Prescribing in Breastfeeding
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
52 Terms
Why does breastfeeding boost immune function?
Maternal hormones and immunoglobulins passed to baby.
Important in pre-term babies who will have delayed IgA production.
Why is IgA important in allergies?
To protect mucosal barriers and to reduce incidence of ear, GI, respiratory and UTI infections.
What are some benefits of breastfeeding for the baby?
- Reduces diarrhoea.
- Reduces anaemia.
- Reduces SIDs (sudden infant death) risk by 50%.
- Improves cognitive development.
Why does breastfeeding reduce iron-related anaemias?
Bc iron in breastmilk is more easily absorbed than if given in supplement.
What are some possible long term benefit of breastfeeding?
Reduced adult obesity, adult diabetes and adult osteoporosis.
What are some benefits of breastfeeding to the mother?
Physical benefits:
lowers blood pressure
decreases osteoporosis risk
reduces post partum blood loss
protects against breast cancer
Mental benefits:
- Improves mood - oxytocin.
- Bonding with baby.
- Convenient, flexible, cost-effective.
What is the advantage of breastfeeding for the NHS?
Improved health outcomes - fewer GP visits and hospital admissions, so less cost.
What information do we need to know about the mother when considering prescribing in breastfeeding?
- What meds are they taking?
(Dose, route, frequency, duration of treatment).
- Medical Hx.
- Are they exclusively breastfeeding or mixed?
What information do we need to know about the baby when considering prescribing in breastfeeding?
- Gestation at birth - pre or full term?
- Any renal/liver dysfunction?
- Does the baby have any medicines themselves?
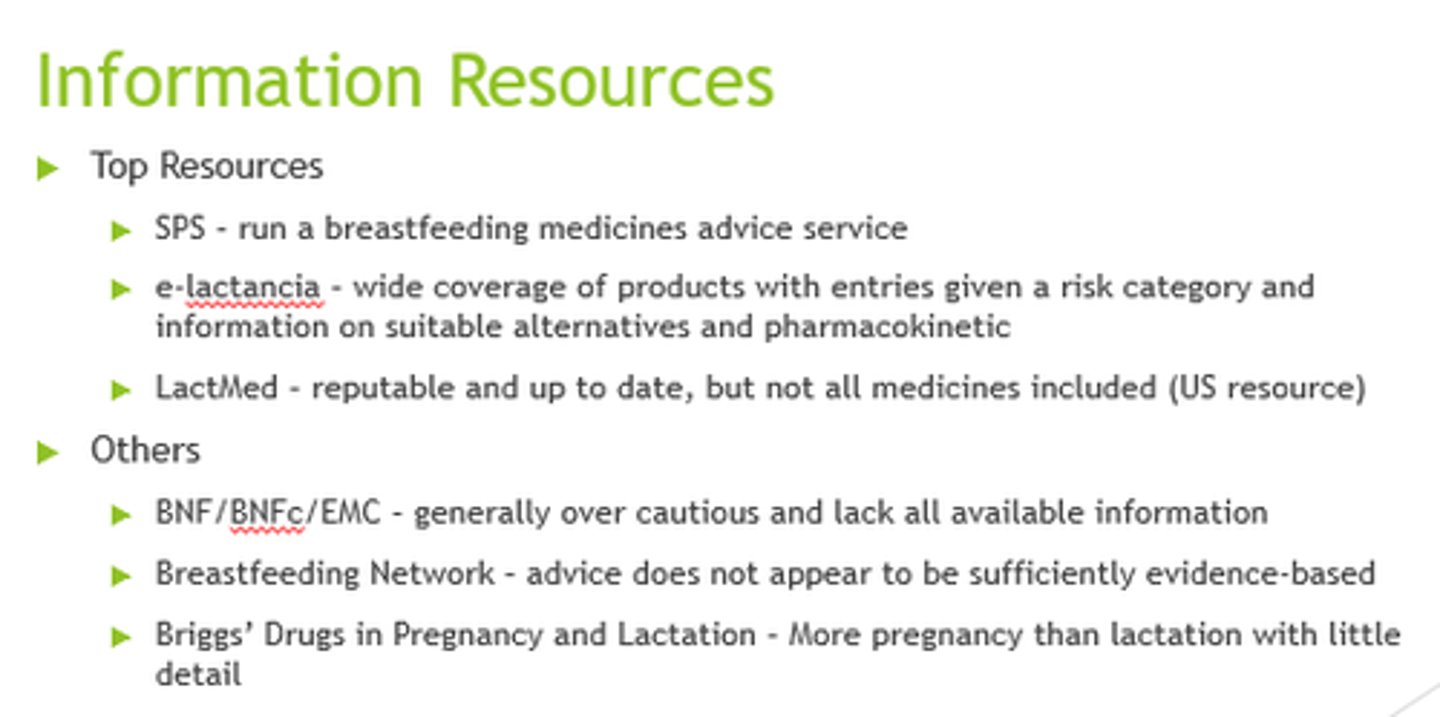
What are some key resources to use when considering prescribing in pregnancy?
- SPS (Specialist Pharmacist Service).
- E-lactancia.
- LactMed.
What are some factors to consider with medication safety in breastfeeding?
- Maternal plasma concentrations.
- BA.
- Drug properties.
- Metabolism and Elimination.
- Do we use this medication in babies?
Why do we consider bioavailability in medicine safety in pregnancy decisions?
If less orally BA, it's less likely to be absorbed via milk.
Eg insulin/vancomycin.
What kind of drug property considerations do we need to make in breastfeeding mothers?
Properties: Acid- base balance, protein binding capacity, fat solubility, MW, t1/2
Acids: weak acids don’t accumulate
Bases: weak bases ionise and accumulate in acidic milk
Protein binding: highly bound don’t pass, free drug will pass into milk
When considering metabolism and elimination, how many half lives do drugs need to undergo before it's suggested that it's safe to use?
5x t1/2s
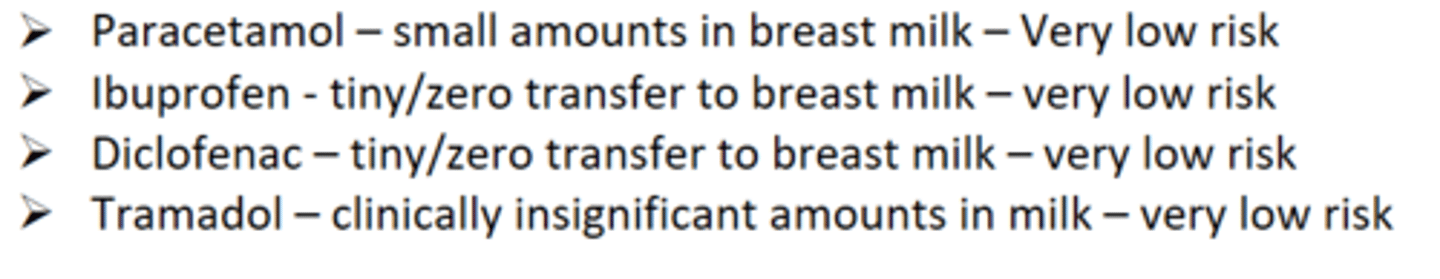
Which analgesics have very low risks in breastfeeding?
- Paracetamol.
- Ibuprofen.
- Diclofenac.
- Tramadol.
Which analgesic has a low risk in breastfeeding based on drug properties and anecdotal evidence?
Dihydrocodeine
Which is the strong opioid of choice in breastfeeding?
Morphine - lowest effective dose for shortest time. Monitor infants.
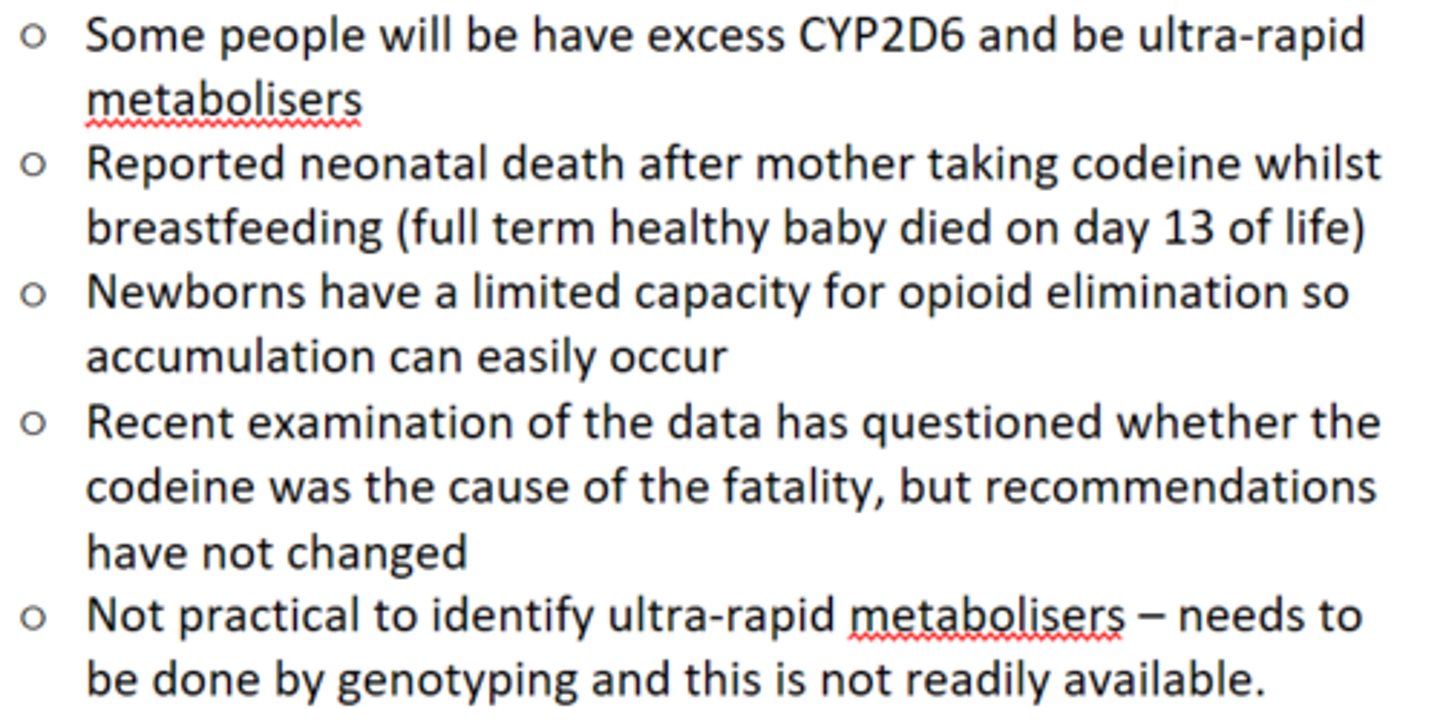
What do the MHRA advise about codeine in breastfeeding?
DON'T use codeine in breastfeeding!!
-> metabolised to morphine bia CYP2D6.
Discuss use of gabapentin in breastfeeding.
- Small molecule with low protein binding.
- So can pass into milk.
- Limited evidence, only small amounts.
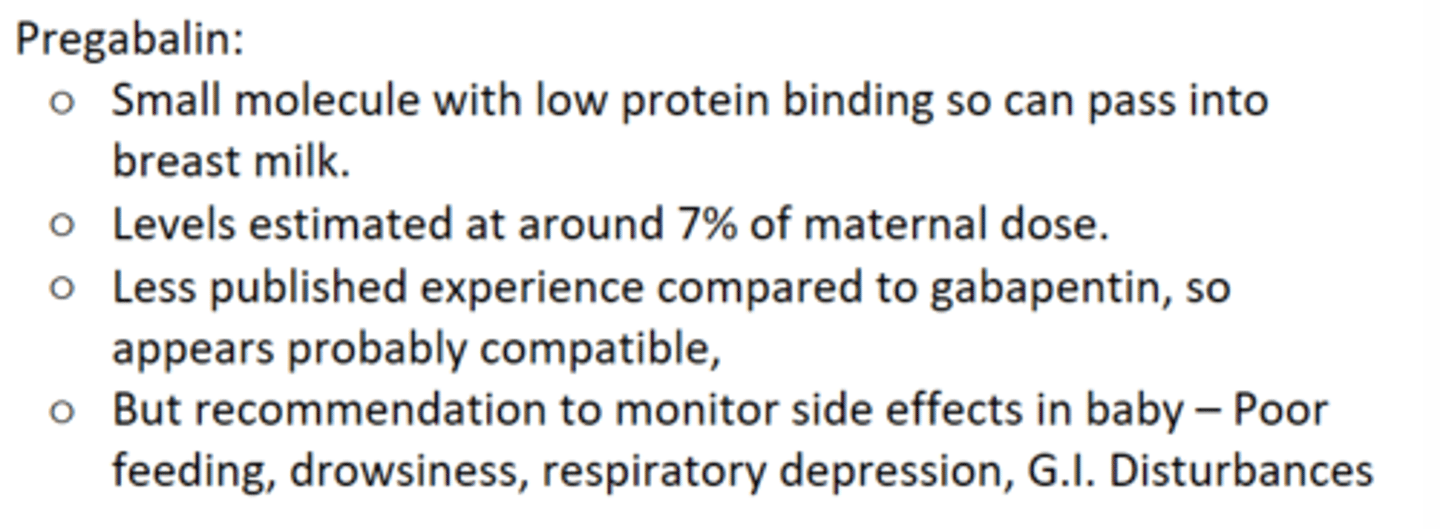
Discuss use of pregabalin in breastfeeding.
- Small molecule w/low protein binding.
- Passes into milk.
- Monitor for sfx in baby.
Discuss use of penicillins in breastfeeding.
- Fluclox, Pen V and Amoxicillin all ok.
- All acidic in nature.
- So negligible quantities pass into milk.
Discuss use of Nitrofurantoin in breastfeeding.
- Clinically insignificant excretion into milk.
- Not to be used with babies under 2 weeks, w/G6PD deficiency or jaundice.
Discuss use of Metronidazole in breastfeeding.
- Moderate amounts excreted.
- Low MW, low protein binding.
- Fully orally available.
- Short t1/2.
- OK for short courses, monitor GI effects.
- Prems/newborns can't metabolise well so use min. effective dose or see alternative.
Discuss use of gentamycin in breastfeeding.
- Excreted in insignificant amounts.
- Poorly absorbed form GIT.
- Used in neonates.
Discuss use of Macrolides eg clarithromycin/erythromycin in breastfeeding.
- Excreted in negligible amounts.
Clarith = Low risk, monitor for GI.
Eryth = Avoid in 1st month due to risk of hypertrophic pyloric stenosis.
Discuss use of SSRIs in breastfeeding.
What are the SSRIs of choice?
- Paroxetine and sertraline = SSRIs of choice.
- Bc shorter t1/2s and pass into milk in smaller amounts.
Discuss use of Tricyclic antidepressants in breastfeeding.
- Low levels bc undergo 1st pass metabolism.
- Long t1/2s can increase accummulation and increased sfx.
- Better to keep taking throughout pregnancy.
- Risk of postnatal depression.
- Baby could get withdrawal.
What are TCAs of choice in breastfeeding? Why?
- Nortriptyline and imipramine bc less sedating and reduce risk of infant sedation.
- Dulox, mirtaz, trazodone and venlafaxine can be used w/caution and monitoring.
What are the anxiolytics of choice in breastfeeding?
Short acting benzodiazepines - Eg lorazepam, oxazepam.
Use lowest effective dose.
Why might diazepam not be recommended in breastfeeding?
= Longer acting benzodiazepine.
- Excreted in clinically significant amounts.
- Risk of sedation and poor sucking in infant.
- Sedatives - effect on mother looking after baby?
What drugs should we use for sleeping disorders in breastfeeding?
Z drugs - zopiclone and zolpidem - short t1/2 and small amounts in milk.
What antipsychotics are preferred in breastfeeding?
Oral and non-depot with less sedative properties and short t1/2.
Discuss the use of olanzapine in breastfeeding.
- Doses up to 20mg od produce low levels in milk.
- Long t1/2 so monitor for accummulation signs - sedation, poor feeding etc.
Name an antipsychotic excreted in milk in variable amounts which could be clinically significant.
Haloperidol.
Discuss the use of lithium as an antipsychotic in breastfeeding.
- Excreted in moderate amounts.
- Plasma levels in infant can reach 10-60% of therapeutic levels in mother.
- Use with caution - regularly check infant for signs of lithium toxicity - monitor poor feeding, poor weight gain, changes in behaviour etc.
Discuss the use of methylphenidate in breastfeeding.
- Excreted in clinically insignificant amounts.
- No short/long-term problems observed in infants exposed.
- Monitor weight gain and irritability.
Discuss the use of Heparins in breastfeeding.
- LMHWs and UFH safe.
- High MWs so less get into breastmilk.
What is the oral anticoagulant of choice in breastfeeding? Why?
Warfarin!
- Highly protein bound so less "free" drug to pass into milk.
- But NOT used in pregancy as teratogenic.
Discuss DOAC use in breastfeeding.
Dabigatran?
Rivaroxaban?
Apixaban + Edoxaban?
Dabigatran:
- Largest DOAC.
- Large Vd.
- Passes into milk in low amounts.
- Low oral BA, so infant unlikely to absorb a lot.
Rivaroxaban:
- Small passage into milk.
- Large Vd.
- High % protein bound.
Apix/Edox:
- Not recommended.
What should we monitor the infant for is the breastfeeding mother is taking a DOAC?
Bruising and bleeding in vomit, urine or stools.
What are the beta-blockers of choice for hypertension in breastfeeding?
Labetalol, metoprolol, propranolol.
- Shorter t1/2s so lower acummulation risk.
Which beta-blocker should be used with caution in breastfeeding?
Bisoprolol!
- Low protein binding.
- High oral BA.
- t1/2 = 9-12hrs and 50% excreted in urine.
Which are the preferred CCBs of choice in breastfeeding?
Nifedipine and Verapamil.
More favourable PK.
Why do we use amlodipine with caution in breastfeeding?
- Less favourable PK.
- Long t1/2.
- High oral BA.
What is the ACEi of choice in breastfeeding?
Enalapril.
- Most favourable PK.
- Active metabolite poorly absorbed.
Which ACEi has a risk of accumulation due to a long t1/2 of 30-120hours?
Perindopril
Discuss the use of levetiracetam for epilepsy in breastfeeding.
- Variable amounts in milk.
- Infant levels low or undetectable.
- Monitor infant for drowsiness.
Discuss the use of lamotrigine for epilepsy in breastfeeding.
- Clinically significant amount in milk.
- Long t1/2 increases accumulation risk.
- Daily dose of 500mg+ may mean halting feeds.
- Monitor for rash, apnoea, drowsiness.
Discuss the use of carbamazepine for epilepsy in breastfeeding.
- Low risk.
- Suitable.
- Excreted in small amounts.
Discuss the use of phenytoin for epilepsy in breastfeeding.
- Very low risk.
- Excreted in non-significant amounts.
Discuss the use of topiramate for epilepsy in breastfeeding.
- Very low risk.
- Moderately excreted but no observed effects.
Discuss the use of valproate for epilepsy in breastfeeding.
- Very low risk.
- Excreted in insignificant amounts.
- not suitable in pregnancy due to risk of bith defects (pregnancy prevention programme 2018).