Vander's Cardiac Physiology
1/163
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
164 Terms
WITTF: the percentage of blood volume that is erythrocytes
hematocrit
When blood is centrifuged, what are the layers formed (from top down)?
plasma, platelets and leukocytes, erythrocytes
What is the normal hematocrit of a healthy male?
45%
What is the normal hematocrit of a healthy female?
42%
Estimated number of capillaries?
10 billion
WITTF: the collective term for arterioles, capillaries, and venules
microcirculation
What group of organs receives most of the blood flow in the body at rest?
abdominal organs
What organs have a portal system?
liver (hepatic portal system) and pituitary (hypophyseal portal system)
WITTF: the pressure exerted by any fluid
hydrostatic pressure
Flow rate is calculated by:
F = change in P / R
The relationship between viscosity and resistance is:
directly proportional
What can cause an increase in the viscosity of blood?
an increase in hematocrit
What can cause an increase in hematocrit?
extreme dehydration
What are the three determinants of resistance?
blood viscosity, length of blood vessel, radii of blood vessel
WITTF: the fibrous sac enclosing the heart
pericardium
WITTF: the inner layer of the pericardium closely attached to the heart
epicardium
WITTF: the walls of the heart primarily composed of cardiac muscles
myocardium
WITTF: the lining of the inner surface of the heart and blood vessels
endothelium
WITTF: a muscular wall that separates the two ventricles
interventricular septum
WITTF: the right atrioventricular valve
tricuspid valve
Why is the tricuspid valve called so?
it has three fibrous flaps
How many flaps does the mitral valve have?
two
What is another name for the mitral valve?
bicuspid valve
t/f: the opening of the AV valves is a passive process achieved by pressure differences
true
WITTF: condition in which AV valves are pushed up into the atria
prolapse
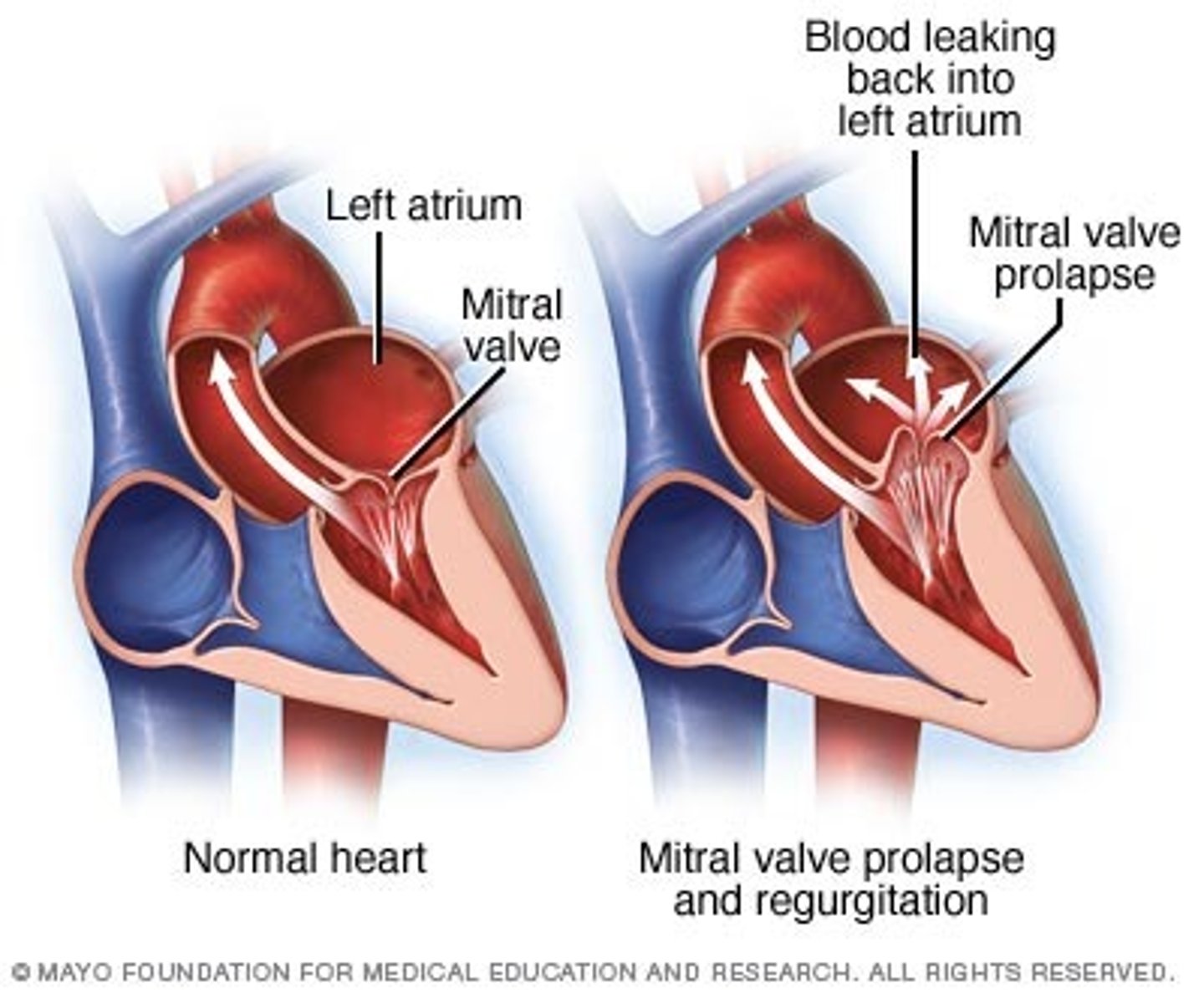
WITTF: muscular projections that the AV valves are fastened onto to prevent prolapse
papillary muscles
WITTF: fibrous strands that connect AV valves to papillary muscles
chordae tendineae
t/f: the semilunar valves are open and closed actively
false
t/f: a little blood is ejected back into the veins (vena cava and pulmonary vein) during atrial systole
true
WITTF: system of ~1% of cardiac cells that initiates the heartbeat and helps spread the impulse rapidly throughout the heart
conducting system
Cells where in the heart secrete a family of peptide hormones known as atrial natriuretic peptide?
atria
What nerve provide parasympathetic stimulation to the heart?
vagus nerve
What do sympathetic postganglionic fibers release to the heart?
norepinephrine
Where do sympathetic postganglionic fibers terminate in the heart?
everywhere
What do parasympathetic postganglionic fibers release to the heart?
acetylcholine
Where do parasympathetic postganglionic fibers terminate in the heart?
atria
What type of receptors are the norepinephrine/epinephrine receptors of the heart?
beta adrenergic
WITTF: effects that change heart rate
chronotropic
What type of receptors are the acetylcholine receptors of the heart?
muscarinic
WITTF: effects that cause a change in conduction velocity in the AV node and thus the speed of electrical conduction in the heart
dromotropic
WITTF: effects that cause a change in the force or energy of muscle contractions
inotropic
WITTF: effects that cause a change the rate in myocardial relaxation
lusitropic
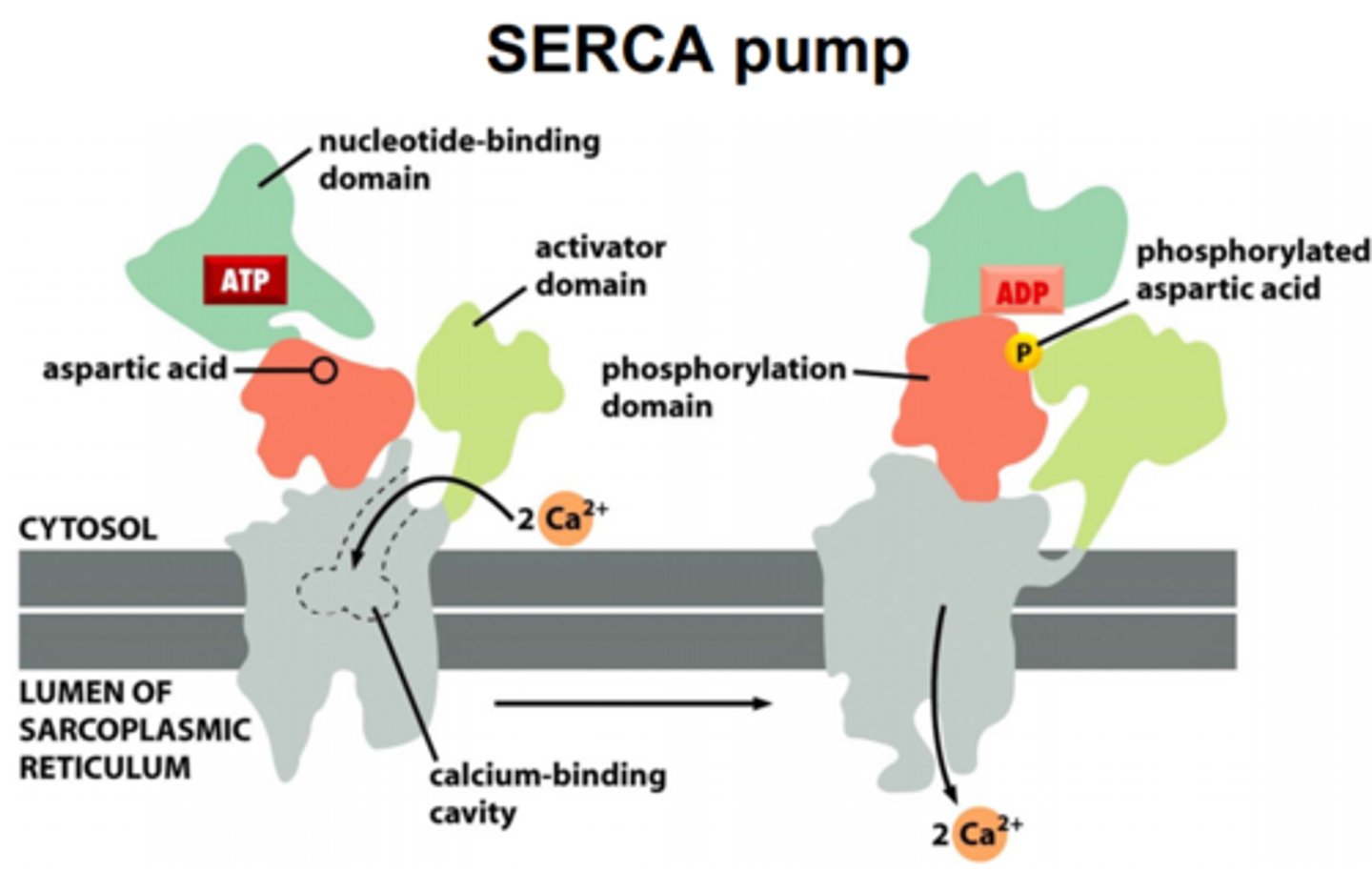
An increase in the cytoplasmic calcium in cardiac myocytes leads to what?
increased inotropy but decreased lusitropy
Is dopamine a positive or negative chronotrope?
positive
WITTF: primary active transporter that pumps calcium from cytoplasm of myocyte to sarco-endoplasmic reticulum
SERCA
WITTF: arteries supplying the myocardium
coronary arteries
Where do coronary arteries exit from?
the first part of the aorta
WITTF: a single large vein that all the cardiac veins drain into
coronary sinus
Does coronary blood flow enter the vena cava?
no
Where does the initial depolarization occur during a heartbeat?
sinoatrial node
Where is the sinoatrial node located?
right atrium near superior vena cava
Where is the atrioventricular node located?
base of right atrium
How long does it take action potentials to be conducted through the AV node?
0.1 seconds
What is the point of delaying the action potential at the AV node?
Allows atrial contraction to be completed before ventricular excitation occurs
WITTF: conducting-system fibers that is the only electrical connection between the atria and ventricles
bundle of His
Within the interventricular septum, what does the bundle of His divide into?
left and right bundle branches
What do the left and right bundle branches come into contact with?
Purkinje fibers
WITTF: large conducting cells that rapidly distribute the impulse throughout the ventricles
Purkinje fibers
What do Purkinje fibers come in contact with?
ventricular myocardial cells
Where does depolarization of the ventricles begin?
at the apex
Why is resting membrane potential closer to the equilibrium for potassium (-90mV) than for sodium (+62mV) it's -> (-60mV)?
cell membrane is more permeable to potassium than to sodium
WITTF: calcium channels that open slowly compared to sodium channels and remain open for a prolonged period of time
L-type calcium channels
What keeps the plasma membrane depolarized at a plateau value (~0mV)?
opening of L-type calcium channels that balances the outflow of potassium ions from the cell
When does repolarization occur again in myocytes?
calcium channels inactivate and potassium exits the cell
Is the plateau phase in the action potential of atrial cells longer or shorter than that of ventricular cells?
shorter
WITTF: the gradual depolarization in conducting system cells
pacemaker potential
WITTF: sodium channels in pacemaker cells that open when membrane potential is at negative values
F-type sodium channels
WITTF: calcium channel in pacemaker cells that open briefly as a final depolarizing boost to the pacemaker potential after the F-type sodium channels
T-type calcium channels
WITTF: the capacity for spontaneous, rhythmical self-excitation
automaticity
What provides the SA node with automaticity?
pacemaker potential
WITTF: other cells in the conducting system besides the SA node that produce their own action potentials with automaticity
ectopic pacemakers
What happens if the AV node fails?
autorhythmic cells in the bundle of His or Purkinje fibers begin to initiate excitement at their own inherent rate
What is the permanent treatment for all AV conduction disorders?
implantation of an artificial pacemaker that electrically stimulates the ventricles at a regular rate
t/f: atrial systole is not essential unless there is strenuous exercise
true
WITTF: the primary tool for evaluating the electrical events within the heart
electrocardiogram (ECG)
What event does the P wave correspond with?
atrial depolarization
What event does the QRS complex correspond with?
ventricular depolarization
Why is the QRS complex so complex?
the paths taken by the waves of deflection through the thick ventricular walls differ from instant to instant
What event does the T wave correspond with?
ventricular repolarization
Why is atrial repolarization not evident in the ECG?
it occurs at the same time as the QRS complex
WITTF: typical clinical ECGs with multiple combinations of recording locations on the limb and chest
ECG leads
An ECG is not what?
a direct record of changes in membrane potential across individual cardiac cells
What does an ECG measure?
the currents generated in the extracellular fluid of many cardiac cells
What type of heart defects can a ECG not detect?
mechanical defects
What is the order of electrical events for a partial/complete atrioventricular block? Why?
PQRSTP; P wave still occurs but signal cannot reach ventricles
What happens when the current through voltage-gated potassium channels is delayed and reduced?
the T wave is delayed because ventricular repolarization takes longer
What does the entrance of small amounts of calcium ions from L-type calcium channels trigger?
further release of large amounts of calcium from ryanodine receptors in the sarcoplasmic reticulum membrane
What receptors in the sarcoplasmic reticulum in cardiac muscle cells release large amounts of calcium?
ryanodine receptors
What pumps return calcium to the extracellular fluid and cytoplasm?
Ca2+-ATPase pumps, Na+/Ca2+ cotransporters
t/f: the strength of contraction in cardiac muscle can be altered by the amount of calcium released
true
Why can't the heart generate tetanic contractions?
a long absolute refractory period
What causes a long refractory period?
inactivation of sodium channels
How long does each cardiac cycle approximately last?
0.8 sec
How many secs of the cardiac cycle is systole?
0.3
How many secs of the cardiac cycle is diastole?
0.5
WITTF: the first part of systole in which the ventricles contract but all the valves are closed, so no blood is ejected
isovolumetric ventricular contraction
In isovolumetric ventricular contraction, the muscle develops tension, but does not _________
shorten
WITTF: the volume of blood ejected from each ventricle during systole
stroke volume
WITTF: what happens when the pressure in the ventricles exceeds that of aorta and pulmonary trunk after isovolumetric ventricular contraction
ventricular ejection
WITTF: the first half of diastole, where the ventricles relax and the AV and semilunar valves close
isovolumetric ventricular relaxation