NSG 3040 Neuro | 77 questions and answers | 2025 latest update | Pass Guranteed
1/76
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
77 Terms
central nervous system
brain and spinal cord
peripheral nervous system
inculdes cranial and spinal nerves
- autonomic and somatic systems
neurons
Individual cells in the nervous system that receive, integrate, and transmit information.
neurotransmitters
communicate messages from one neuron to another or to a specific target tissue
- can potentiate, terminate, or modulate a specific action or can excite or inhibit a target cell
- many neuro disorders are caused by an imbalance of neurotransmitters.
health history - neuro
ask about
- pain
- seizures
- dizziness (abnormal sensation of imbalance or movement) and vertigo (illusion of movement, usually rotation)
- visual disturbances
- abnormal sensations
- past family history -> avm arterial venous malformation
arterial venous malformation
-abnormal coupling of arteries and veins
- congenital malformation
-hemorrhage may occur
arteries
carry oxygenated blood away from the heart
veins
Blood vessels that carry blood back to the heart
cranial nerve 1
Olfactory
- responsibe for smell (olfaction)
cranial nerve 2
Optic
- responsible for vision and transmitting visual information from the retina to the brain
cranial nerve 3
Oculomotor
- primarily controls the movement of eye muscles including those that control pupil constriction and position of the eyelid
cranial nerve 4
Trochlear
- controls the superior oblique muscle of the eye which aids in downward and inward eye movements.
cranial nerve 5
Trigeminal
- sensation in the face and motor functions in the face and mouth such as chewing
cranial nerve 6
Abducens
- controls the lateral rectus muscle of the eye which is involved in outward eye movement.
cranial nerve 7
facial
- responsible for controlling facial expressions, taste sensation from the anterior two thirds of the tongue including salivary glands and tear glands.
cranial nerve 8
Vestibulocochlear
- responsible for hearing and balance and spatial orientation
cranial nerve 9
Glossopharyngeal
- involved in taste sensation from the posterior 1/3 of the tongue as well as swallowing and controlling certain throat muscles
cranial nerve 10
Vagus
- controls the parasympathetic nervous system.
cranial nerve 11
accessory
- primarily controls the sternocleidomastoid and trapezius msucles which are involved in head and shoulder movements.
cranial nerve 12
Hypoglossal
- controls the muscles of the tongue, allowing for speech and swallowing
neuro assessment
- consciousness and cognition: mental status, intellectual function, thoughts...
- cranial nerves
- motor system: muscle size, muscle tone and strength
- sensory system: tactile sensation, superficial pain, temperature,
- reflexes
- vitals
glasgow coma scale
scored between 3 and 15, with 3 being the worst and 15 the best. It is composed of 3 parameters: best eye response (E -4), best verbal response (V - 5), and best motor response (M-6).
what tests are commonly used to assess neuro injury
CT and MRI
- can be done with or without contrast (need consent from patient for contrast)
contrast agent used for CT MRI
- get consent
- no allergies to iodine or shellfish
- do they have adequate kidney function to excrete the contrast agent
cerebral angiography
x-ray imaging of the arterial blood vessels in the brain after injection of contrast material
lumbar puncture
testing cerebrospinal fluid for RBC, WBC, infection, viruses - commonly done for meningitis.
- position the patient on their side for the procedure - want to premedicate but not too much still need to be conscious.
- patient will have pain and pressure
- nurse should provide comfort and will be taking vital signs every 5 min
what position should the patient be in after lumbar puncture
patient should be in supine position after lumbar puncture because you want pressure on injection site and want CSF to equalize.
lumbar puncture complications
headache
nausea
if lasts for 60 min after then tell the provider
how do you know if CSF is leaking out
look at the dressing site and allow it to dry. if it dries in halos then it is CSF fluid.
what is the most important indicator of a patients neuro condition
level of responsiveness and consciousness
LOC
- it is a continuum from normal alertness and full cognition to coma
- altered LOC is not the disorder but the result of a pathology
coma
unconsciousness, unarousable unresponsiveness
- prolonged state of unconsciousness in which an individual is unresponsive to external stimuli including pain
akinetic mutism
unresponsiveness to the environment; the patient makes no movement or sound but sometimes opens the eyes
persistent vegetative state
devoid of cognitive function but has sleep-wake cycles
locked in syndrome
inability to move or respond except for eye movements due to a lesion affecting the pons
monro kellie hypothesis
because of limited space in the skull, an increase in any one of the components of the skull (brain tissue, blood, CSF) will cause a change in the volume of the others.
with disease or injury ICP may increase which causes
- a decrease in cerebral perfusion and causes ischemia, cell death, and further edema
- brain tissues may shift through the dura and result in herniation
autoregulation brain
refers to the brains ability to change the diameter of blood vessels to maintain cerebral blood flow.
does CO2 play a role in increased ICP
decreased co2 results in vasoconstriction and increased co2 results in vasodilation
CPP
cerebral perfusion pressure (closely linked to ICP)
- CPP = MAP - ICP
- normal: 60-80
- CPP of less than 50 results in permanent neuro damage.
normal MAP
60-180
- average pressure within a person's arteries during one cardiac cycle
normal ICP
5-10
how to maintain cerebral perfusion
- avoid extreme head rotation
- HOB may be flat or elevated 30 degrees
- head should be midline and straight
- monitor Resp status
early manifestations of increased ICP
- Changes in LOC
- Any change in condition:
Restlessness, confusion, increasing drowsiness, increased respiratory effort, purposeless movements
- Pupillary changes and impaired ocular movements
- Weakness in one extremity or one side
- Headache: constant, increasing in intensity, or aggravated by movement or straining
late signs of increased ICP
- projective vomitting
VS: increase in systolic BP, widening of pulse pressure, and slowing of HR, pulse may fluctuate rapidly from tachycardia to bradycardia, temp increase
- hemiplegia (paralysis of one side)
- decortication
- decerbration
- flaccidity
- respiratory pattern alterations including cheyne stokes breathing and arrest
- loss of brainstem reflexes: pupil, gag, corneal, and swallowing
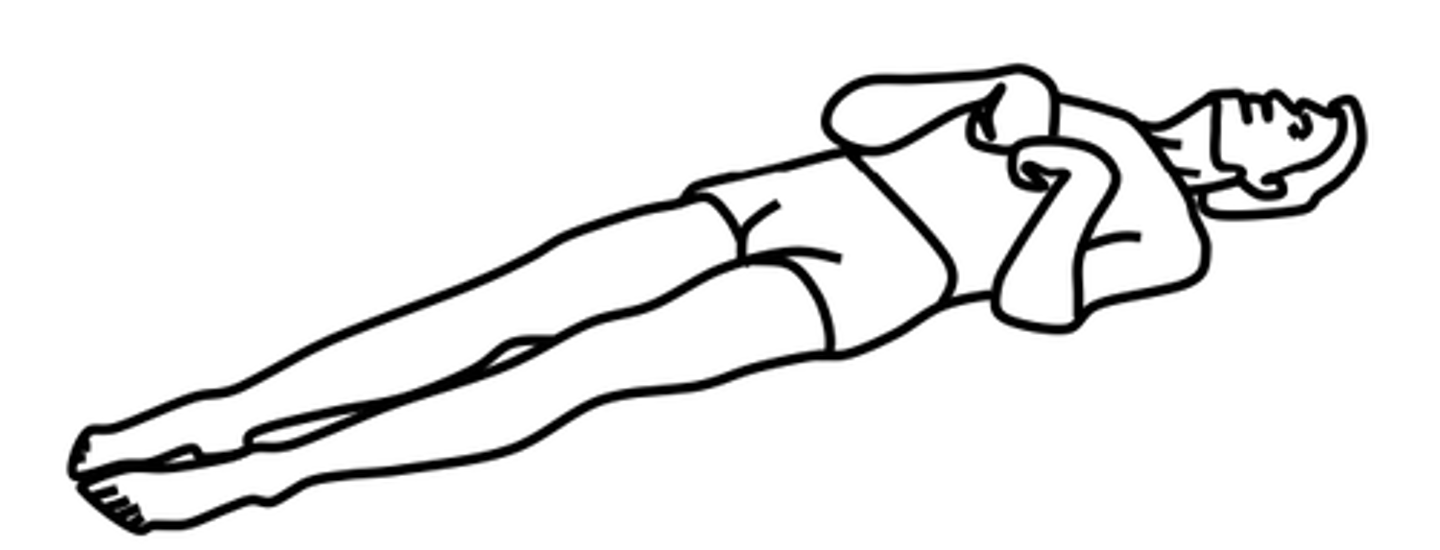
Decorticate posturing
arms flexed inward and bent in toward the body and the legs are extended
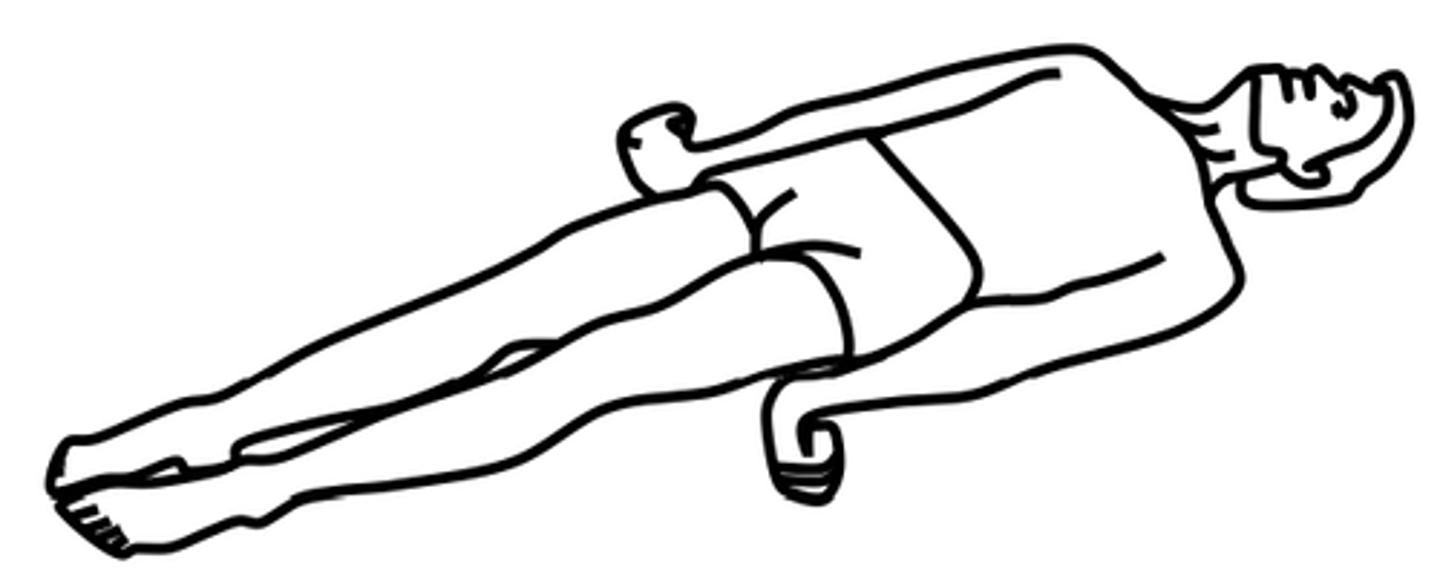
Decerebrate posturing
position of an unconscious person where the upper extremities and lower extremities are extended and the wrists are flexed
primary brain injury
- caused by the initial damage
- contusions, lacerations, damage to blood vessels, acceleration/decerleration, or by foriegn object penetration
secondary injury
- damage that evolves after the initial insult
- caused by cerebral edema, ischemia, or chemical changes assoc with the trauma
Cushing triad (herniation syndrome)
bradycardia, hypertension, bradypnea
close brain injury
blunt trauma - acceleration/deceleration injury occurs when the head accelertes and then rapidly decelerates, damaging brain tissue
concussion
a temporary loss of consciousness with no apparent structural damage
contusion
longer period of unconsciousness more severe injury with possible surface hemorrhage.
after head trauma you should observe/report
- observe for any changes in LOC
- difficulty in awakening, lethargy, dizziness, confusion, irritability, anxiety
- difficulty in speaking or movement, headache, vomiting
- patient should be aroused and assessed frequently
open brain injury
object penetrates the brain or trauma is so severe that the scalp and skull are opened
- scalp wounds bleed a lot
skull fractures
- usually have localized, persistent pain
- may have bleeding and CSF leakage from nose, pharynx, or ears
- csf leak = halo
management of the patient with a head injury
if patient has a fall you always want to assume that a cervical spine injury is present till you rule out. ruled out by a scan and radiography
- patient will wear a c collar around neck to keep it immobile until ruled out
where is an epidural hemorrhage
bleeding between dura and skull
where is a subdural hematoma
collection of blood under the dura mater
- usual vessels are bridging veins from skull to brain tissue
where is an intracerebral hematoma
a hematoma located inside the brain
cause, treatment and describe an epidural hematoma
- patient may have a brief loss of consciousness with return of lucid state; then as hematoma expands, increased ICP will often suddenly reduce LOC.
- emergency situation
- treatment: reduce ICP, remove the clot, and stop bleeding (burr holes or craniotomy)
- patient will need respiratory support
- this is an arterial bleed and the usual vessel is the middle meningeal artery. bleeds more
acute vs chronic subdural hematoma
- acute: symptoms develop over 24-48 hours and requires immediate craniotomy and control of ICP
- Chronic: develops over weeks to months, causative injury may be minor and forgotten, s/s may fluctuate, treatment is evacuation of the clot
- happens more frequently in older adults secondary to brain shrinking that places tension on bridging veins.
cause and treatment of intracerebral hemorrhage
- may be caused by trauma or a nontraumatic cause
- treatment: supportive care, control of ICP, admin of fluids, electrolytes, and antihypertensive meds. craniotomy or craniectomy to remove clot and control hemorrhage; this may not be possible because of the location or lack of circumscribed area of hemorrhage.
ischemic stroke
a clot blocks blood flow to an area of the brain
- accounts for thrombotic, embolic, or TIA
- number one cause is AFIB
- accounts for about 80% of strokes
- s/s: sudden weakness or numbnesss in the face, arm or leg. difficulty speaking or understanding speech; confusion; trouble with vision; headache
- treatment: often TPA to dissolve the clot and sometimes mechanical clot retrieval procedures
hemorrhagic stroke
- consists of aneurysms, AVM, and HTN
- occurs when a blood vessel in the brain ruptures and blood leaks into surrounding brain tissue
- s/s: severe headache, n/v, weakness or numbness, difficulty speaking, vision problems, LOC
- treatment: craniectomy, burr hole, and evacuate any bleeding
- risk factors: patients w afib, htn, smoking, and unhelathy lifestyle
right sided facial droop
left sided brain injury
stroke assessment
B = balance
E = eyes - can they open/close
F = face - drooping
A = arms - issues with strength or mobilization in arms
S = speech - slurred. dysarthria
T = time - tissue death
- call RRT. it is a stroke until it is not
swallowing and stroke
- at high risk for aspiration
- strokes can cause dysarthria which is difficulty articulating words.
- may have inability to nourish themself via oral route
mainentance of airway for neuro dysfunction
- positioning to faciliate drainage or oral secretions with HOB usually elevated 30 degrees to decrease venous pressure
- suction with caution
- prevention of aspiration and respiratory insufficiency
- monitor ABG's, ventilation, and mechanical vent
- monitor for pulmonary complications, aspiration, and potential ARDS
interventions for stroke
- maintain airway - HOB at 30 degrees
- oral suctioning
- aspiration prevnetion signage
- monitor ABGs
- keep accurate I&O and daily weight
- patient can become easily constipate - never want them to bear down because that increases cranial pressure
- may give ativan to slow or stop seizure
spinal cord injury
- result of concussion, contusion, laceration, or compression of spinal cord
- primary injury is the result of the initial trauma
- secondary injury isually the result of ischemia, hypoxia, and hemorrhage that destroys the nerve tissues. thought to be reversibel or preventable during the first 4-6 hours after injury
SCI care
- monitor respirations and breathing pattern
- assess for spinal shock
- monitor for bladder retention ro distention, gastric dilation, and ileus
spinal shock
- A sudden depression of reflex activity below the level of spinal injury
- Muscular flaccidity, lack of sensation and reflexes
- determination of long term dysfunction should be delayed to allow for spinal shock to resolve
autonomic dysreflexia s/s and triggers
Acute emergency!
Occurs after spinal shock has resolved and may occur years after the injury.
Autonomic nervous system responses are exaggerated.
Symptoms include severe pounding headache, sudden increase in blood pressure, profuse diaphoresis, nausea, nasal congestion, and bradycardia.
Triggering stimuli include distended bladder (most common cause), distention or contraction of visceral organs (e.g., constipation), or stimulation of the skin.
who does AD occur in
Occurs in persons with SC lesions above T6.
interventions for AD
- place patient is seated position to lower BP
- eliminate triggers by: empty the bladder using a urinary catheter or irrigate or chagn indwelling catheter. examine recutm for fecal mass. examine skin. examine other stimulus.
- administer ganglionic blocking agents such as hydralazine hydrochloride (Apresoline) IV.
contractures
muscle loss because of lack of mobilization