Infertility, Contraception, and Abortion Overview
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
63 Terms
What is the definition of infertility for women under 35 years of age?
Infertility is defined as 1 year of regular, unprotected intercourse without conception.
What is the definition of infertility for women over 35 years of age?
Infertility is defined as 6 months of regular, unprotected intercourse without conception.
Fecundity
The chance of achieving pregnancy and subsequent live birth within one menstrual cycle.
Averages 20% in couples who are not experiencing reproductive difficulties.
What are the two main types of infertility?
Primary infertility (has never conceived) and secondary infertility (has been pregnant in the past).
List some factors associated with female infertility.
Ovarian factors, tubal and peritoneal factors, uterine factors, vaginal-cervical factors, isoimmunization, and other factors.
What are some male infertility factors?
Hormonal disorders, testicular factors (e.g., undescended testes, hypospadias, varicocele), factors associated with sperm transport, and idiopathic male infertility.
What are some assessment methods for female infertility?
History and physical exam, diagnostic tests (anatomy evaluation, bimanual examination, CBC, STI testing, ovulation detection, hormone analysis, ultrasonography, endometrial biopsy, laparoscopy, hysterosalpingography).
What assessments are performed for male infertility?
History and physical exam, semen analysis, sperm penetration assay, hormone analysis, scrotal ultrasound, transrectal ultrasound.
What are some nonmedical nursing care recommendations for infertility?
Healthy lifestyle (normal BMI, moderate exercise), stress management, and avoiding alcohol, smoking, and drugs.
What are some medical treatments for female infertility?
Oral contraceptives for endometriosis, antimicrobials for infections, Clomiphene citrate for ovulation, Metformin for PCOS, and thyroid replacement therapy.
Ovarian Reserve
How many potential ova remain within the ovaries.
A common evaluation is measurement of follicle-stimulating hormone (FSH) levels on the third day of the menstrual cycle
Endometriosis
Implantation of endometrial tissue outside of uterus
Semen Analysis
Study of the effects of cervical mucus on sperm forward motility and survival, and evaluation of the sperm’s ability to penetrate an ovum provide basic information.
Sperm counts vary from day to day and depend on emotional and physical status and sexual activity. Therefore, a single analysis may be inconclusive.
A minimum of two analyses must be performed several weeks apart to assess male fertility.
The specimen is usually collected by masturbation following 2 to 5 days of abstinence from ejaculation
Clomiphen Citrate
Often the initial pharmacological treatment of the infertile patient because it is inexpensive and the adverse effect profile is less than that of other medications that induce ovulation.
There is an increased risk of giving birth to twins or higher-order multiples with clomiphene therapy
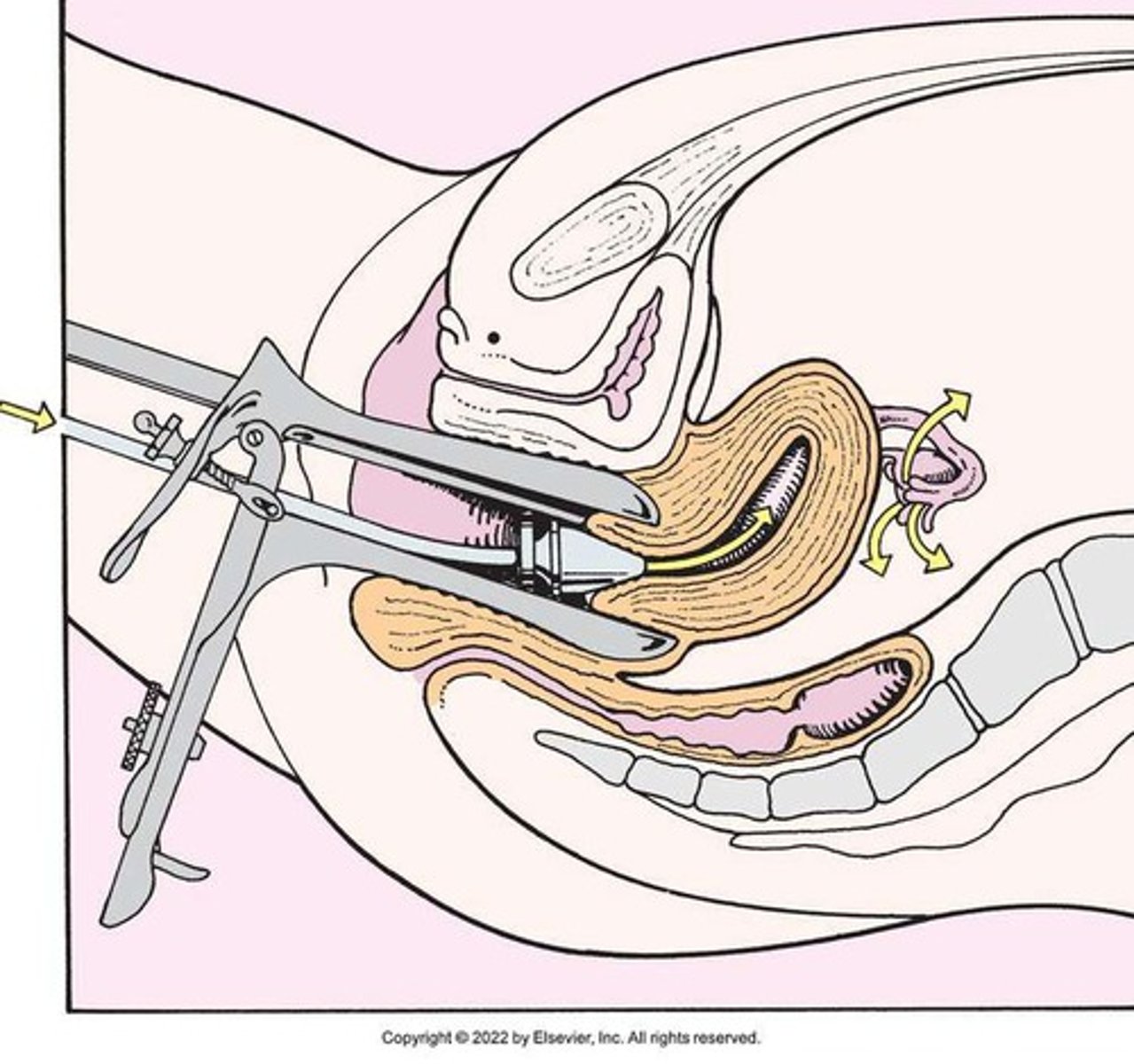
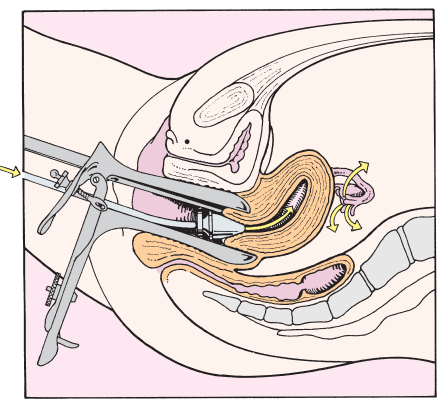
Hysterosalpinogography
Useful for identification of tubal obstruction and for the release of blockage
Contrast medium flows through the intrauterine cannula and out through the uterine tubes.
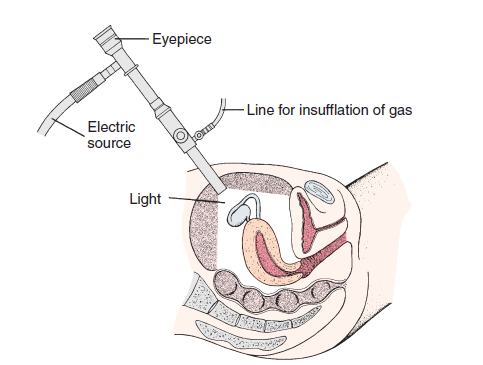
Laparoscopy
Delicate adhesions may be divided and removed, and endometrial implants may be destroyed by electrocoagulation or laser
What is assisted human reproduction (AHR)?
AHR includes techniques like in vitro fertilization (IVF), gamete intrafallopian transfer (GIFT), zygote intrafallopian transfer (ZIFT), donor oocyte, embryo adoption, and therapeutic donor insemination.
Invitro Fertilization
Oocytes are retrieved from the ovary, fertilized in the laboratory with sperm, and transferred to the uterus after normal embryo development has occurred
Indication:
Tubal disease or blockage; severe male infertility; endometriosis; unexplained infertility; cervical factor; immunological infertility
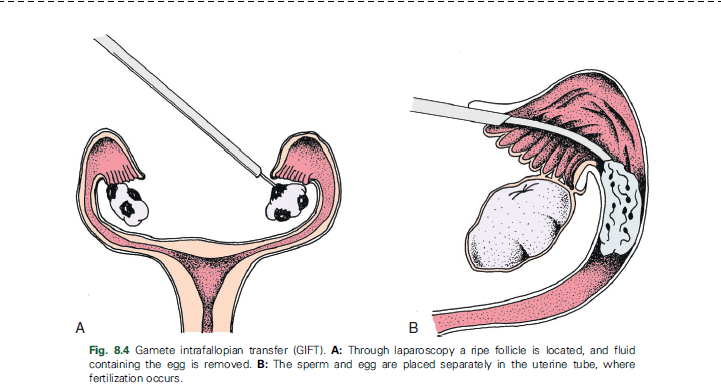
Gamete Intrafallopian Transfer
Oocytes are retrieved from the ovary, placed in a catheter with washed motile sperm, and immediately transferred into the fimbriated end of the uterine tube. Fertilization occurs in the uterine tube.
There must be normal tubal anatomy, patency, and absence of previous tubal disease in at least one uterine tube
Zygote Intrafallopian Transfer
This process is similar to IVF-ET; after IVF the ova are placed in one uterine tube during the zygote stage
Donor Oocyte
Eggs are donated by an IVF procedure and the donated eggs are inseminated. The embryos are transferred into the recipient’s uterus, which is hormonally prepared with estrogen–progesterone therapy.
Indication:
Early menopause; surgical removal of ovaries; congenitally absent
ovaries; autosomal or sex-linked disorders; lack of fertilization in
repeated IVF attempts because of subtle oocyte abnormalities or
defects in oocyte–spermatozoa interaction
Embryo Adoption
Donated embryo is transferred to the uterus of an infertile person at the appropriate time (normal or induced) of the menstrual cycle.
Indication:
Infertility not resolved by less aggressive forms of therapy; absence of ovaries; male partner is azoospermic or severely compromised
Therapeutic Donor Insemination
Donor sperm are used to inseminate the female partner.
Indication
Male partner is azoospermic or has a very low sperm count; couple has a genetic defect; male partner has antisperm antibodies; lesbian couple
Intracytoplasmic sperm injection
One sperm cell is selected to be injected directly into the egg to achieve fertilization. It is used with IVF.
Same indications as TDI
Assisted Hatching
The zona pellucida is penetrated chemically or manually to create an opening for the dividing embryo to hatch and implant into the uterine wall.
Indication
Recurrent miscarriages; to improve implantation rate in women with previously unsuccessful IVF attempts; advanced age
Zona Pellucida
An extracellular matrix that surrounds the plasma membrane of the egg cell. it protects the egg.
What is the definition of abortion?
Intentional interruption of pregnancy before 20 weeks of gestation.
What are the two main types of abortion?
Elective and therapeutic.
What are some methods of first-trimester abortion?
Surgical (aspiration) abortion and medical abortion (e.g., Mifepristone/Misoprostol).
What are the discharge instructions for patients post-abortion?
Call HCP if experiencing fever, chills, flu-like symptoms, heavy bleeding, foul-smelling discharge, severe pain, or if the period does not return after 8 weeks.
What is contraception?
Intentional prevention of pregnancy.
What is the purpose of family planning?
To make conscious decisions about when to conceive or avoid pregnancy.
What are some methods of natural family planning (NFP)?
Fertility awareness-based methods, lactational amenorrhea, coitus interruptus, and abstinence.
Fertility Awareness Based method
Patients learn how to determine the beginning and the end of the fertile period of their menstrual cycle. The individual would then avoid unprotected intercourse during this “fertile window.”
Calendar days Method
Based on the number of days in each cycle, counting from the first day of the menstrual cycle.
The fertile period is determined after accurately recording the length of menstrual cycles for 6 to 12 months.
The beginning of the fertile period is estimated by subtracting 20 days from the length of the shortest cycle. The end of the fertile period is determined by subtracting 10 days from the length of the longest cycle.
Standard Days Method
Has a “fixed” number of days of fertility for each cycle (i.e., days 8 to 19 in individuals who have a menstrual cycle from 26 to 32 days in length).
Day 1 of the menstrual flow is counted as the first day to begin the counting.
Although this method is useful to patients whose cycles are 26 to 32 days long, it is unreliable for those who have longer or shorter cycles.
Basal Body Temperature
Is the lowest body temperature of a healthy person, taken immediately after waking, after at least 6 hours of sleep and before getting out of bed. Usually varies from 36.2° to 36.3°C during menses and for approximately 5 to 7 days afterward.
Basal Body Temperature Method
About the time of ovulation, a slight drop in temperature (approximately 0.5°C) may occur in some patients, but others may have no decrease at all. After ovulation, in concert with the increasing progesterone levels of the early luteal phase of the cycle, the BBT increases slightly (approximately 0.5°C). The temperature remains on an elevated plateau until 2 to 4 days before menstruation.
To use this method, the fertile period is defined as the day of first temperature drop, or first elevation, through 3 consecutive days of elevated temperature.
Abstinence begins the first day of menstrual bleeding and lasts through 3 consecutive days of sustained temperature
Cervical Mucus Ovulation Detection Method
Requires that the patient recognize and interpret the cyclic changes in the amount and consistency of cervical mucus before and during ovulation to facilitate and promote the viability and motility of sperm.
Without adequate cervical mucus, coitus does not result in conception.
This method requires that a patient check the quantity and character of mucus on the vulva or introitus with their fingers or with tissue paper each day for several months.
This way they can learn how their cervical mucus responds to ovulation during their menstrual cycle.
Intercourse is considered safe without restriction beginning on the fourth day after the last day of wet, clear, slippery mucus, which would indicate that ovulation has occurred 2 to 3 days previously. After ovulation, mucus first becomes thick, opaque, and reduces in volume.
Sympthothermal Method
A method that combines BBT and cervical mucus methods along with awareness of secondary, cycle phase-related symptoms.
The person gains fertility awareness as they learn the psychological and physiological symptoms that mark the phases of their cycle.
Secondary symptoms include increased libido, midcycle spotting, mittelschmerz (cramplike pain before ovulation), pelvic fullness or tenderness, and vulvar fullness.
The patient is taught to palpate their cervix to assess for changes indicating ovulation: the cervical os dilates slightly, the cervix softens and rises in the vagina, and cervical mucus is copious and slippery.
Calendar calculations and cervical mucus changes are used to estimate the onset of the fertile period; changes in cervical mucus and the BBT are used to estimate its end.
Two day Method
Involves an evaluation of cervical mucus to determine a patient’s fertility. If cervical secretions were present “today” and “yesterday” a patient is very fertile.
If the secretions were present either “today” or “yesterday” they are fertile.
If there was no cervical mucus “today” or “yesterday” the fertility is low
Home predictor Kits for ovulation
The urine or saliva predictor test for ovulation detects the sudden surge of LH that occurs approximately 12 to 24 hours before ovulation.
Unlike BBT, the test is not affected by illness, emotional upset, or physical activity.
A positive response indicating an LH surge is noted by a colour change that is easy to read.
Coitus Interruptus
Involves the male partner withdrawing their penis fromthe individual’s vagina before they ejaculate.
Breastfeeding: Lactational Amenorrhea Method
When the infant suckles at the breast, a surge of prolactin hormone is released, which inhibits estrogen production and suppresses ovulation and the return of menses.
Three factors are necessary for it to be effective:
• the patient is less than 6 months postpartum;
• they are fully or nearly fully breastfeeding; and
• their period has not returned
What are barrier methods of contraception?
Spermicides, condoms (male and female), diaphragm, cervical cap, and contraceptive sponge.
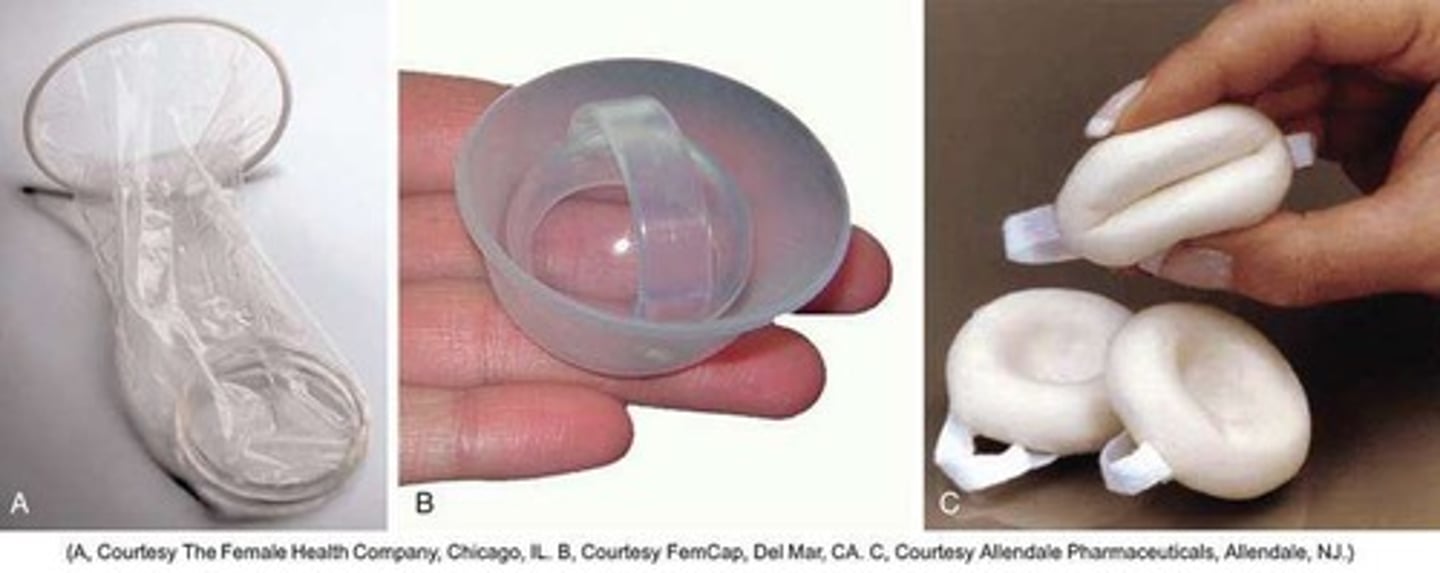
Diaphragm
A shallow, domeshaped, latex or silicone device with a flexible rim that covers the cervix.
Along with the use of a gel, is a mechanical barrier to the meeting of sperm with the ovum
Users should use an acidbuffering lubricant such as the SILCS diaphragm gel or Contragel, which forms a physical barrier in front of the cervix and lowers the pH of the vaginal fluid, thereby inhibiting sperm motility
Must remain in place for at least 6 hours following intercourse and removal before this time increases the risk of pregnancy. Side effects may include increased risk of urinary tract infections.
Contraindicated for patients with pelvic relaxation (uterine prolapse) or a large cystocele.
Toxic shock syndrome (TSS), although very rare, can occur
Cervical Cap
Made of silicone rubber and has a soft dome and firm brim.
It fits snugly around the base of the cervix close to the junction of the cervix and vaginal fornices.
It is recommended that it remains in place no less than 6 hours and not more than 48 hours at a time.
The seal provides a physical barrier to sperm, but it should also be used with an acidbuffering lubricant to inhibit sperm mobility.
Contraceptive Sponge
A small, disposable, round, polyurethane sponge that contains N-9 spermicide
It is designed to fit over the cervix (one size fits all).
The side that is placed next to the cervix is concave for better fit.The opposite side has a woven polyester loop to be used for removal of the sponge.
The sponge must be moistened with water before it is inserted into the vagina to cover the cervix.
It provides protection for up to 24 hours and for repeated instances of sexual intercourse.
It should be left in place for at least 6 hours after the last act of intercourse.
Wearing it longer than 24 to 30 hours may put the person at risk for TSS.
Common Toxic Shock Syndrome Signs
Sunburn-type of rash
Diarrhea
Dizziness
Faintness,
Weakness
Sore throat
Aching muscles and joints
Sudden high fever, and
Vomiting.
What are hormonal methods of contraception?
Progestin-only contraceptives, combined hormonal contraceptives (CHC), and emergency contraception.
Combined Hormonal Contraception
Refers to contraceptive methods that contain both an estrogen and a progestin.
Combined Oral Contraceptives
Regular ingestion suppresses the action of the hypothalamus and anterior pituitary, leading to insufficient secretion of FSH and LH; therefore, follicles do not mature, and ovulation is inhibited
Contraindications for Combined Oral Contraceptives
A history of thromboembolic disorders
Cerebrovascular or coronary artery disease
Breast cancer
Estrogen-dependent tumours
Pregnancy
Impaired liver function
Liver tumour
Lactation less than 6 weeks postpartum
Smoking if older than 35 years of age
Migraine with aura
Surgery with prolonged immobilization or any surgery on the legs
Hypertension (160/100), and
Diabetes mellitus (of more than 20 years’ duration) with vascular disease
Signs of potential complications of Oral Contraceptives
A—Abdominal pain: may indicate an issue with the liver or gallbladder
C—Chest pain or shortness of breath: may indicate possible clot within lungs or heart
H—Headaches (sudden or persistent): may be caused by cardiovascular accident or hypertension
E—Eye conditions: may indicate vascular accident or hypertension
S—Severe leg pain: may indicate a thromboembolic process
Stop taking pill immediately and contact HCP
Transdermal Contraceptive System
Delivers continuous levels of progesterone and ethynyl estradiol.
The patch can be applied to the lower abdomen, upper outer arm, buttock, or upper torso (except the breasts).
Application is on the same day once a week for 3 weeks but not at the same site, followed by a week without the patch.
Withdrawal bleeding occurs during the “no patch” week.
Associated with less breakthrough bleeding and spotting but more breast discomfort or pain, nausea and vomiting, and dysmenorrhea
Contraceptive Vaginal RIng
A flexible, soft, transparent ring made of copolymer ethylene vinyl that delivers continuous levels of progesterone and ethynyl estradiol, which is absorbed through the vaginal epithelium.
It is worn for 3 weeks, followed by a week without the ring.
Withdrawal bleeding occurs during the “no ring” week.
It can be inserted by the patient and does not have to be fitted
Oral Progesting (Minipill)
Contain a lower dose of progestin and must be taken at the same time every day.
If the pill is taken more than 3 hours late (27 hours after the last pill), a backup contraceptive method must be initiated.
Injectable Progestin
Depot medroxyprogesterone acetate (DMPA) is given subcutaneously or intramuscularly in the deltoid or gluteus maximus muscle.
DMPA should be initiated during the first 5 days of the menstrual cycle and administered every 12 to 13 weeks.
When administering an injection of DMPA, the site should not be massaged after the injection because this action can hasten the absorption and shorten the period of effectiveness.
Adverse Effect of DMPA
Decreased bone mineral density, weight gain, lipid changes,
Increased risk of venous thrombosis and thromboembolism,
Irregular vaginal spotting, decreased libido, and breast changes.
Other disadvantages include no protection against STIs.
Return to fertility may be delayed as long as up to 18 months after discontinuing DMPA.
What is the role of emergency contraception (EC)?
Used within 5 days of unprotected intercourse to prevent pregnancy.
What is intrauterine contraception (IUC)?
A small, T-shaped device inserted into the uterine cavity to prevent pregnancy.
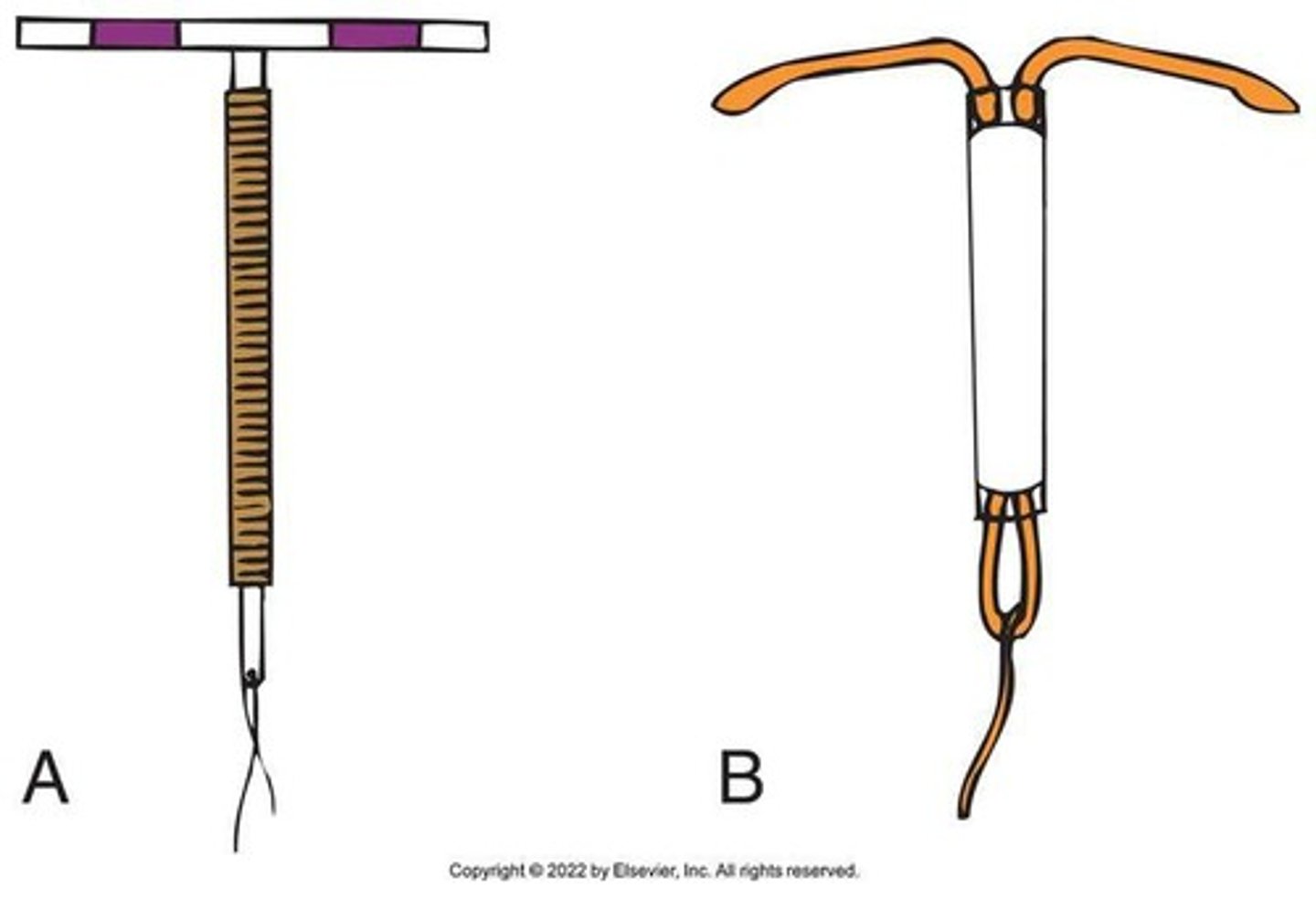
Signs of Potential complication of Intrauterine devices
P—Period late, abnormal spotting or bleeding
A—Abdominal pain, pain with intercourse
I—Infection exposure, abnormal vaginal discharge
N—Not feeling well, fever, or chills
S—String missing; shorter or longer
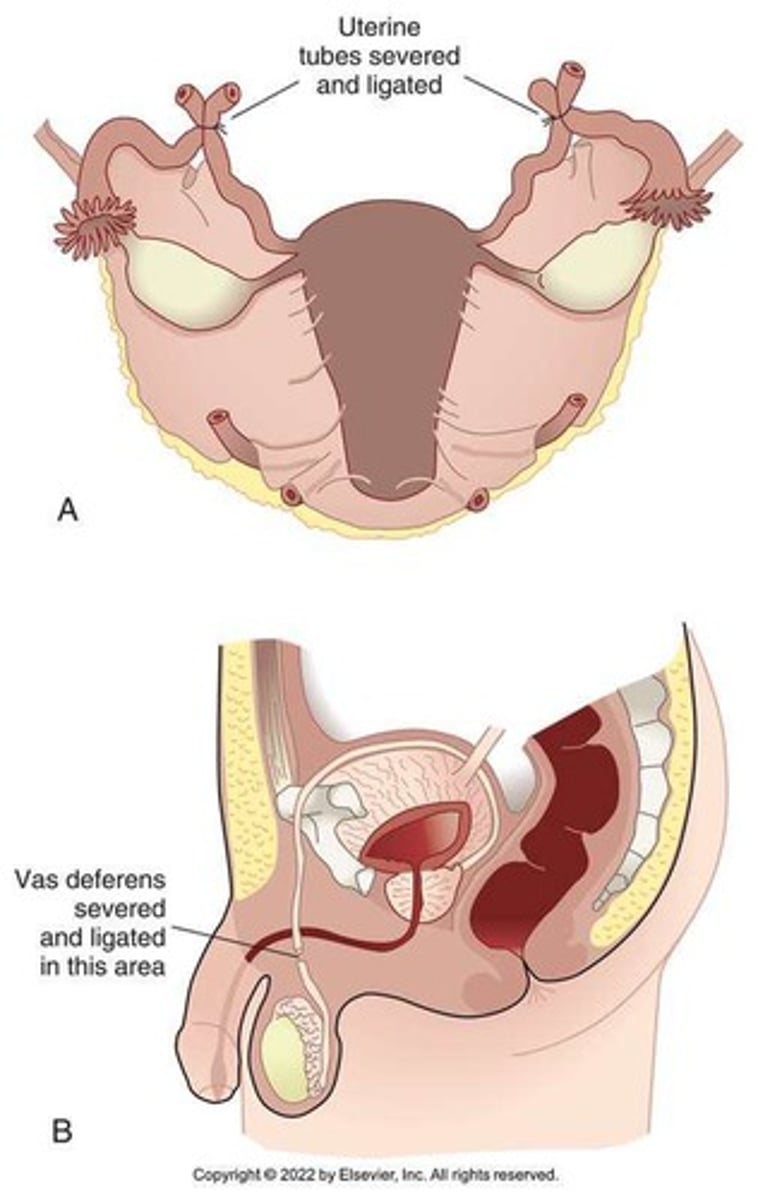
What are the sterilization methods for contraception?
Female sterilization (tubal occlusion) and male sterilization (vasectomy).