Module 5: section 3 - electrical activity of the heart
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
60 Terms
what type of organ is the heart
electro-mechanical
what does electro-mechanical mean
it has both electrical activity and large muscle to contract
what electrical activity is the heart experiencing
it generates and conducts action potentials like nerves
what types of cells does the heart have to accommodate its electro-mechanical
a type to contract and do the mechanical work and another type that is electrical that generate and propagate action potentials to the contractile cells
how can the SNS and/or PNS affect heart rate
physical and emotional stress can cause changes in HR
Epinephrine being released to increase rate (SNS)
illness/injury can cause an increase in blood flow to peripheral tissue, increases HR (SNS)
exercise increases a need for oxygen to muscles which brings more blood around the body
what are autorhythmic cells
specialized cardiac muscle cells that can produce action potential
what makes autorhythmics difference
they have ion channels that cause the membrane potential to slowly depolarize untl the threshold potential is reached and an action potential is fired instead of having a flat, constant resting membrane potential
what type channels do autorhythmic cells contain
If channels
what happens when If channels are activated
both sodium and potassium can enter the cell to cause depolarization of the membrane potential
what causes If channels to activate
either from the hyperpolarization-activated cyclic nucleotide-gated channel family, or that a type of calcium channel is involved (t-type)
what is unique about autorhythmic cells
the upstroke of the action potential is due to another type of calcium channel, the L-type channel, instead of sodium channels
where are autorhythmic cells found
sinoatrial node, atrioventricular node, bundle of His, Purkinje fibres
what is the sinoatrial node
a small area foind in the right atrial wall near the opening of the vanae cavae
what is the atrioventricular node
a small area found in the right atrium where the right atria and right ventricle come together
*often said to be located in theinteratrical septum since its around the centre of the heart
what is the bundle of His
a bundle that has specialized cells that arise from the AV node. divides into two bindle branches that go down each side of the septum to the bottom of the heart where they curve around and travel towards the atria
what are purkinje ribres
small fibres that branch off the bundle of His and spread along the inner surface of the ventricles
which autorhythmic cells have the fastest depolarization
the ones in the SA node; are considered the pacemaker cells
why are SA node autorhythmic cells considered the pacemaker cells
because they control heart rate and keep it at 70-80 beats/min (without an action potential present).
what happens when an action potential is generated via SA node
it conducts through the rest of the cardiac conduction system, overriding the pacemaker activity of other autorhythmic cells
what needs to happen for the ventricles to fill up wiwth blood completely
the blood from the atria must be removed into the ventricles; atrial excitation and contraction should be complete before the onset of ventricular contractions
why do the AV valves open during relaxation of the heart
because the pressure in the ventricles is lower than the atria pressure
what does opening of the AV vales help with
allowing the passive flow of blood from the atria to the ventricles
what does passive blood flow account for
~80% of total ventricular filling with the remaining 20% coming from when the atria contract
what happens during a normal heartbeat
the atria contract about 160msec before the ventricles
what criteria needs to be satisfied for efficient cardiac contraction
atrial excitation and contraction should be complete before onset of ventricular contractions
excitation of the cardiac muscle fibres needs to be coordinated
the pair of atria and the pair of ventricles must be functionally coordinated
why do the chambers need to have a coordinated contraction
because if different regions of a ventricular wall were to depolarize and contract at different times, then it would not be possible for ventricles to eject blood
what is ventricular fibrillation
when uncoordinated depolarization happens
how can the blood move throughout the body
the atria need to contract together and the ventricles need to contract together
what happens if the ventricles contracted out of sync
stress on the ventricular walls will happen without any reason and a pacemaker may be needed to re-coordinate the contraction
*is not normally dangerous, but can lead to more problems that are
how does the action potential fired by the SA node travel throughout the atria
by gap junctions and pathways
how do gap junctions help
by sending the depolarization signal between atrial cells
what pathways help with the spreading of action potential
interatrial pathway and internodal pathway
how do the interatrial and internodal pathways work
act like nervous tissue by moving the excitation wave faster than possible by gap junctions
where does the interatrial pathway extend
extends from right atrium to the left atrium and ensures that the wave of excitation spreads across both atria
what does the internodal pathway do
connects SA node to the AV node
how can the electrical signal move from the atria to the ventricles
only by the AV node and bundle of His due to there being a dense region of connective tissues between the atria and ventricles
what is the purpose of the AV nodal delay
to make sure the atria have has a chance to contract before the ventricles (160msec)
to maximize the atrial emptying of blood into the ventricles
what are the ventricles
a larger mass of muscle, hollow organs
why are gap junctions needed
to innervate the cells that the purkinje fibres to not reach
what is the "resting” membrane potential for a cardiac myocyte
~-80 mV
why do cardiac myocytes have a resting potential
since these cells have no pacemaker currents
what do cardiac myocytes have
well defined t-tubule system
what are the steps on how a myocyte is activated to initiate contraction
action potential in cardiac contractile cell cause L-type calcium channels to open
release of calcium
either the calcium directly interats with the contractile apparatus or interacts with ryanodine receptors on SR membrane to trigger more calcium to be released (CICR)
the influx of calcium initiates contraction of cardiac muscle
when does a cardiac muscle contraction end
when calcium is removed from the cytosol
*either by moving it across the plasma membrane or pumping it back into SR
why cant cardiac muscle not undergo summation and tenanus
since it would lead to inefficient, life-threatening contractile patterns
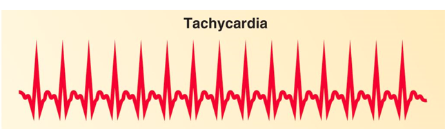
what is tachycardia
a heart rate that is faster than the normal resting heart rate
what can tachycardia do
decrease the cardiac output due to reduced ventricular filling
what does tachycardia look like
what is extrasystole
when a heartbeat is started by purkinje fibres rather than the SA node
what can extrasystole be a sign of
reduced oxygenation in healthy hearts
how does extrasystole work
ventricles contract before atria and therefore are not optimally filled with blood which leads to reduced cardiac output
is extrasystole dangerous
only if it is frequent
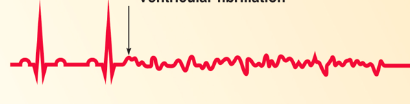
what is ventricular fibrillation
when the heart is quivering rather than pumping due to abnormal electrical activity in the ventricles
what can ventricular fibrillation cause
cardiac arrest with loss of consciousness and no pulse
what does extrasystole look like

what does ventricular fibrillation look like
what is complete heart block
third degree atrioventricular block
the impulse generated at the SA node does not travel to the ventricles forcing the pacemaker cells in the AV node to independently activate the ventricles
what independent rhythms does complete heart block allow to be seen on an ECG
p wave with regular P to P intervals
a QRS complex which does not always follow a P wave
what does a complete heart block look like
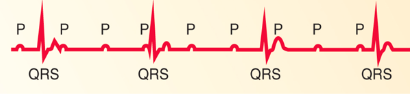
how does complete heart block present
abnormally low heart rate and blood pressure