Physio Lect 26 - Microcirculation Part Three: Fluid Flux
1/17
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
18 Terms
What are some important characteristics of capillaries?
Capillaries are permeable to water.
Blood pressure causes filtration of fluid out of capillaries.
Plasma osmotic pressure balances blood pressure and limits
filtration.
T/F: Fluid filtration or absorption has no effect on diffusion.
T
T/F: Diffusion is much faster than fluid flux.
T
What are the three factors that regulate fluid flux?
Hydrostatic Pressure
Oncotic Pressure
Endothelial Permeability
We already know a little bit about oncotic pressure because we have learned about osmotic pressure, what is the main difference between the two?
Proteins create oncotic pressure
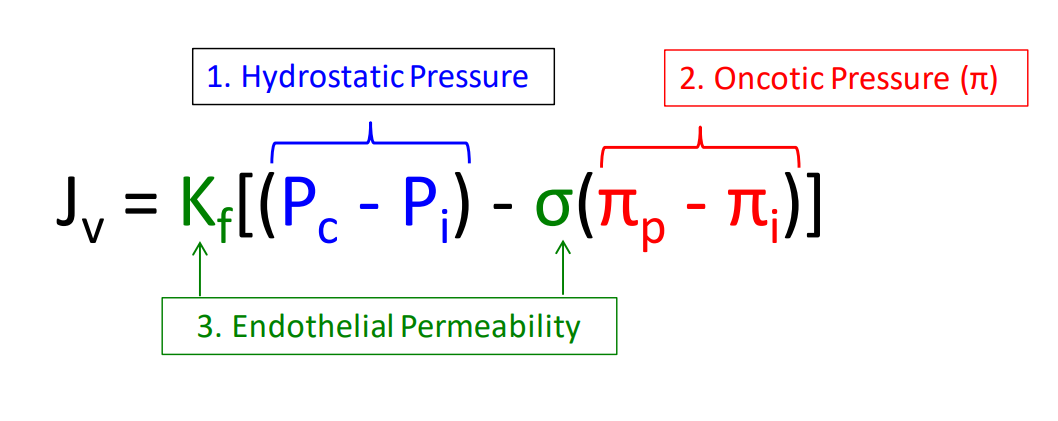
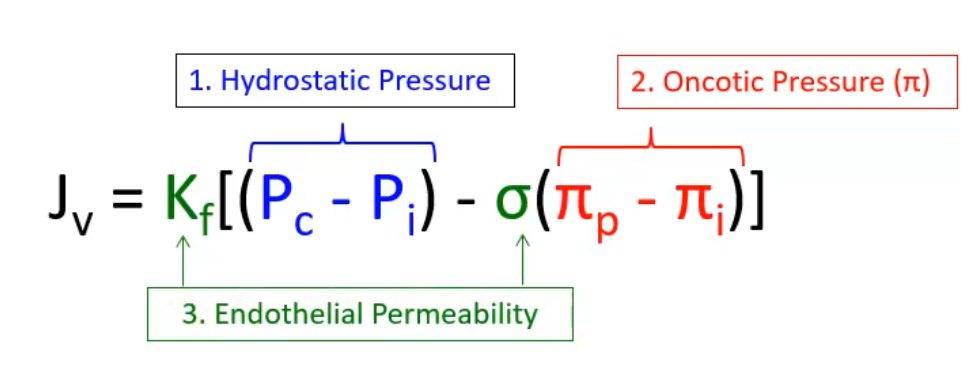
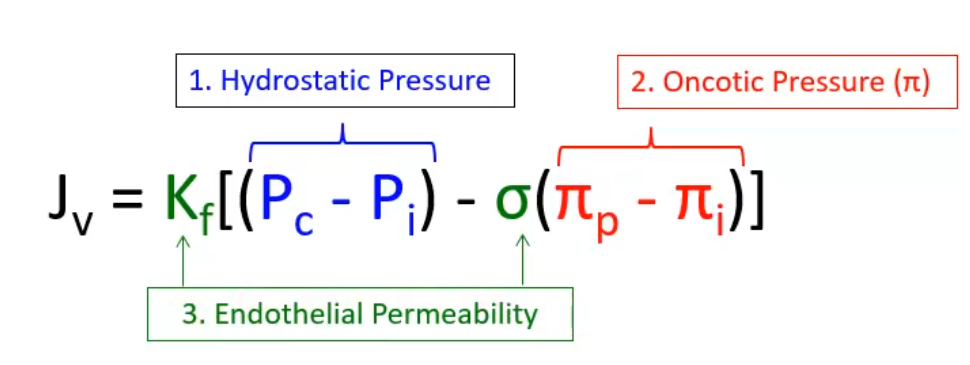
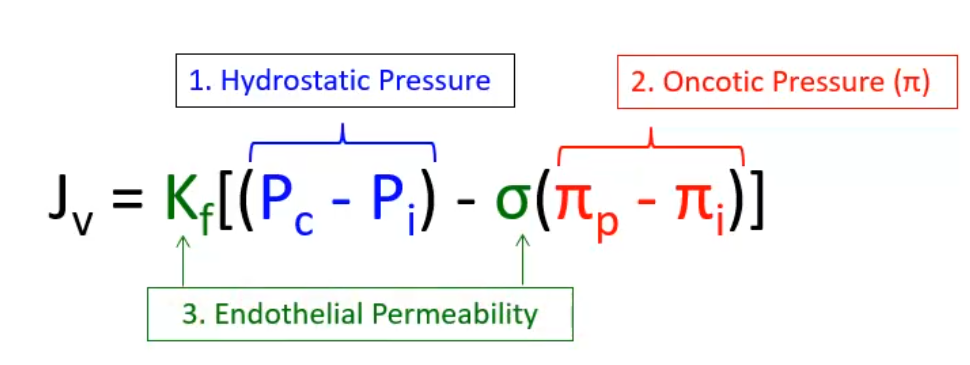
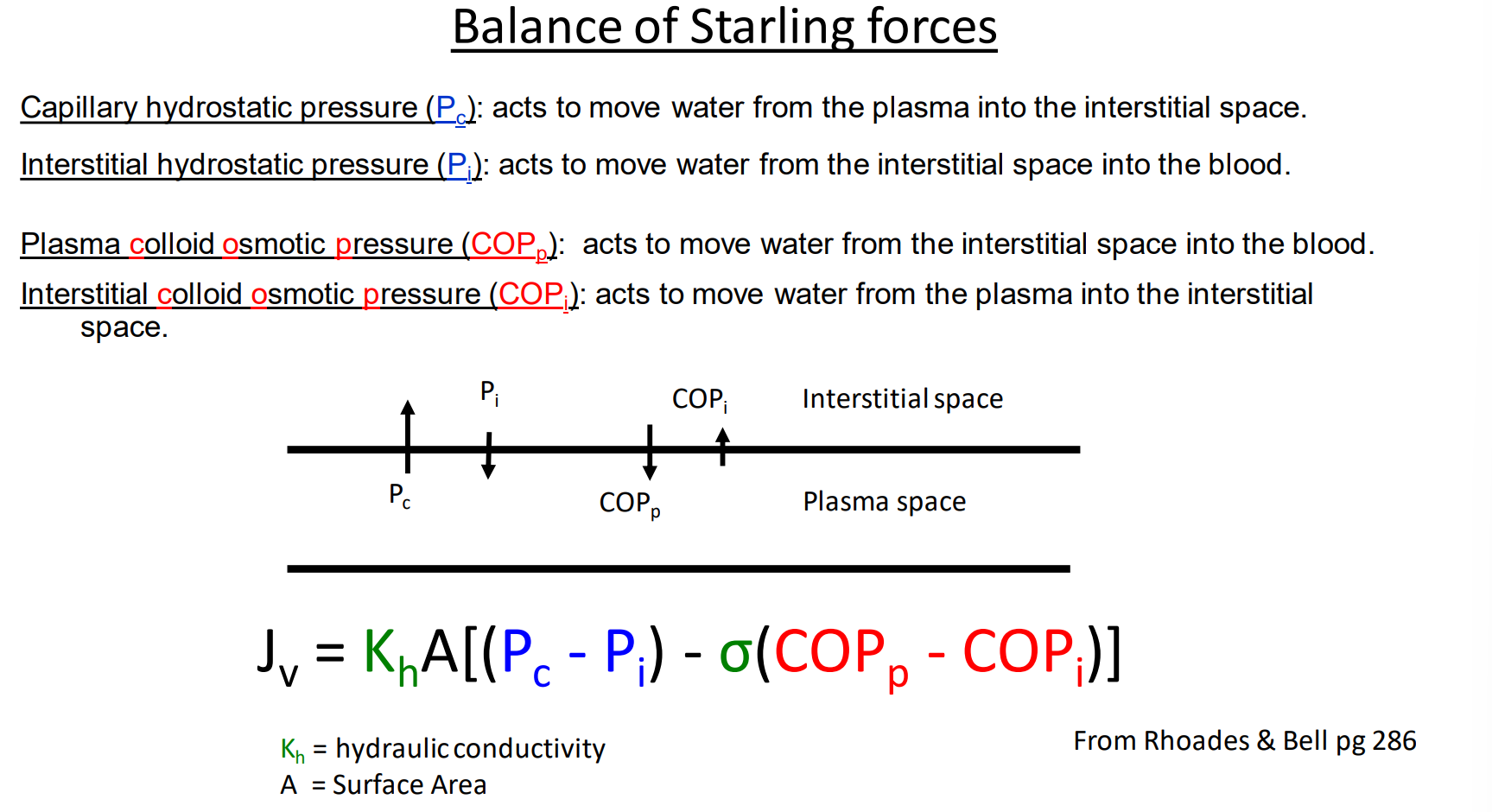
What does the starling equation look like?
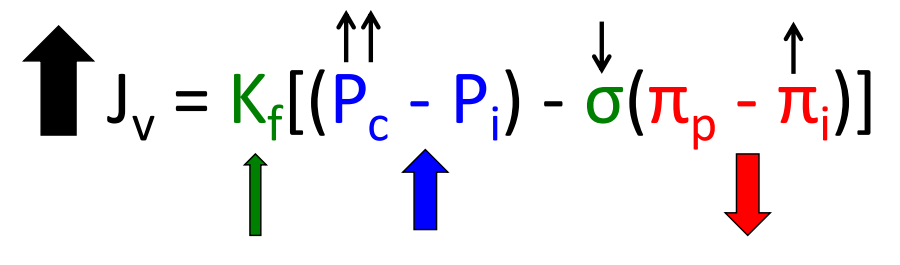
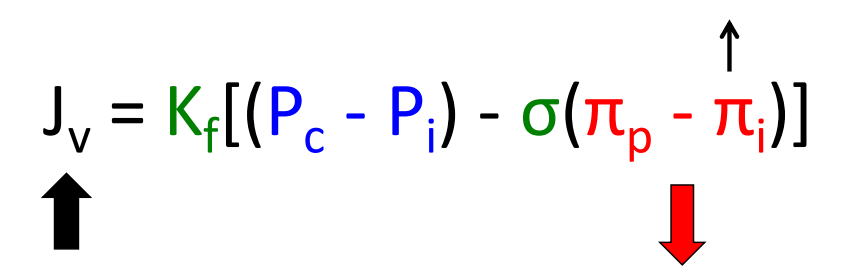
Jv = Kf [(Pc - Pi ) - σ(πp - πi )]
![<p>Jv = Kf [(Pc - Pi ) - σ(πp - πi )]</p>](https://knowt-user-attachments.s3.amazonaws.com/cb2cb6b0-e737-4143-946a-9e9253e5484d.png)
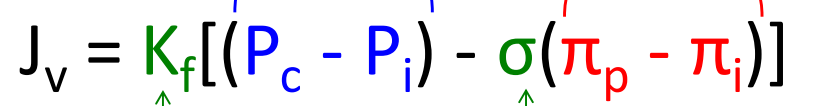
Can you explain what aspects of the starling equation correspond to hydrostatic pressure, oncotic pressure, and endothelial permeability?
Hydrostatic pressure - Pc - Pi
Oncotic pressure - πp - πi
Endothelial permeability - Kf and σ
What does Kf stand for in the starling equation?
Capillary filtration coefficient is the capacity of a membrane (endothelial monolayer) to allow flux of water in response to a 1 mm Hg pressure gradient
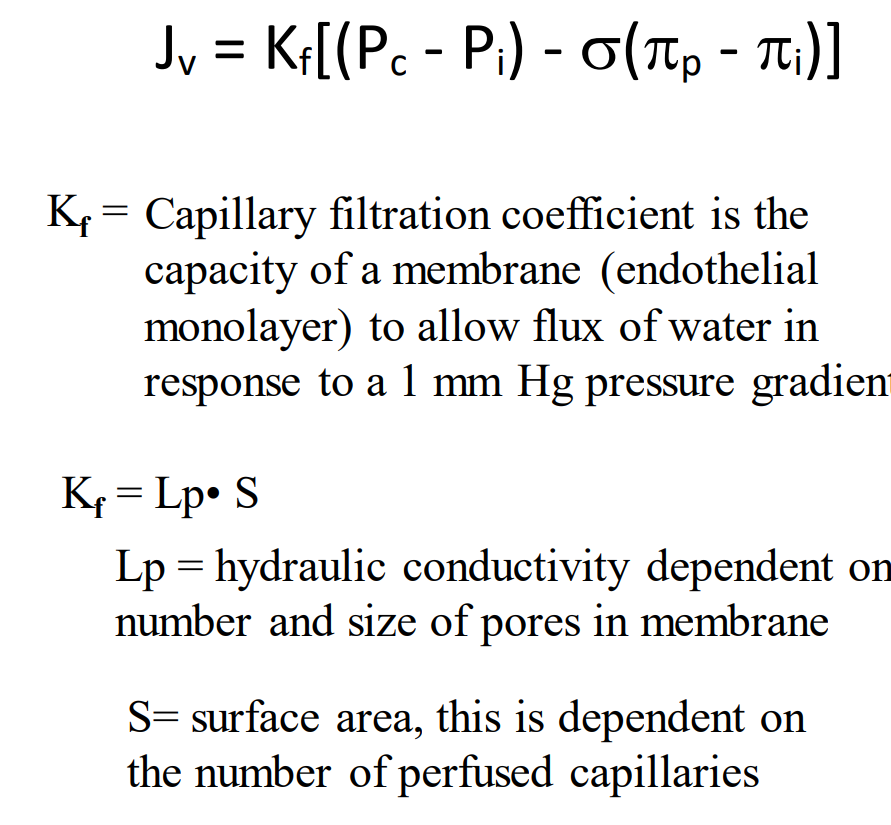
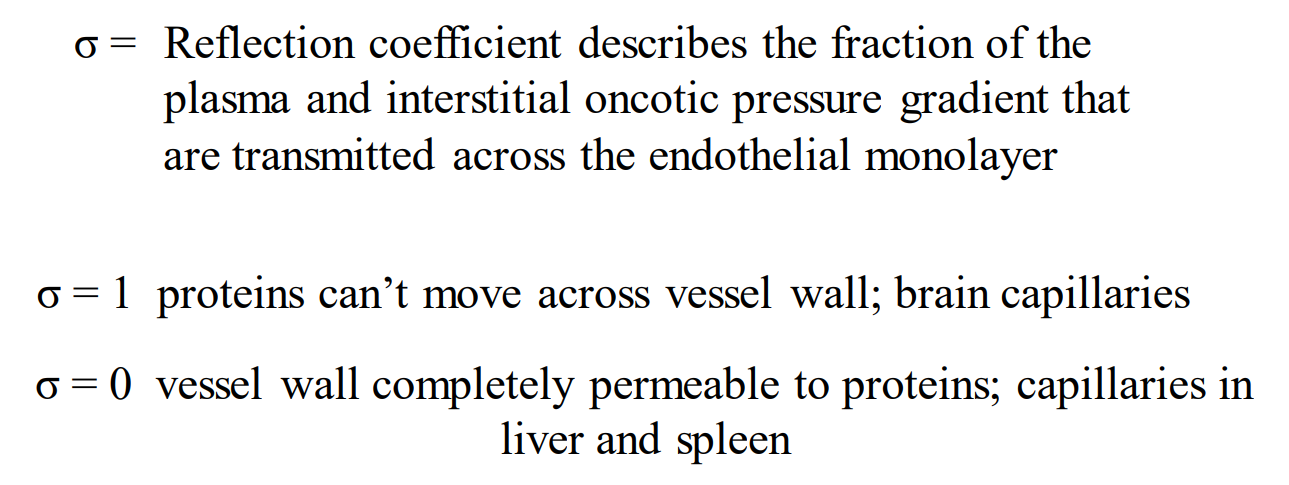
What does sigma stand for in the starling equation?
Reflection coefficient describes the fraction of the plasma and interstitial oncotic pressure gradient that are transmitted across the endothelial monolayer
Explain how we find the hydrostatic pressure difference in the starling equation:
We measure the capillary hydrostatic pressure and the interstitial hydrostatic pressure. To get our delta P we find the difference between the two
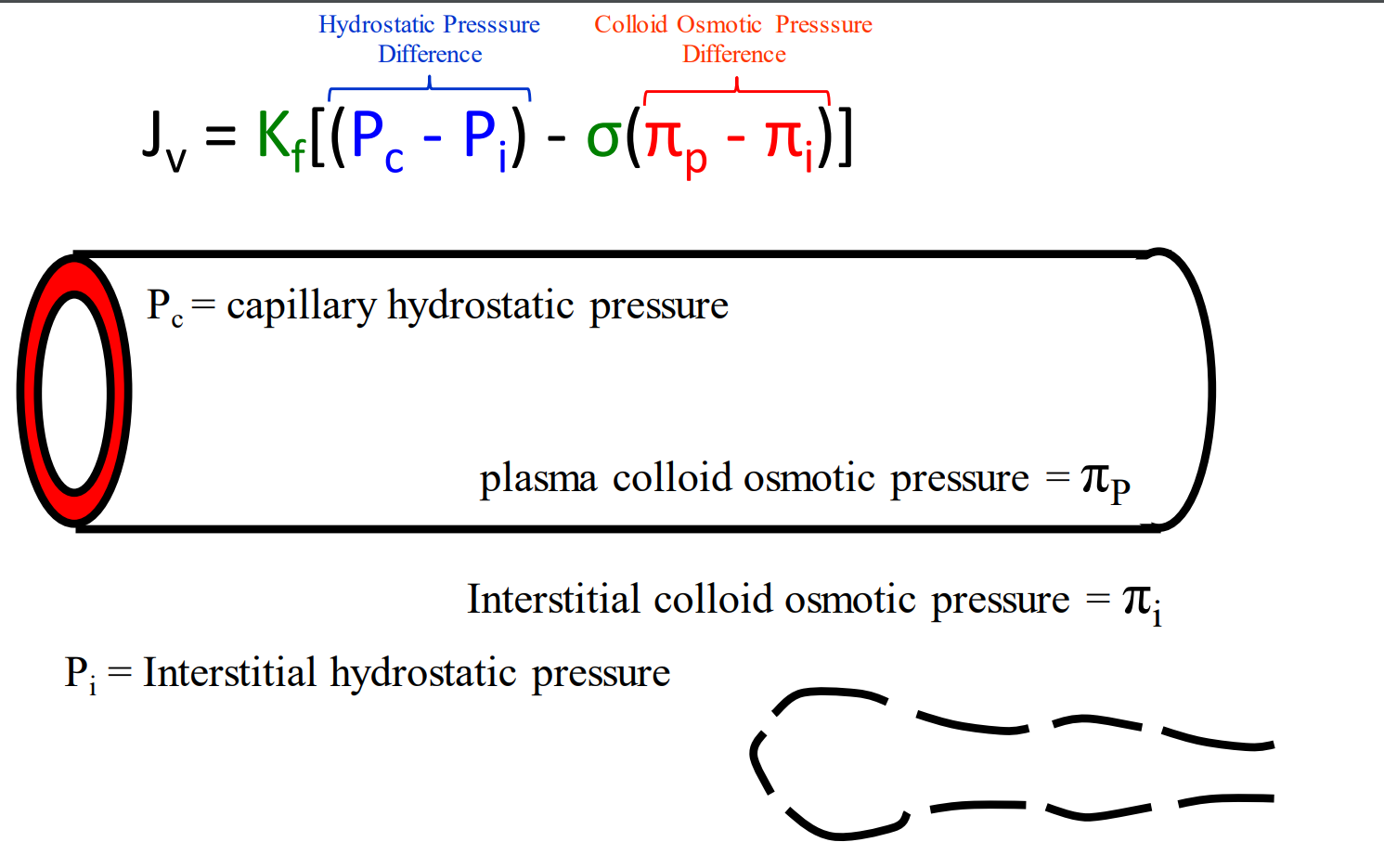
What direction do each of these pressures, hydrostatic and colloid osmotic, send the fluid?
Pc - Capillary hydrostatic pressure tries to draw water out
Pi - Interstitial hydrostatic pressure tries to draw water in
πP - Plasma colloid osmotic pressure tries to draw water in
πI - Interstitial colloid osmotic pressure tires to draw water out
Referring to slide 11 - hereis a summary of how the starling forces are balanced:
Do your best to understand this
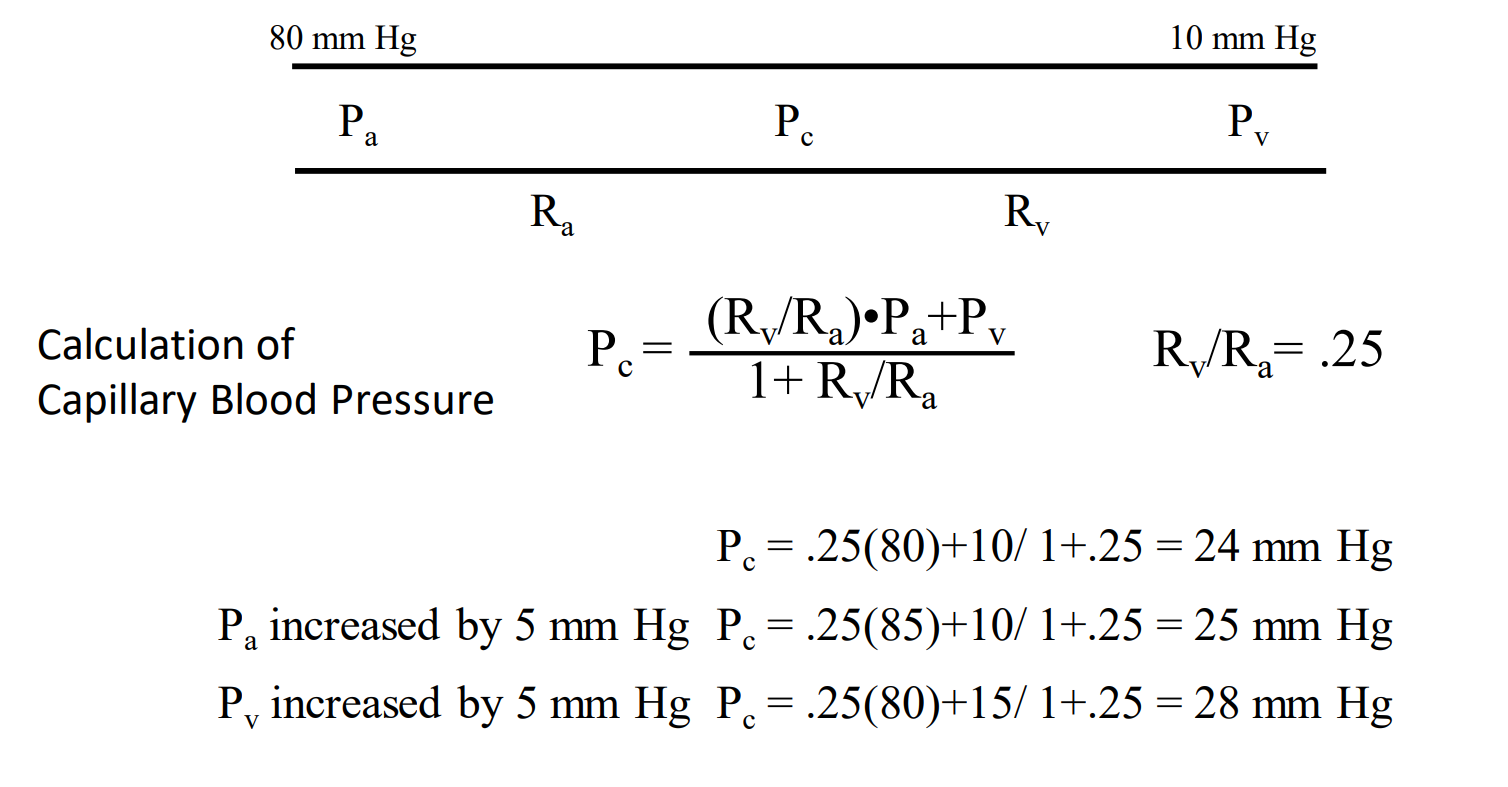
T/F: Changes in venous pressure can and will effect a change in capillary pressure
T
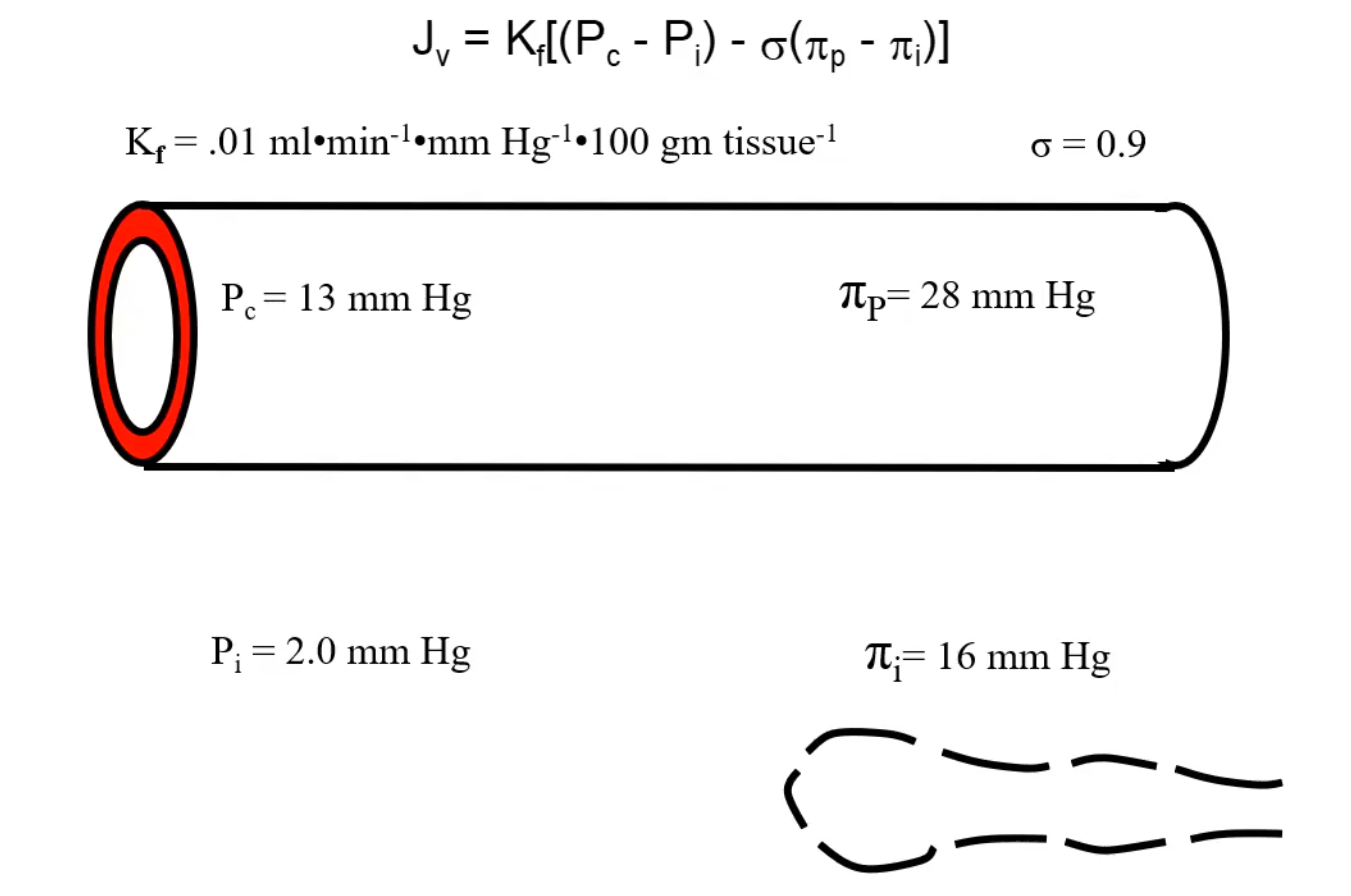
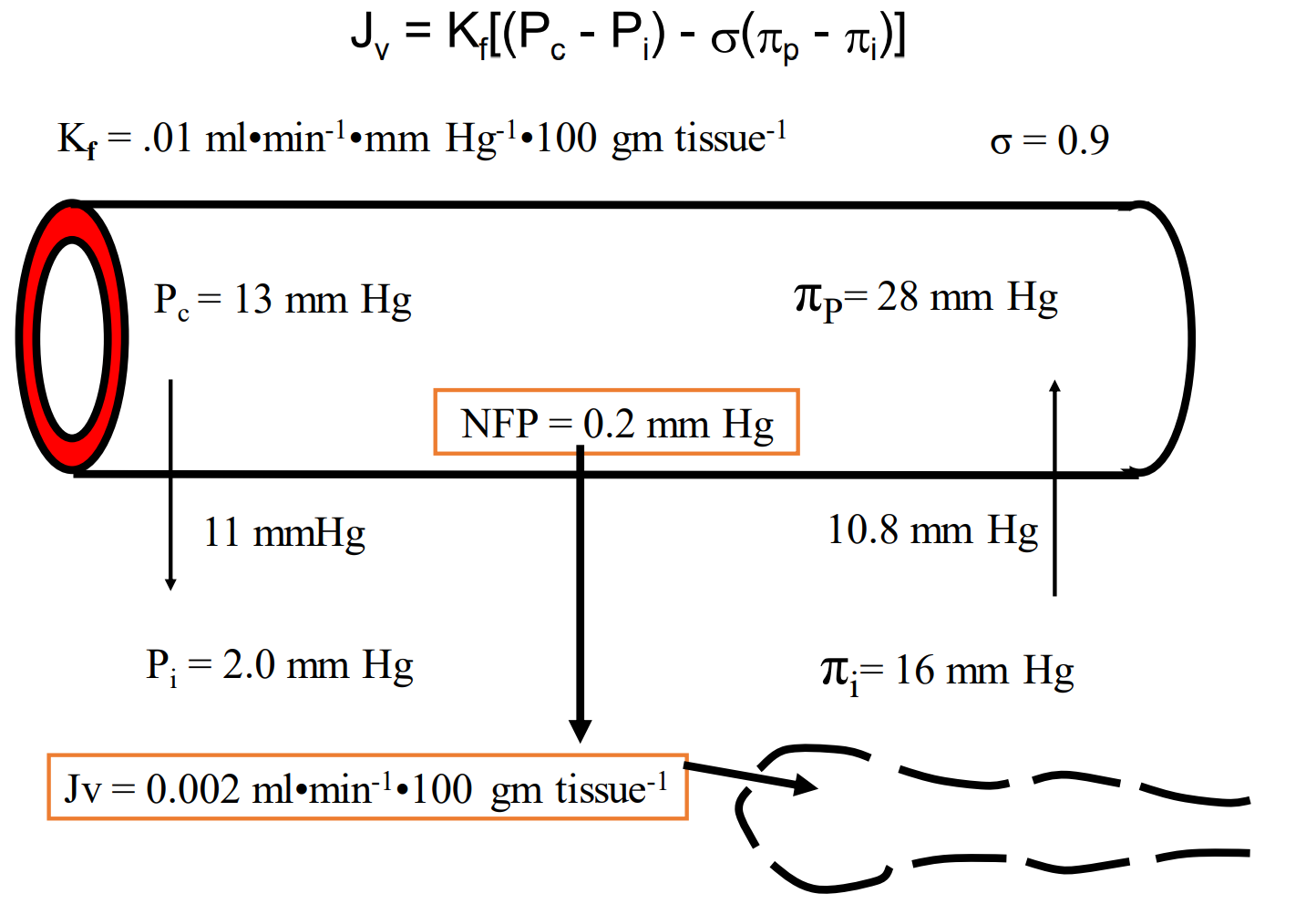
Calculate net filtration pressure:
13-2=11 mmHg, gives us Pc-Pi.
(28-16)*0.9=10.8, gives us sigma*(πP-πI).
Take the difference between 11 mmHg and 10.8 and we get 0.2 mmHg pointed to the interstitial.
To get Jv, just multiply that number by Kf (which is 0.01 ml*min-1*mmHg-1×100 gm tissue-1) —> giving us 0.002 ml*min-1 x 100 gm tissue-1
Here’s an example of how different things can impact this equation - let’s look at histamine. What things will histamine increase? What will it decrease?
Increases Kf because Lp increases.
Increases hydrostatic pressure difference. (Increases Pc)
Increases protein flux into the interstitium, decreasing the oncotic pressure difference. (Increases Pi I)
Decreases limiting oncotic effect
Increases Jv overall
An increase in protein concentration in the interstitial fluid would tend to cause all of the following EXCEPT.
A. an increase in lymph flow
B. an increase in interstitial oncotic pressure
C. a decrease in capillary filtration
D. edema
E. a decrease in net transcapillary oncotic pressure gradient
Answer = C. Remember you are looking for the exception. Increasing the protein concentration (i.e., oncotic pressure; B) would increase the forces favoring filtration by decreasing the oncotic pressure gradient (E). The increase in fluid flux into the interstitium, would increase lymph flow (A). It would also increase, not decrease (not C), the amount of filtration. There would be a tendency for the accumulation of fluid, yielding edema (D).
In a healthy individual, a 10 mm Hg increase in venous pressure across a skeletal muscle vascular bed will result in a decrease in the muscle’s :
A. interstitial pressure
B. interstitial volume
C. interstitial protein concentration
D. movement of fluid into its interstitial space
E. lymph flow
Answer = C. The increase in venous pressure will cause an increase in capillary pressure and, thus, increase the rate of filtration via the Starling forces. The increase in filtration will increase interstitial volume, pressure, and lymph flow; and the increase protein free fluid will dilute proteins while the increase in lymph flow will cause the interstitial protein concentration to decrease.
Movement of fluid from the capillaries to the interstitial space:
A. occurs because the capillary wall is only slightly permeable to fluid
B. occurs when the balance of forces favors filtration over reabsorption
C. requires that the capillary wall be impermeable to all solutes
D. occurs only in cases that produce edema, such as heart failure or hypertension
Answer = B. The movement of fluid from the capillaries to the interstitial space is a dynamic process that is constantly changing, depending on the moment-to-moment status of the balance of the Starling forces (hydrostatic and oncotic) causing either net filtration or net reabsorption (not D) at any particular site within the body. Although the permeability (not C) of the capillary is an important determinant of the rate of fluid movement, it does not determine the direction (not A).