L13 Corneal Injury
1/82
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
83 Terms
while assessing corneal injury what aspect of intro exams is most important
hx, get a complete description of the traumatic event
what characteristics of object trauma is important (2)
foreign body (inert vs inflammatory)
energy (amount, type, wavelength, power, and duration)
what is corneal abrasion
removal of corneal epithelium
corneal abrasion is also a ____ defect without underling corneal _____ or infection
epithelium, inflammation
t/f corneal abrasion is one of the most common defects
true
how causes corneal abrasion
tangential impact from foreign body
t/f corneal abrasions can be from finger nails, paper, mascara brushes, plants and CL use
true
tangential force applied--> epithelial cells separate from underlying attachement
this is the pathophysiology for
corneal abraison
t/f corneal abrasions doesn't always include Bowmans membrane
true
while examining corneal abrasion you should look for (3)
extent, location, and globe penetration
a patient comes you complaining of pain and foreign body sensation. upon silt lamp and prelims they present tearing, photophobia with a VA worse than 20/20. as well as loose epithelium, staining defect, roughening of corneal reflex, AC reactions and granular stroma. What is your diagnoisis
corneal abrasion
what corneal abrasion you just diagnosed, what are 3 treatment options
1. cycloplegia possibly with NSAID for symptoms
2. topical antibiotics for prophylactic reasons
3. protective healing
one of tx options is cycloplegia; what are the 3 options available with dosing
1. cyclopentolate 0.5% or 1% 1gtt BID or TID for small to moderate abrasions
2. homatropine 5% or scopolamine 0.25% for larger abrasions
3. ketorolac 0.4-0.5% QID x3 days
one of tx options is topical antibiotics; what are the two options
1. broad spectrum abx: polytrim 1gtt OR fluoroquine 1gtt QID or tobramycin/gentamicin
2. aminoglycosides
for protecting healing, you should avoid patch if CL related? yes or no. why
yes; risk of MK
for protecting epithelium healing for corneal abrasions. what is the process
epithelial debridement may be a patch of BCL
1 day f/u if patching or BCL and corneal abrasion is large or central
AND
2-5 days f/u if small or peripheral
is management for
non CL wearer
Close f/u with additional 1-2 days of abx prophylaxis following closure then resume CL wear after 1 week cessatin of abx
this is the management for
CL wearer
what can occur after a corneal abrasion
Recurrent corneal erosion
what is an recurrent corneal erosion (RCE)
repeated breakdown of epithelium due to dysfunction in epithelial-stromal complex integrity
what are some risk factors / etiology for RCE (4)
history of corneal injury/ truama
dystrophies
ocular surace disease
systemic illnesses
where does RCE typically occur
within lower half of cornea
the 4 different Pathophysiology for _____ is
1. abnormalities in normal adhesion of epithelium leads to epithelial elevation and accumulation of debris disrupts attachment of epithelium
2. random production of BM and CT material leads to disrupted attachment of epithelium
3. increased epithelial separation at night + eyelid adherence leads to shearing forces to epithelium
4. MMP degrade collagen and laminin leading to upregulation of MMPs leads to BM degradation and poor BM adhesion
RCE
a patient comes to you complaining about pain. they explain the pain is more severe when just waking up. The pain is random and not constant. they elaborate they sometime feel like they cant see, their eyelids get swollen , teary, and light is bothersome. with redness. during slit lamp examine you notice the epithelium is loose and some epithelial microcysts. with staining, there is some stain as well as areas with negative staining. what is your diagnosis
RCE
a sign of RCE is there are areas of negative staining, which is significant. why?
there are divots/ folds that will stain and then areas that will not because it is elevated
when considering RCE as a diagnosis what are some important clinical hx to ask (5)
1. previous trauma
2. prior episodes
3. pain on waking
4. epithelial defect or loose epithelium
5. predisposing conditions
RCE can lead to (3)
bacterial keratitis, fibrosis, decreased vision
what is the tx for acute RCE (3-4)
cyclopentolate 1% tid
AND
erythromycin or bacitracin QID -6xday (topical 1gtt QID if large or BCL)
POSSIBLY: 5% NaCl for proplyctic reasons
what is the tx for resolved RCE (2)
artificial tears/ointment
5% NaCl qhs x 3-6 months
what are the pro and cons of topical ointment
pro: longer contact time
cons: cant see when its on but can use the other eye
RCE can be recalcitrant or not respond to tx, what are the tx options then?
1. 5% NaCl prophylactically
2. oral doxy 50 mg +/- topical steroid (fluorometholone 0.1% BID- QID for 2-4wks)
3. extended BCL
4. anterior stroma puncture (manual or laser)
5. debridement + diamond burr polish
6. phototherapeutic keratectomy (PTK)
___ ___ ___ is corneal damage following exposure to UV radiatin
ultraviolet keratopathy (photokeratitis)
what is the wavelength for UVA
320-400nm
what is the wavelength for UVB
290-320nm
what is the wavelength for UVC
200-290nm
the cornea absorbs what UV wavelengths
UVB and UVC
what can 3 things that can lead to ultraviolet keratopathy (photokeratitis)
welders keratitis, snow blindness, UV lamps
a patient comes to you telling you they feel like there is something stuck in their eye, pain and overall discomfort. they also cant stand looking at light. you ask for history and they said they are daily welders. during slit lamp there is slight edema, dull corneal reflex, less corneal sensitivity, and some epithelial defects. what is your diagnosis
photokeratitis- UV radiation
when someone is diagnosed with photokeratitis- UV radiation. what is their prognosis
usually full recovery
what can occur after photokeratitis- UV radiation (2)
pterygium, endothelial morphology changes
what are other differentials to think about when diagnosing photokeratitis- UV radiation (4)
dry eye, drug toxicity, chemical exposure, viral conjunctivitis
what are 3 tx options for photokeratitis- UV radiation with dosing
cycloplentolate 1% gtt TID
erythromycin or bacitracin 4-8x daily
oral analgesics prn
___ ___ ___ ___ is corneal damage due to wavelengths above the visble spectrum (10^-4). usually accompanied by intense heat
infrared radiation corneal injury
what are two types of infrared radiation corneal injury
flame and contact
although possible to get a infrared radiation corneal injury, its rare because of our ___ reflex and ___ turn
blink, head
clinical presentation of infrared radiation corneal injury consists of destruction of the ______, stromal _____ which is worse than the epithelial damage. the changed within 20 minutes with continued ____ and stromal edema
epithelium, opacification, progression
_____ ___/____ is corneal injury secondary to direct application of heat.
thermal burn/ keratopathy
for thermal burn/ keratopathy, tissue reaction is dependent on
temperature of heat source
for thermal burn/ keratopathy with HOT WITH HIGH HEAT leads to (4 in chronicological order)
-->severe burn getting deeper layers--> opacification--> sloughing-->corneal thinning
for thermal burn/ keratopathy with LOW HEAT leads to (2 in chronicological order)
--> tear films cools cornea--> cast of anterior surface of eye
what are prognastic factors for thermal burn/ keratopathy (4)
temperature, heat-retaining capacity of material, duration, area
a patient comes to you with signs of thermal burns. you consider it to be severe. what are the tx for this
surgical intervention for corneal ectasia or symblepharon
a patient comes to you with signs of thermal burns. you consider it to be minor. what are the tx for this (3)
similar to corneal:
alleviate sx, prophylactic antibiotics, protective healing
what can occur after a thermal burn/ keratopathy (4)
angiogenesis, corneal flattening, scarring/opacification, corneal necrosis
___ ___ is a chemical, nonmechanical injury to the eye that damages the ocular surface.
chemical burn
can a chemical burn cause permanent vision loss? yes or no
yes
can chemical burns causes acute and chronic changes?
yes
chemical burns often happen in who?
young, working individuals,
lower to middle income
(dr e said basically anyone)
what is the pathophysiology for alkali and and acid burn?
stromal penetration--> shrinkage of collagen--> distortion of TM release of PG--> acutely elevated IOP
____ of chemical burn depends on
type of chemical
concentration & pH of solution
extent of exposure
duration of exposure
degree of penetration
severity
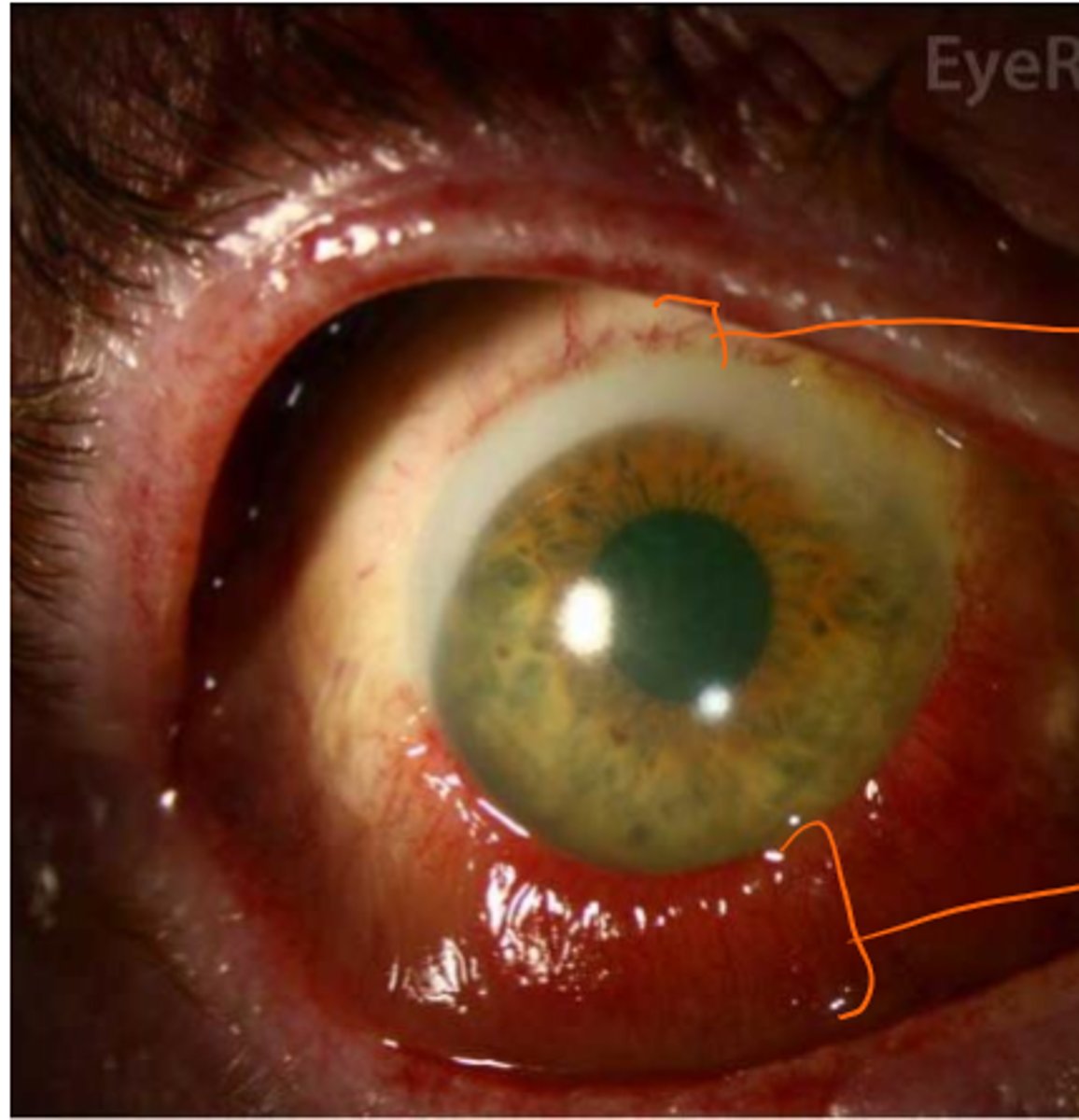
there are many sequelae to chemical burns in the conj/ limbus or cornea, but what are the important 6?
limbal stem cell defiency
persistent epithelial defects
recurrent corneal erosions
dry eye
uveitis
glaucoma
____ chemical burn is damage secondary to alkalis. its more frequent
alkali
alkali chemical burn is more severe than other type of burns? yes or no
yes
during alkali burns, _____ intraocular damage noted at pH greater than or equal to ___
irreversible, 11.5
pathophysiology of alkali burn: begins with a hydroxyl ion ______ fatty acids in cell membranes leading to cell ___ and then to hydrolysis and _____ of proteoglycans & collagen
saponifies, lysis, denaturation
greater penetration of alkali burns lead to
greater damage to stroma & endothelium + intraocular structures
what causes alkali burns (6)
ammonia
lye
calcium hydroxide (lime)
potassium hydroxide
airbag powder
how does alkali chemical burns present?(2)
ischemic necrosis and blanches conjunctival vessels
alkali chemical burn- superior is worse than inferior bc there is no blood supply leading to necrosis of the cells (irreversible)
____ chemical burn is
corneal injury secondary to exposure to acids
acid
acid chemical burn is generally ____ severe
less
t/f in acid burns, superficial damage due to immediate precipitation of epithelial proteins unless strong or high concentration acid
true
pathophysiology of acid burn begins with hydrogen ion of acidic alters __ and then anion leading to protein ____ and ____ in corneal epithelium and superficial stroma allowing penetration of the barrier
pH, binding and precipitation,
what causes acid burns (10)
sulfuric, sulfurous, hydrochloric, nitric, acetic, formic, hydrofluoric
battery acid, pool cleaner, vinegar
a patient comes to you office complaining of severe pain and they mentioned they were squeezing lime and decent amount got into their eye. whats their diagnosis?
alkali chemical burn
a patient comes to you office complaining of severe pain and they mentioned they were charging their tesla and the battery exploded and got into their eye. whats their diagnosis?
acid chemical burn
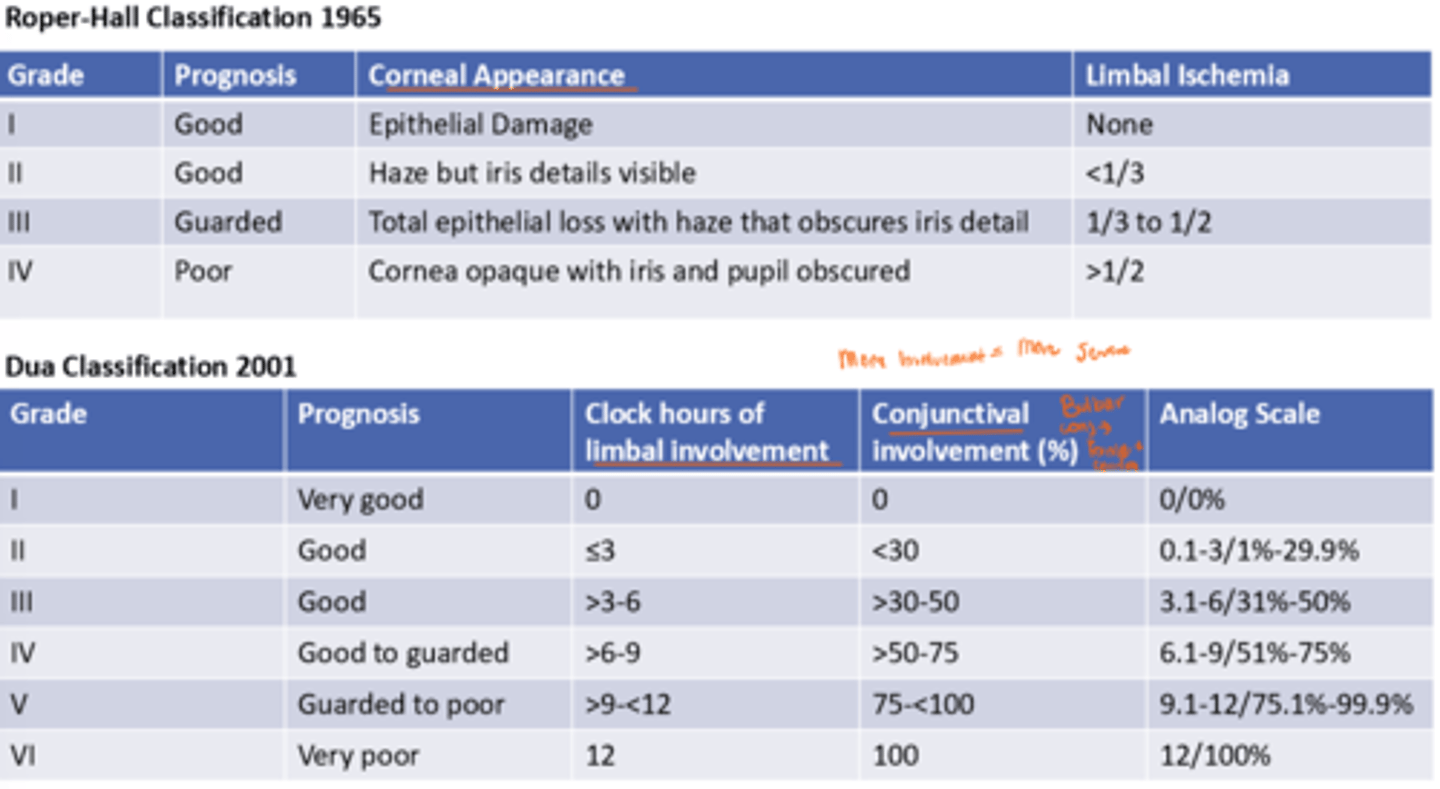
a patient comes to your office with a chemical burn. you decide its a grade I or acute. whats the treatment (3)
1. irrigate with 1L for 15 mins until neutral pH. get into fornices
2. debride of necrotic tissue
3. topical steroid & oral pain med
care with ciproflaxin bc its a vasoconstrictor
while irrigating what is something important NOT to do
do NOT irrigate with opposite neurilizing agent
while treating acutely or Grade I chemical burn. what is added if IOP is elevated? (4)
acetozolamide 250mg PO qid or 500 mg PO BID
OR
methazolamide 25 to 50mg po bid or tid
add b-blocker (timolol 0.5% bid)
NO a-agonist
what is tx options for Grade II-III chemical burn (7)
10% topical ascorbate or citrate for alkali q2h
BCL
doxy 100mg po bid
oral vitamin C
amniotic membrane (inoffice)
autologous serum tears
platelet rich plasma
what is the tx options for a Grade IV chemical burn including if melting/perforating (5)
tarsorrhaphy
melting: collagenase inhibitors,
cyanoacrylate tissue adhesive,
patch graft,
corneal translate
tx for _____ chemical burn includes
reconstruction of eyelids & fornix
- conj graft or tasorrhaphy
amniotic membrane transplant
LSC transplant
keratoprosthesis
glaucoma management
chronic