bioethics
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
35 Terms
Coercion
“A patients decision is coerced when the patient is threatened, either explicitly or implicitly, with unwanted and avoidable consequences unless the patient makes the desired choice”
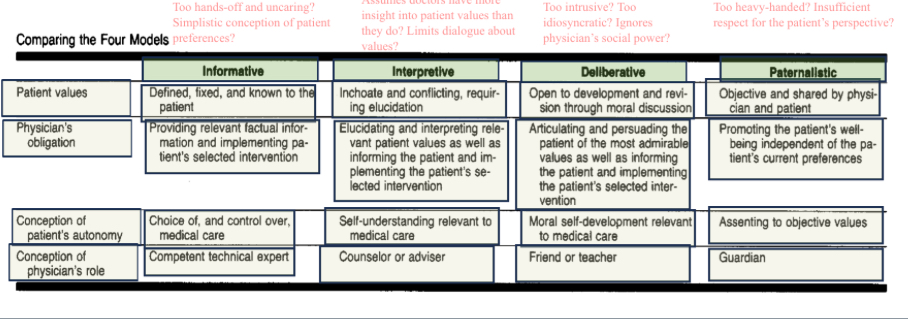
Ezekiel and Linda Emanuel “Four Models of the Physician-Patient Relationship
Agency, Authenticity, and Competence
Brudney and Lantos think that the value of agency stands behind the idea of decisional competence
Brudney and Lantos attribute to Kant the view that we ought to always respect the decisions of competent agents
Brock’s definition of competence may appeal to the ideal of authenticity
Manipulation
Withholding information
Emotional manipulation
Manipulative framing of information
They are not told of alternative treatments to the one the physician prefers, or if significant risks or side effects of a recommended treatment
Physicians manner and tone
Autonomy
Authenticity and agency
Two duties
A negative duty to ultimately respect the choices of competent patients (even unwise ones).
•But also a positive duty to do what we can to facilitate more autonomous, more responsible decision-making.
The Traditional View
The role of doctors is to restore health and keep patients alive.
The Problem
New medical advances dramatically increased the power of doctors to extend life. But sometimes this was of questionable benefit to the patient and served only to extend the dying process.
The Right to Refuse Life-sustaining Treatment
The legal doctrine of informed consent seemed to guarantee competent patients the right to refuse
Dresser and Robertson
Skeptical of relying the patient’s former directives or former values to determine proper care for the patient now, especially for cases where the patient remains responsive and communicative
Dworkin
Experiential interests: Things a person cares about, which seems good or bad for her, because she likes or dislikes experiencing them
Critical interests: Things that lend genuine meaning and coherence to our lives, valuable achievements, meaningful experiences
Beneficence should be directed towards the person, not just as he is now, but in the context of the whole life
Autonomy
we should respect autonomy in large part because they have an interest in living a life of integrity: we want to let “people lead their lives out of a distinctive sense of their own character, a sense of what is important to them.” (Dresser 33)
What is the “orthodox view” about how we should make decisions for incompetent patients?
Advance Directive: If we should defer to the choice of a competent patient about her present medical care, then we should defer to the choice of a formerly competent patient about her future medical care in the event that she should become incompetent.
2.Substituted Judgment: If the formerly competent patient never expressed a choice about her future medical care, then we should do what we believe the formerly competent patient would have chosen, given our knowledge of her character, values, and aims.
3.“Objective Best Interests”: If we cannot determine what a person would have chosen, we should make a decision in the best interests of the patient from a medical point of view.
Declaration of Helsinki
“Clinical research on a human being cannot be undertaken without his free consent after he has been informed” (1964).
Canterbury v. Spence
“True consent to what happens to one's self is the informed exercise of a choice, and that entails an opportunity to evaluate knowledgeably the options available and the risks attendant upon each” (US Court of Appeals 1972).
The Standard
The general nature of the proposed procedure.
2.Risks (including their seriousness, their probability, their timing) which a reasonable person would want to know.
•Common risks
•Uncommon serious risks like death, serious disability
3.Medically appropriate alternatives to the treatment, including the alternative of no treatment.
4.The expected benefits of treatment.
---------------
5.Conflicts of interest?
6.Particular facts about the provider or facility
Exceptions to the Requirement to Obtain Informed Consent
It is widely believed that there are some exceptions to the duty to obtain informed consent, but there is disagreement about which exceptions are valid and how broad they are.
•Lack of decision-making competence (e.g., the patient is a young child, or is unconscious, or has severe dementia)
•Emergency (no time to obtain consent)
•Public health emergency (refusal of treatment poses a threat to others)
•Waiver (patient does not want to be fully informed or to make the decision herself)
Paternalism
“The informed consent doctrine amounts to a rejection of this traditional authoritarian and paternalistic conception of the physician-patient relationship.
But why should that traditional conception be rejected, given its long and important historical role and its seemingly reasonable character?
To answer that question, the values served by the doctrine of informed consent must be examined.” (Brock, “Informed Consent,” 24)
Regulation of Medicines
Until the 1900s, foods and drugs were unregulated
first regulations require drugs be properly labeled
the predecessor to the US food and drug administration was created in 1906
the Canadian Food and Drug Act was enacted in 1920
in 1937, the S. E. Massengill Company took the popular antibiotic sulfanilamide and combined it with diethylene glycol to make it into a syrup. But diethylene glycol turned out to be poisonous and at least 105 people in the US died.
As a result, a 1938 bill was passed in the US Congress that required drugs to be tested for safety before being put on the market; a similar law passed in Canada in 1951
The Current Gatekeeper
Pharmaceuticals require regulatory approval for safety and efficacy before they may be sold.
Many pharmaceuticals require a physician prescription before a patient can access them
The Argument from Medical Outcomes
Does the prescription system improve or worsen medical outcomes?
•Flanigan appeals to an empirical study (Peltzman 1987) claiming that the prescription system does not reduce accidental or suicidal poisonings.
•Another study suggests that prescription requirements reduce availability and worsen health.
The Epistemic Argument
The patient is in a better position than a physician to judge whether the only benefits or risks of consenting to a treatment are justified
Plastic surgery comparison
If patients can assume risks for overall benefits in this case why not for prescription drugs as well?
Adderall for All
A stimulant combining amphetamine and dextroamphetamine.
•Currently prescribed to treat ADHD.
•Also can be used (illegitimately) as a “study drug” and performance enhancer or as a recreational drug.
•Adderall generally has only mild side effects when taken at lower dosages. Higher dosages can lead to various physical and psychological side effects.
•Flanigan would make it possible for all competent adults to buy Adderall without a doctor’s prescription.
The Respect for Autonomy
The third and strongest justification is based on the non-consequentialist premise that physicians ought to respect a patients autonomous decisions even if they’re not in their best interest
Antibiotics
Widespread use of antibiotics can create bacterial resistance to antibiotics (“superbugs”).
•Therefore, using antibiotics can impose harms on others.
•Flanigan concedes that antibiotics should be controlled by prescription.
Expanded Access to Try By Laws
•Starting in the 1970s, it has been possible for patients with life-threatening illnesses to seek permission from the FDA to access experimental therapies which have not yet been approved by the FDA and which have only passed Phase I trials (testing basic safety for human beings).
•The equivalent program in Canada is known as the “Special Access Programme.”
•Starting in 2014, many US states have passed “right to try” laws. Right to try laws allow patients to bypass FDA permission, but have been little used by the pharmaceutical companies.
The Best-Interest Standard
Decisions about children often cannot appeal to their former values – since they didn’t have any.
•It seems that surrogate decisions makers for parents must appeal to some understanding of the child’s interests.
•Legal cases involving children in other domains (e.g., custody disputes) often appeal to the child’s best interests.
•For this reason, the law has often assumed that the state may intervene with parental decisions if this is in the child’s best interests.
•What does it mean to promote the child’s best interests?
•Buchanan and Brock: “acting so as to promote maximally the good of the individual”
•Beauchamp and Childress: “a surrogate decision maker must determine the
Best Interest Objections
What is in the child’s best interests, even from a medical point of view, is not always clear. (Should ADHD be medicated? Is a treatment worth the side effects it may occasion?)
•Religious parents who make decisions that are not in their children’s best interests from a medical perspective might believe they are acting in their children’s best interests from a clinical perspective.
•Sometimes decisions to maximize the child patient’s good would compromise the interests of other family members.
Conditions on Interventions
Diekema offers eight conditions that must be met for state intervention to be justified (252-254). These can be summarized thus:
•Is there good evidence that the refused treatment is necessary to prevent a significant risk of immediate serious harm (and that there is no other effective alternative more acceptable to the parents)?
• Do the expected benefits of the treatment significantly outweigh the burdens?
•Would we be willing to generalize this intervention to similar cases, and would most parents agree that this would be reasonable?
The Harm Principle Applied
Refusal of blood transfusion or insulin for diabetes.
•Focus on “objective harm,” not parental views about “spiritual” or “moral” harm
•Uncertain and burdensome treatment: The case of Colin Newmark
•Three-year-old diagnosed with Burkitt’s Lymphoma.
•Doctors believed chemotherapy would provide him a 40% chance of survival.
•The parents, Christian Scientists, refused treatment. Instead of allowing an uncertain and painful treatment, they would rely on prayer.
•Vaccine refusal
•Cases where there is strong “herd immunity”
•Emergency cases (e.g., possible tetanus exposure)
•Public health emergencies (pandemics)
Best Interests or Harm?
•Shah, Rosenberg, & Diekema suggest that the case might have been resolved differently if the courts had relied on a harm standard rather than a best interests standard.
•It is arguable whether the experimental therapy was in Charlie’s best interests.
•On the other hand: “While the details of Charlie Gard’s case are difficult to know from a distance, it is hard to argue that allowing his parents opportunities to explore experimental options was sufficiently harmful to Charlie that the choice should have been precluded by the courts” (938).
Parental Authority of Medicine
•Parents often know their children’s interests best.
•Parents are better positioned to know how decisions affect other family members.
•Parents have an interest in raising their children according to their own values and beliefs.
•Family needs protection from intrusion to flourish.
Parental Authority is Limited
•“The doctrine of parens patriae holds that the state may act as ‘surrogate parent’ when necessary to protect the life and health of those who cannot take care of themselves, including children.”
•It is uncontroversial that the law ought to prohibit clear cases of child abuse and exploitation.
•But at least sometimes it seems like the state can intervene to address neglect too.
•When can the state intervene to prevent medical neglect?
(Diekema 244)
Parents Refusing Treatment
Failure to seek medical care for child in an emergency
•Refusal of medical treatment for child for religious reasons (e.g., Jehovah’s Witness rejects blood transfusion)
•Parent opts for alternative medicine child in lieu of standard medicine for a serious condition, like cancer
•Parent refuses to vaccinate child
•Parent declines to have the child’s cleft palate treated
•Parent does not seek medical condition for disruptive but non-life threatening skin disease