StemUp: OCR A A level Biology 5.1.2 Excretion as an example of homeostatic control
1/96
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
97 Terms
What is excretion? (1)
The removal of the waste products of metabolism from the body
What are the main metabolic waste products in the body? (3)
- CO2
- Bile pigments
- Nitrogenous waste
How is CO2 formed and excreted? (2)
- Waste product of respiration
- Excreted by the lungs (too much CO₂ in the blood is toxic)
How are bile pigments formed and excreted? (2)
- From the breakdown of haemoglobin in the liver
- Excreted into the small intestine via the gall bladder and bile duct
How are nitrogenous waste (urea) formed and excreted? (2)
- Formed from the breakdown of excess amino acids in the liver
- Excreted by the kidneys in urine
What are the main veins, arteries, and ducts associated with the liver? (4)
- Hepatic artery: Supplies the liver with oxygenated blood for respiration (producing ATP)
- Hepatic vein: Takes deoxygenated blood away from the liver
- Hepatic portal vein: Brings blood from the duodenum and ileum, containing the products of digestion
- Bile duct: Takes bile to the gall bladder for storage; bile emulsifies fats
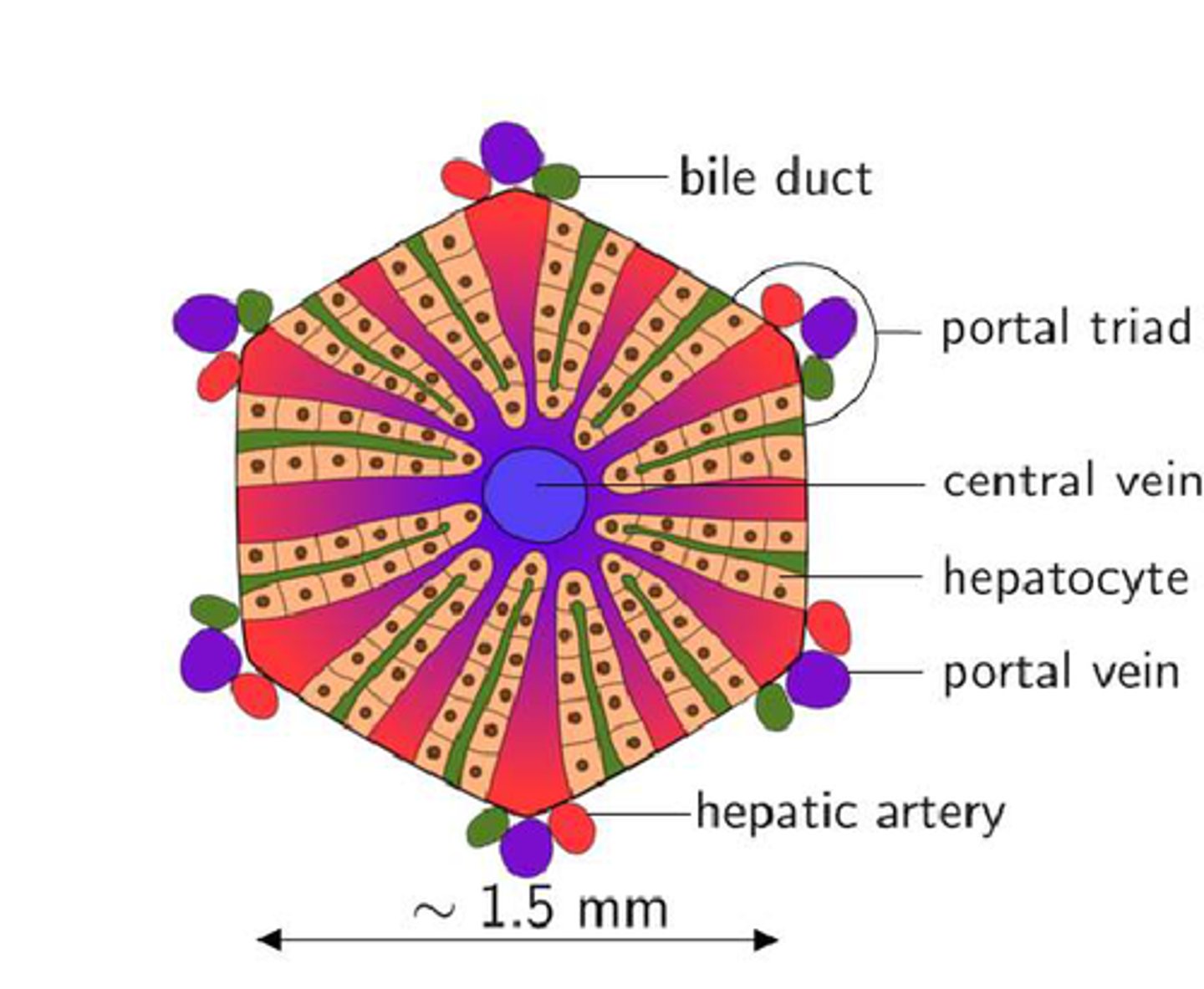
What is the structure of the liver? (4)
- The liver is made up of cylindrical structures called liver lobules
- Composed of hepatocytes arranged in rows radiating from the center
- Each lobule has a central vein connected to the hepatic vein
- Branches of the hepatic artery, hepatic portal vein, and bile duct connect to each lobule
How do the hepatic artery and hepatic portal vein connect to the central vein? (3)
- Through capillaries called sinusoids
- Blood flows through the sinusoids past hepatocytes
- Which remove harmful substances and oxygen from the blood
What role do hepatocytes play in liver function? (3)
- Hepatocytes remove harmful substances from the blood
- Breaking them down into less harmful substances
- Which then re-enter the blood
What is the function of Kupffer cells in the liver? (2)
- Kupffer cells are attached to the sinusoids
- Remove bacteria and break down old red blood cells
How is bile transported in the liver? (2)
- The bile duct is connected to the central vein by tubes called canaliculi
- Which transport bile
Draw and label a diagram of the structure of a liver lobule (7)
How does the liver contribute to carbohydrate metabolism? (3)
- When blood glucose levels rise
- Insulin stimulates hepatocytes to convert glucose to glycogen for storage
- Which can later be converted back when glucose is needed for energy
How is excess protein converted into urea? (5)
1. Protein is converted into amino acids
2. Excess amino acids undergo deamination
3. Ammonia is formed
4. Ammonia is converted into urea in the ornithine cycle
5. Urea is released into the blood and excreted by the kidneys in urine
What is deamination? (2)
- Process where the nitrogen-containing amino groups are removed from excess amino acids
- Producing ammonia and organic acids
Why is deamination necessary? (2)
- The organic acids can be respired for ATP production
- Or stored as glycogen
Why is ammonia converted into urea in the liver? (3)
- Ammonia is too toxic for mammals to excrete directly
- So it is combined with CO₂ in the ornithine cycle to form urea
- Which is less harmful and can be excreted
How does the liver detoxify harmful substances like alcohol? (2)
- The liver breaks down alcohol (ethanol) into ethanal
- Which is then broken down into acetic acid, a less harmful substance
What can prolonged alcohol consumption lead to? (2)
- Cirrhosis
- Where liver cells die, and scar tissue blocks blood flow
How does the liver process paracetamol? (2)
- Paracetamol is broken down by the liver
- Excess amounts can lead to liver and kidney failure
How does the liver regulate insulin? (2)
- The liver breaks down excess insulin
- Preventing problems with blood glucose concentration
What is the large white circular shape seen in a stained sample of liver tissue under a light microscope? (1)
Central vein
What are the cells that radiate out from the central vein in a liver tissue sample? (2)
- Hepatocytes
- The red dots inside the cells are the nuclei
What are the white spaces between the cells in a stained liver tissue sample? (1)
Sinusoids
Draw and label the structure of a nephron (10)
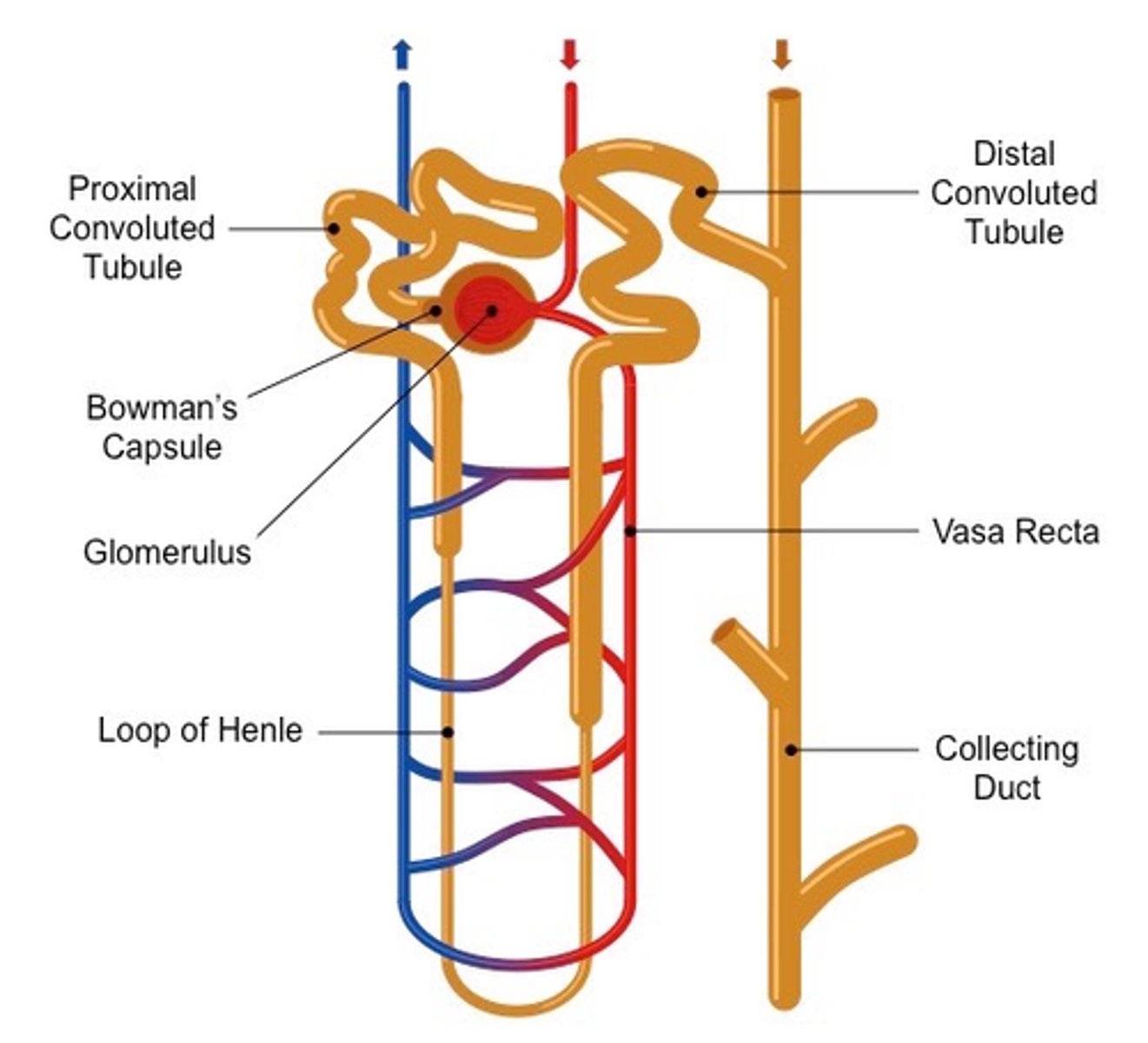
What is the nephron and its role in the kidney? (2)
- Filtering unit of the kidney
- Responsible for filtering blood and producing urine
What is the Bowman's capsule in the nephron? (3)
- Structure in nephron
- That contains a knot of blood vessels - glomerulus
- Involved in the filtration of blood
What are podocytes in the nephron? (2)
- Specialised cells that make up the inner layer of the Bowman's capsule
- Wrap around the capillaries of the glomerulus
What are the main structures of the nephron in sequence? (5)
1. Bowman's capsule
2. Proximal convoluted tubule (PCT)
3. Loop of Henle
4. Distal convoluted tubule (DCT)
5. Collecting duct
What are the two main functions of the kidney? (2)
- To excrete waste products, such as urea
- To regulate water potential in the body
What is ultrafiltration, and where does it occur in the kidney? (2)
- Process by which substances are filtered out of the blood under high pressure in the glomerulus
- Into the Bowman's capsule
Why is the blood in the glomerulus under high pressure? (2)
- The afferent arteriole (bringing blood into the glomerulus) is wider than the efferent arteriole (carrying blood away)
- Creating high pressure
What are the three layers that substances must pass through during ultrafiltration? (3)
- The capillary wall.
- The basement membrane
- The epithelium of the Bowman's capsule
Why can't proteins and blood cells pass through the basement membrane during ultrafiltration? (2)
- Proteins and blood cells are too large to pass through the basement membrane
- So they remain in the blood
What happens to the liquid and small molecules that pass through the Bowman's capsule? (3)
- The liquid and small molecules, now called filtrate
- Pass along the nephron, and useful substances are reabsorbed along the way
- The remaining filtrate flows through the collecting duct and exits the kidney through the ureter
What is selective reabsorption, and where does it take place? (3)
- The process where useful substances (e.g., glucose)
- Are reabsorbed back into the blood from the filtrate
- As it flows through the PCT, loop of Henle, and DCT in the medulla and cortex of the kidney
What are the adaptations of the epithelial cells lining the PCT for selective reabsorption? (4)
- Microvilli
- Provide a large surface area for reabsorption
- Many mitochondria
- Provide ATP for active transport
How are useful solutes reabsorbed during selective reabsorption? (3)
- Glucose, amino acids, vitamins, and some salts are reabsorbed along the PCT
- By active transport and facilitated diffusion
- Some urea is reabsorbed by diffusion
How is water reabsorbed during selective reabsorption? (2)
- Water enters the blood by osmosis because the water potential of the blood is lower than the filtrate
- Water is reabsorbed from the loop of Henle, DCT, and collecting duct
What does the filtrate that remains in the nephron become, and what does it consist of? (5)
- Becomes urine that consists of
- Water.
- Dissolved salts
- Urea
- Hormones and excess vitamins
What substances are not found in urine in a healthy person, and why? (4)
- Proteins and blood cells
- Too large to pass through the basement membrane
- Glucose, amino acids, and vitamins
- Selectively reabsorbed back into the blood
What happens to the unwanted substances that remain in the filtrate? (3)
1. They pass through the tubules
2. Along the ureter to the bladder
3. Are expelled as urine
How does the filtered blood leave the kidneys? (1)
The filtered blood passes out of the kidneys through the renal vein
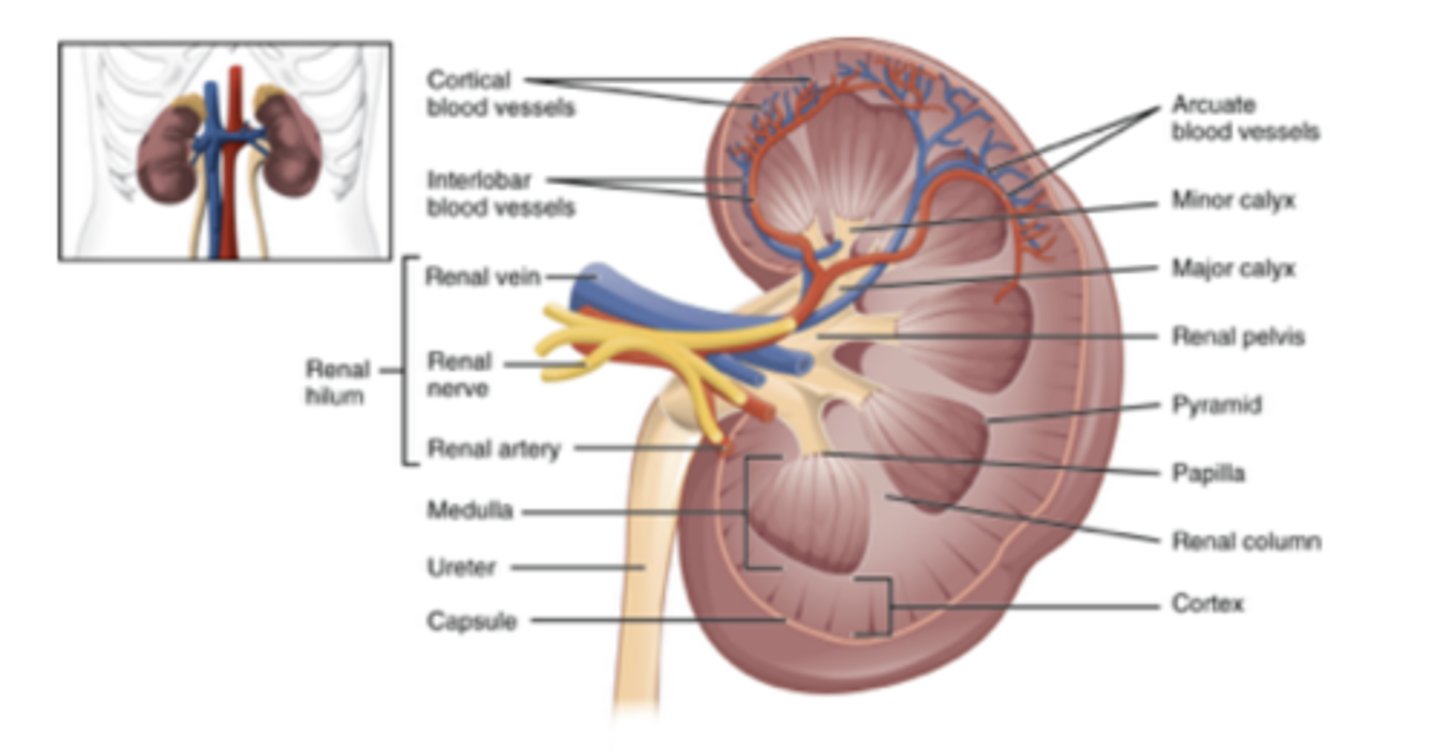
What covers the outside of the kidney? (2)
- Thin, strong membrane
- Renal capsule
What lies beneath the renal capsule in the kidney? (1)
Cortex
What is the indented part of the kidney called? (1)
Renal hilum
What structures come out of the renal hilum? (3)
- Renal vein
- Renal artery
- Ureter
How can you differentiate the renal artery, renal vein, and ureter during external examination? (2)
- The renal artery has a thicker wall than the vein
- The ureter is likely to have the most adipose (fatty) tissue around it
What does the cortex of the kidney look like during an internal examination? (1)
Appears dense, grainy, and darker than the medulla
What structures are found in the medulla of the kidney, and what do they look like? (3)
- Renal pyramids
- Cone-shaped structures that appear stripy
- Because they contain straight sections of the nephron (loop of Henle and collecting ducts).
What structures lead from the base of the renal pyramids? (3)
- Renal calyces
- Hollow cavities that lead to the larger renal pelvis
- Which connects to the ureter
What can you see when examining a stained section of the cortex of the kidney? (3)
- Glomerulus: Bundles of capillaries
- Bowman's capsule: A white area around the glomerulus
- PCTs and DCTs: Circular areas surrounded by squamous epithelial cells
What can you see when examining a stained section of the medulla of the kidney? (2)
- Loops of Henle: White areas surrounded by capillaries
- Red dots in the capillaries represent red blood cells
Draw and label a structure of a kidney (10)
What can you observe when examining the cortex of a stained section of the kidney? (3)
- Glomerulus
- Bowman's capsule
- PCTs and DCTs: Circular areas surrounded by squamous epithelial cells
What is the countercurrent multiplier mechanism, and how does it help reabsorb water? (4) - part 1
1. Loop of Henle acts as a countercurrent multiplier
2. Na⁺ and Cl⁻ ions are actively transported out of the ascending limb into the medulla (the ascending limb is impermeable to water)
3. This creates a low water potential in the medulla
4. Water moves out of the descending limb (which is permeable to water) by osmosis into the medulla
What is the countercurrent multiplier mechanism, and how does it help reabsorb water? (3) - part 2
1. The filtrate becomes more concentrated as ions cannot leave the descending limb
2. Water in the medulla is reabsorbed into the blood through the capillary network
3. Na⁺ and Cl⁻ ions diffuse out near the bottom of the ascending limb, further lowering the medulla's water potential
How does the collecting duct contribute to water reabsorption? (2)
- The water potential gradient created in the medulla causes water to move out of the collecting duct by osmosis
- This water is reabsorbed into the blood via the capillary network
How is the volume of water reabsorbed into the capillaries controlled? (1)
By changing the permeability of the DCT and the collecting duct
How does the length of the loop of Henle affect water reabsorption? (3)
- A longer loop of Henle allows more sodium and chloride ions to be actively pumped out
- Creating a greater water potential gradient in the medulla
- This allows more water to be reabsorbed by osmosis, resulting in more concentrated urine
Why do animals living in dry environments have longer loops of Henle? (2)
- Longer loops of Henle provide a more extended countercurrent multiplier
- Allowing for greater water reabsorption and the production of very concentrated urine
Explain the role of the loop of Henle in the production of urine (4) - part 1
1. The loop of Henle acts as a countercurrent multiplier
2. It establishes a water potential gradient in the medulla
3, Sodium and chloride ions are actively transported out of the ascending limb into the medulla
4. The walls of the descending limb are permeable to water
Explain the role of the loop of Henle in the production of urine (3) - part 2
1. Water moves out of the descending limb by osmosis
2. The water potential of the tissues surrounding the collecting duct is lower than the filtrate inside it
3. Water is removed from the filtrate in the collecting duct, and the remaining fluid becomes urine
What is osmoregulation? (2)
- The process by which the hypothalamus controls the water potential of the blood,
- An example of homeostasis and negative feedback
How is osmoregulation related to water reabsorption? (2)
- Water reabsorption occurs via the countercurrent multiplier mechanism
- The amount of water reabsorbed is controlled at this stage (by osmoregulation)
How do osmoreceptors in the hypothalamus respond to dehydration? (5)
1. When water levels in the blood decrease, osmoreceptors in the hypothalamus shrink
2. Triggering the release of ADH from the posterior pituitary gland
3. ADH increases the number of aquaporins in the DCT and collecting duct
4. Making them more permeable to water, so more water is reabsorbed into the blood
5. This results in less water being lost in urine and the production of small amounts of concentrated urine
How do osmoreceptors in the hypothalamus respond to over-hydration? (5)
1. When water levels in the blood increase, the hypothalamus detects this through osmoreceptors
2. The posterior pituitary gland releases less ADH, reducing the number of aquaporins in the DCT and collecting duct
3. Making them less permeable to water
4. Less water is reabsorbed
5. Resulting in more water lost in urine and the production of a large volume of dilute urine
What is kidney failure? (1)
Occurs when the kidneys cannot carry out their normal functions properly
How can kidney failure be detected? (3)
- Can be detected by measuring the glomerular filtration rate (GFR)
- Which is the volume of blood filtered by the kidneys over time
- A blood test for creatinine levels is used to estimate GFR
What does a high creatinine concentration in the blood indicate? (2)
- A high creatinine concentration indicates reduced kidney function due to low GFR
- Meaning the kidneys are not working properly
What factors affect GFR measurements? (2)
- GFR decreases steadily with age
- Men tend to have higher muscle mass than women, which increases creatinine levels
What are the causes of kidney failure? (4)
- Kidney infections
- Inflammation damages kidney cells, interfering with filtration and reabsorption
- High blood pressure
- Damages the glomeruli, allowing large molecules like proteins to enter urine
What is the consequence of the accumulation of waste products in kidney failure? (2)
- Accumulation of waste products
- Like urea leads to symptoms such as weight loss and vomiting
How does fluid retention affect the body during kidney failure? (2)
- Fluid retention causes swelling in the legs, face, and abdomen
- As the kidneys are unable to remove excess water from the blood
Why does kidney failure lead to high blood pressure? (2)
- High blood pressure results from the kidneys' inability to regulate water balance
- Leading to increased pressure in the blood vessels
How does kidney failure affect electrolyte balance? (2)
- Loss of electrolyte balance means sodium, potassium, and chloride ions are not excreted properly
- Leading to osmotic imbalances and possible death
What causes anaemia in patients with long-term kidney failure? (2)
- Kidney failure reduces the production of erythropoietin
- Which leads to fewer red blood cells
What is haemodialysis and how does it work? (3)
- Haemodialysis is a process where a machine filters a patient's blood by passing it through a partially permeable membrane
- The blood flows in the opposite direction to dialysis fluid (countercurrent flow)
- Waste products, excess water, and ions diffuse across the membrane into the dialysis fluid, removing them from the blood
How does the dialysis fluid prevent the loss of useful substances during haemodialysis? (2)
- The dialysis fluid contains normal plasma levels of glucose and mineral ions
- Preventing glucose loss and ensuring only excess ions move out of the blood
What are the disadvantages of haemodialysis? (2)
- Patients can feel unwell between sessions due to waste product buildup
- Sessions take 3-5 hours, 2-3 times per week, and usually take place in hospitals, making dialysis expensive and inconvenient
What is the main benefit of haemodialysis over kidney transplants? (1)
Less risky than the major surgery involved in a transplant
How does peritoneal dialysis work? (3)
1. Dialysis fluid is introduced into the abdomen using a catheter
2. Urea and excess ions pass from the blood capillaries into the tissue fluid and across the peritoneal membrane into the dialysis fluid
3. The fluid is drained and discarded
How is the peritoneal membrane different from the artificial dialysis membrane? (2)
- The peritoneal membrane can perform active transport and facilitated diffusion
- Unlike the artificial dialysis membrane
What is a kidney transplant? (3)
- A new kidney is transplanted into a patient to replace a damaged kidney
- The kidney must come from a person with a matching blood and tissue type
- Either from a living relative or an organ donor
What are the advantages of a kidney transplant over dialysis? (3)
- Cheaper in the long term
- More convenient for the patient (no regular dialysis)
- No periods of feeling unwell between dialysis sessions
What are the disadvantages of kidney transplants? (4)
- Major surgery is risky
- The immune system may reject the transplant
- Requiring lifelong immunosuppressant drugs
- Which can reduce the ability to fight infections
Why is it important to closely match the donated kidney to the recipient? (5)
1. If not closely matched, the kidney will be recognized as foreign
2. The antigens on the donated kidney will differ from those of the recipient
3. This causes the immune system to reject the kidney
4. Even with close matching, lifelong immunosuppressant drugs are required
5. If the recipient is a small child, the donor kidney must be a suitable size
What hormone is tested for in a pregnancy test, and where is it found? (2)
- hCG
- Which is found in the urine of pregnant women
What happens when urine is applied to the application area of a pregnancy test? (2)
1. The hCG binds to monoclonal antibodies attached to blue beads
2. Forming an antigen-antibody complex
How does the test strip of a pregnancy test turn blue? (3)
- If hCG is present
- It binds to immobilised antibodies on the test strip
- Concentrating the blue beads and turning the strip blue
What happens if a woman is not pregnant during a pregnancy test? (3)
- No hCG is present
- So the urine passes through the test strip without binding
- The test strip does not turn blue
What are anabolic steroids, and why are athletes tested for them? (3)
- Anabolic steroids build muscle tissue
- But they have dangerous side effects (e.g., liver failure)
- Are unfair to other athletes
What testing method is used for detecting anabolic steroids in athletes' urine? (2)
Gas chromatography/mass spectrometry (GC/MS)
How does gas chromatography work in steroid testing? (2)
1. The urine sample is vaporised and passed through a polymer column
2. Where substances are separated based on their movement speed
How does mass spectrometry work in detecting anabolic steroids? (2)
- Converts substances into ions and separates them based on mass and charge
- A computer compares the results with known substances
How are recreational drugs detected using a urine test strip? (2)
1. Test strip contains antibodies that bind to the drug being tested (e.g., cannabis, ecstasy, cocaine)
2. A colour change occurs if the drug is present
What happens if a urine test for recreational drugs shows a positive result? (2)
- The urine sample is sent for further testing using GC/MS
- To confirm which drugs were taken