Salivary Glands
1/130
Earn XP
Description and Tags
Ten Cate, Chapter 11
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
131 Terms
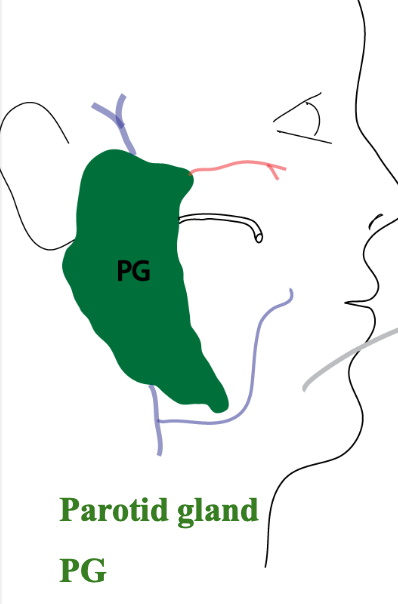
What are the three pairs of major salivary glands?
Parotid
Submandibular
Sublingual
What are the functions of saliva?
Wetting
Lubricating
Digestive
Mineralization of teeth
Protective
What do parotid glands produce?
A serous (watery) secretion and produces only 20% of daily saliva volume (but includes SIgA and other defense chemicals) but of the components it makes, it is one of the major providers of protection in the oral cavity
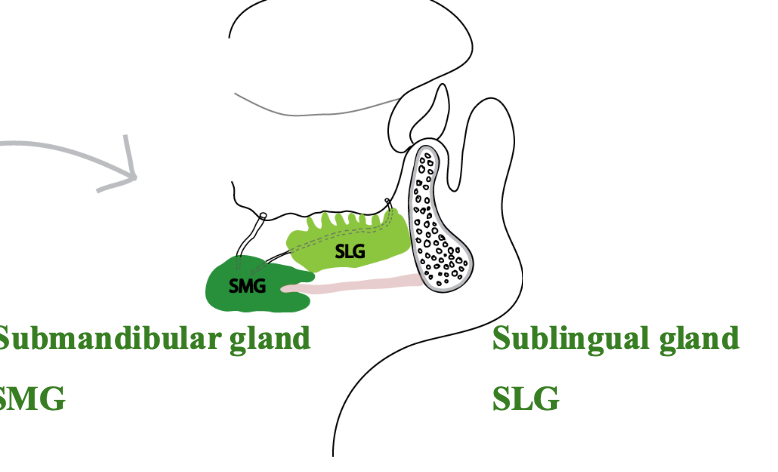
What do submandibular glands produce?
A mixed serous and mucous secretion, produce 65% of daily saliva volume (dsv)
What do sublingual glands produce?
Secrete a predominantly mucous saliva, = 5% of daily saliva volume
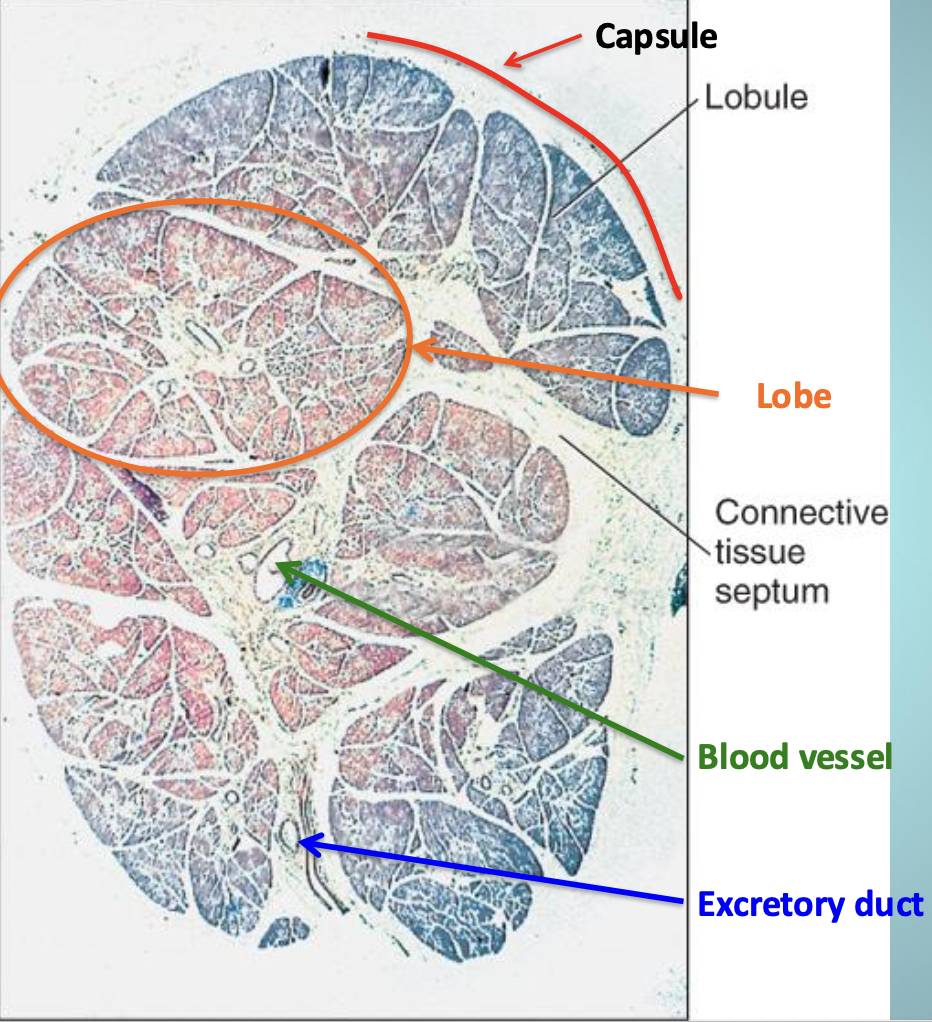
Describe the salivary gland structure
Has lots of lobules within each lobe
The connective tissue capsule is rich in collagen fibers and continuous with the connective tissue septa within the gland
Blood vessels, nerves, and excretory ducts run within the connective tissue septa
What components make up salivary glands?
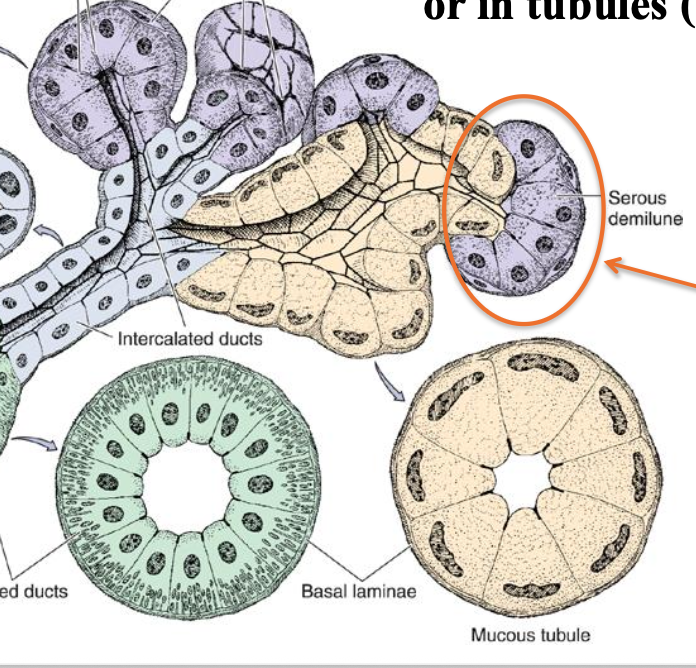
A capsule surrounding a branched duct system ending in acini or compound acinar gland (serous) or in tubules (mucous)
What are some artifacts of preparation in salivary glands?
Secretory end pieces called demilunes
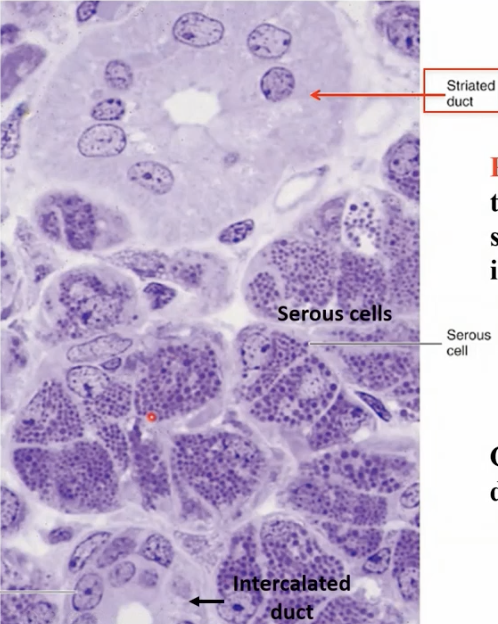
What are serous cells?
pyramidal in shape
broad base attached to basal lamina
narrow apical end towards lumen
polarized cells
protein secreting cells
round nuclei
What do serous cells secrete that begin to digest dietary starch into maltose?
Alpha-amylase
What is the function of alpha-amylase?
Digest dietary starch into maltose
Serous cells always stain
Dark purple
What do serous cells secrete?
A watery fluid with proteins, and are devoid of mucus cells

What are mucous cells?
Pyramidal in shape
Have flattened nuclei
Polarized cell (nuclei near basal end)

Mucous cells stain
Light pink
What do mucous cells produce?
A very mucus-rich secretion (mucin) stored in large, light-colored vesicles
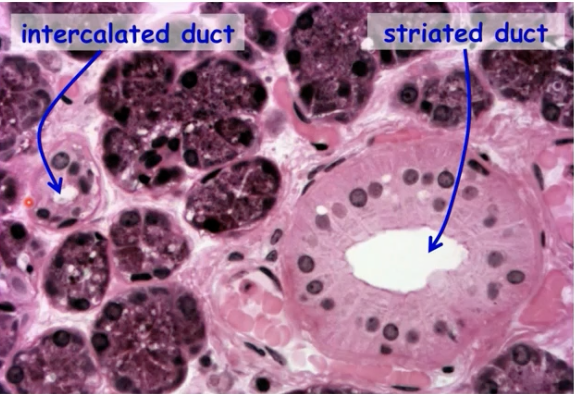
What are myoepithelial cells?
They are present between serous cells and their basal lamina in the serous acini as branched “basket cells”
They are part of the epithelium that has constructed the gland
What is the function of the myoepithelial cells?
Because of the star shape, they are going to squeeze the serous gland and contain a lot of actin and myosin
What is the origin of myoepithelial cells?
The intercalated ducts resemble smooth muscle cells, but they are ectodermal in origin
Where are myoepithelial cells located?
At the acini and intercalated ducts where they cover 25-50% of their surface area
What is the duct system
The secretory end pieces that empty into intercalated ducts
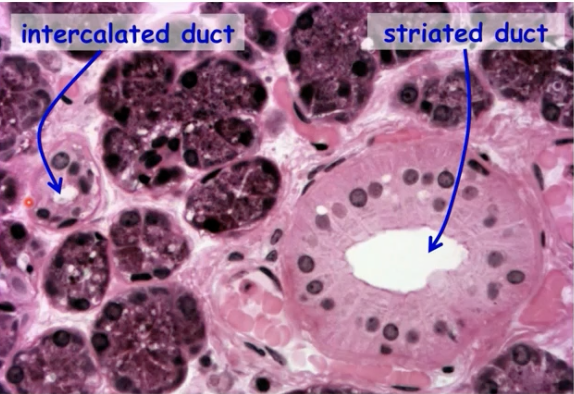
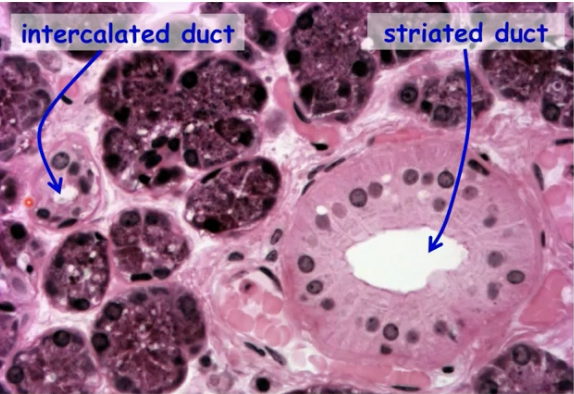
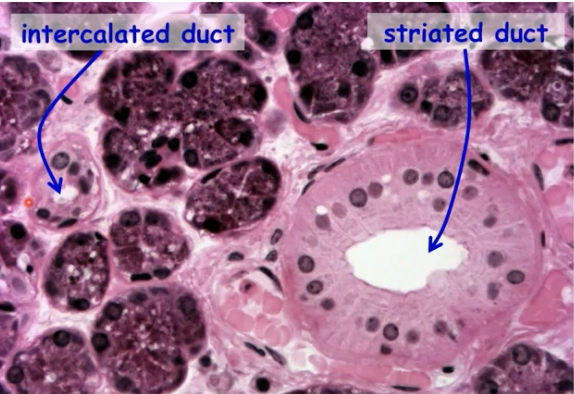
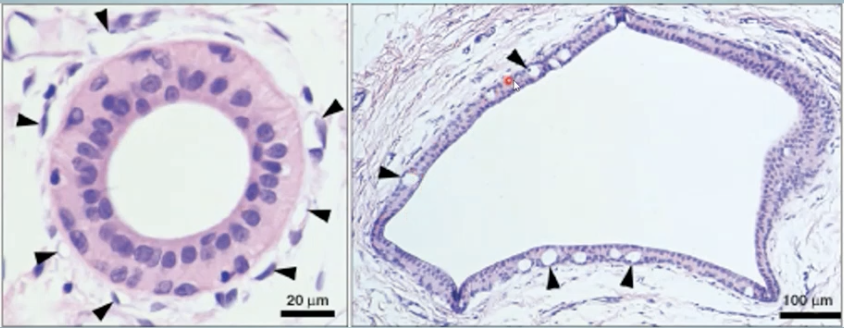
What are intercalated ducts?
It serves as a stem cell for both the secretory end piece cells and for the ductal cells
Both the secretory and ductal cells are considered
Intralobular ducts - intercalated and striated
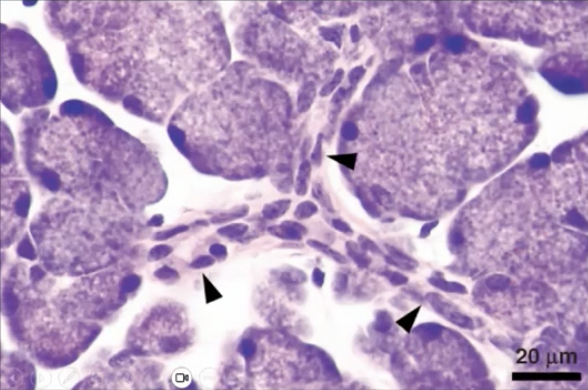
What are striated ducts?
They connect to several intercalated ducts and are “striated” due to the infoldings of the basal plasma membrane (for ion transport)
Excretory ducts are considered
Interlobular and have their own stem cells
What are characteristics of intercalated duct cells?
Nonpolar
Small diameter and drain individual secretory units
Synthesis and secretion of lysozyme and lactoferrin
Source of salivary gland stem cells
What are striated duct cells?
Mainly in Parotid and Submandibular glands
Polarized cells
Striated appearance in basal plasma membrane with many mitochondria
Role in the assembly and transcytosis of SIgA
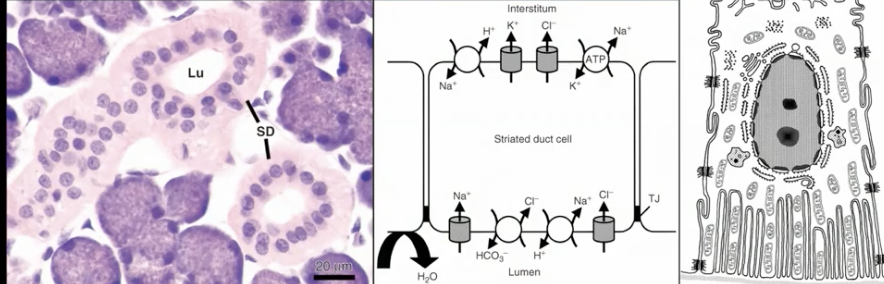
What are excretory ducts?
They are stratified and bilayered
Two layers of cuboidal cells
Generally are passive conducting tubes
Maybe pseudostratified to stratified
Contain both goblet cells and stem cells
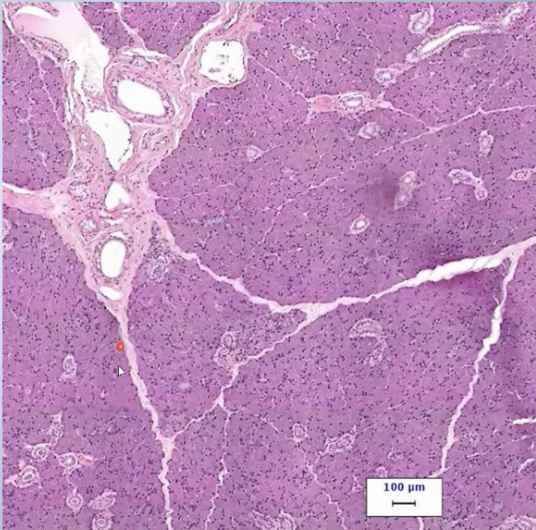
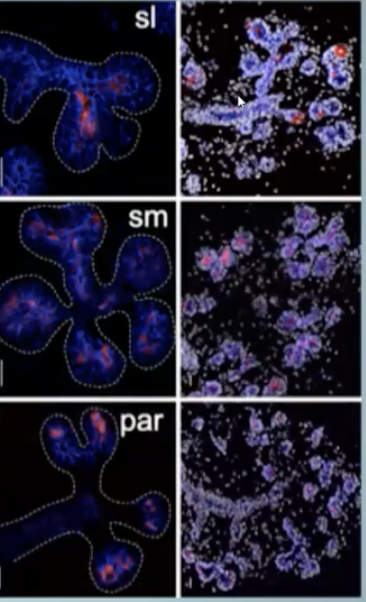
What is the Parotid Gland?
100% serous acini
A well developed duct system
highest amount of amylase of all salivary glands
Defensive chemicals
Stimulated saliva (produces little saliva during resting = not eating)
Parotid gland with the amylase producing serous cells storing enzyme in secretory granules
The granules also contain defensive proteins as well
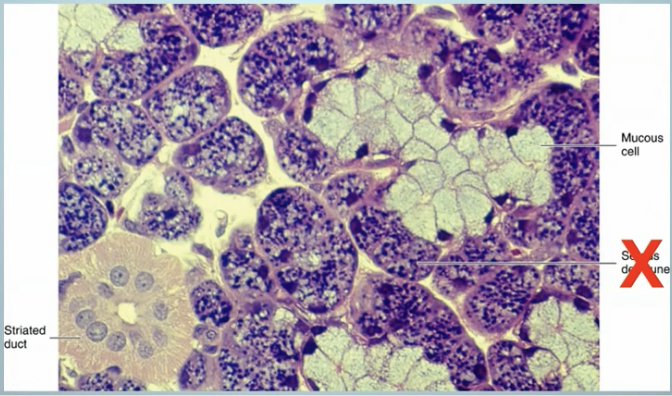
What are submandibular salivary gland?
Mixed gland with both serous and mucous cells
Branched tubuloacinar gland composed of serous and mucous cells
70% of the ducts end in serous acini, 30% mucous acini
Serous cells secrete lysozyme to kill bacteria
Saliva produced is mostly resting saliva
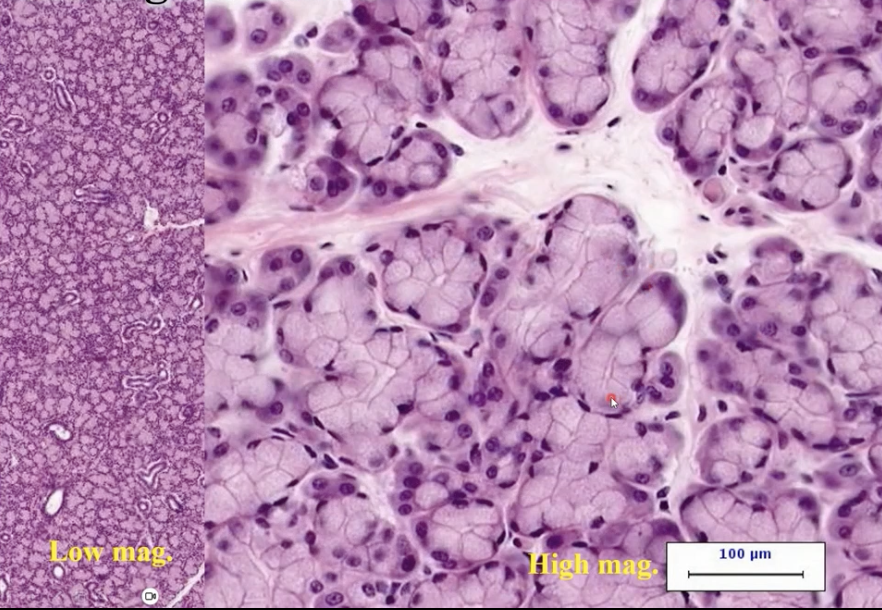
Sublingual salivary gland
Predominately a mucous salivary gland
50% mucous acini and 50% serous acini
Branched tubuloacinar glands
Resting saliva
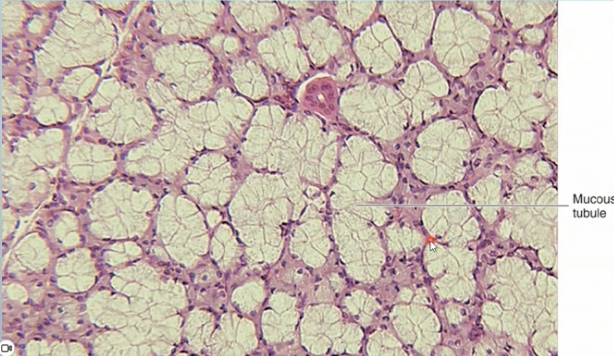
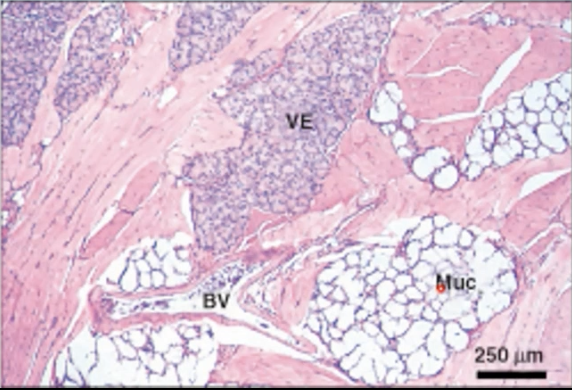
What is this, and what does it contain?
Sublingual gland containing lighter areas of mucous cells (large and take up most of the space), Some serous cells
Minor salivary glands
Mucous
Serous
Mixed
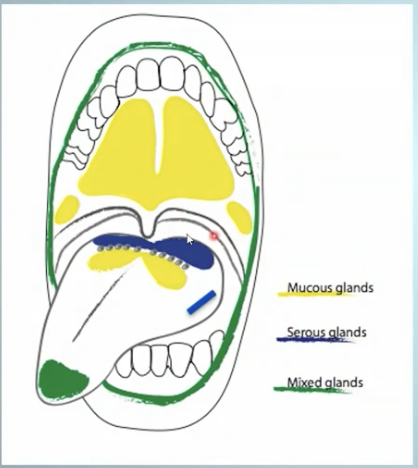
What are the minor mucous salivary glands?
Palatine glands
Posterior lingual glands
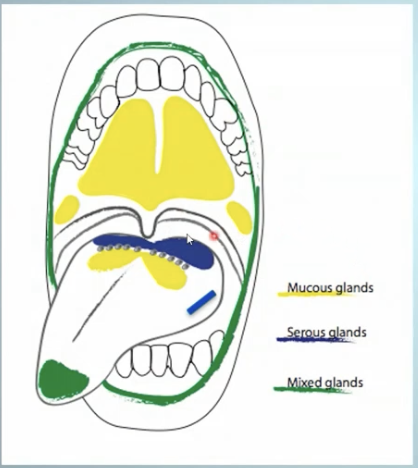
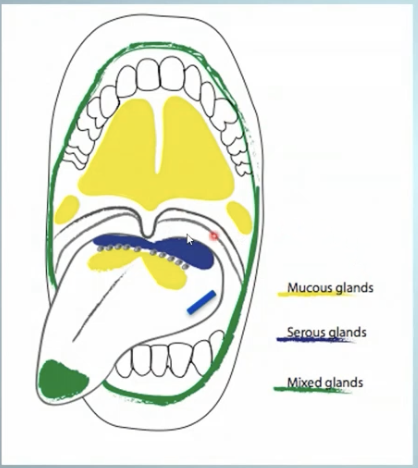
What are the minor serous salivary glands?
Glands of von Ebner

What are the minor mixed salivary glands?
Anterior lingual glands
Buccal glands
Labial glands
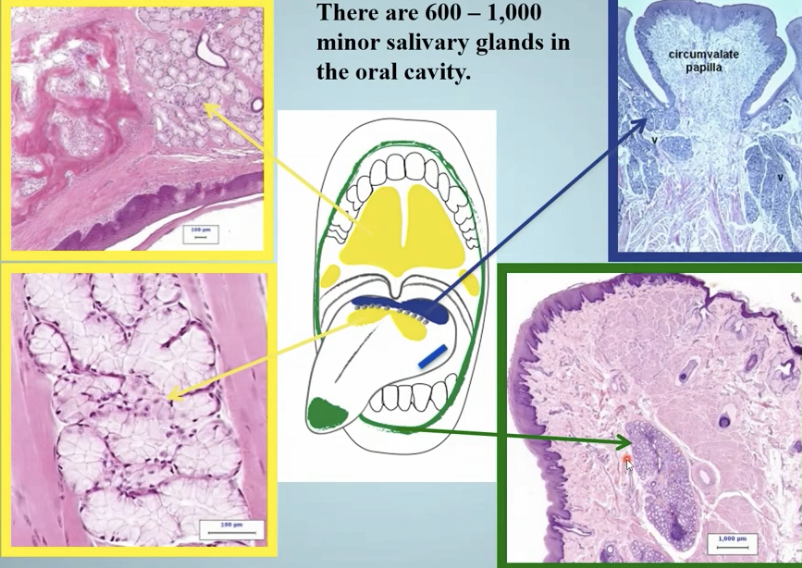
How many minor salivary glands do we have in the oral cavity?
600-1000
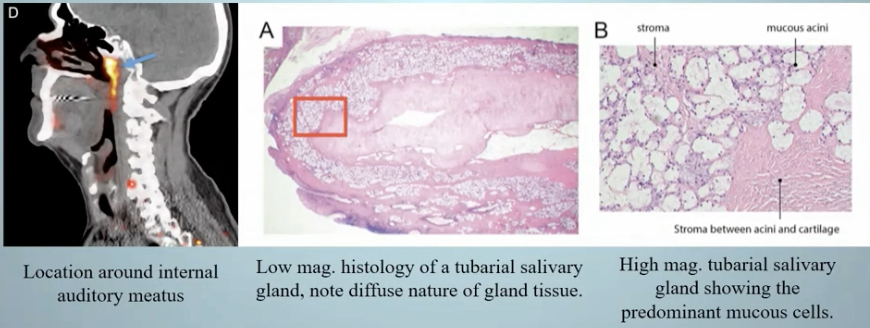
What is the new minor human salivary gland discovery made?
Two predominantly mucous glands with multiple draining ducts near the torus tubarius, superior the the eustachian tube
“tubarial glands”
What are tubarial salivary glands?
Primarily mucous glands with minor serous output
Location in the submucosa, diffuse nature of the glandular tissue and lack of capsule suggest a minor salivary gland designation
The gland is comparable to the mucous glands in the soft palate and assist in swallowing
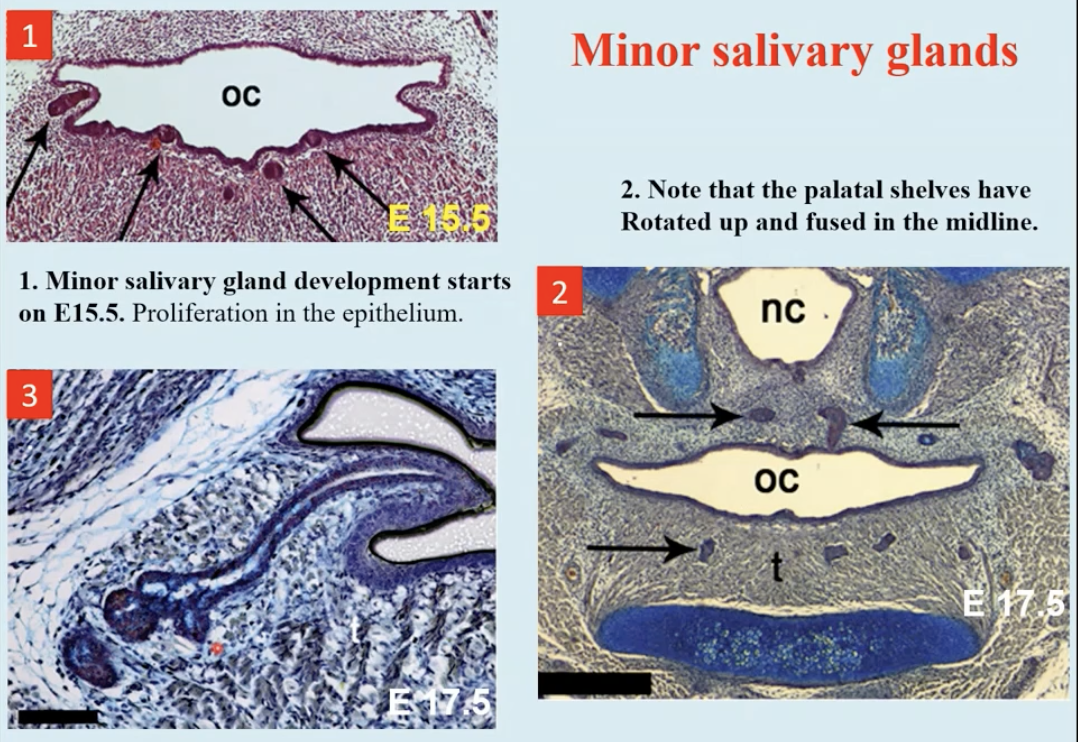
What do minor salivary glands look like?
Individual lobules that don’t grow any more extensive
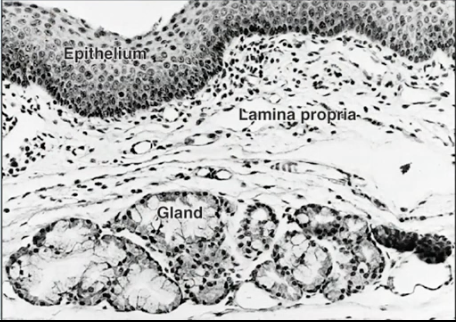
What is the role of the minor salivary glands in the submucosa?
Only 10% of the salivary secretion, but 70% of the mucous secretion
Important contributors to unstimulated or resting saliva
Have shorter excretory ducts
Have poorly developed intercalated and striated ducts
They are not surrounded by a connective tissue capsule
What are the Glands of von Ebner?
Serous glands on our tongue associated with papillae that have lots of taste buds with them
Posterolingual in the tongue
Secretions are released in areas with significant number of taste buds
Near the troughs and clefts of circumvallate and foliate papillae
What do von Ebner glands secrete?
Serous fluid with digestive enzymes and other proteins which assist in the perception of taste, they are associated with Weber’s glands (mucous glands)
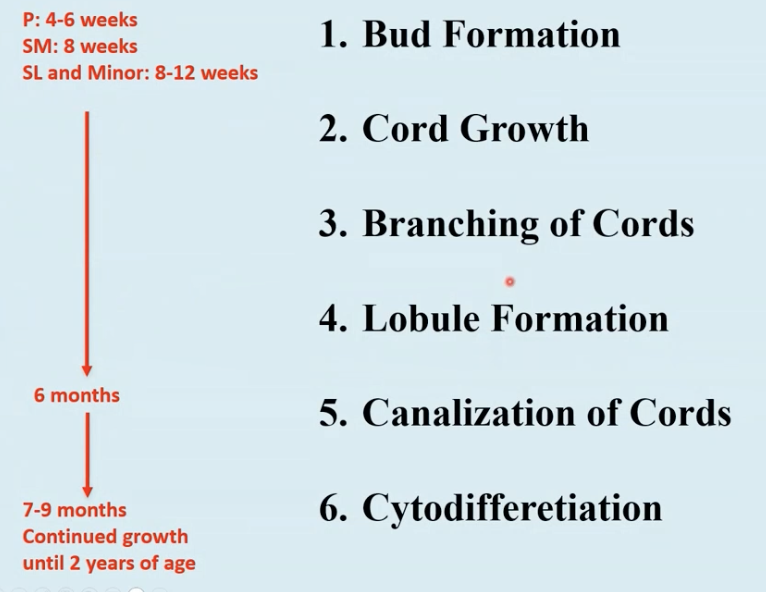
What does the development of a salivary gland compare to?
The development of a tooth bud in regards to beginning in a similar structure, and using the same signaling molecules
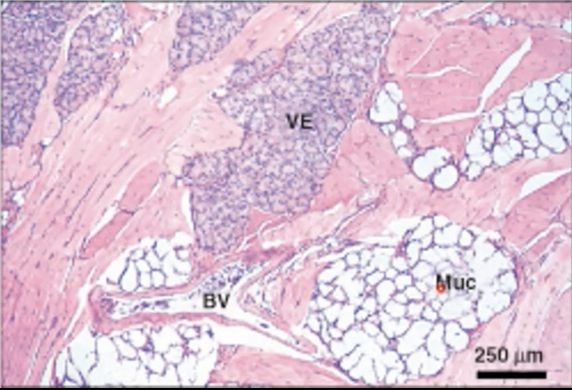
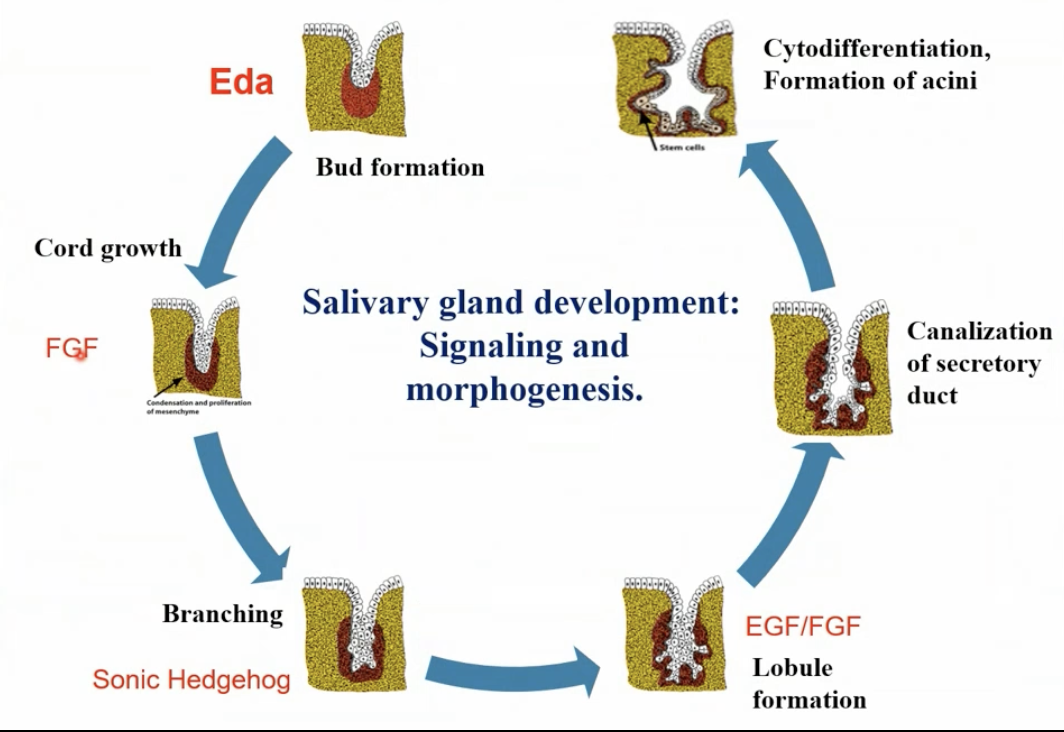
What are the developmental steps of salivary glands?
What are some differences between facial exocrine glands and exocrine glands located elsewhere in the body?
Ectomesenchyme reacts differently than mesenchyme
There is less reciprocal induction signals received from ectomesenchyme
Teeth and sweat glands are more affected by hypohidrotic ectodermal dysplasia
Higher degree of epithelial interactions in salivary glands
Very few mesenchyme locations will support development of salivary glands from oral ectoderm
What is hypohidrotic ectodermal dysplasia?
Abnormal development of structures including the skin, hair, nails, teeth, and sweat glands
62% of people have reduced salivation
What is the only other place that we can see mesoderm that can cause salivary glands?
Mesoderm associated with mesenchyme from urogenital ridge
Skin vs. oral ectoderm-derived organs
Reciprocal inductive signals originating from Oral Ectoderm and Neural Crest derived Ectomesenchyme
What dictates what kind of cell you’re going to be? (gland shape/product)
The structure/shape of a gland is dictated by the mesenchyme
The product is dictated by the epithelia (serous or mucous)
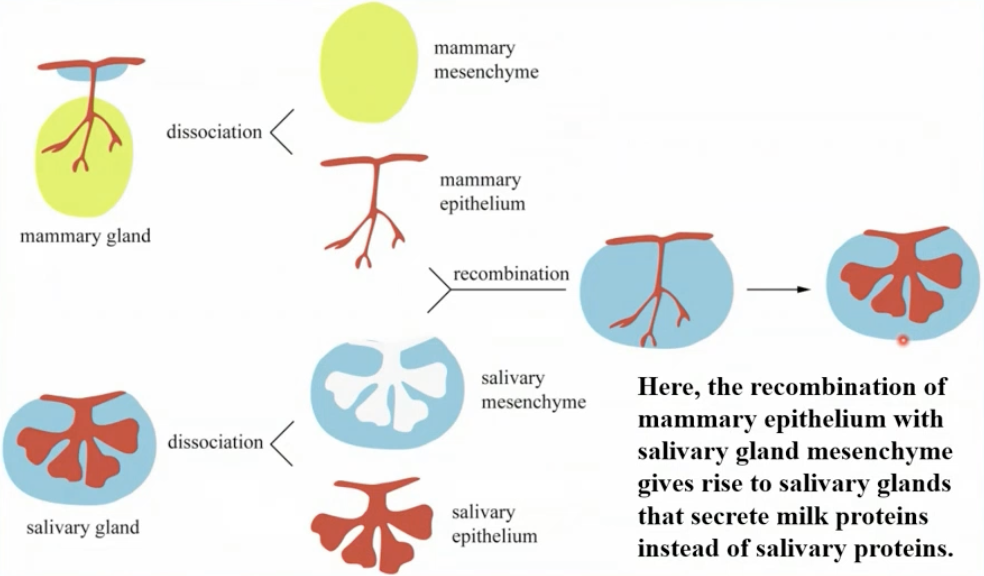
What designates the product of the gland (serous or mucous)?
The epithelia
What designates the shape of the gland?
Mesenchyme
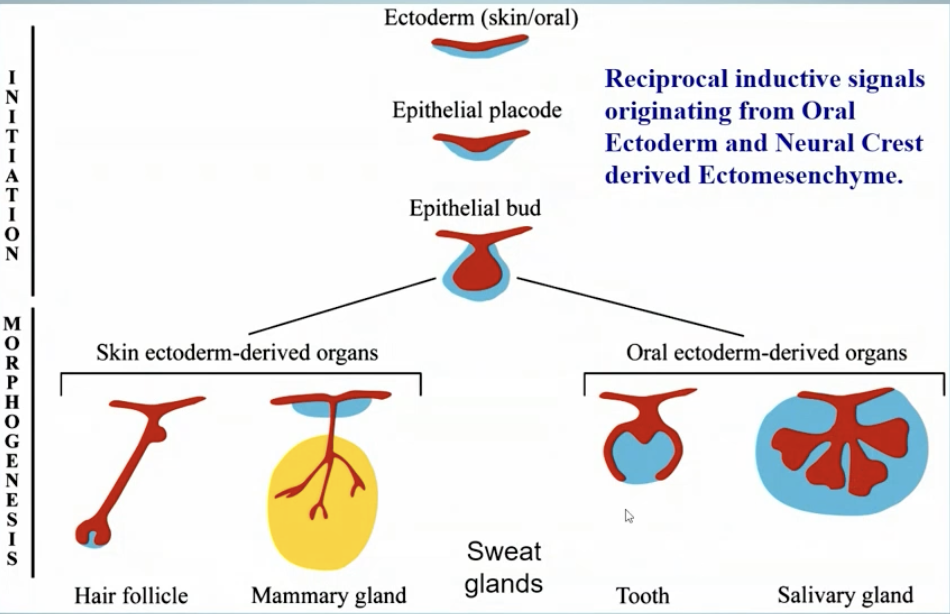
Salivary Gland Development
What is ectodysplasin A (EDA)?
A signaling molecule that is necessary to go from a placode to a beginning bud. It is necessary for our salivary glands and tooth buds. There is a receptor that the epithelial cells have to have
What mades EDA?
Underlying mesenchyme that works with the receptor on the epithelia to make a bud form
What is sonic hedgehog?
Epithelial cell proliferation, survival and differentiation, creating branching
What is elongation?
Fibroblast growth factor, secretion of collagen- cleft formation
What is epidermal growth factor?
Stimulates epithelial proliferation and differentiation

People with Hypohidrotic ectodermal dysplasia are (HED)
Deficient in producing EDA from the mesenchymal cells
The epithelial cells are deficient in making receptors
Often tend to lack production of fibroblast growth factor to cause the elongation of the bud
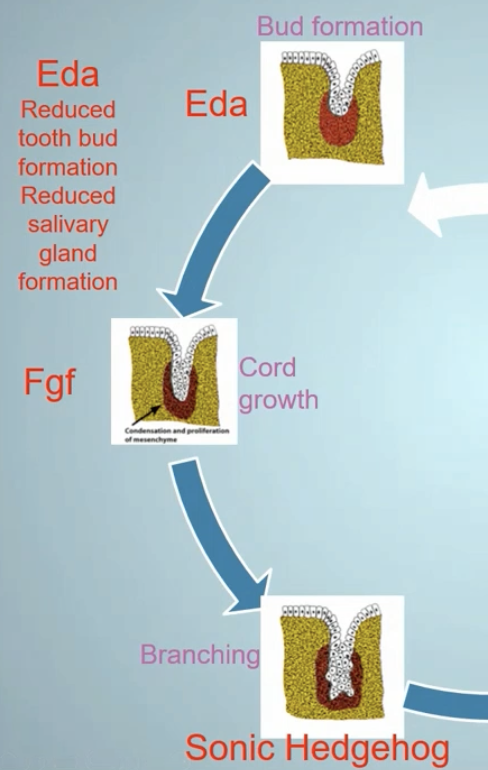
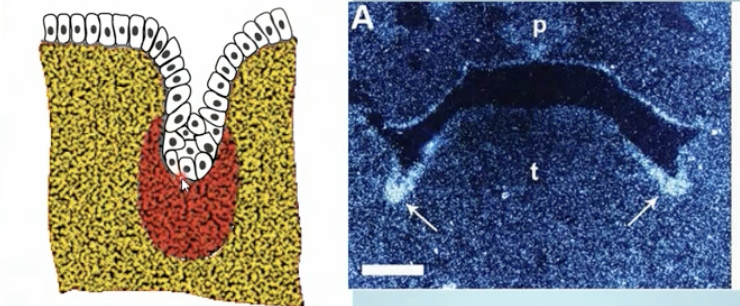
What happens during Bud Formation (1)?
Human development late 4th week
EDA is produced by the underlying mesenchymal
Receptors are on epithelial cells causing growth of placode down into a bud shape
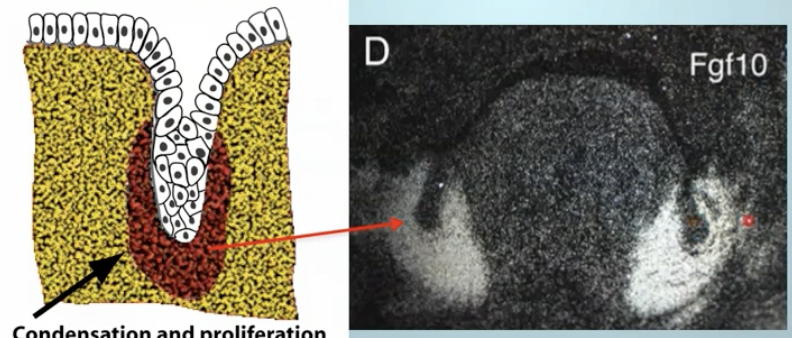
Fibroblast growth showing development of salivary glands
What happens during Cord Growth (2)?
Using fibroblast growth factors as a signaling molecule, there is a lot more condensation of ectomesenchyme
Early week 5
Bud growing into ECM because of FGF from ECM
Parotid, submandibular and sublingual gland growth
Extracellular matrix of ectomesenchyme (NCCs) growth
What is the origin of parotid glands?
Epithelial cells of ectodermal origin
What is the origin of submandibular and sublingual glands?
Epithelial cells of endodermal origin
Development of various portions of salivary glands

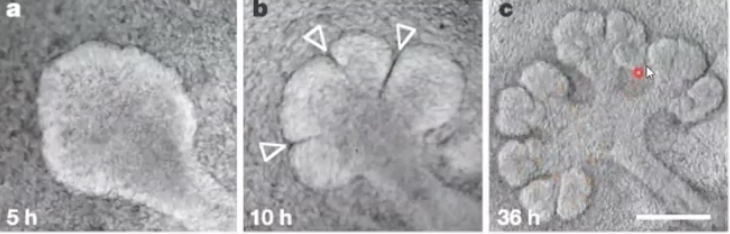
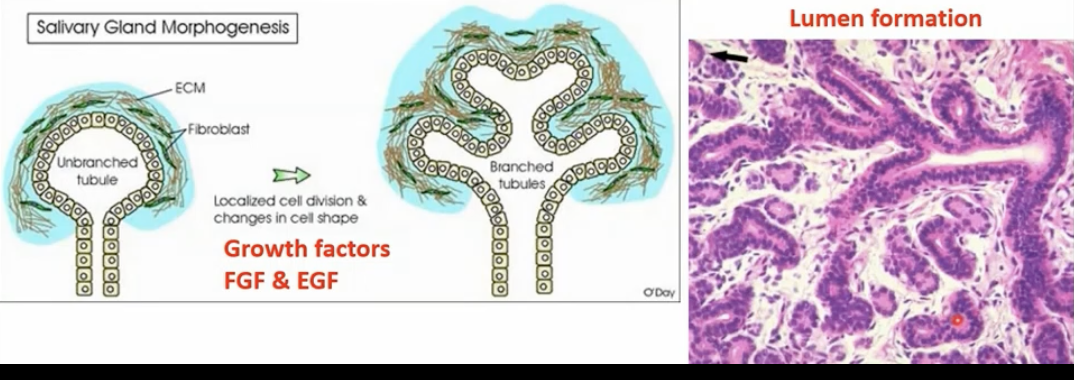
What happens during Branching of Cords (3)?
Clefts develop in the bud forming two+ buds
Growth factors like Shh and TGFb (transforming or tumor growth factor) from mesenchyme result in clefts from changes in epithelial cell shape
Fibronectin and Collagen III (reticular fibers) in the ECM are important to cleft formation, as is non-muscle myosin
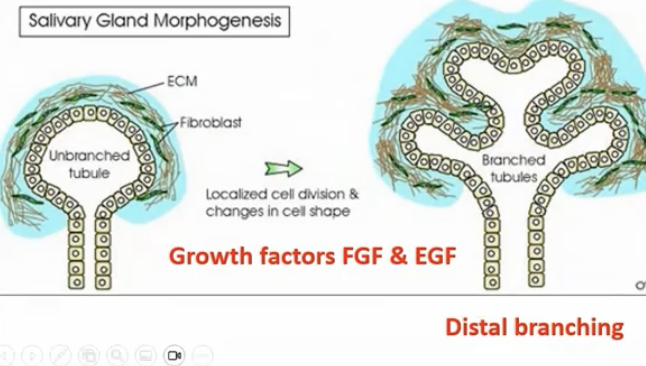
What is Lobule Formation (4)?
The result of repeated branching and budding along major branches of the cord stimulated by FGF and EGF (epidermal growth factor).
E-cadherin is important in acinar formation
What is this
In the cleft, there is a lot of expression for collagen III/I being on the outside.
There is an original bulb and there are clefts starting to develop along with branching
Fibronectin is important because it holds all of it together
What is important for branching and cleft formation?
Collagen III and Fibronectin
What is Collagen IV important for?
Basement membrane
Branching (acinar morphogenesis)
What are proteoglycans and GAGs important for?
Branching
What are Laminins important for?
Basement membrane assembly of
Lumen formation
FGFR signaling
Acinar formation
How can branching be inhibited?
If treated with collagenase so no clefts with form
Antibodies against collagen IV for the basement membrane will result in
No terminal end buds forming
What is the Canalization of Cords (5)?
Creating space (making them hollow) using water and apoptosis.
All ducts (lumens) form before the formation of secretory granules within the acinar cells
Lumens appear first at the distal end of main cord and in the branches, then at the proximal end and finally in the central portion of the main cord
Lamina form in the ducts before they form in the acini
Canalization of Cords
What is Cytodifferentiation (6)?
Signaling molecules come out to designate what are going to be serous, mucous, intercalated duct, striated duct, excretory cells, etc
Cells of the bulb region are the stem cells that undergo cell proliferation and differentiation Into acinar and ductal cells
Myoepithelial cells also arise from the stem cells of the terminal bulbs and develop in concert with acinar cells
What is the development of minor salivary glands?
They develop in the same way as the major salivary glands but they stop development early.
Formation of minor salivary glands (1-3)
What is saliva?
A complex oral biofluid
A mixture of components derived from multiple sources (different salivary glands)
What is the secretion of saliva?
Water
Proteins and glycoproteins
Electrolytes
What is saliva production stimulated by?
Unconditioned reflexes (things that stimulate saliva)
Conditioned reflexes (such as hearing, thinking about or looking at food, things that you associate with eating that then generate saliva)
What are the unconditioned reflexes?
Gustatory Stimulus- Taste
Taste receptors on tongue, soft palate, pharynx and epiglottis
Masticatory Stimulus- Chewing
Sensory receptors within the periodontal ligaments
Olfactory stimulus - smelling (lamina cribrosa)
What is the nerve input for unconditioned reflexes?
Taste buds (neuroepithelial cells)
Gustatory salivary reflex- neurons are located in lower brainstem
Lateral hypothalamus modulates this center
Mechanoreceptor fibers are sensitive when pinching the tongue
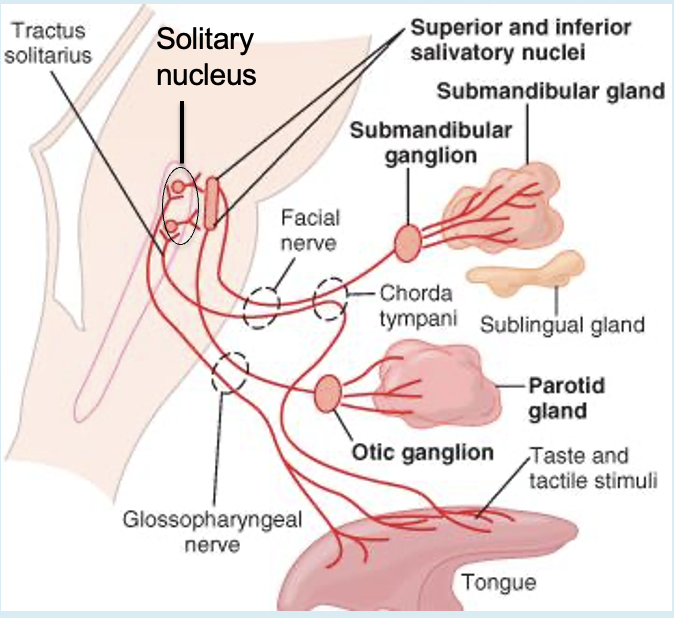
What are the afferent pathways?
Taste- facial (VII) and glossopharyngeal (IX) nerves
To solitary tract nucleus in the medulla
Plus input from higher centers of brain in response to smell
What are the efferent pathways?
Parasympathetic nerve
To sublingual and submandibular glands
From facial nerve (VII) via submandibular ganglion
Parotid gland from glossopharyngeal (IX) via otic ganglion
Sympathetic postganglionic nerve from cervical ganglion
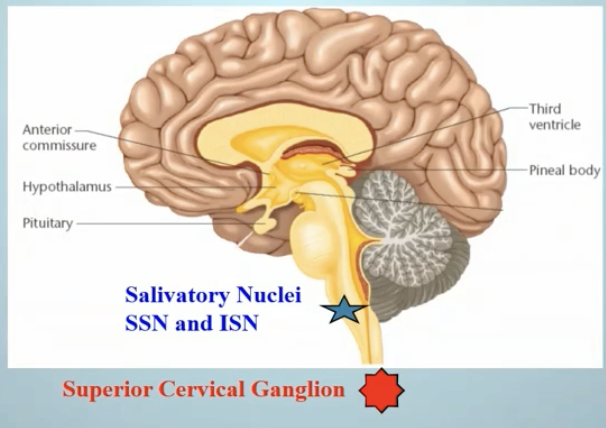
What is the separation between the superior and inferior salivatory nuclei?
There is none
What do preganglionic fibers innervate from the superior salivatory nucleus?
Submandibular salivary glands
Sublingual salivary glands
Efferent fibers travel with which nerve to the submandibular and sublingual salivary glands?
Chorda tympani nerve (facial nerve, VII)
What do preganglionic fibers innervate from the inferior salivatory nucleus?
Parotid glands (serous saliva production)
von Ebner’s glands
Efferent fibers travel with which nerve to the parotid and von Ebner’s glands?
Glossopharyngeal nerve (IX)
Fluid and electrolytes present in saliva are derived from blood plasma in
Ion and water channels
What surrounds acini and salivary ducts?
Capillary networks
What is needed in order to maintain a rapid and sustained secretion of saliva into oral cavity?
An extensive blood flow
What are the components of unstimulated saliva (resting)
Basal Production
Confers most protection
Importance of Minor Salivary and Submandibular Glands
Low output during sleeping hours
What are the components of stimulated saliva (resting)
Protection during mastication
Rich in digestive enzymes
Importance of Parotid Gland output
When do we need to use our reflex salivary flow?
For short periods in the day when we need to taste or chew
</= 10x increase in salivation
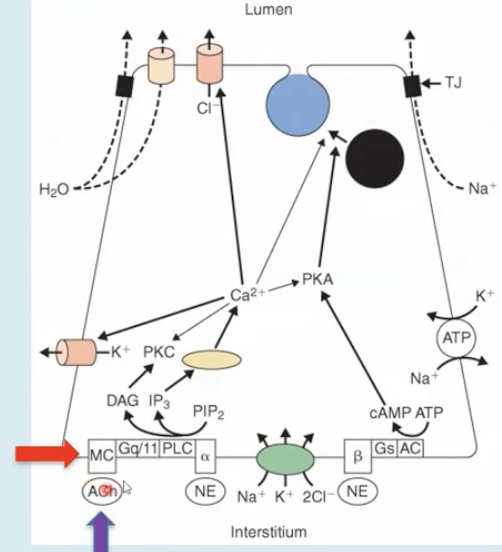
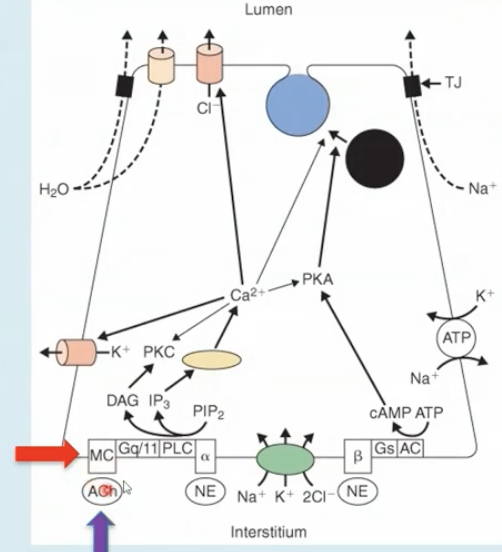
Autonomic nerves control what?
The secretion of salivary fluid and proteins
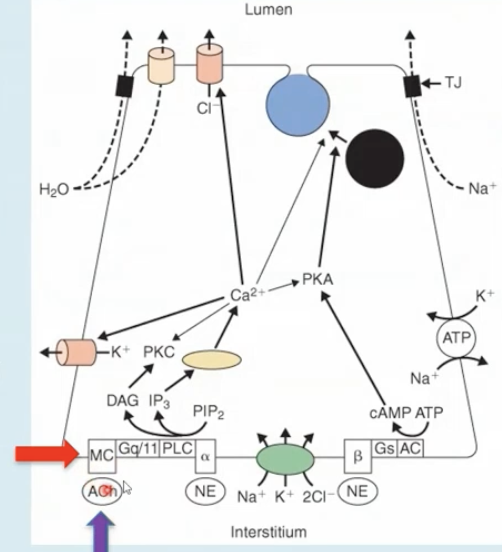
Cholinergic parasympathetic nerves release what to supply salivary glands?
Acetylcholine
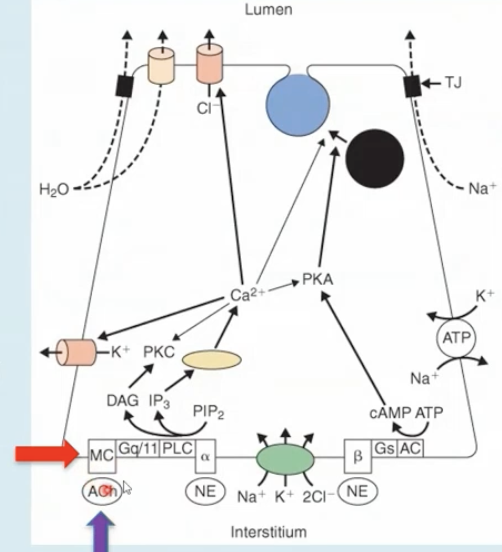
Acetylcholine binds to M3 and less to M1 muscarinic receptors to
Envoke saliva secretion