Pediatrics 2
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
45 Terms
A 10-year-old boy presents with Coca-Cola–colored urine and edema of his lower extremities. On physical examination, the patient has a blood pressure of 185/100 mm Hg.He does not appear to be in any distress. His lungs are clear to auscultation, and his heart has a regular rate and rhythm without any murmurs, gallops, or rubs. His past medical history is remarkable for a sore throat that was presumed viral by his physician 2 weeks before. What is the Diagnosis and etiology of this disease?
Acute post streptococcal Glomerulonephritis
Follows infection with nephrogenic strains of group A beta-hemolytic strepto- cocci of the throat (mostly in cold weather) or skin (in warm weather). Spread through droplets.
Mention the age range involved and clinical presentation involved in this case presentation?
Most 5–12 years old (corresponds with typical age for strep throat).
1–2 weeks after strep pharyngitis or 3–6 weeks after skin infection (impetigo) .
Ranges from asymptomatic microscopic hematuria to acute renal failure, oedema, hypertension, hematuria (classic triad) .( Dark urine (brown -tea-or coca coloured).
Pharyngitis
Periorbital edema, Generalised oedema
Hypertension, oliguria
Circulatory congestion e.g dyspnea
Non specific sympptoms -general malaise, anorhexia, fever, abdominal or flank pain, nausea and vomiting.
Unusual presentation can be Atypical HUS, Refractory hypoxic respiratory failure, Seizures and other central nervous system, Severe nephritis including acute kidney injury and heamatologic anomalies.
What are the clinical investigations you’ll request for this patient?
Urinalysis—RBCs, RBC casts, protein 1–2 +, polymorphonuclear cells
Mild normochromic anemia (hemodilution and low-grade hemolysis)
Low C3 (returns to normal in 6–8 weeks)
Need positive throat culture or increasing antibody titer to streptococcal anti- gens; best single test is the anti-DNase antigen
For diagnosis of prior Strep infection, use streptozyme (slide agglutination), which detects antibodies to streptolysin O, DNase B, hyaluronidase, streptokinase, and nicotinamideadenine dinucleotidase.
Consider biopsy only in presence of acute renal failure, nephrotic syndrome, absence of streptococcal or normal complement; or if present >2 months after onset
What are the complications of this disease?
Hypertension
Acute renal failure
Congestive heart failure
Electrolyte abnormalities
Acidosis
Seizures
Uremia
What are the treatment of this this disease? (in-patient, if severe)
Antibiotics for 10 days (penicillin)
Sodium restriction, diuresis
Fluid and electrolyte management
Control hypertension (calcium channel blocker, vasodilator, or angiotensin- converting enzyme inhibitor)
You are working in a Paediatric Out Patient clinic, You encountered Selma, a 12 year old girl of Asian descent. She describes a two month history of general malaise and decreased energy. Her mother states that her daughter has felt “feverish” on and off for the last 2 months. She used to play soccer regularly, but she has stopped participating not only because she feels “too run down” but she has also been having pain and stiffness in her left knee. Last week when she was out in the sun with her classmates she developed a Butterfly rash on her cheeks. What would your approach be to this patient??
What is the diagnosis of this patient and definition?
SLE is a systemic multi-system autoimmune disease characterized by the presence of autoantibodies and multiorgan system involvement.
What are the 11 criteria of this diagnosis?
M- Malar rash: this rash is a fixed erythematous rash over the malar eminences – commonly called a ‘butterfly rash’. It can be flat or raised, and tends to spare the naso- labial folds
D- Discoid rash: this is a raised, scaling and scarring rash. It is extremely rare in paediatric patients
S- Serositis: literally means ‘inflammation of a serous membrane’; most commonly involving the heart or lungs in SLE, i.e. pleuritis or pericarditis
O- Oral/Nasal ulcers – this ulceration is usually painless, and is often on the palate or nasal septum
Arthritis – this is non-erosive arthritis involving two or more peripheral joints, characterized by tenderness, decreased range of motion, and effusion.
P- Photosensitivity– rash from sun exposure (notably, sun exposure can trigger a flare of SLE and therefore sun protection is key in patients with SLE).
B – Blood abnormalities – this includes hemolytic anemia (with reticulocytosis), leukopenia, lymphopenia and thrombocytopenia.
R – Renal dysfunction – there are 6 classes of SLE nephritis and a broad range of presentation and severity, from asymptomatic to severe nephritic or nephrotic syndrome.
A – ANA positive – This is anti-nuclear antibody. Essentially all patients with SLE are ANA positive.
I – Immunologic – These are other specific antibodies, including anti-ds-DNA, anti-Smith, anticardiolipin antibodies and lupus anticoagulant.
N – Neurologic – Lupus can present with a wide array of central and/or peripheral signs and symptoms. This can be anything from headaches and difficulty concentrating to seizures and psychosis.
How will you approach history of this patient?
HPI: General description from the patient on the course of her symptoms
Rheumatologic Review of Systems
General: Any fever? Weight loss? Malaise?
CNS: Any headaches? Recent difficulties with concentration,school performance, depression, memory loss, hallucinations? Seizure activity?
Head and Neck: Very dry eyes and/or dry mouth (SICCA symptoms)? Nose bleeds or sores in your nose? Sores in your mouth? Any hair thinning or falling out?
Cardiorespiratory: Any chest pain (worse with deep breaths)? Shortness of breath or exercise intolerance?
GI: Any stomach pain or diarrhea (serositis in SLE can include abdominal lining)?
GU: Any blood or coke-coloured urine? Any foamy urine? Any swelling in your feet or around your eyes (nephrotic syndrome)? Any headache or visions changes consistent with hypertension?
MSK: Any joint pain, swelling or tenderness (associated morning stiffness?)? Any muscle weakness or pain?
Derm: Any colour changes from white-blue-red in your hands or feet consistent with Raynauds phenomenon? Any rashes (specifically after being out in the sun)? As in all cases, a thorough Pediatric History should include: medications (some medications can trigger Drug-induced lupus), Allergies, Immunizations, developmental History, past Medical History
Family History (often other autoimmune diseases in the family)
Social History (including HEAADS in adolescent history)
How will you approach your physical exam in this patient?
Vitals (tachypnea, hypertension)
Alopecia
Facial rash or edema
Oral or nasal ulcers? (Make sure you look on the palate and in the nose because the patient will often not even realize that they have them.)
Palpate for lymphadenopathy
Thorough respiratory and cardiovascular exam
Thorough GI exam
Complete detailed MSK and neurological exam assessing for arthritis and weakness and other neurological features
Exam for peripheral edema
Thorough skin exam for rashes (malar, discoid, vasculitic, periungal erythema)
What is your clinical investigations of this case presentation?
CBCd, blood film, extended lytes, Cr, Urea, ESR, CRP, urinalysis including microscopy, urine protein: creatinine ratio. AST, ALT, albumin, INR, PTT , CK (myositis)
TSH, ANA, C3, C4, Immunoglobulin panel, Rheumatoid Factor, DAT (Coombs test)
Consider infection (either DDx or trigger of a flare of SLE): depending on the patients features -parvovirus, CMV, EBV, blood and urine culture (consider)
More extensive work-up: ENA Panel (4 Extractable Nuclear Antigen Antibodies), Anti- dsDNA, Anti-phospholipid antibodies
May consider: glucose, anti-TTG, D-dimer, fibrinogen, cholesterol studies, ferritin, haptoglobin, LDH
As symptoms indicate: CXR, ECG, echo – other investigations and consultations as necessary
Opthalmologic Eye exam is essential
How will you treat your patient?
Treatment approach:
Non-pharmacologic – sun protection is key to preventing rashes and avoiding flares
Pharmacologic treatment (these would all be initiated in conjunction with advice from pediatric rheumatology)
- Hydroxychloroquine (Plaquenil)
- NSAIDS (If no renal involvement)
- Steroids (from low dose oral to high dose IV steroids)
- Disease Modifying Anti-Rheumatic Drugs (DMARDS), biologic medications or cytotoxic drugs
Pandu is 10months old boy, brought into POPD with gastro-enteritis which started 2 days ago. You noticed in his Clinic Card that he only received birth Immunisations, the rest was not given. She is RVD unexposed, rapid negative (1month ago), she is thriving along the -1 Z-score WFL (weight-for-length). She had a T:37.6 °C HR:135 bpm RR: 40. She was breastfed for 8months and her mother started weaning her on Formula milk and soft feeds.
Which age Immunisations are outstanding?
6 weeks, 10 weeks, 14 weeks, 9 months
Which Immunisation for the specific ages are outstanding for Pandu?
6 wks:
Polio 1
Pentavalent (Diphtheria, Pertusis,
Tetanus, Haemophilus influenza type B,
Hepatitis B
Pneumococcal vaccine (PCV)
Rotavirus 1.
10wks:
Polio 2
Pentavalent (DPT,Hib, HepB)
Pneumococcal vaccine 2
Rotavirus 2
14wks:
Polio 3
Pentavalent
Pneumococcal vaccine
9mo:
Measles
Rubella (MR)
Based on her age which Immunisations are contra-indicated?
Rotavirus vaccine
You are the Medical Intern seeing the patient, you counselled the mother on the
importance of vaccinations. She understands the implication of not been vaccinated.
She agrees for you to catch up Pandu’s Immunisation. Which immunization would you
give first?
Measles vaccine
How would you space the rest of the rest Immunisations and how many doses are
required?
Polio: 4 weeks apart, (2more doses)
Pentavalent: 4 weeks apart (3 doses)
PCV: 4weeks (between dose 1-2) then 8 weeks (between 2-3rd dose) = total 3dose
Mrs Angula, Pandu’s mother further elaborates that Pandu previously had a fever of
38°C the previous day and after her first Immunisation she cried for 1hour, thus she
was reluctant to take her for the subsequent Immunisation.
What would be absolute contra-indications for not Vaccinating?
Severe allergic reactions (Anaphylactic shock) after a
vaccine.
Encephalopathy not due to another identifiable cause
occurring within 7 days of a Pertusis vaccine.
Live vaccines should be avoided in patients with Severe immunodeficiency states, like Severe Combined Immunodeficiency (SCID), patients on high dose corticosteriods, patients with malignancy-post Chemotherapy
Which vaccines in the Namibian EPI schedule is live-attenuated?
Oral Polio vaccine
BCG
Rotavirus
Measels vaccine
14month old girl Dankiros was brought in by her father Mr Matroos to the POPD with 2week history of lethargy, not been playful and swelling of the body. The father reveals that the mother is currently nursing a 2month old baby, thus Agaros was weaned off the breast at 4months when the mother noticed that she was pregnant. Dietary, Dankiros has been formula fed since 4months and drink supplementary Magua (Porriage-based drink), when funds are available she sometimes eat vegetables, fruits, rice and yoghurt. He often pica for soil and ice. On examination Dankiros was irritable, lethargic, with pitting pedal oedema, pallor, desquamating skin rash and hepatomegaly. Her Anthropometry is demonstrated below:
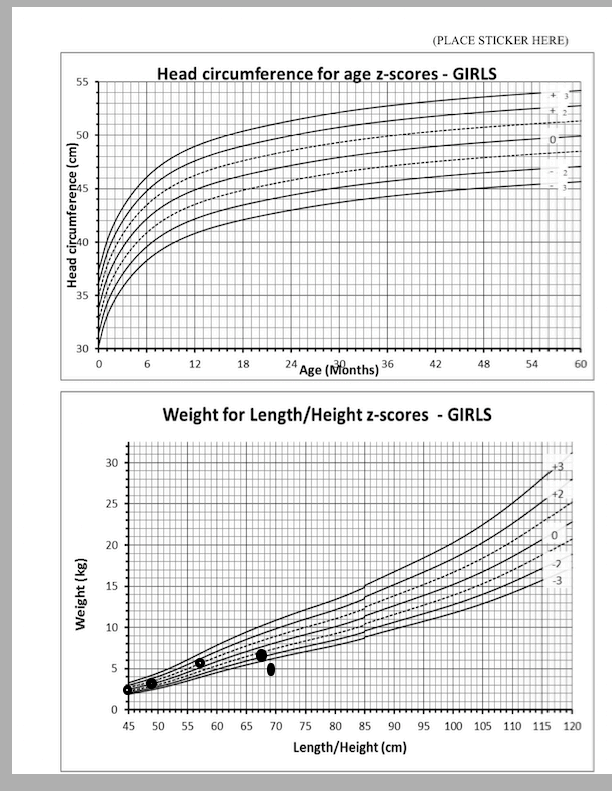
Interpret the above anthropometry
Failure to thrive with crossing centiles, initially was growing well on the 0-z-score then dropped his Z-score to -2 then -2 to -3 z-score and now less than -3 Z-score. (WFA)
WFA: severe UWFA, <-3 Z-score
HFA: severely stunded, <-3 Z-sore
WFH: severely wasted, <-3 Z-score
What is the most likely diagnosis?
Severe acute malnutrition with oedema
Which other Anthropometry marker would you like to know to confirm your diagnosis?
What do you expect it to be?
Mid-upper Arm Circumference (MUAC) <11.5cm
Supply FOUR (4) reasons for your most likely diagnosis?
She has Severe Acute Malnutrition with oedema (Kwashiokor) because she is weaned off from breastfeeding early due to mother who had to feed a sibling and was started on carbohydrate based drink.
Possibly the formula feeding is not adequate or not mixed properly to provide proteins and other micronutrients the patient need to thrive.
Children with Kwashiokor have pitting oedema in the extremities depends on the severieties.
These children also have abdominal distension secondary to poor abdominal musculature and hepatomegaly secondary fatty infiltration.
Skin changes are charcteristics and progress over a few days, become hyperpigmented, dry and then splits open
when stretched, reaveling pale areas between the cracks
called crazy paving or flanky paint dermatosis.
Name FIVE (5) major GROUP abnormalities you should correct as part of the
management of this patient?
Correct Hypoglycaemia
Correct Hypothermia
Correct Macronutrient deficiencies
Correct Micronutrient deficiencies
Correct electrolytes: Hypokalemia, hypomagnesaemia,
hypophophataemia, hypocalaemia
Correct dehydration
Treat infection
Mr Matroos further states that Dankiros had diarrhea for the past 10days, which (a) TWO (2) supplements will you include as part of his management? (b) Which one has been included in the Namibian EPI schedule to further decrease diarrhea and name one (1) major toxicity signs/symptoms (except Nausea, headache,Vomiting)?
(a) Zinc and Vitamin A
(b) Vitamin A: Raised Intracranial pressure, Alopecia, hepatomegaly, fatigue, dry skin, hyperostosis and irritability.
While examining Dankiros’ abdomen you noticed that it is distended and the liver is enlarged, explain the pathophysiology for hepatomegaly in light of his underlying condition? Total Protein: 70 (43-70) Albumin: 15 (36-51) ALT 20 (18-32)
Hepatic glucose stores are depleted and gluconeogenesis is impaired (especially in more advance disease). Synthesis of lipoprotein is reduced, which leads to a limited ability to mobilize fat resulting in fatty infiltration, the lipid that accumulate is triglycerides and disappears in about 3weeks as the child recovers. Synthesis of albumin is low, but synthetic function of liver is relatively preserved.
You discussed this patient with your Medical Officer, one of the bloods suggested to
do is an FBC? Below are the results:
WCC: 25 X109 /L (6-18)
RCC: 1.85 X 1012 (3.8-5.4)
Hct: 0.096 l/l (0.31-0.46)
Hb: 7.2 g/dL
MCV: 65fl (70-86)
RDW: 26% (11.6-14.5)
Platelets: 600 X 109 /L
Interpret the FBC?
Differential count: Neutrophil predominance, with 15% Bands
Mr Matroos further is concerned why Dankiros likes to eat soil, how will you explain this to him?
Microcytic hypochromic anaemia with high RDW most
likely Iron deficiency anaemia
In the acute phase which supplement should you avoid, based on the underlying problem in the above FBC?
Iron should be deferred until infection is treated and outside acute phase
You decided to start feeding at day 2 admission, however when the father was not monitored, so he decided to feed larger volume feeds, in the hope that Dankiros will gain weight faster and be discharged. On your call you found that after the presumed improvement he had made in the pass 3 days he was now hypotonic from muscle weakness, cardiac failure and had 1 seizure. Bloods taken:
Na: 132 (131-145) K: 2.1 3.6-5.2) U: 3.5 (1.7-6.5) Cr: 52 (27-55) Ca (corrected):
2.3 (2.25-2.73) Mg 0.6 (0.70-1.15) PO4: 0.3 (1.10-1.91)
What is the most likely explanation for his sudden deterioration? How will you explain this to the father?
REFEEDING SYNDROME:
§ This is caused by the metabolic and physiological consequences of the depletion, repletion and compartmental shifts of phosphorus, potassium, magnesium, glucose metabolism, vitamin deficiency and Insulin levels increase after re-feeding. This result in Phosphorus, potassium and magnesium shift to the intracellular spaces, causing a drop in serum levels. Clinical presentation include muscle weakness, seizures, rhabdomyolysis, cardiac arrhythmias, cardiac failure and haemolysis. Thus before re-feeding is instituted the electrolyte imbalance, vitamin and trace element deficiencies should be corrected.
Mention 2 strategies we can use to prevent the above and what is the target weight gain rate?
(a) Feeding slowly and increasing cautiously.
(b) Correct electrolyte imbalance, vitamin and trace element deficiencies.
(c) Supplement Thiamine prior to re-feeding with carbohydrates, since Thiamine utilization increases with re-feeding .
(ii) At least 10g/kg/day
You are working in the Pediatric out-patient department at Intermediate hospital Katutura, Jayden a 6-month-old boy presents with cough and difficulty in breathing. Jayden’s mother who is 15-years-old, reports that she tested positive for Human Immunodeficiency virus (HIV)infection during antenatal care in the last semister and she is on first line treatment. She also reports that Jayden was also given medication post-delivery.
What is the recommended HIV prophylaxis for a high-risk neonate? What is the duration?
Nevirapine and AZT( Zidovudine) Ideally for 6 weeks.
§ If breastfeeding AND mother’s VL > 40 or more or unknown,
continue with NVP daily
§ If NOT breastfeeding since birth or in last 4 weeks, OR mother’s
VL<40, discontinue infant prophylaxis and continue to
monitor mother’s VL as prescribed
What are the THREE criteria you will consider to initiate Jayden on high-risk prophylaxis?
Born to women with HIV infection who have received less than 4 weeks of ART at the time of delivery
Born to women with HIV infection with VL >40 copies/ml in the
3 months prior to delivery
Unknown VL
Born to women with HIV infection diagnosed during labour
and delivery, post-partum or in the breastfeeding period
What is the recommended age in infants to start co-trimoxazole prophylaxis in HIV exposed infants and reasons?
From 6 weeks till HIV status is confirmed.
§ Prevent PCP in HIV exposed infants
§ Protect against common bacteria infections, toxoplasmosis and malaria
When do you stop the co-trimoxazole in an infant who is HIV exposed?
I month After cessation of breastfeeding after
confirmation of DNA PCR negative results
You decide to admit Jayden and treat for the pneumonia. His polymerase chain reactive (PCR) test is positive for HIV even though he was given prophylactic therapy. What are the possible explanations or reasons why Jayden is HIV infected even though his mother mentioned Jayden received prophylaxis and mother was on treatmentduring pregnancy?
Jayden was a high risk patient because his mother started ARV treatment in the last semester possibly he got infected in utero, intrapartum and postnatally through breatfeeding.
The factorS for MTCT is host genetic factors, maternal or infant coinfection, behaviorand nutruition
Genetic factors
§ Fetal Gender and HLA type
§ Maternal – Fetal HLA concordance
§ SNPs for chemokines/chemokines receptors/innate immune factors
Maternal factors
§ Chorioamnionitis
§ STIs: genital ulcer diseases including HSV2 and syphilis
§ Malaria
§ TB
§ Mastitis/breast abscess
§ Oral candidiasis in the infant
§ Resistance to medication
§ High viral load
Behavioral factors
§ Illicit drug use during pregnancy
§ Frequency of sexual intercourse during pregnancy
§ Number of sex partners during pregnancy
§ Infant feeding practices: breastfeeding, mixed feeding, food premastication.
§ Adherence to the prophylaxis medication.
§ Underdosing the medication.
Maternal nutritional status
§ Advanced maternal disease with immunosuppression and malnutrition
§ Vitamin A deficiencies
§ Other micronutrients deficiencies
STI: Sexually transmitted infection
What condition will you investigate before starting Jayden on antiretroviral therapy?
TB
What drug regimen will you initiate Jayden?
Infants 4 weeks to 2 years old ABC/3TC/DTG where Jayden age group belongs
Jayden’s results are positive for cytomegalovirus (CMV) pneumonia, negative for Pneumocystis jiroveci pneumonia (PJP/PCP) and negative for other tests. He is still being breastfed and the mother has a two-months history of cough and constitutional symptoms. What prophylaxis would you give Jayden if you suspect that the mother has tuberculosis and why?
Isoniasid Preventive Treatment.
§ All newborns with no signs and symptoms of active Tb disease that are born to mothers with active Tb disease.
§ All under 12 months HIV-infected children without signs and symptoms of active TB disease and with a known Tb contact.
§ All HIV- infected children who are 12 months or older with no signs and symptoms of active Tb disease.
Signs of allergic rhinitis
Allergic shiners: dark discoloration beneath the eyes as aresult of obstruction of lymphatic and venous drainage, chronic nasal obstruction and suborbital oedema.
Dennie-mogan lines: creases in the lower eyelid radiating outward from the inner canthus, caused by spasm in the muscles of maxiller around the eye as a result of chronic congestion and stasis of blood
Allergic salute: a gesture characterized by rubbing the nose with the palm of the hand upward to decrease itching and temporarily open nasal passages
Allergic crease: transverse crease near the tip of the nose
A child presents with 3day hx of puffy eyes, worse in the morning, swollen feet and distended abdomen. Her mother reports that prior to this presentation she had a mild URTI 1 week before. On examination she looks well and apyrexial, but has periorbital pitting oedema, pitting pedal oedema and ascites. Her HR 115bpm, BP108/74, temp 36, with cap refill time 2sec.
UA: blood1+,protein4+,Leuc(-), nit(-), pH6
Bloos Tproit65, alb 19g/dl(38-54), FBC,UEs Norm
What is the most likely dx?
Nephrotic syndrome
What are the 4 classic features?
Oedema
Severe proteinuria (3-4+)
Hypoalbuminemia <25g/l
Hyperlipidemia/hypertriglycaeremia
List 3 other investigations you will request to make definite dx
Lipogram
C3,C4
UPCR
T/F
The pathophysiology of nephrotic syndrome is both humoral and cell mediate, resulting in inflammation of the glomeruli, which further caused antigen trapping in the basement membrane, this antigen-antibody reaction result in glomeruli damage and protein leakage.
False; this is for nephritc sx
This disease doesnt occur in children with scd
false, SCD pts are high risk and should be screened routinely
Hep B, HIV, TB, congenital syphyllis are secondary causes
True