure at the end of _____
EXHALATION
What are the advantages of PEEP - Extrinsic?
Mitigates alveolar collapse
Increases gas exchange/oxygenation
May reduce Ventilator Assisted Pneumonia (VAP)
Helps decrease leakage of pharyngeal secretions into the lower airway
Helps mitigate effects of Auto-PEEP
What is the typical small amount of PEEP-Extrinsic?
3-5 cm H2O is pretty routine
“Physiologic PEEP”
What is the typical large amount of PEEP-Extrinsic?
> 5 is needed in acute lung injury, ARDS, or some other hypoxemia conditions
“Supraphysiologic PEEP”
What is Dead Space (DS)?
volume of inspired air that is not used in gas exchange
ventilation w/o perfusion
volume ≈ 1/3 of resting tidal volume
≈ mL of lean mass lbs (ex: 100 lbs = 100 mL DS)
Total or Physiologic DS = Anatomic DS + Alveolar DS
Anatomic (air that never made it to capillaries)
mouth, pharynx, trachea, bronchioles
Alveolar (dead space in between alveoli)
sum of the volume of the individual alveoli that have little or no blood flow through their capillaries
Negligible in healthy people; can increase dramatically in lung diseases
(DS) Is breathing faster & shallower more effective?
NO! Breathing slower & deeper is more effective than breathing faster & shallower, even if total volume remains the same
10 bpm x 500 ml = 5000 ml IS BETTER THAN
20 bpm x 250 ml = 5000 ml exchanged per minute
Why is breathing slower and deeper more effective?
More DS w/ faster shallower breathing
“wasted” respiratory effort, leading to fatigue & possible acidosis
More CO2 retention = Higher PaCO2, & possible respiratory acidosis
Less Oxygen Perfusion
(Mechanical Ventilation Options) What are the Types of Ventilation?
Positive Pressure Ventilation
Negative Pressure Ventilation
High Frequency Ventilation
What are the 2 air delivery methods?
Non-Invasive
Invasive
Non-invasive =
External (air gets blown into mouth externally)
Invasive =
Internal
Endotracheal tubes (air being blown through tube in you)
Tracheostomy tubes
What is Positive Pressure Ventilation?
Machine provides pre-set positive pressure (above atmospheric pressure), pushes a pre-set volume of gas into the airway, inflates the lungs, increases intra-alveolar pressure
Pressure stops, exhalation occurs
Cycles at pre-set interval or Respiratory Rate
Passive inspiration
Passive exhalation
Invasive or Non-Invasive
Invasive is Common in ICU’s
What is the sequence of Positive Pressure Ventilation?
Machine provides positive pressure → Air is pushed into lungs → Lungs & Alveoli Expand
Can positive pressure ventilation be only be invasive?
No, can be invasive or non-invasive!
Invasive: Endotracheal tube, Tracheostomy
Non-Invasive (external): CPAP, BiPAP, VAPS
What is Negative Pressure Ventilation?
Ventilators go “around the body”
Machine creates a vacuum around the chest wall & acts as inspiratory musculature
Chest wall is sucked outward, diaphragm is lowered, & pleural pressure falls (goes below atmospheric pressure), lungs & alveoli expand as air rushes in
Vacuum stopped, exhalation occurs
Cycle repeats at pre-set interval
“Active-ish” inspiration
Passive exhalation
Not so common these days
Non-invasive only
What is the sequence of Negative Pressure Ventilation?
Vacuum sucks out chest; creates negative pressure → Lungs & Alveoli expand → Air rushes in
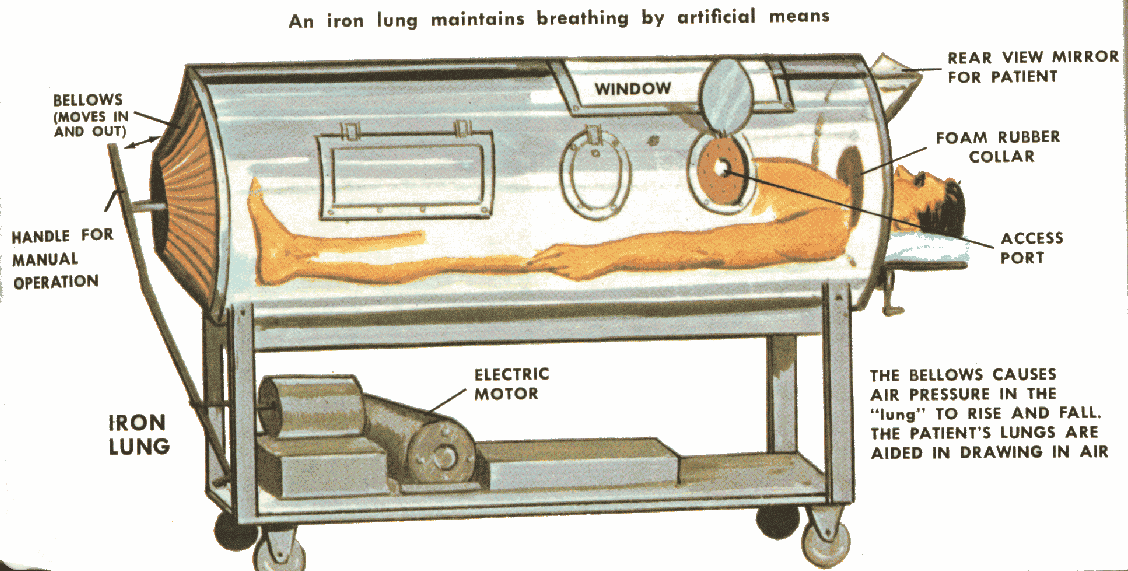
What are the Negative Pressure Types?
Iron Lung
Cuirass
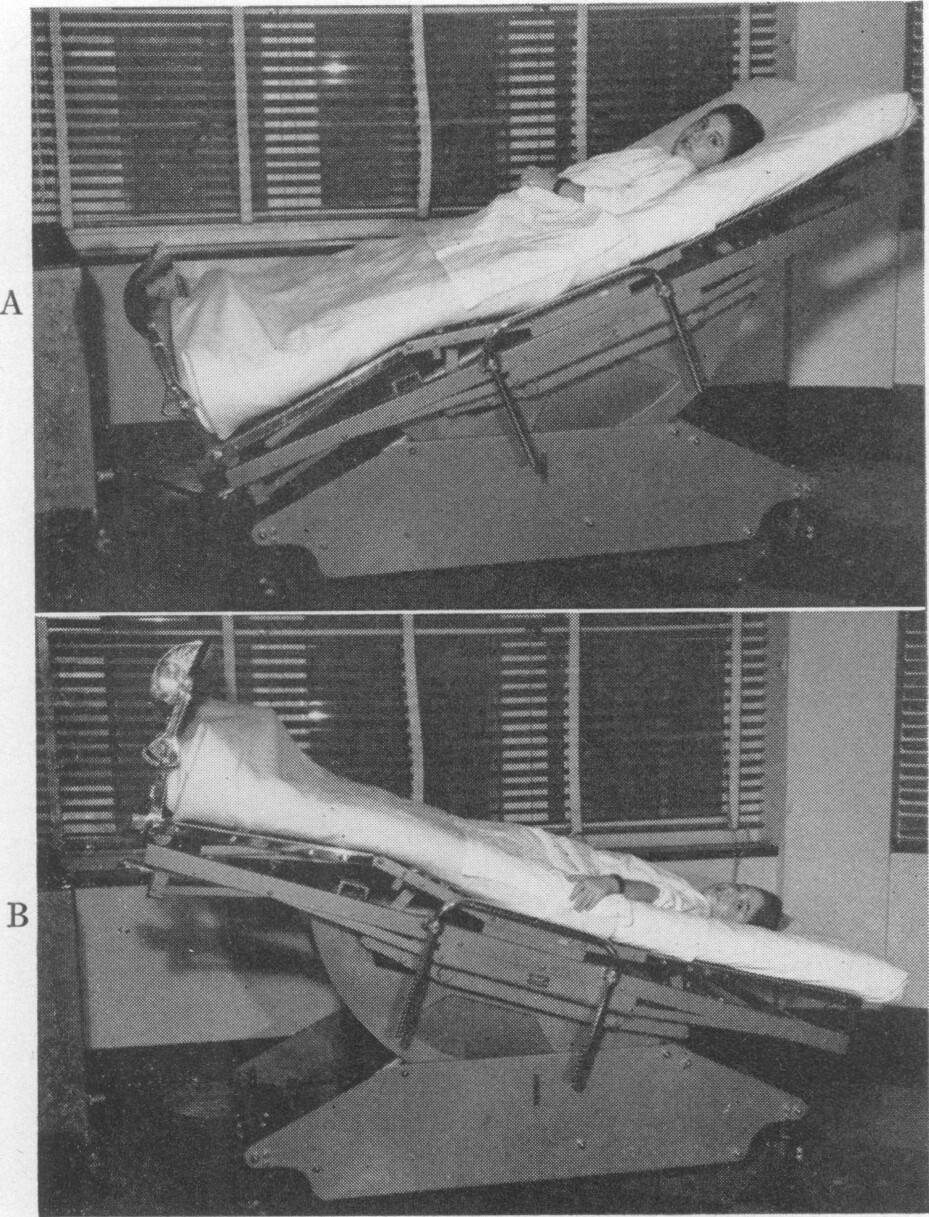
Rocking Bed
Pneumobelt
Iron Lungs:
full body surrounded by machine (Polio)
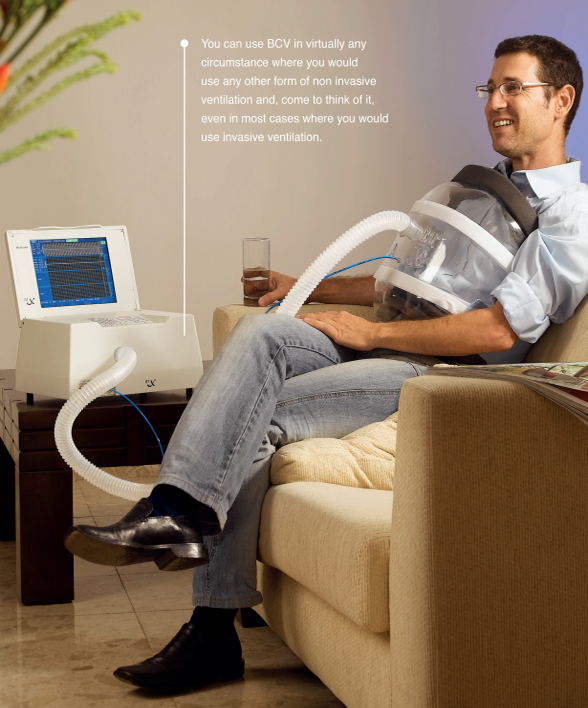
Cuirass:
chest piece attached to a vacuum
replaced iron lungs
Rocking Bed:
uses gravity to pull on abdomen & displace diaphragm
Head of bed UP → Diaphragm pulled down → Inhale
Head of bed DOWN → Diaphragm pulled up → Exhale
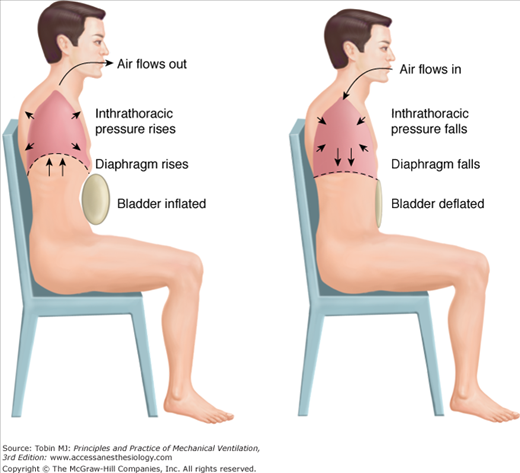
Pneumobelt:
forces diaphragm upward to assist w/ exhalation
What is High Frequency Ventilation (HFV)?
respiration is set much higher than normal rates
Low tidal volumes; i.e., very shallow, fast breathing
Limit the amount of lung inflation
Used in neonates & in cases of adults w/ severe ARDS
Lowers risk of Ventilator-Associated lung injury
Disadvantage - higher risk of atelectasis
What are the 3 types of High Frequency Ventilation (HFV)?
HF Positive Pressure Ventilation (HFPPV)
HF Jet Ventilation (HFJV)
High Frequency Oscillating Ventilation (HFOV)
What is HF Positive Pressure Ventilation (HFPPV)?
Same underlying principle as Positive Pressure Ventilation
But, respiratory rate is set high (50-150 bpm) (usually at machine’s limit)
Tidal volume is slightly GREATER THAN airway dead space
Applies negative pressure for Active Exhalation
What are indications for HFPPV?
Pulmonary Interstitial Emphysema (PIE)
Pulmonary barotrauma
Failed conventional mechanical ventilation
What are contraindications for HFPPV?
Same as any type of mechanical ventilation except for HFV is used to reduce risk of VAP
Increased risk of atelectasis
Increased secretions
What is HF Jet Ventilation (HFJV)?
Rapid pulses of air from a high-pressure source
Pulse duration = 0.02 seconds
Pulse frequency = 100-600 bpm
Tidal volume is slightly GREATER THAN airway dead space
Gas exchange is from newly pulsed air mixing w/ already present air, forming some amount of air turbulence
Creates the lowest possible alveolar pressure
Exhalation is Active
What is High Frequency Oscillating Ventilation (HFOV)?
Similar to HF Jet, pulse rate = 300-3000 bpm
Inhalation & Exhalation are “almost” simultaneous (goes so fast, it oscillates between inhale & exhale)
Tidal Volume is LESS THAN airway dead space
What is Heliox?
Use of Helium to help deliver oxygen
_____ flows faster through airway than non-helium enriched air
the higher the concentration of helium, the faster the airflow
What are indications for Heliox?
lower-airway obstruction (COPD, asthma), especially w/ hypercapnea
need to enhance aerosol delivery to lung periphery
need to facillitate weaning from mechanical ventilation
used as a last resort!
What are Non-Invasive Positive Pressure Ventilation Types?
CPAP
BIPAP
(Non-Invasive [NIV]) Continuous positive airway pressure (CPAP)?
Patient is spontaneously breathing, has adequate level of consciousness, hemodynamically stable, manage secretions
Delivers one constant level of air pressure
Air pressure is higher than atmospheric
Maintains open airway throughout the breath cycle
Triggers when the person inhales
Used primarily for mild obstructive sleep apnea (OSA)
Also used w/ acute pulmonary edema
Nose mask (typically)
What are the 2 Sleep Apnea types?
Obstructive Sleep Apnea (OSA)
Central Sleep Apnea
What is Obstructive Sleep Apnea (OSA)?
Physical obstruction interfering w/ breathing during sleep
Adults → usually due to combined effects of weaker muscles & obesity
Tongue & Pharynx “collapse” during sleep blocking airflow
Leads to snoring (Not all snoring is from OSA; but, all OSA has some level of snoring)
Pediatrics → typically due to large tonsils, macroglossia, or other craniofacial differences
What is Central Sleep Apnea?
Neurologic issue w/ brainstem central pattern generator
Slows down & stops triggering breathing
Typically occurs during sleep, but, doesn’t have to
(Non-Invasive [NIV]) What is Bi-level positive airway pressure (BiPAP)?
Variation of CPAP
Delivers 2 levels of air pressure:
Inspiratory Pressure/Inhalation Stress (IPAP): higher pressure
Expiratory Pressure/Exhalation Strain (EPAP); lower pressure
Reduced WOB while sleeping
Helps eliminate extra CO2
Multiple trigger settings: auto, timed, adaptive
Face mask (typically)
May have a humidification feature added
Used for mild to severe sleep apnea
OSA
central sleep apnea
Also used for COPD, CHF, chronic respiratory failure, & avoiding intubation or trach
(Non-Invasive [NIV]) What is MIPPV?
Intermittent daytime mouthpiece noninvasive ventilation
of BiPAP
Patient chooses to use it when needed
Uses a mouthpiece