SPCH3212 - Mental Health and Justice MSE
1/81
Earn XP
Description and Tags
This flashcard deck is for the SPCH3212 - Mental Health and Justice mid semester exam.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
82 Terms
causes of mental illness
biological factors (e.g. genetics, hormones, development)
environmental factors (e.g. trauma)
cognitive patterns (e.g. ways of thinking, delusions, persistent negative thoughts)
the role of the speech pathologist in supporting mental health
gathering case history
observation
identify language difficulties
supporting client to understand high level language needed to undergo mental health treatments
emotional regulation - assisting the client to use words to describe emotions
identity development - using language to describe identity
• Identify language difficulties & contribute to formulation
• Adjust interventions to language needs
• Teach communication skills & strategies
• Support environments to adapt communication
• Build functional language & adaptive behaviours
• Develop emotional regulation via language
• Teach social thinking & conversational skills
• Strengthen narrative skills for self-expression
• Support participation in therapy through language-building activities
• Build self-advocacy & independence
categories of mental disorders according to ICD-11
anxiety disorders
depression/s
bipolar/s
psychotic
eating disorders
neurodevelopmental disorders
disruptive disorders
substance use disorders
common background factors for young people who offend
• Disabilities, mental health issues, DLD.
• Substance and alcohol abuse.
• Experiences of complex trauma (abuse, neglect).
• Attachment issues with parents/caregivers.
risk need responsivity framework
Helps assess the risk of reoffending and allows for prescription of intervention
Risk Factors:-
Child: disability, low IQ, poor social skills, trauma
Family: parental mental illness, violence, neglect-
School/Community: school failure, bullying, poverty
Protective Factors:-
Strong family attachments, good coping, school engagement-
Prosocial peers, community support
Underlies smart sentencing principle (targets the right intervention to the right person with the right intensity)
what the Age Crime Curve tells us about young people who offend
the evidence based theory that the majority of children who offend will ‘grow out of’ the need to offend and become law abiding with age
most offending takes place between 14-25
offending may be part of development for some people who then grow out of it
demographics of juvenile detention
60%-90% of young people who offend have communication difficulties
17% of young people in juvenile detention have an IQ >70
Aboriginal and Torres Strait Islander overrepresented (60% of juvenile detention population were First Nations, according to AIHA)
had experienced trauma
People with cognitive impairments and/or mental health disorders are 3–9 times more likely to be imprisoned than peers without disability (McCausland et al., 2013).
ADHD 5x more common in juvenile offenders
common factors in persistent youth offenders
• Persistent offenders: small group, high reoffending (responsible for the majority of youth crime)
• Common Factors:- Trauma, neurodevelopmental conditions, live with ongoing social disadvantage
• Aboriginal & Torres Strait Islander Youth:- 17x more likely in detention- Linked to child protection, housing instability, trauma
how incarceration increases the risk of young people offending
‘Peer contagion’ – learn how to offend more effectively from peers
Children arrested before the age of 14, are three times more likely to reoffend as adults
Children are not ‘little adults’
Locking children up does not decrease the risk of reoffending (no shit)
effective approaches to reducing youth offending
community based rehab
trauma-informed, culturally safe programs
early intervention
the problem with ‘adult crime, adult time’
not evidence-based
children do not have the same responsibility as adults because their brains are not fully developed
does not reduce youth offending/keep communities safe
increases chance of child reoffending (more arrests/interactions with legal system = more future offenses)
NOT ALIGNED WITH THE UN CONVENTION ON THE RIGHTS OF A CHILD (Australia way behind other first world countries)
unfairly and disproportionately targets disadvantaged communities (racism and intergenerational trauma concerns)
child less likely to be employed as an adult
child separated from family and community (traumatic for child, increases likelihood of reoffending)
theories of adult offending
Social Model of Crime
criminal behaviour does not happen in a vacuum and is informed by the person’s environment. once the person is identified as a criminal, they start to see themselves as outside society
Control Theory of Conformity
a person must have: healthy attachment to family, culture, and community, personal ambitions, have a good daily routine, and strong beliefs/values (not just about avoiding punishment, it is about having something to lose)
The good lives model of offender rehabilitation
the more areas of life the person is satisfied with, the less likely they are to offend
Integrated systems theory
holistic view of crime and decision making. offending probability is made up of a mosaic of factors, only some of which the person is in control of
connection between mental health and communication disorders
• Communication difficulties impact people across the lifespan
• 50–75% of children with speech/language difficulties develop emotional or behavioural problems
• 60–95% of children with social, emotional, or behavioural difficulties also have communication difficulties (often unidentified)
• Language disorders linked to mental health issues in adolescents & young adults
• Studies show:– Declining vocabulary → Higher risk of mood disorders & substance misuse– Speech/language delays at age 5 → Greater risk of anxiety & mental health issues into adulthood (Beitchman et al., 1996, 2001; Brownlie et al., 2016)– Poor vocabulary predicts treatment dropout in adolescents with depression
impact of communication intervention on reoffending
Offenders gaining oral language skills through communication interventions were 50% less likely to re-offend in the year after release
communication, mental, and neurodevelopmental statistics for adult offenders
Adults in prisons:
• 54% people literacy of an 11-year-old
• Majority low levels of literacy and numeracy
• Majority not completed high school
• Only 40% sufficient literacy and numeracy to independently participate in the workforce
People with cognitive impairments and/or mental health disorders are 3–9 times more likely to be imprisoned than peers without disability (McCausland et al., 2013).
pw neurodevelopmental disabilities over represented (especially when not adequately treated as a child)
ADHD rates up to 10 x higher than general population
role of a speech pathologist in justice
• Identifying and addressing speech, language, communication, and swallowing needs
• Supporting early intervention, diagnosis, and tailored treatment planning
• Modifying programs (e.g., behavioural, educational, vocational) to suit individuals with SLCN
• Ensuring accessible communication through simplified forms, documents, and processes
• Providing training and consultation for justice professionals and other service providers
types of trauma
• Primary Traumatisation: The direct impact of experiencing a traumatic event (e.g. losing a loved one).
• Secondary Traumatisiation/Traumatic Stress: Emotional distress from being close to someone who experienced trauma (e.g. family or support workers who witnessed the event).
• Vicarious Trauma: Deep emotional changes from hearing others’ trauma stories – your view of yourself, others, or the world may shift.
signs of vicarious trauma
• Difficulty managing your emotions: helplessness, guilt, anger, dread and horror, idealisation, personal vulnerability, avoidance reactions are common
• Difficulty accepting or feeling okay about yourself
• Difficulty making good decisions
• Problems managing the boundaries between yourself and others (e.g. taking on too much responsibility, trying to step in control other’s lives)
• Problems in relationships, social withdrawal
• Physical problems such as aches & pains, illnesses, accidents
• Difficulty feeling connected to what’s going on around and within you
• Changes in worldview (e.g. spirituality, identify, or beliefs about own needs)
risk factors for vicarious trauma
Individual
• Less experience
• Current personal stressors
• Unresolved trauma history
• Personality & coping style
• Inability to attend to self-care
• Unhelpful beliefs, ideas, values, expectations (about work and clients) —> think about the negative things you may have heard other healthcare workers say about clients/the work and how it makes you feel
• Social support (lack of) - feelings of isolation
• Spiritual resources (lack of)
Work Context
• Clients with ongoing traumatic experiences or in crisis
• Lack of resources and time
• Lack of control over work
• Uncertainty regarding roles
• Uncertainty about how to support client appropriately
• Lack of organisational support
• Lack of acknowledgement of the impact of trauma on volunteers / workers
• Overwork
why it is important to recognise compassion fatigue (CF) and vicarious trauma (VT) as an SLP
as a compassionate profession, the risk of CF/VT is high
if we don’t understand the risks and how to maintain resilience, we are likely to experience negative emotional outcomes
being aware of the risk factors, and signs in ourselves and others can assist in identifying CF/VT
knowing what you can do to prevent getting CF/VT out/how to recover keeps practitioners healthy long term (prevention/early intervention is more effective)
how to avoid compassion fatigue
•Remembering to ask myself how I need to look after myself with each client
• Being mindful of clients “hitching a ride” home with me at the end of the day.
• Paying attention to how I dress with clients (referring to dress as an expression of the effect the client/student is having on you).
• Being aware that I have a choice in how much my client’s feelings do or do not impact on me. Having more choices of how to be with a client.
• Maintaining a feeling for my edges (skin boundaries).
• Becoming better at judging when one needs to lower one’s arousal, and when it is better to stay with it yet contain it.
• A good session doesn’t mean that I must suffer along with my client.
• Becoming more efficient (through awareness and practice of these strategies) without losing empathy.
Seek professional supervision
how to manage vicarious trauma
Self
look for the signs of vicarious trauma/compassion fatigue
tune in to your own feelings (remember mirror neurons? recognise the physiological effect of the emotions/trauma of others and how it effects your body. consider doing regular body checks to assess the impacts of the interactions in your day.)
recognize that self-care is a necessity
do a transitional routine when you get home from work
maintain diet
regular exercise
use humor
mindfulness in daily activities
taking time to slow down
do things that are fun/pleasurable
spending time with people who uplift you
acknowledge/express feelings
therapy
Organization
• Arrange supervision/group debriefing
• Develop a balanced work/home life
• Defining and remaining aware of your goals
• Boundary keeping (time with “clients”, taking work home, self disclosure, realistic understanding of impact you have)
• Planning for difficult times
• Clarity regarding roles, tasks & • accountability
• Taking breaks and holidays
mental health first aid: aims and tools
Aims:
Preserve life where a person may be at risk of harm
Provide help to prevent the mental health problem from becoming more serious
Promote recovery of good mental health
Provide comfort to a person with a mental health problem.
Tools:
Approach, assess, and assist with any crisis
Listen non-judgmentally
Give support and information
Encourage appropriate professional help
Encourage other supports
definition of compassion fatigue (CF)
Feeling drained or affected from caring for and supporting others.
definition of burnout
A more severe state – when ongoing work stress harms your health or outlook on life.
compassion satisfaction: definition and signs
Definition:
The rewarding and fulfilling aspects of supporting others. The sense of meaning, purpose, and growth that many get when reflecting on the impact they’ve had. Allows a balanced view of vicarious trauma (there are positive and negative outcomes).
Signs:
deeper understanding of the world
renewed sense of meaning/purpose
renewed/changes in spirituality
greater value for relationships
greater degree of compassion
greater understanding of different cultures
description of ideal range of relationships
Towards survivor = ‘crusader approach’ → more emotional involvement but way higher risk of burnout
Away from survivor = ‘efficiency approach’ → less risk of burnout, but higher risk of negative emotional detachment from the person (e.g. victim blame).
Ideal range = professional detachment + boundaries + curiosity + empathy (for client and yourself!) + shared responsibility
mirror neurons: definition and how to un-mirror
Definition:
mirror neurons are brain cells that fire both when we act and when we observe others acting. they allow us to "feel with" others, forming the basis of empathy. constant mirroring (especially with traumatised people) can lead to feelings of distress and restlessness.
How to un-mirror:
sit up straight
cross or uncross legs
sip water
take a bathroom break
tense and relax muscles
move around
blink eyes
take a deep breath in/out
how to talk to someone about suicide
Anyone can safely talk about suicide — if you’re calm, empathetic, non-judgmental, and emotionally ready. have the conversation as soon as you believe the person is at risk.
Steps for safe conversations
o Be ready
o Look for signs
o Use clear language
o Listen without judgement
o Respect privacy but don’t promise secrecy
o Connect to further safety and support
duty of care/confidentiality for speech pathologists and healthcare workers
“ … a duty of care is breached when a client is injured because of an action (or inaction) of a speech pathologist, it was reasonably foreseeable that such action or inaction would result in a risk of injury to the client and the action (or inaction) causing the injury was unreasonable.” — SPA clinical guidelines for mental health
“All Queensland Health staff have a duty of care to disclose any relevant information about a consumer to avert a serious risk to the life, health or safety of the consumer or another person or to public safety.” — QLD Health guidelines for confidentiality in mental health (duty of care overrides confidentiality when a person’s safety is at risk)
supervision: what is it? how does it help? how do you seek it?
mentor: how are you going in your career and what are your goals?
supervisor: how are you going in your professional practice now?
helps you seek feedback
supports autonomy
provides support/allows reflection
assists you in navigating difficult/complex cases
helps support reflective practice and life-long learning
where to get supervision: you can find it through your workplace, SPA website, professional groups (FB, linked in). you can seek supervision in a specialist area.
support services available for families
13-FAMILY → a one stop shop for families that are struggling (e.g. parenting advice, connection to mental health services)
Aboriginal and Torres Strait Islander Family Wellbeing Services → Support Aboriginal and Torres Strait Islander families to improve social, emotional, physical, and spiritual wellbeing and help them safely care for their children.
Intensive Family Services → Support families with multiple and/or complex needs who are at risk of involvement in the child protection system.
who to contact if you have concerns for the safety of a child you’re working with
• Referral to Family and Child Connect
• Report to Child Safety- online form or phone call
• See Queensland Child Safety website
obligations of speech pathologists concerning child safety
not mandatory reporters
ethical obligation to report all suspected abuse/endangerment to Child Safety or 000 if danger is immediate
all QLD adults are obligated to report child sexual abuse
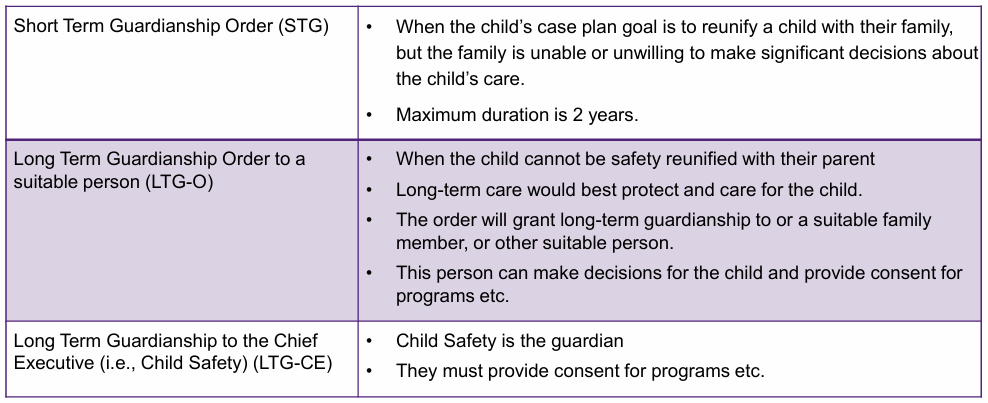
types of guardianship orders
note: children on LTG automatically have funding for childcare costs (e.g. education). children with complex needs on LTG get additional allowances (e.g. mental health care, OT)
different carer types in child safety
kinship carer → family member, friend, close community member, or cultural community member for indigenous children
foster carer → approved carer who is unrelated to the child
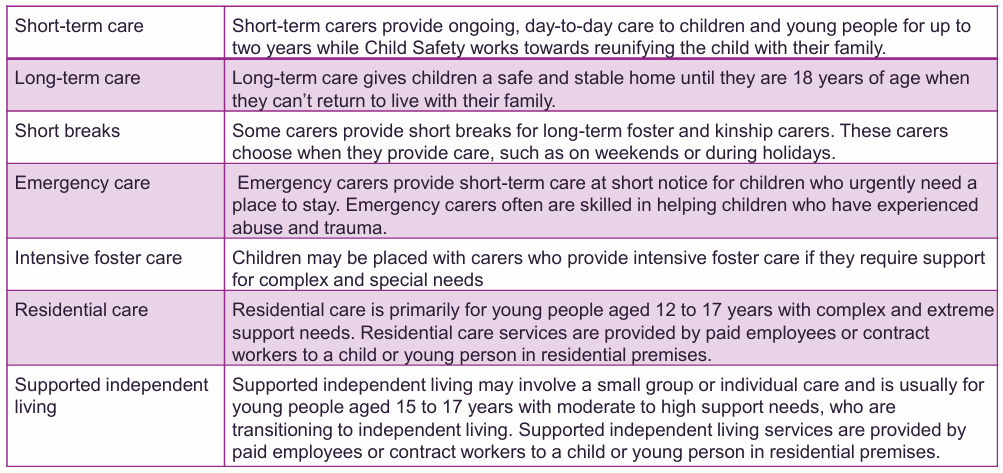
types of foster care for children
role of the SLP in working with children in care
Beginning of Care Arrangement:
• Ease transition by addressing communication barriers: helping the child adjust by supporting expressive communication
Ongoing Support:
• Provide regular communication support and advocacy.
• Monitor development and address emerging communication needs.
• Use age-appropriate tools to support participation in meetings and decision-making → ensure child’s views are heard and considered!
Cultural Responsiveness:
• Support cultural engagement for children with specific cultural needs (e.g., Aboriginal and Torres Strait Islander children).
• Use culturally appropriate communication methods.
role of SLP in transitioning out of foster care
make sure their voice is heard about anxieties/feelings leading up to transitioning out of care
prepare them for adult communication needs (e.g. getting a job)
support communication for tasks of daily living (e.g. following recipes, understanding a phone contract, etc.)
mental health services available for children in QLD
Head to health → free gov. support up to 12 years (developmental, behavioural, emotional challenges)
CYMHS → provides day programs, etc. can also refer to hospital >13 = child mental health unit <13 = adolescent unit
Evolve Therapeutic Services → for children in out of home care and is a joint program with youth justice and queensland health
Children’s Health Queensland (CHQ) → specialist eating disorder services → slps can manage ARFID + provide differential diagnosis (e.g. ASD)
CHQ → specialist gender affirming care → slps can assist with expressive and receptive language to engage with therapy, and gender affirming voice care. evidence-based care guided by World Professional Association for Transgender Health Standards of Care.
Headspace → mental health, alcohol and drug concerns. good source of mental health resources! supports holistic approach from all clinicians.
adult stakeholders for mental health in QLD
General:
Head to Health
1300 MH CALL (1300 642 255)
24/7 crisis helplines: Lifeline
Other supports: –GP–counsellors (13 11 14), 13YARN–Psychologists and psychiatrists–public mental health services (13 92 76).– NDIS.
For Aboriginal + Torres Strait Islanders:
TSICHS Social Health Team – culturally appropriate counselling in Brisbane
Aboriginal and Torres Strait Islander Mental Health program appropriate services. → funds culturally
Proppa Deadly' –addressing depression and anxiety through telling own stories.
Institute for Urban and Indigenous Health
stakeholders for adult drug and alcohol services
drug and alcohol diversion programs →
police drug diversion program
Illicit drugs court diversion program
drug and alcohol assessment and referral
Biala
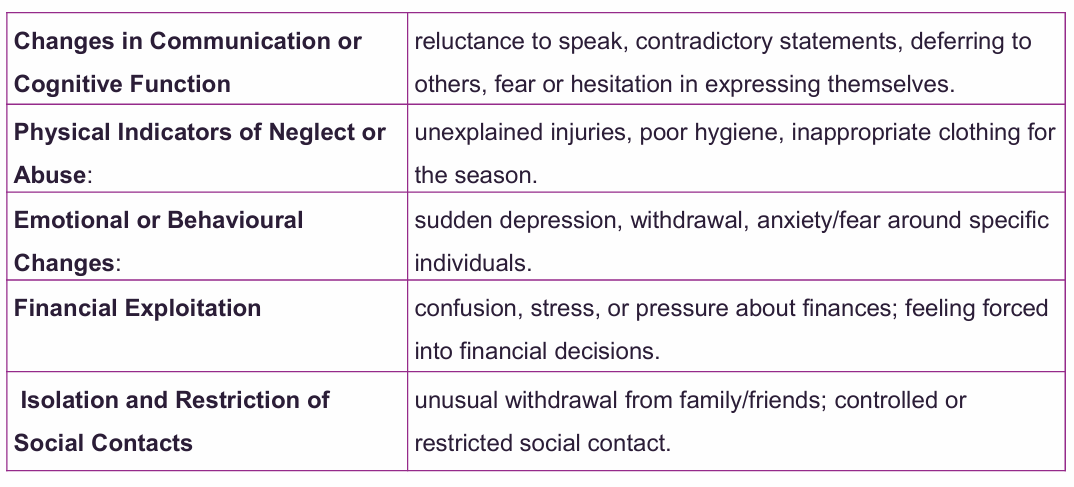
role of slp in elder abuse + signs of elder abuse
understand the signs
understand the nuances
create safe, supportive environment for clients
consider how mental health conditions predispose elders to abuse
document signs of elder abuse
speak to client on their own
ask open questions so the client can share their feelings without feeling pressured
how to keep yourself safe as a clinician in a complex/risky environment
risk awareness + training → understand how to identify, mitigate, de-escalate risky situations
follow personal safety protocols (e.g. know location of duress buttons, PPE, etc.)
understand and follow all communication and documentation protocols (e.g. incident and near miss reports)
consider the differences between settings and specific safety rules for each location (e.g. no skirts, dresses, unbelted pants, earrings, need to sign in/get clearance for specific area, etc.)
consider that you may need extra time to clear security/organize a prison escort
count resources upon exiting session (e.g. pens and pencils)
know location of doors/exits/alarms and know whether doors are locked/unlocked
relational security for slps working in adult prisons
• Confidentiality – Report safety risks (self-harm/harm to others) to prison management.
• Social Media Safety – Limit personal information; adjust privacy settings.
• Ongoing Training – Build knowledge of high-risk populations and related conditions.
• Safety Planning – Follow protocols to manage risk.
• Maintain Boundaries – Avoid sharing personal details.
• Support Access – Use Employee Assistance Services for counselling/debriefing.
• Person-First Language – e.g., “person who has offended” instead of “offender”.
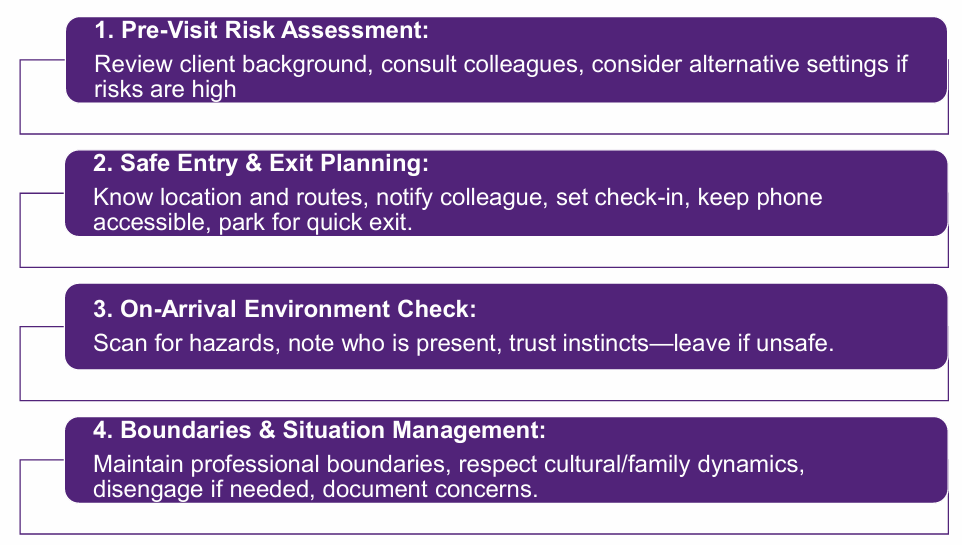
steps for mitigating risks during home visits
obligations for suicide/self-harm risk mitigation for slps
identify risk
conduct risk assessment
share results with team
understand the risk factors for self-harm (e.g. indigenous, immigrants, gender/sexually diverse people, history of child abuse, remote/isolated)
understand and follow the guidelines for your specific workplace
support communication to create a safety plan with the client alongside relevant stakeholders (make sure the client can understand and follow the safety plan)
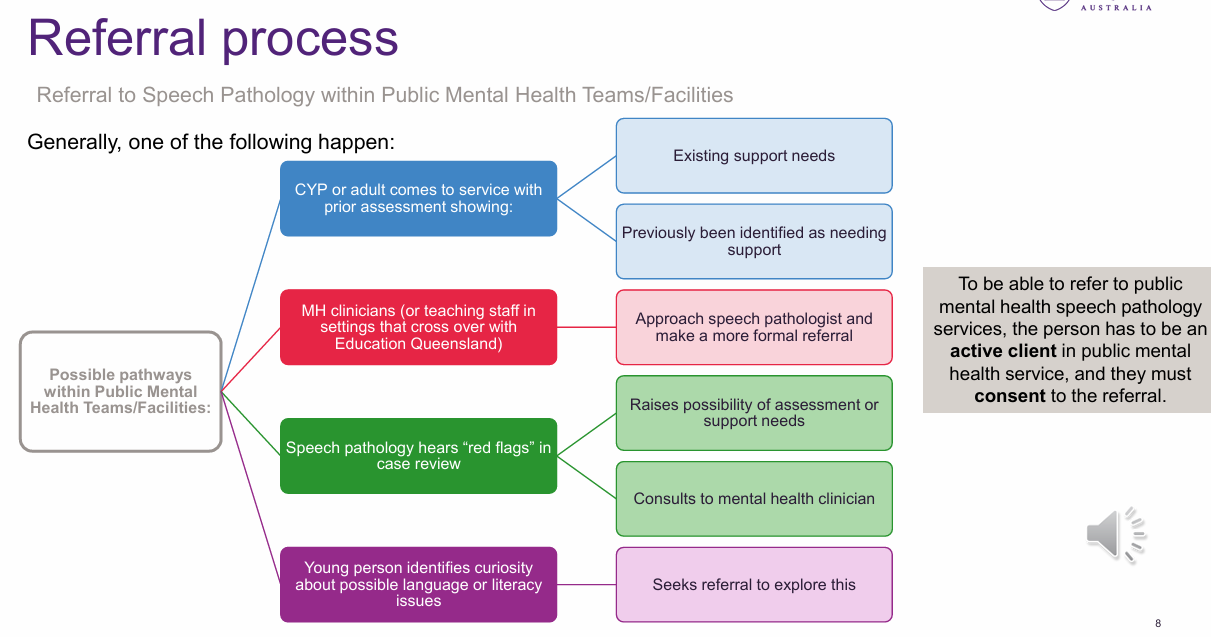
the referral process for the speech pathologist in mental health settings
REFERRAL: often have a lot (or too much) information, but level of information in referral varies.
Public mental health service: primary → GP, private practice, secondary → CYMHS (for more complex cases, requires GP referral) tertiary → specialist clinic, day clinic, inpatient unit, gender clinic, etc.(referral can only be made internally)
consent:
if under 12 → caretaker consent needed, 12-17 ‘mature minor’ + caretaker, adult (with capacity)
substitute decision maker if person doesn’t have capacity (e.g. drug addiction, psychosis, eating disorders, the mental health act has been evoked when the person’s ability to understand their situation and make decisions is impaired and their safety is at risk)
confidentiality:
can involve parents in sessions with minors, but high level of confidentiality is expected
the referral process for the speech pathologist in justice settings
referral:
youth: all youth justice clients have a caseworker → the caseworker will have a conversation with the young person and explain what a speech pathologist does and ascertain whether the young person would like to see you
adult: person identifies issues or caseworker/psych/etc. referrals based on goals to re-engage in community
consent:
youth: from young person and legal guardian (or witnessed by youth justice worker). child 14 + can be deemed legally able to consent on their own
adult: can provide consent + assumed capacity
how to do a comprehensive case history in mental health and justice settings
case history:
youth: personal history, family history, substance use, mental health, previous intervention, developmental milestones, hearing, vision, medications, cultural background, diagnoses, history with youth justice, etc.
observation very important, think about observing the person’s ability to hear and understand what you say. observe possible mental health, communication, and neurodivergent signs.
note: you may have to get in contact with previous case workers in child safety, CYMHS, etc. Think about who/what services your client has previously been in touch with
risk assessment in justice and mental health settings
Justice
youth: youth level of service (YLS) or case management inventory (CMI)
Mental health
risk factors, risk assessment, risk formulation, risk management → can be risk to self or others
consultant psych overseas the process with the mental health team
can do MSE
challenges for case history gathering and engagement in mental health services
how to do a comprehensive case history in mental health settings
case history:
timeline of difficulties, family history, developmental history, mental health and contextual factors, educational history
(dig into developmental/educational and the how it interacts with mental health, pick out relevant information).
lots of case notes to go through so make sure you give yourself enough time to do it.
holistic observation, parent/teacher report, self-report, etc.
remember to use as many sources of infor
considerations for consent in justice and mental health
person doesn’t have much choice/agency when participating in the justice/mental health system
person may have attachment difficulties/trauma/ACEs
person may assume their consent doesn’t matter
person may struggle to trust clinician/rapport building is hard
lack of trust in ‘system’
cultural trauma
understanding explanations of what consent is/what the person is consenting to
understanding explanations of mandatory reporting/confidentiality
the 5 P’s framework
The 5 P’s:
• Presenting – current issues: factors affecting the here and
• Predisposing – Long-term vulnerabilities that increase risk.
• Precipitating – Recent events or triggers.
• Perpetuating – Ongoing factors that maintain the problem.
• Protective – Strengths, supports, and resources.
purpose of speech pathology assessment in the mental health environment
child and youth
understand developmental level
understand functional impacts of strengths and weaknesses (can the child self-advocate?)
gauge ability to talk about thoughts and feelings (metacognitive and emotional regulation)
determine social communicative competence (use? start conversations? non-verbal cues? adapted to different social situations?)
academic performance
differential diagnosis (to develop comprehensive intervention plan)
impact of mental health on communication and mealtimes/eating experiences
assess impact of communication on emotional wellbeing
adult
understand cognitive and communication function in the context of mental health
understand functional impacts of strengths and weaknesses
understand the impact of mental health condition on successful communication and mealtimes
understand ability to express emotions and use emotional regulation
social communication competence (humor? sarcasm? figurative language?)
assess impact of communication difficulties on self-esteem and wellbeing
identify impact of mental health on communication patterns and processing
support differential diagnosis + creating tailored intervention plans
SLP involvement in assessing children and young people in the mental health setting
consent
risk assessments
safety planning
goal setting
intervention planning
discharge planning
help the person understand the connection between their mental health condition and their communication difficulties
identify therapy targets
adjust mental health assessments to meet communication needs
what is assessed in the child/youth mental health context?
(language is main area of assessment)
pragmatics (social language? masking? narratives? social skills? non-verbal skills?)
cognitive linguistic features (categorising, analysing, critical thinking, etc.)
core language skills (comprehension at the word, sentence, discourse level)
functional language skills (how are they using language? ask for things? interact?)
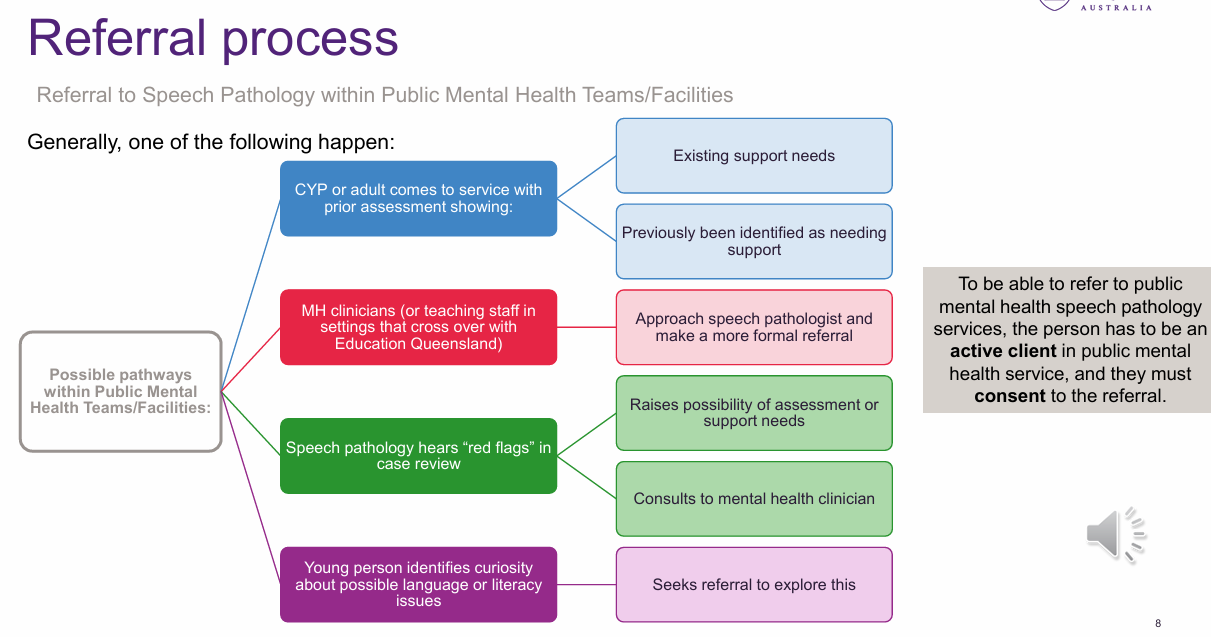
how the SLP can support the consumer during the assessment process
the therapeutic alliance is the fundamental building block of providing assessment in the mental health system!
considerations for assessment selection in mental health
age of client
what measures are appropriate and available
standardized and non-standardized tools
what info has already been gathered?
what assessments has the person already done?
what strengths and weaknesses have already been identified?
what difficulties have already been reported (e.g. situational mutism, you might need receptive only assessments)
what do you know about the person’s higher-level communication and pragmatics?
who is in the MDT?
what can mental health clinicians tell you about the client?
what does assessment of children and youth look like in the mental health setting?
highly variable
may need to meet the person where they are at if they’re hard to reach
may use F2F or iPads
reinforcement activities effective (food? go to park? game?)
rapport extremely important
start with ‘being with’
assessment may take longer than expected
may need to negotiate shorter but more frequent sessions (e.g. the person has ADHD)
you’ll have to take an even more flexible approach (if the person can’t do the assessment but they want to talk about their feelings, then do that)
consideration of emotions and triggers
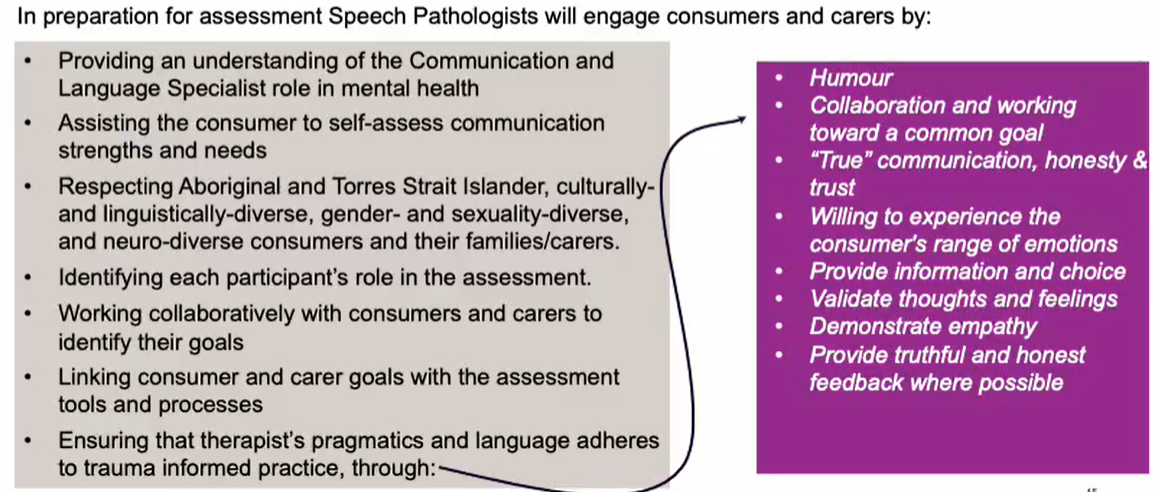
assessment approaches in mental health
informal → observation, informal assessment (self-assessment to identify strengths and weaknesses, caregiver survey, structured activities to assess specific targets).
dynamic → responsive assessments that measure the person’s ability to adapt and learn (test, teach, retest approach)
formal → (see image)
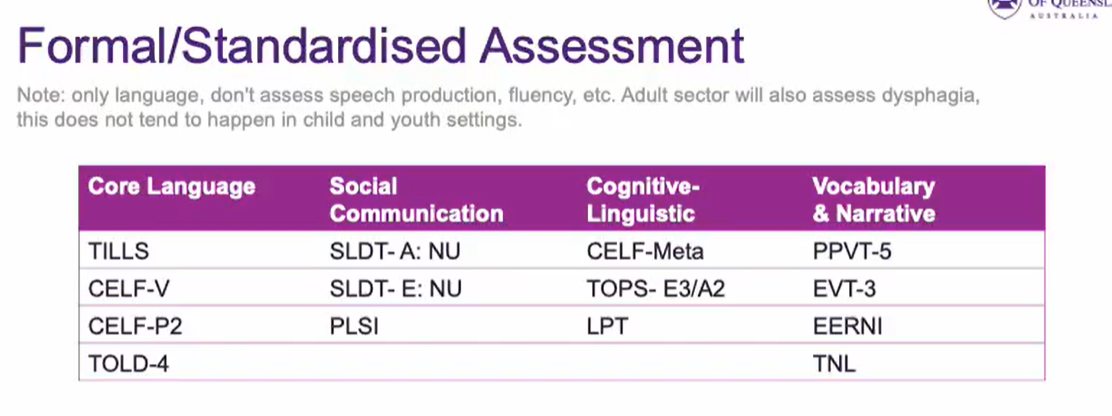
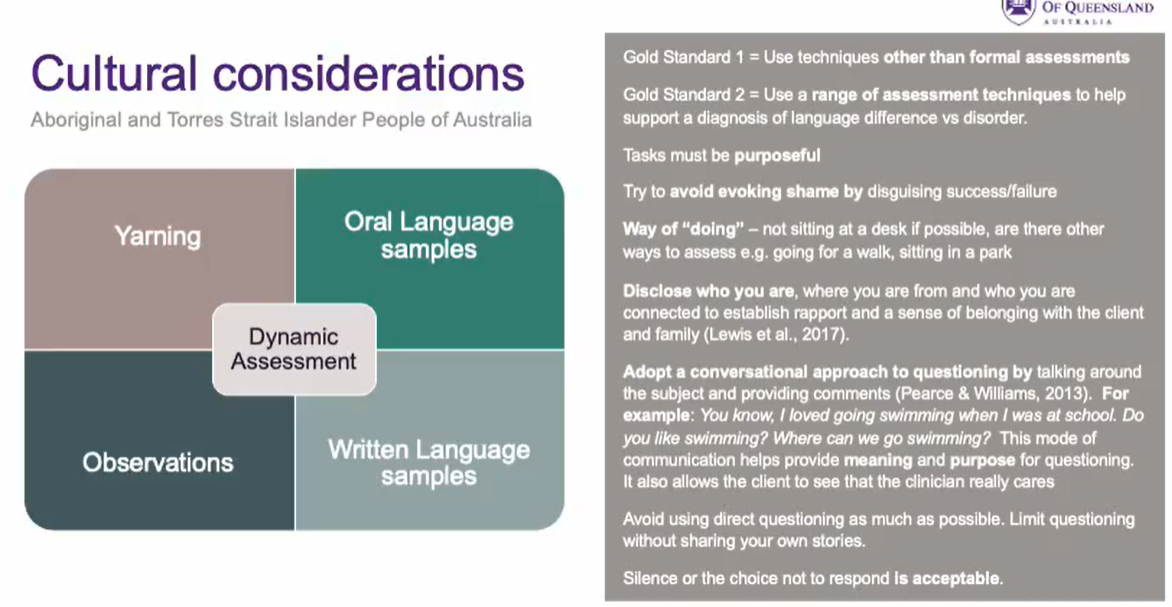
considerations for assessment of Indigenous children in the mental health setting
Gold standard 1 = don’t use standardized assessments!!!
Gold standard 2 = use a range of techniques that differentiate between language difference and language disorder
Dynamic assessment → observation, yarning, oral language sample, written language sample
ways of doing → see image!!
considerations for assessing adults in the mental health context
linguistic performance vs confidence (is this what they’re usually like or just how they are performing on the day?)
fluctuations in mental state (e.g. psychosis)
symptoms and cognitive deficits (memory? auditory hallucinations?)
compliance (do they want to engage?)
medication effects (can impact speech, memory, etc.)
institutionalization (how comfortable is the person in a new situation? how long have they been part of the mental health system?)
tools for assessing adults in the mental health context
Formal assessments
Thought, Language, and Communication Scale (TLC) - tangential, circumstantial, derailment in speech
Communication Awareness Scale - how aware is the person of strengths/weaknesses? does the person know how often conversations break down? does the person try to repair?
Broadmoor - cognitive and language functioning and their impact on communication abilities and behaviour
can use standardized assessments but may [e.g. BDAE, WAB, TROG, BNT] but these may not be as effective with the population
Informal
discourse assessments (picture description, narratives, procedural, cohesion analysis, communication breakdown/repair)
language samples
observation
Differential diagnosis
work with MDT
liase with key stakeholders
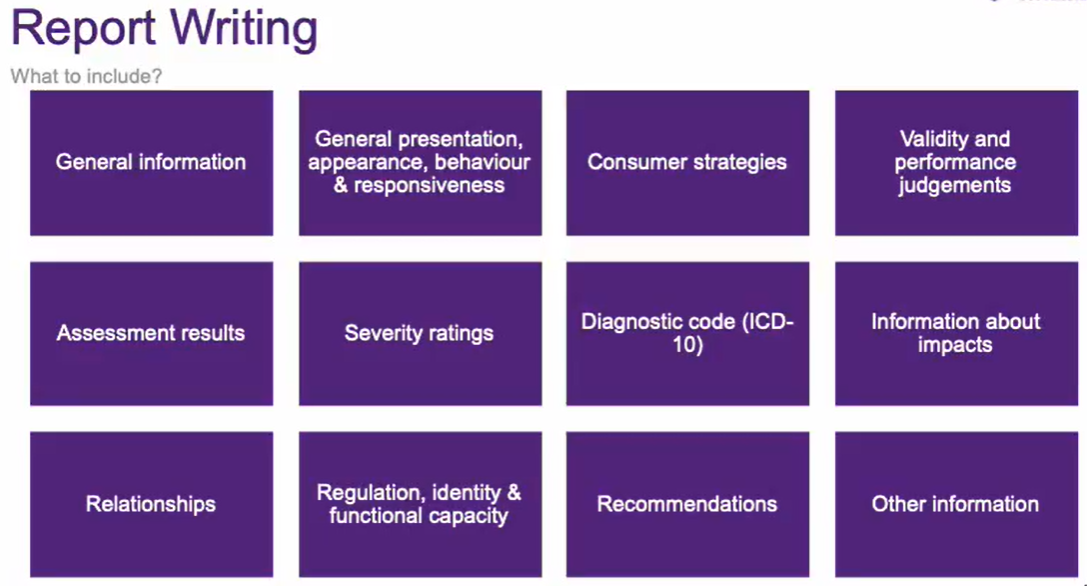
what to include in your report writing in the mental health setting?
provide person-appropriate results to the consumer (e.g. provide a visual for a child, etc.)
differences to other report writing include gender identity, mental health diagnosis, and medications
as always, consider the reader’s health literacy and reading skills (use accessible language, etc.)
consider consent about who is allowed to view the report
consider easy read language, highlighting information, include a visual, highlight priorities, consider colour-blindness
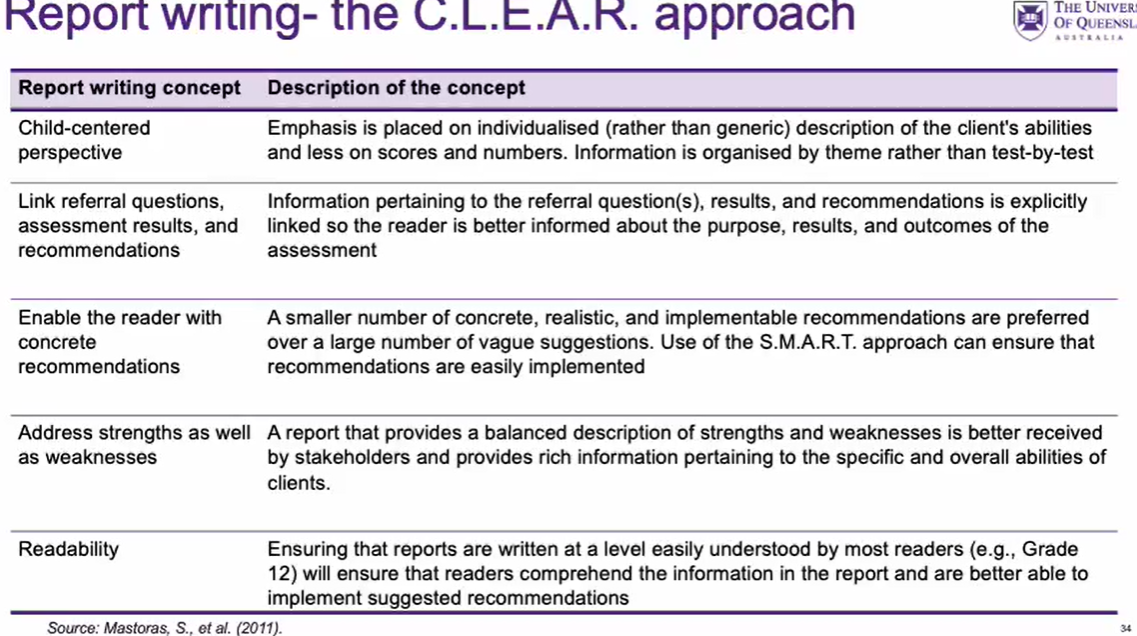
the CLEAR report writing approach for children in the mental health setting
(see image) provides a client-centred approach to report writing the centres the child and is easy to understand by most readers!
considerations for providing mental health results to the client
do it in person
use language the person can understand
select more relevant information
use visual
use keywords
link to referral concerns
link to key examples of behaviour to enhance understanding
key features of the therapeutic alliance
1. Setting goals together
2. Agreeing on tasks used in therapy
3. Affective bond between clinician & client
impacts of therapeutic alliance:
1. Increased trust & comfort
2. Increased client self-awareness & motivation
3. Better understanding of your client
4. Collaborative approach to treatment
5. Increased client satisfaction
6. Reduced drop-out rates
7. Improved treatment outcomes
stages of the therapeutic alliance
rapport building
development of a therapeutic alliance
maintenance of a therapeutic alliance
closure
why and how to repair a therapeutic alliance
Purpose – restore connection and reengage after a negative interaction (Cook et al., 2018).
Clinician initiates repair, but always on the client’s terms.
Models vulnerability – acknowledging fault shows clients how to repair relationships in future.
Strategies for repair:
Offer a genuine apology
Articulate awareness and self-reflection of missteps.
Collaboratively develop strategies to prevent recurrence.
Without repair – risk of fractured relationship, broken trust, client disengagement (Beaulieu, 2016; Mitchell et al., 2016).
challenges of forming a therapeutic alliance with a child in mental health and justice
person factors:
trauma
distrust of adults
physical and mental state of child
disability
developmental age
chronological age
cultural factors
environment
purpose for communication
giving consent safely
communication difficulties
understanding speech pathology
systemic factors:
working within the foster/kinship system
child may have multiple agencies working together to help them
strategies for forming a therapeutic alliance with children in the mental health and justice system
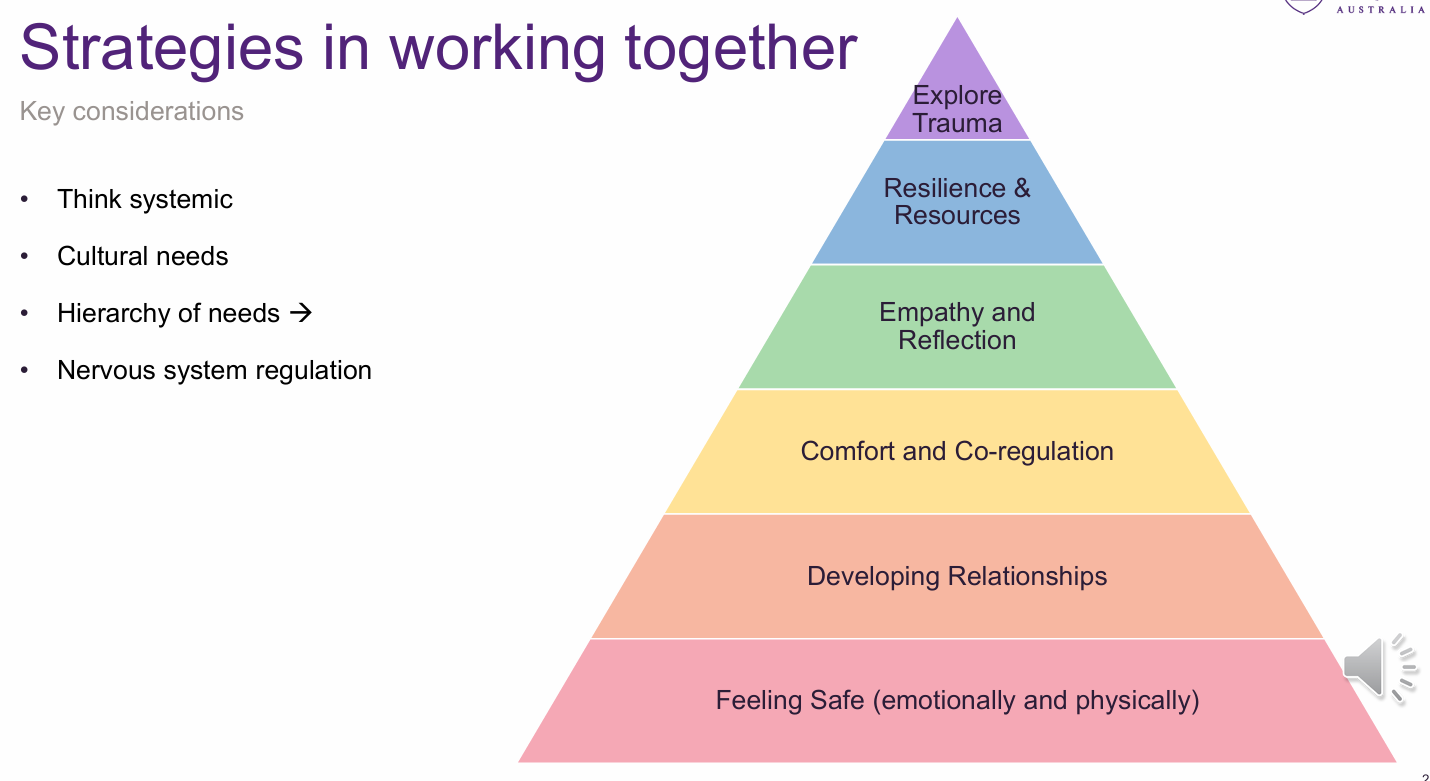
consider hierarchy of needs (see image) → have the child’s lower tier needs been met?
use multiple formats (visual, verbal, etc.)
encourage caregiver involvement
avoid jargon
be adaptable
incorporate play
aboriginal and torres strait islander social and emotional wellbeing cards (SEWBs)
factors that impede the development of a therapeutic alliance
• Not feeling heard and/or respected
• Receiving treatments/interventions they did not agree with
• Not maintaining confidentiality
• Systemic factors (e.g., change in clinician)
• Needing time to gain trust and familiarity
• Difficulty building trust based on negative past experiences
• Fearing consequences of trusting others
• Power dynamics and autonomy
distrust of authority
emotional and behavioural responses
trauma
ACES
reluctancy to open up
inconsistent engagement
strategies for forming therapeutic alliances
guide don’t rule
meet the person where they are at
don’t judge them
offer choice
transparency, respect for privacy and confidentiality
avoid assumptions
be curious and open
be flexible with mode of communication (e.g. texting vs emailing)
agree on guidelines
agree on goals
if indigenous use SEWB cards
the five guiding principles of trauma informed care
(see image)
safety
choice
collaboration
trustworthiness
empowerment

the trauma informed care approach
avoid re-traumatisation
realise impact of trauma on access to services
respond by changing policy, procedure, and practices
train staff to recognise signs and symptoms
integrate knowledge about trauma to services
motivational interviewing
4 Core Principles
• Express empathy
• Develop discrepancy
• Roll with resistance
• Support self-efficacy
• Collaborative, person-centred counselling approach • Strengthens motivation and commitment to change
• Creates supportive, non-judgmental environment where clients explore their own reasons for change
• Benefits in speech pathology:– Builds a trusting therapeutic relationship– Encourages client autonomy– Respects individual readiness and willingness to engage
• Particularly relevant in mental health & justice contexts with clients who may be harder to engage or have lower self-efficacy
PACE
PACE (Playfulness, Acceptance, Curiosity, Empathy) & DDP (Dyadic Developmental Practice)
• Therapeutic framework for paediatric clients in mental health and justice contexts.
• Designed to foster trust and emotional safety, especially for children with trauma or ACEs.
• Supports children in ‘sitting with uncertainty’ without rushing trust-building.
• Teaches that adults can be trusted and tough times can be worked through together. • Provides opportunities to strengthen relationships and help children feel secure.
• Helps children feel that caregivers/clinicians:
– Genuinely want to connect.
– Understand perceptions and feelings.
– Provide safe, non-reactive responses.
MBT
rooted in attachment theory
originally used for people with BPD
targets developing the ability to examine one’s own thoughts and feelings and understand the motivations, thoughts, and feelings of others. this allows the person to identify underlying mental states that impact their interactions with others.
Techniques
1. Broadcast (mark) our minds clearly • Make it clear: “these are my thoughts” → acknowledge clients may think/feel differently. • Support clients in tolerating different perspectives. • Be mindful of epistemic hypervigilance (heightened scepticism of new information).
2. Adopt a Mentalising Stance • Show curiosity, inquisitiveness, playfulness, and open-mindedness. • Take a “not knowing” position – check in, avoid assumptions. • Promote attentiveness to mental states.
3. Marked Mirroring • Identify and describe client’s emotions and expressions in a clear, validating way. • Use activities (e.g., cartoons, thought bubbles) to teach perspective-taking. • Discuss the nature of mental states and people’s internal worlds. • One can’t know what is another’s minds unless they describe their mental state
4. Contingent Responsiveness • Show emotional sensitivity and empathy. • Be reliable and consistent. • Reflect client’s experience accurately and sensitively. • Demonstrate curiosity about client’s thoughts and beliefs.
5. Use Ostensive Cues • Shared eye contact and joint attention. • Use client and family names. • Be mindful of tone of voice. • Maximise gestures and visual supports.
6. Encourage Mentalising Language • Support families to use mentalising language at home. • Emphasise conversations about emotions. • Teach emotional vocabulary. • Teach grammar for talking about thoughts/feelings. • Provide social skills training in emotion recognition & perspective taking. • Teach use of narratives. • Provide psycho-education about thoughts, feelings, and the opacity of minds.
AMBIT
• Team-based, mentalisation-focused approach for complex, hard-to-reach young people. • Recognises key challenges:– Network complexity (multiple services/agencies involved).
– Hard-to-reach young people and families.
– Managing worry and risk in care.
– Learning at work through team reflection and support.
• Mentalising applies to all aspects of practice – not just the client–worker relationship.
• Strong emphasis on initial engagement and relationship building.
• Illustrated in the AMBIT Wheel

core counselling skills for speech pathologists
attending:
posture
appropriate body motion
eye contact
non-distracting environment
following:
door openers
minimal encouragers
attentive silence
let people cry
reflecting skills:
paraphrasing
reflect feelings
reflect meaning