Bones & Skeletal Tissue: Nutrients, Hormones, and Growth Processes
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
What nutrients are essential for bone health?
Calcium and Vitamin D
How does Vitamin D affect calcium absorption?
Dietary calcium absorption requires Vitamin D.
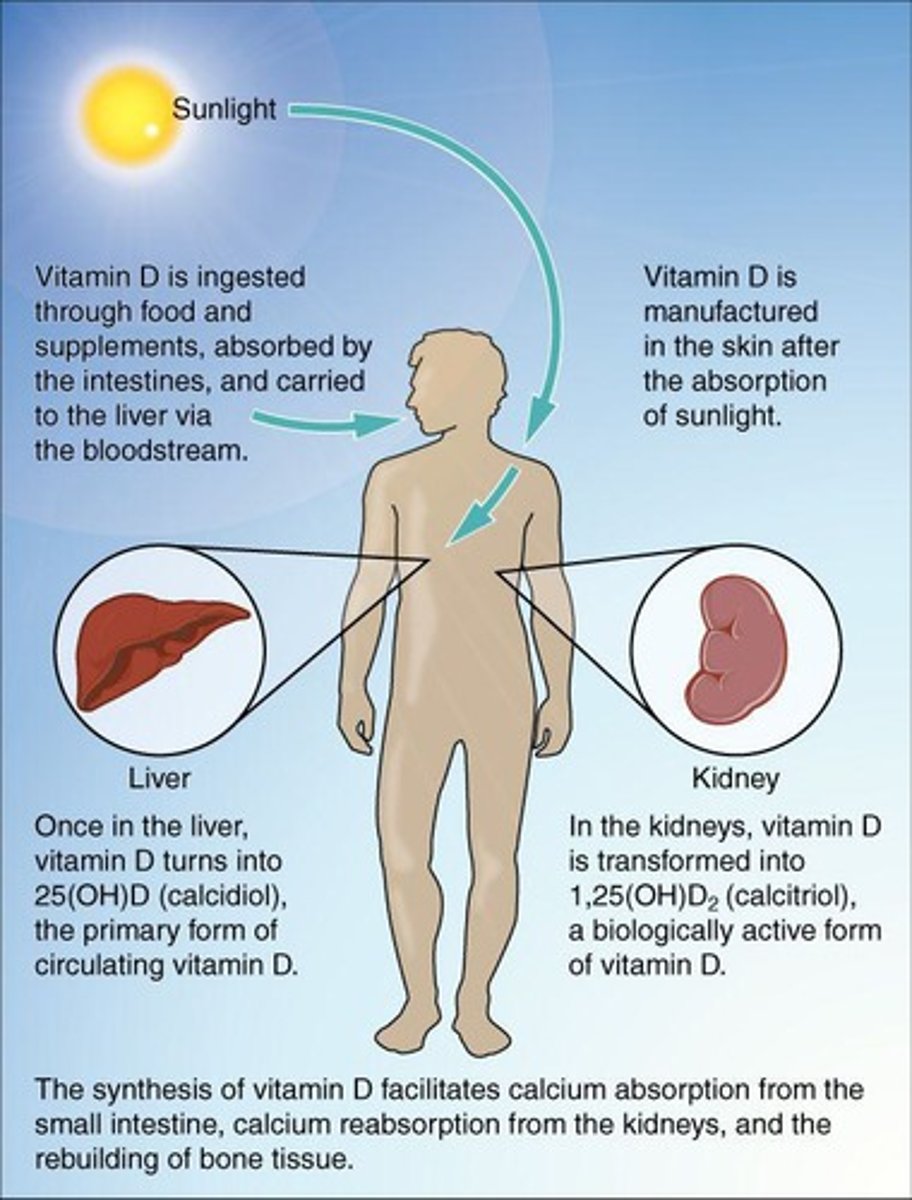
What are some dietary sources of Vitamin D?
Fatty fish like salmon and tuna, fortified milk or cereal.
What is calcium homeostasis?
The process of maintaining stable calcium levels in the body.
What are the functions of calcium in the body?
Nerve impulse transmission, muscle contraction, blood coagulation, secretion by glands and nerve cells, cell division.
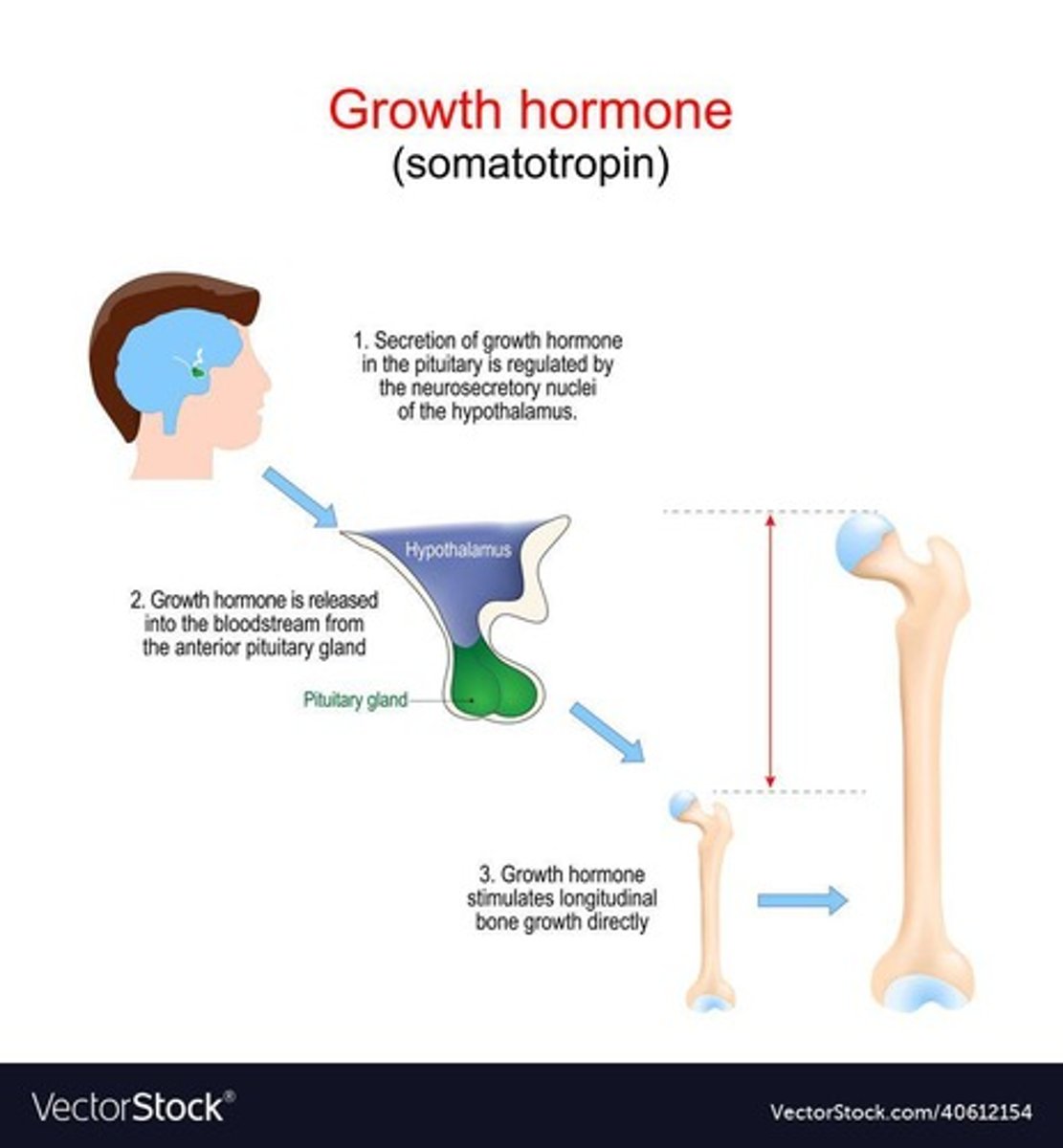
What role does growth hormone play in bone health?
Stimulates epiphyseal plate activity in infancy and childhood.
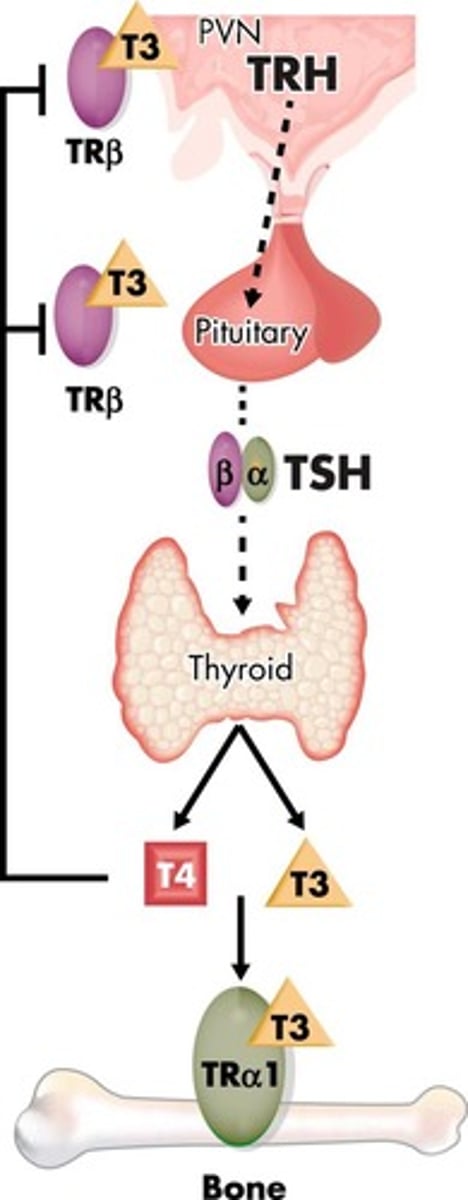
How does thyroid hormone affect bone development?
Modulates growth hormone activity and promotes osteoblast activity.
What is the effect of sex hormones on bone?
Promote osteoblastic activity and are responsible for the adolescent growth spurt.
What happens to bone health with excess or deficit of hormones?
Causes abnormal skeletal growth, such as acromegaly.
What is the function of parathyroid hormone (PTH) in calcium regulation?
Stimulates osteoclasts and removes calcium from bone.
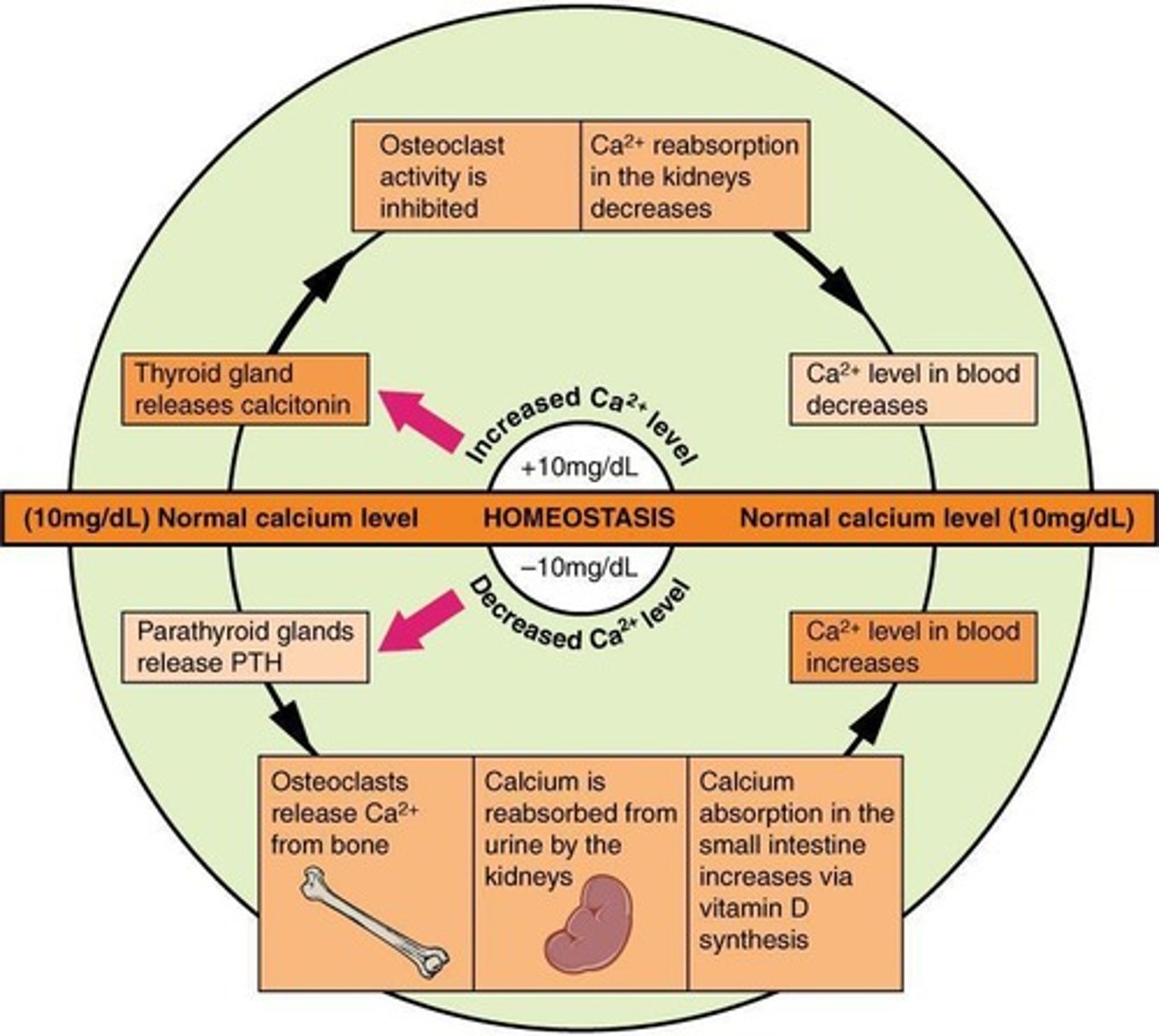
What is the role of calcitonin?
Lowers blood calcium levels temporarily.
What are the effects of hypocalcemia?
Clotting disorders, heart arrhythmias, brittle bones.
What are the effects of hypercalcemia?
Sluggish nerve responses and calcium deposits in blood vessels and kidneys.
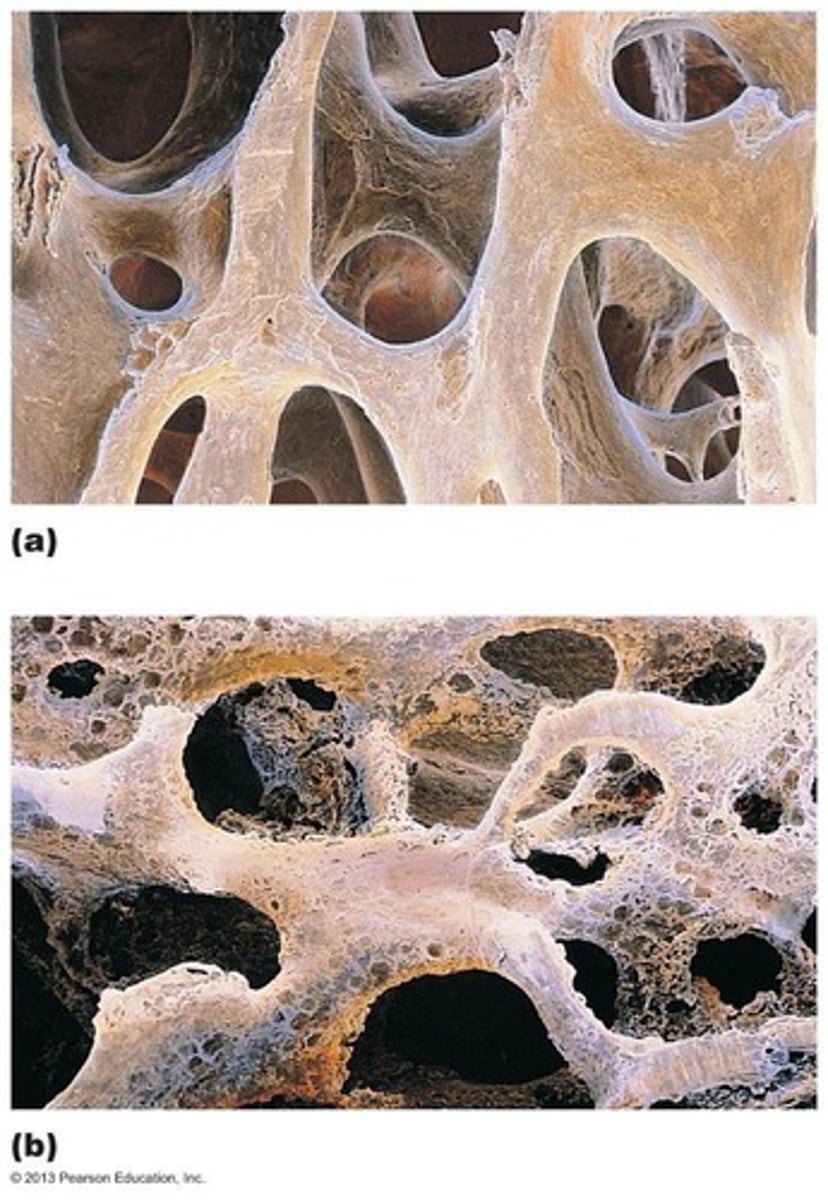
What is osteoporosis?
Condition where bone resorption outpaces deposit, leading to fragile bones.
What are common risk factors for osteoporosis?
Age, sex, smoking, immobility.
What is rickets?
Condition characterized by bowed legs and bone deformities due to Vitamin D deficiency or insufficient dietary calcium.
How does serotonin affect bone density?
Interferes with osteoblast activity, potentially lowering bone density.
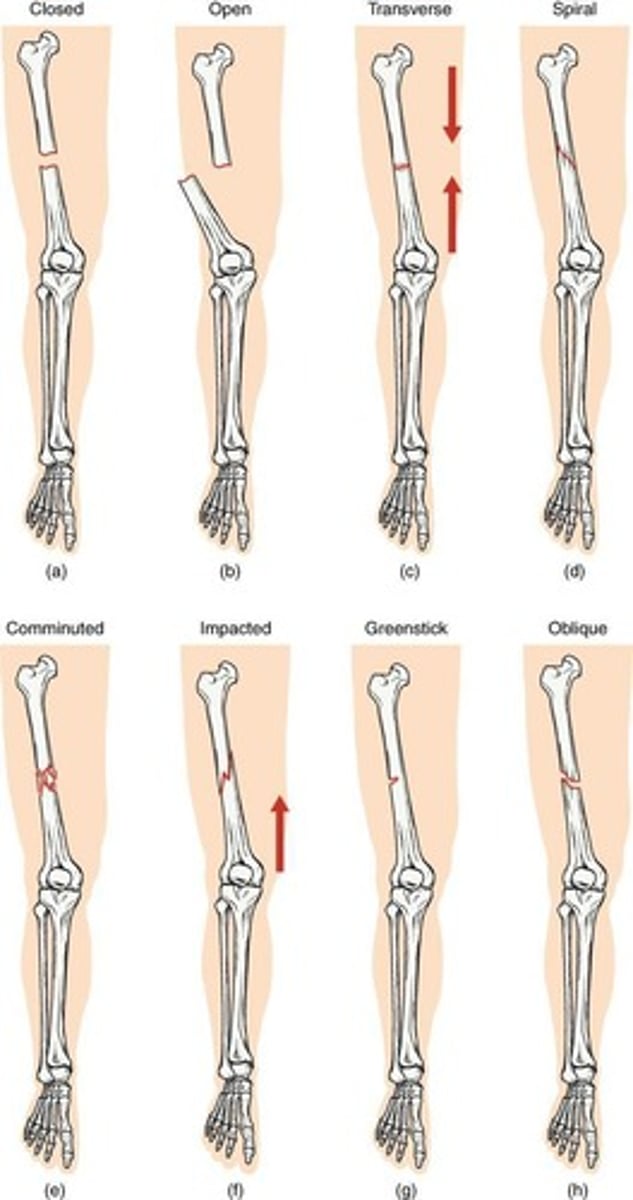
What are the classifications of fractures?
Based on location, severity, completeness (complete/incomplete), and whether the skin is penetrated (open/closed).
What is the first stage of bone repair?
Hematoma formation.
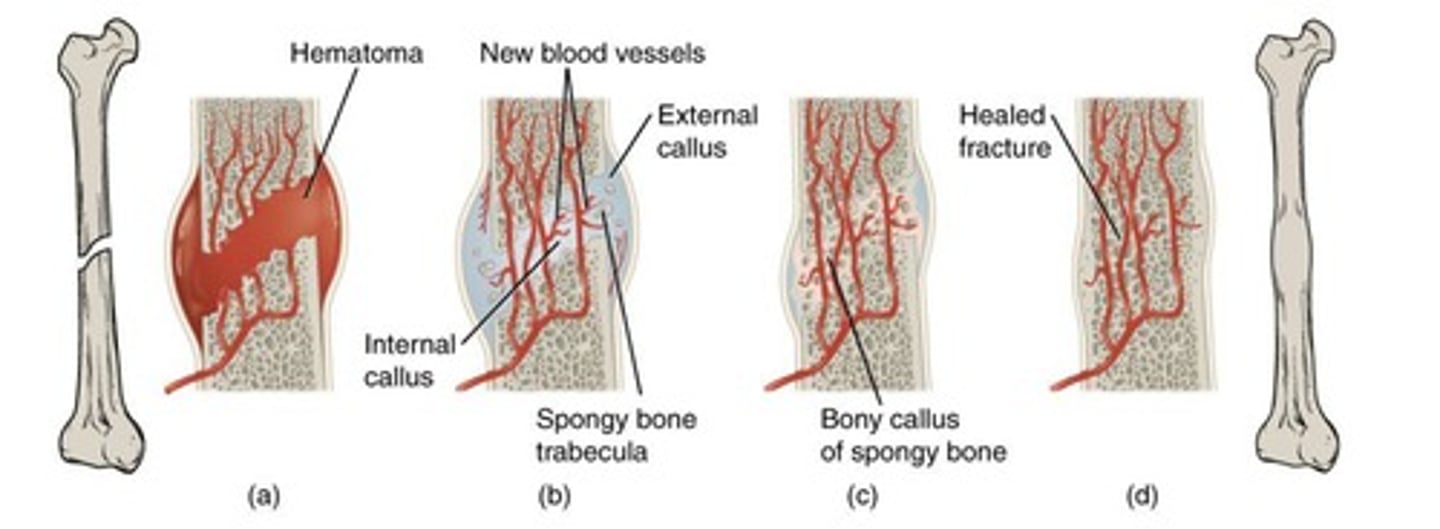
What follows hematoma formation in bone repair?
Fibrocartilaginous callus formation.
What is the third stage of bone repair?
Bony callus formation.
What is the final stage of bone repair?
Bone remodeling.
What is intramembranous ossification?
A process where bones are formed directly as bone, primarily in facial and most cranial bones.
What is endochondral ossification?
A process where bone replaces a hyaline cartilage template, occurring in all bones below the head except the clavicle.
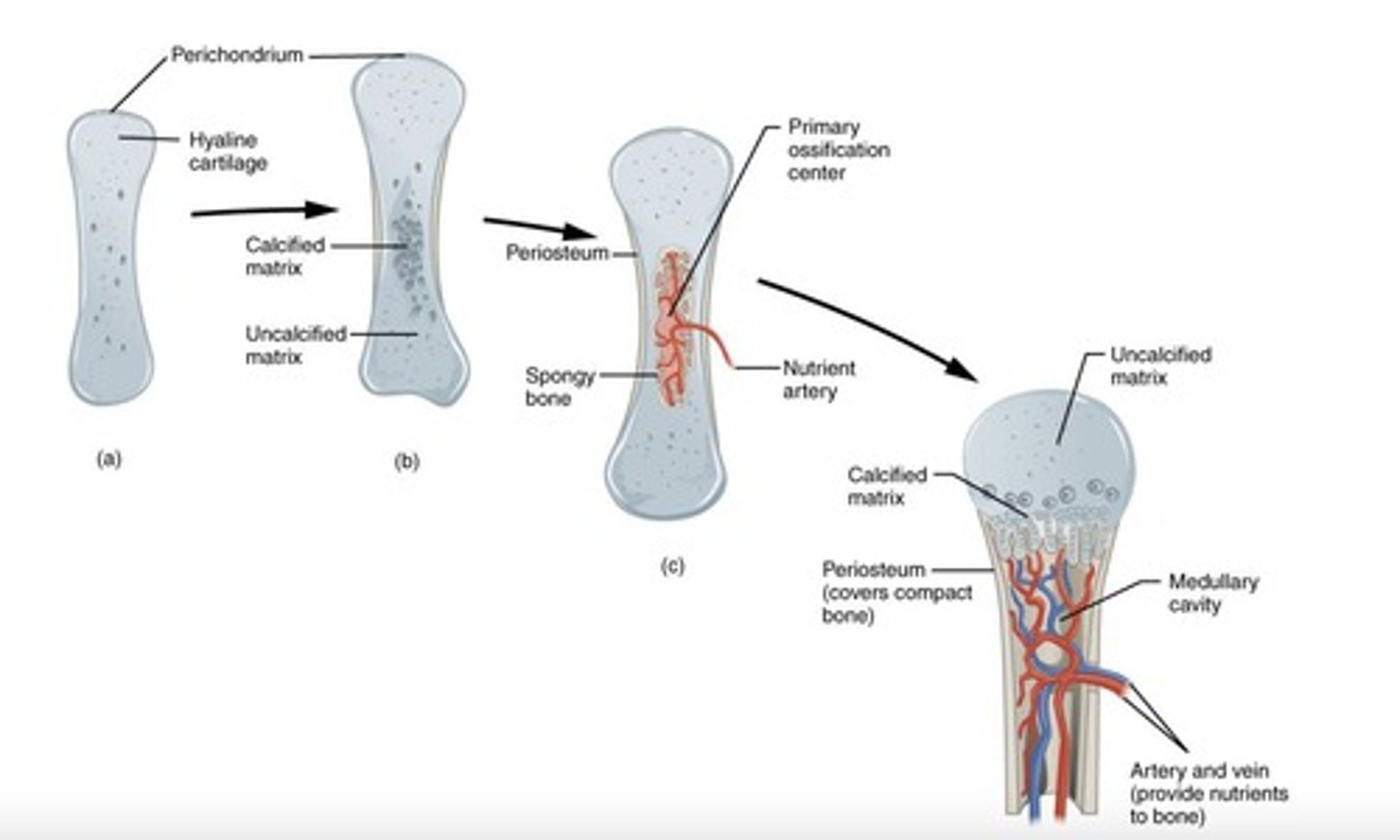
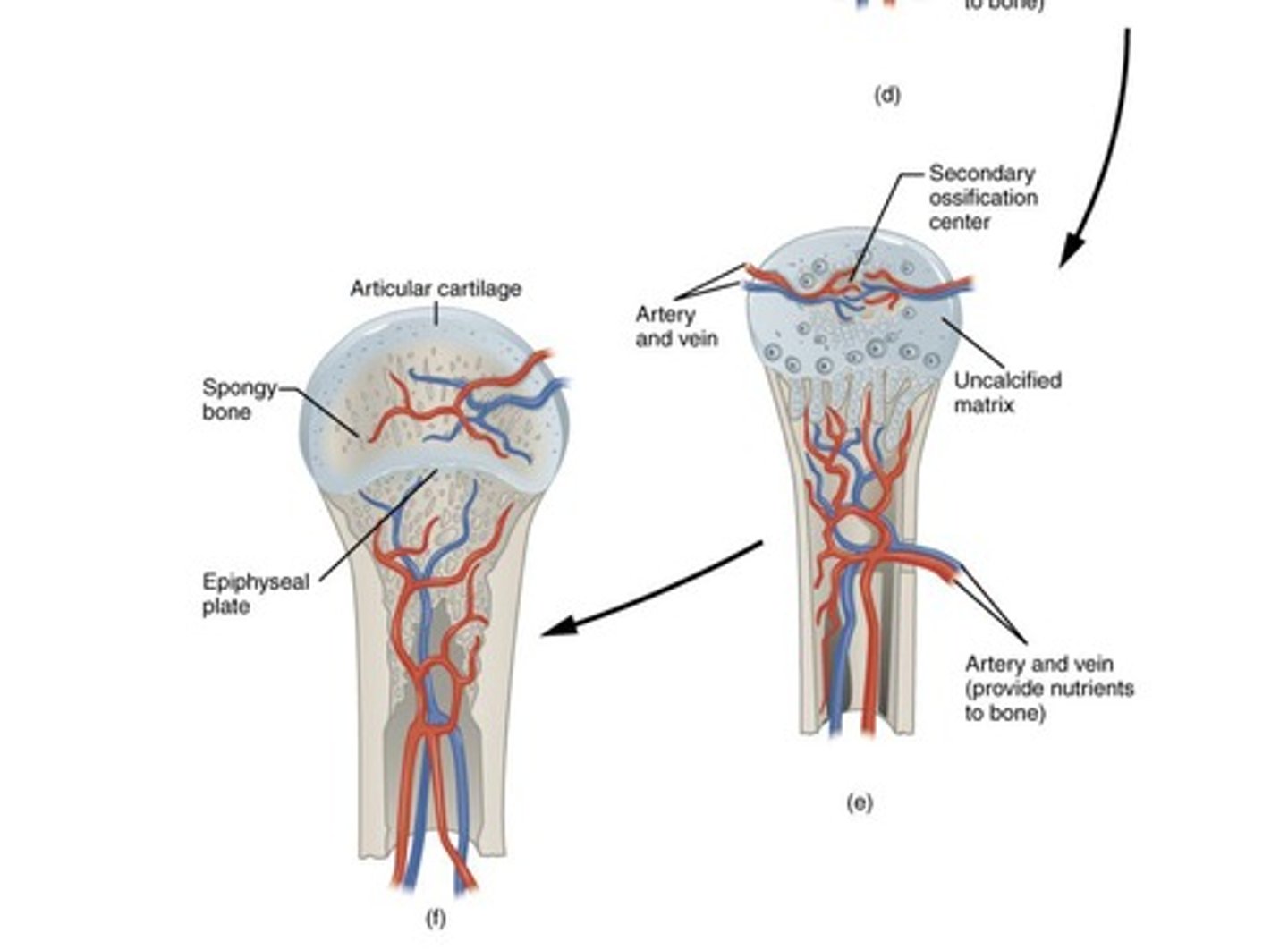
What are the steps of endochondral ossification?
1. Mesenchymal cells differentiate into chondrocytes to form the cartilage model. 2. The cartilage model and perichondrium form. 3a. Capillaries penetrate cartilage; perichondrium transforms into periosteum. 3b. Primary ossification center develops. 4. Cartilage and chondrocytes grow at bone ends. 5. Secondary ossification centers develop; cartilage remains at epiphyseal plate and joint surfaces.
What are the steps of intramembranous ossification?
1. Mesenchymal cells differentiate into osteoblasts, forming ossification centers. 2. Secreted osteoid traps osteoblasts, which become osteocytes. 3. Trabecular matrix and periosteum form. 4. Compact bone develops above trabecular bone, and blood vessels condense into red marrow.
What is the growth activity at the epiphyseal plate?
It involves the balance of cartilage growth on one side and bone replacement on the other, maintaining constant thickness.
What are the five zones of postnatal bone growth at the epiphyseal plate?
1. Resting (quiescent) zone 2. Proliferation (growth) zone 3. Hypertrophic zone 4. Calcification zone 5. Ossification (osteogenic) zone.
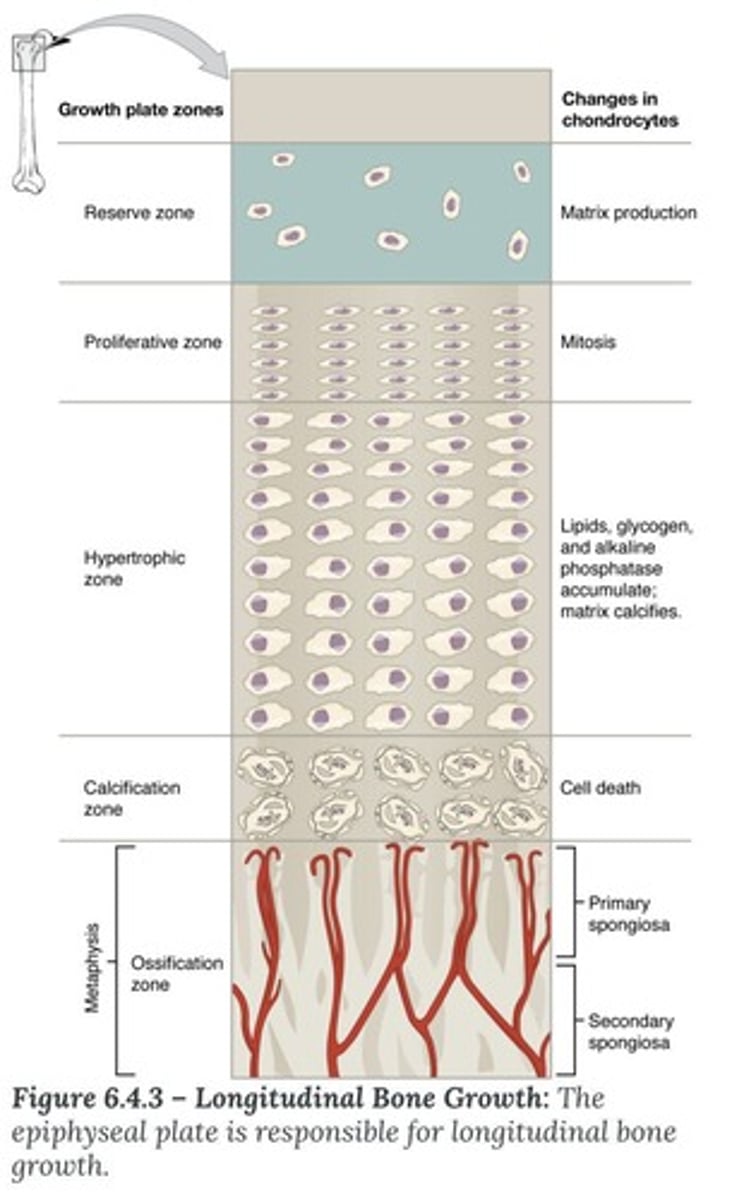
What occurs in the resting (quiescent) zone of the epiphyseal plate?
This zone contains inactive cartilage cells that serve as a reserve for future growth.
What happens in the proliferation (growth) zone?
Cartilage cells undergo mitosis, contributing to bone lengthening.
What characterizes the hypertrophic zone?
Older cartilage cells enlarge, preparing for calcification.
What occurs in the calcification zone?
The matrix calcifies, cartilage cells die, and blood vessels invade the area.
What happens in the ossification zone?
Osteoblasts deposit bone matrix, completing the bone formation process.
What is epiphyseal plate closure?
The process where bone lengthening ceases, and the epiphysis fuses with the diaphysis, occurring around age 18 for females and 21 for males.
What is bone remodeling?
The process where adjacent osteoblasts and osteoclasts work together to recycle bone mass, with adults recycling 5-10% of bone mass each year.
What role do osteoclasts play in bone remodeling?
They secrete enzymes that digest the bone matrix and convert calcium salts to soluble forms, phagocytizing demineralized matrix and dead osteocytes.
What is the significance of the epiphyseal plate in postnatal bone growth?
It allows for the lengthening of long bones through the balance of cartilage growth and bone replacement.
What might account for differences in leg length after a fracture at the epiphyseal plate?
If the epiphyseal plate is damaged, it may lead to uneven growth, resulting in one leg being longer than the other.
How can x-rays determine if a person has reached full height?
X-rays can show whether the epiphyseal plates have closed, indicating that no further lengthening of the bones will occur.
What are the main differences between modeling and remodeling of bones?
Modeling refers to the formation of new bone, while remodeling involves the recycling and maintenance of existing bone.
What is the role of osteocytes in bone health?
Osteocytes maintain bone tissue and communicate with other bone cells to regulate bone remodeling.
What is the trabecular matrix?
A spongy bone structure that forms during intramembranous ossification, providing support and housing red marrow.