Mycology
5.0(1)
Card Sorting
1/129
Earn XP
Description and Tags
Last updated 4:51 AM on 11/6/22
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
130 Terms
1
New cards
Superficial Mycoses
surface growth: skin and hair
2
New cards
Pityriasis Versicolor
Associated with pigmentation
Malassezia complex
Observed worldwide (Especially in tropical environments)
Long, pink (gram-negative)
Malassezia complex
Observed worldwide (Especially in tropical environments)
Long, pink (gram-negative)
3
New cards
Pityriasis Versicolor: Transmission
Contact with patches
4
New cards
Pityriasis Versicolor: Treatment
Not required -> not dangerous
Rarely resolves on its own
Antifungal ointment or shampoo
“Cosmetic/aesthetic issue”
Rarely resolves on its own
Antifungal ointment or shampoo
“Cosmetic/aesthetic issue”
5
New cards
Tinea Nigra
Hortaea werneckii
Dimorphic (Black mold; Grows as yeast on skin)
Mostly found in the tropics
Usually young adults and children
More common in women than men
Dimorphic (Black mold; Grows as yeast on skin)
Mostly found in the tropics
Usually young adults and children
More common in women than men
6
New cards
Tinea Nigra: Disease
superficial, causes dark pigmentation
looks like patch on skin
looks like patch on skin
7
New cards
Tinea Nigra: Transmission
Unknown!
Patches do not seem to be infectious
Patches do not seem to be infectious
8
New cards
Tinea Nigra: Treatment
Not required -> not dangerous
Rarely resolves on its own
Antifungal ointment
“Cosmetic/aesthetic issue”
Rarely resolves on its own
Antifungal ointment
“Cosmetic/aesthetic issue”
9
New cards
Black Piedra
Piedraia hortae
Rare (Found in tropical regions )
Associated with poor hygiene
Rare (Found in tropical regions )
Associated with poor hygiene
10
New cards
Black Piedra: Disease
unsightly, brown-black nodules on hair strands (gritty)
11
New cards
Black Piedra: Transmission
unknown (not contagious)
12
New cards
Black Piedra: Treatment
removal of hair, hygiene
13
New cards
White Piedra
not dandruff
trichosporon
found in tropical and subtropical regions
associated with poor hygiene
trichosporon
found in tropical and subtropical regions
associated with poor hygiene
14
New cards
White Piedra: Disease
unsightly, white nodules on hair strands
15
New cards
White Piedra: Transmission
unknown (not contagious)
16
New cards
White Piedra: Treatment
removal of hair
hygiene
antifungal (shampoo)
harder than Black Piedra
hygiene
antifungal (shampoo)
harder than Black Piedra
17
New cards
Cutaneous Mycoses
invades skin, hair, or nails
18
New cards
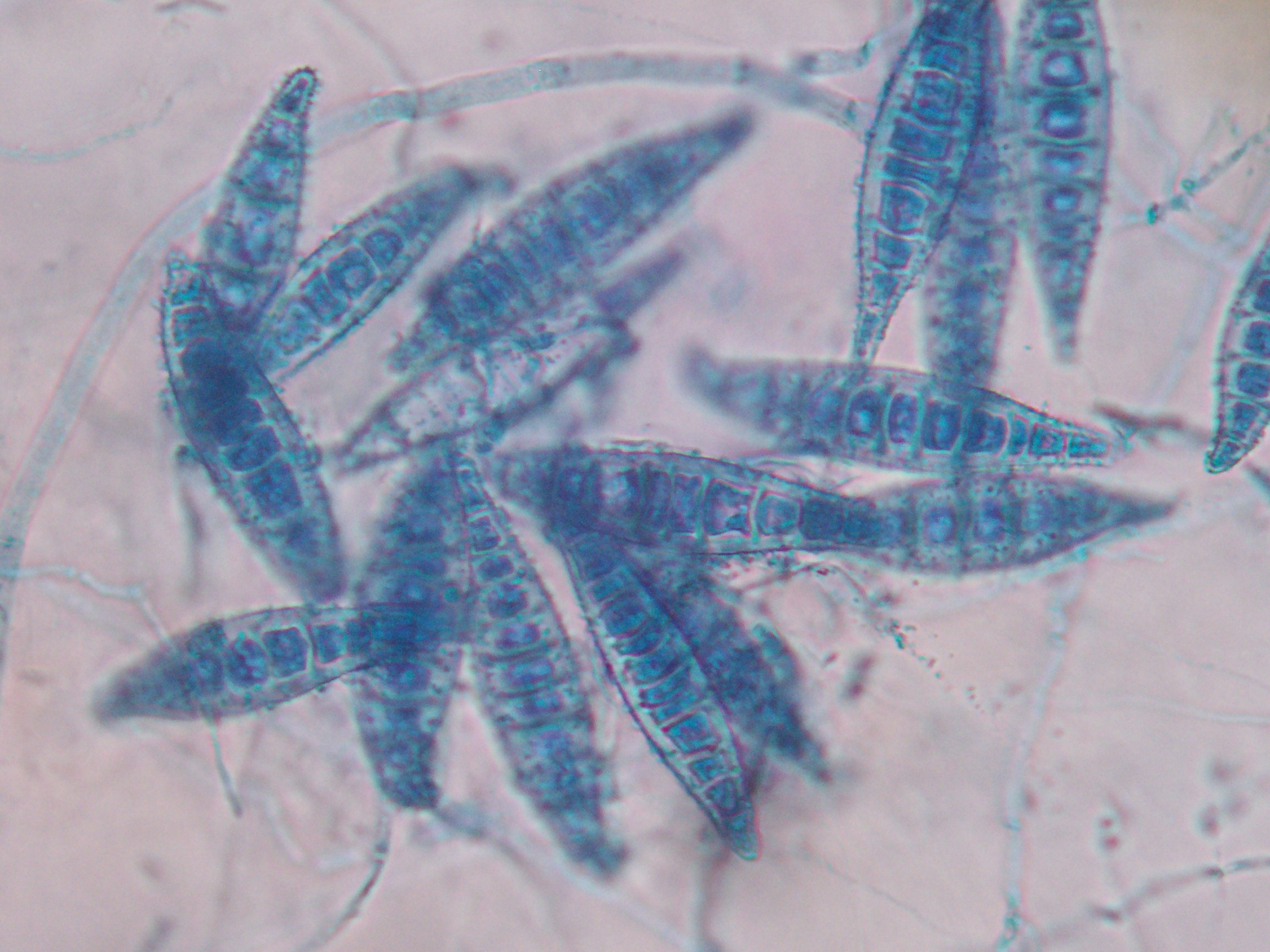
Dermatophytosis
different fungi can be the agent of this
Trichophyton
Epidermophyton
Microsporum
spore formation
Trichophyton
Epidermophyton
Microsporum
spore formation
19
New cards
Dermatophytosis: Disease
break down keratin surfaces (nails)
also can cause ringworm
hair shaft infections
also can cause ringworm
hair shaft infections
20
New cards
Trichophyton
what is this?
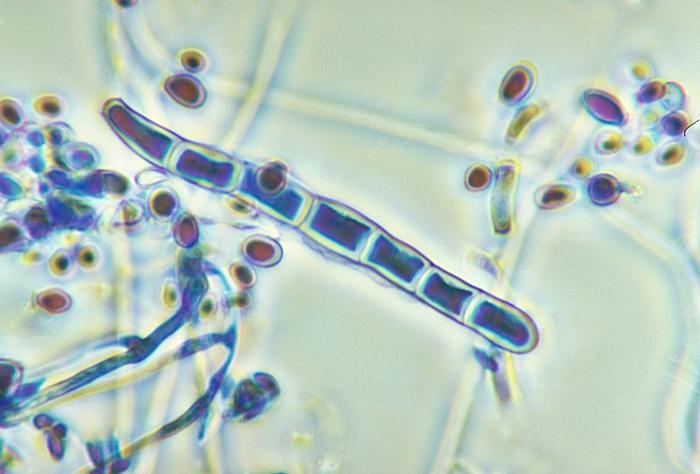
21
New cards
Epidermophyton
what is this?

22
New cards
Microsporum
what is this?
23
New cards
ectothrix
dermatophytosis infection outside hair shaft
24
New cards
endothrix
dermatophytosis infection inside hair shaft
25
New cards
favic
dermatophytosis infection in root of hair
26
New cards
Geophilic Transmission
(dermatophytosis)
(dermatophytosis)
soil (environment)
elicits strong immune response--> may clear infection
elicits strong immune response--> may clear infection
27
New cards
Zoophilic Transmission
(dermatophytosis)
(dermatophytosis)
animals (not humans)
elicits strong immune response--> may clear infection
elicits strong immune response--> may clear infection
28
New cards
Anthroponoses Transmission
(dermatophytosis)
(dermatophytosis)
human to human
doesn't elicit immune responses--> may cause chronic infections
need treatment
doesn't elicit immune responses--> may cause chronic infections
need treatment
29
New cards
Dermatophytosis: Treatment
problem can occur with location
antifungal (topical and oral)
natural resistance
antifungal (topical and oral)
natural resistance
30
New cards
Subcutaneous Mycoses
"deep skin"
31
New cards
Sporotrichosis
sporothrix schenckii
dimorphic fungus
dimorphic fungus
32
New cards
Dimorphic
grows as mold in environment
grows as yeast on skin/humans
grows as yeast on skin/humans
33
New cards
Sporotrichosis: Epidemiology
environmental (soil, vegetation)
animals (armadillo, cats)
geography (Japan, North and South America)
animals (armadillo, cats)
geography (Japan, North and South America)
34
New cards
Sporotrichosis: Disease
Primary site of infection- small nodule (may ulcerate)
Secondary site of infection- migration to draining lymph node
Secondary site of infection- migration to draining lymph node
35
New cards
Sporotrichosis: Transmission
wound contact with molds
-Environmental: forest work, mining, gardening (STICKS)
-Zoonotic: Armadillos, cats
-Environmental: forest work, mining, gardening (STICKS)
-Zoonotic: Armadillos, cats
36
New cards
Sporotrichosis: Treatment
self-limiting (very rare)
Potassium iodide: easy use and access
Antifungals
Potassium iodide: easy use and access
Antifungals
37
New cards
Sporotrichosis: Prevention
clothing, shoes
38
New cards
Chromoblastomycosis
can be cause by multiple genus/species
"wart like nodules"
"wart like nodules"
39
New cards
Chromoblastomycosis: Epidemiology
Environmental: soil, vegetation
Geography: tropics
Geography: tropics
40
New cards
Chromoblastomycosis: Disease
slow growing verrucous nodules or plaques
"wart-like"
-worried about secondary infections
"wart-like"
-worried about secondary infections
41
New cards
Chromoblastomycosis: Transmission
wound contact with molds
-environmental
-wear shoes!
-environmental
-wear shoes!
42
New cards
Chromoblastomycosis: Treatment
usually resistant to antifungals by the time it's detected
if untreated: chronic infection and squamous cell carcinoma (cell cycle messed up)
if untreated: chronic infection and squamous cell carcinoma (cell cycle messed up)
43
New cards
Chromoblastomycosis: Prevention
clothing, shoes
hands, arms, legs, feet
hands, arms, legs, feet
44
New cards
Eumycotic mycetoma
can be caused by multiple genus/species of fungi
"true fungi" infection
-certain bacteria can cause the same disease --> treatment differs based on bacteria
"true fungi" infection
-certain bacteria can cause the same disease --> treatment differs based on bacteria
45
New cards
Eumycotic mycetoma: Epidemiology
environmental: soil, vegetation
geography: tropics with low rainfall
geography: tropics with low rainfall
46
New cards
Eumycotic mycetoma: Disease
localized, chronic granulomatous tissue infection
destruction of muscle, fascia, and bone
destruction of muscle, fascia, and bone
47
New cards
Eumycotic mycetoma: Transmission
wound contact with molds (environmental)
48
New cards
Eumycotic mycetoma: Treatment
resistant to antifungals (may slow spread)
amputation
amputation
49
New cards
Eumycotic mycetoma: Prevention
clothing
50
New cards
Subcutaneous entomophthoromycosis
same order (Entomophthorales)
dimorphic
Conidiobolus coronatus
Basidiobolus ranarum
dimorphic
Conidiobolus coronatus
Basidiobolus ranarum
51
New cards
Subcutaneous entomophthoromycosis: Epidemiology
environmental: plant debris
geography: predominantly observed in Africa
- Middle East, Asia, Latin America also
geography: predominantly observed in Africa
- Middle East, Asia, Latin America also
52
New cards
Conidiobolus coronatus: Disease
mostly adults
facial (nasal cavity --> inhalation)
facial (nasal cavity --> inhalation)
53
New cards
Conidiobolus coronatus: Transmission
inhalation of spores into nasal cavity
54
New cards
Basidiobolus ranarum: Disease
mostly children
appendages (hands and knees primarily)
appendages (hands and knees primarily)
55
New cards
Basidiobolus ranarum: Transmission
wound contact with mold (crawling increases exposure)
56
New cards
Subcutaneous entomophthoromycosis: Treatment
potassium iodide
antifungals
antifungals
57
New cards
Subcutaneous entomophthoromycosis: Prevention
avoidance (both)
Masks (Conidiobolus coronatus)
Clothes (Basidiobolus ranarum)
Masks (Conidiobolus coronatus)
Clothes (Basidiobolus ranarum)
58
New cards
Subcutaneous phaeohyphomycosis
can be cause by multiple genus/species of fungi
infections can range from superficial, subcutaneous, deeply invasive (all three localized) to disseminated (systemic)
-want to diagnose as soon as possible
infections can range from superficial, subcutaneous, deeply invasive (all three localized) to disseminated (systemic)
-want to diagnose as soon as possible
59
New cards
Subcutaneous phaeohyphomycosis: Epidemiology
soil, wood, and decaying vegetation
60
New cards
Subcutaneous phaeohyphomycosis: Disease
paulonodules, verrucous, cysts, abscesses, hyper keratotic or ulcerated plaques, pyogranuloma, non-healing ulcers or sinuses
61
New cards
Subcutaneous phaeohyphomycosis: Transmission
wound contact with molds
-environmental: warm temp
-exposure, penetration of barrier
-environmental: warm temp
-exposure, penetration of barrier
62
New cards
Subcutaneous phaeohyphomycosis: Treatment
surgical excision
antifungals
the earlier the better
antifungals
the earlier the better
63
New cards
Subcutaneous phaeohyphomycosis: Prevention
clothing
64
New cards
Systemic Mycoses
whole body
dangerous to immunocompromised (rare)
masks --> prevent respiratory infections
all are dimorphic
Transmission via spore inhalation
dose and immune status major factors for severity
systemic map: know where the areas are higher risk
dangerous to immunocompromised (rare)
masks --> prevent respiratory infections
all are dimorphic
Transmission via spore inhalation
dose and immune status major factors for severity
systemic map: know where the areas are higher risk
65
New cards
Blastomycosis
Blastomyces dermatitidis
66
New cards
Blastomycosis: Epidemiology
decaying organic material
United States (MN to east coast minus FL)
United States (MN to east coast minus FL)
67
New cards
Blastomycosis: Disease
primary site of infection: pulmonary disease (
68
New cards
Blastomycosis: Transmission
environment: inhalation
-hits warm of respiratory tract, transformed to yeast, can get past the respiratory tract and become systematic
-hits warm of respiratory tract, transformed to yeast, can get past the respiratory tract and become systematic
69
New cards
Blastomycosis: Treatment
antifungal --> if caught early
70
New cards
Blastomycosis: Prevention
avoidance and masks
71
New cards
Coccidioides
Coccidioides (multiple species)
72
New cards
Coccidioides: Epidemiology
desert: enhancement with bat and rodent feces (Mexico and Africa)
South America
South America
73
New cards
Coccidioides: Disease (low dose)
-Make an immune response --> vaccinate themselves
-asymptomatic
-self-limiting pulmonary disease
-protective memory response
-asymptomatic
-self-limiting pulmonary disease
-protective memory response
74
New cards
Coccidioides: Disease (high dose/"other factors")
-other factors: state of respiratory tract
pulmonary disease: skin, soft tissue, bones, joint, and meninges
pulmonary disease: skin, soft tissue, bones, joint, and meninges
75
New cards
Coccidioides: Disease (other)
Immunocompromised: high doses can be lethal
Other factors: ethnicity, age- elderly, gender- higher effect in men, Pregnancy- late or postpartum, hormones play a role
Other factors: ethnicity, age- elderly, gender- higher effect in men, Pregnancy- late or postpartum, hormones play a role
76
New cards
Coccidioides: Transmission
dimorphic
inhalation
inhalation
77
New cards
Coccidioides: Treatment
antifungals (those with risk factors)
-normally, a healthy individual can fight it off themselves
-normally, a healthy individual can fight it off themselves
78
New cards
Coccidioides: Prevention
avoidance, masks
79
New cards
Histoplasmosis
Histoplasmosis capsulati
Histoplasmosis duboisii
Histoplasmosis duboisii
80
New cards
Histoplasmosis: Epidemiology
caves, decaying buildings (bat and bird feces)
81
New cards
Histoplasmosis capsulati: Disease
North America
low dose --> asymptomatic
high dose --> pulmonary : systemic-scaring
low dose --> asymptomatic
high dose --> pulmonary : systemic-scaring
82
New cards
Histoplasmosis duboisii: Disease
Africa
low dose --> asymptomatic
high dose --> pulmonary : skin and bone
low dose --> asymptomatic
high dose --> pulmonary : skin and bone
83
New cards
Histoplasmosis: Transmission
inhalation
84
New cards
Histoplasmosis: Treatment
antifungals --> chronic infections
most individuals will be able to fight off
most individuals will be able to fight off
85
New cards
Histoplasmosis: Prevention
avoidance and masks
86
New cards
Paracoccidiodidomycosis
Paracoccidiodidomycosis brasiliensis
dimorphic
dimorphic
87
New cards
Paracoccidiodidomycosis: Epidemiology
Brazil
??? no one knows
soil?
??? no one knows
soil?
88
New cards
Paracoccidiodidomycosis: Disease
pulmonary infection: inseminate to skin, mucosa, CNS, bones (if untreated)
-ulceration of mouth, lips, gums, and palate
At risk: Children (10-19), Men (30-50)
-estrogen inhibits mold --> yeast transformation
Asymptomatic
-Dormant--> reactivation
-ulceration of mouth, lips, gums, and palate
At risk: Children (10-19), Men (30-50)
-estrogen inhibits mold --> yeast transformation
Asymptomatic
-Dormant--> reactivation
89
New cards
Paracoccidiodidomycosis: Transmission
respiratory --> inhalation with humidity
may also include traumatic inculcation (penetration of barrier)
may also include traumatic inculcation (penetration of barrier)
90
New cards
Paracoccidiodidomycosis: Treatment
antifungals
chronic infection --> long term treatment
chronic infection --> long term treatment
91
New cards
Paracoccidiodidomycosis: Prevention
avoidance and masks
92
New cards
Talaromycosis
talaromycosis marneffei
93
New cards
Talaromycosis: Epidemiology
south east Asia
??? don't know
bamboo roots? soil?
??? don't know
bamboo roots? soil?
94
New cards
Talaromycosis: Disease
only in immunocompromised: mimics TB, leishmaniasis, histoplasmosis, cryptococcus (AIDS related opportunistic infections)
-hard to diagnose/detect --> lead to wrong diagnosis --> improper treatment
Pulmonary infection: skin lesions
-hard to diagnose/detect --> lead to wrong diagnosis --> improper treatment
Pulmonary infection: skin lesions
95
New cards
Talaromycosis: Transmission
unknown because source is unknown (inhalation?)
96
New cards
Talaromycosis: Treatment
antifungals
-difficult to determine when to use if diagnosis is misidentified
-difficult to determine when to use if diagnosis is misidentified
97
New cards
Talaromycosis: Prevention
avoidance and masks
98
New cards
Fungi: non-infections
mycotoxins
-exotoxins: produced by certain fungi
-through inhalation, ingestion, or contact
-notable mycotoxins
-exotoxins: produced by certain fungi
-through inhalation, ingestion, or contact
-notable mycotoxins
99
New cards
Alfatoxins: Source
corn, nuts (can be aerosolized)
100
New cards
Alfatoxins: Disease
-carcinogen (activates proto-oncogenes)
-associated with hepatitis and other liver problems
-associated with hepatitis and other liver problems