Unit 3
1/226
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
227 Terms
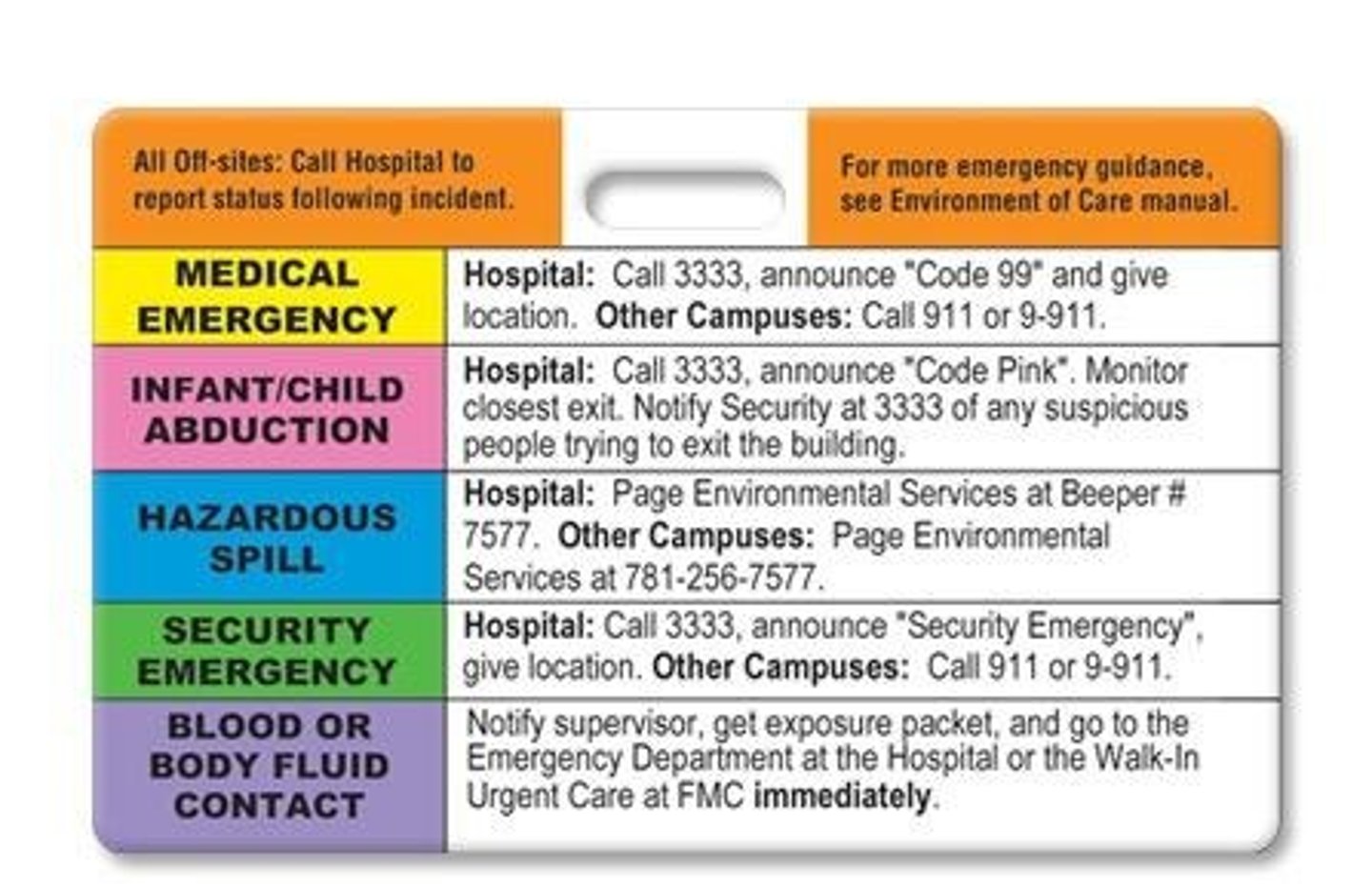
Code Blue
Cardiac Arrest: call a code, get the 'crash cart.'
Code Grey
security
Code Red
fire.
Code Pink/Secure
infant abduction.
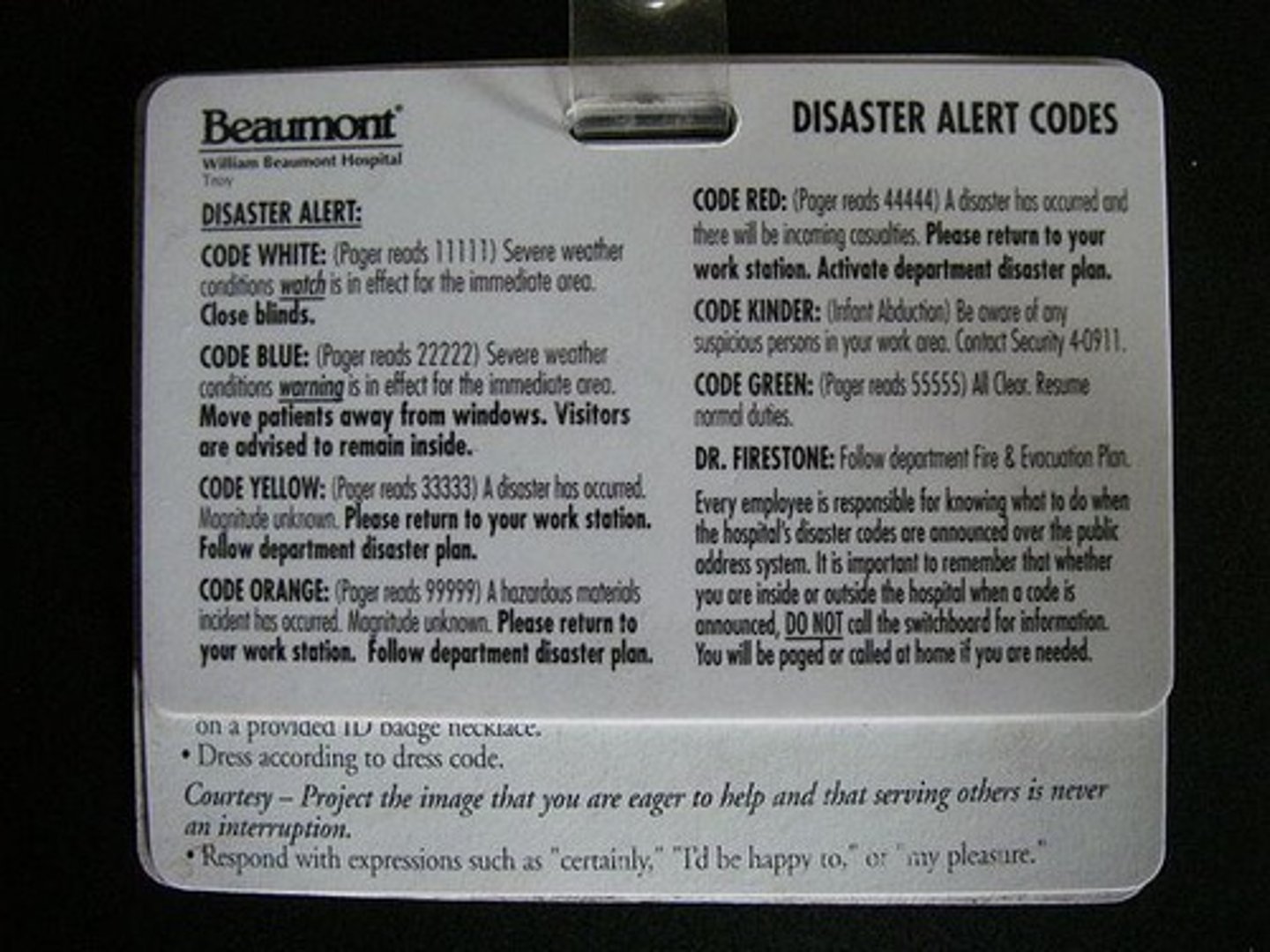
Code Purple
child abduction.
Code Orange
hazardous material spill.
Code Green
incoming cardiac arrest.
Code Triage
internal/external disaster.
Code Yellow
bomb threat.
Code White
pediatric medical emergency.
Code Silver
person with weapon or hostage situation.
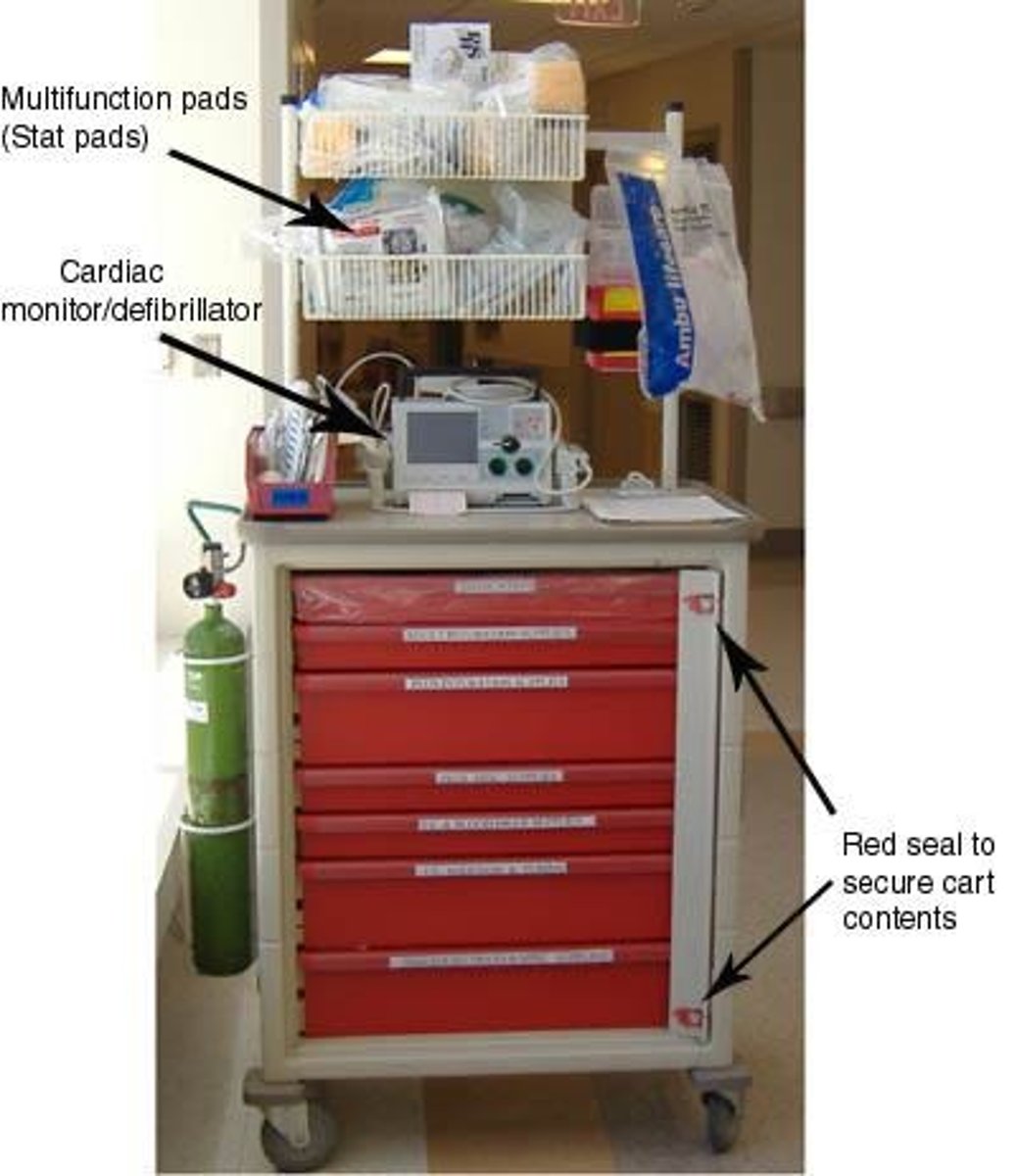
CRASH CART
Located where IV contrast are administered. Contains emergency medicines, supplies, and other life sustaining equipment.
Crash cart Red Seals
Must be checked daily to make sure they are sealed
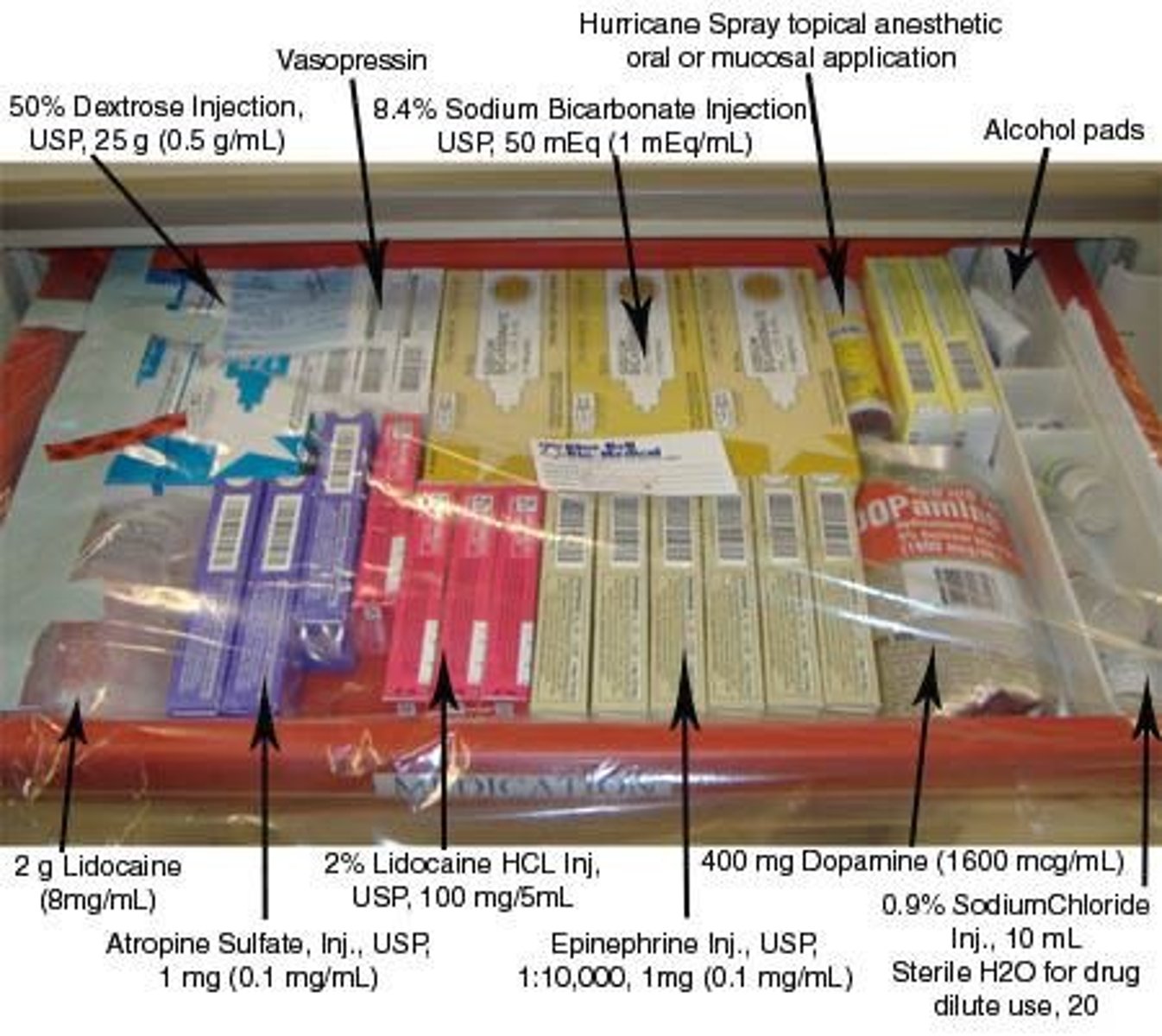
Epinephrine
for severe anaphylaxis. Vasoconstrictor which increases contractility and BP. Make heart more sensitive to electrical conduction
Vasopressin
maintains water, constricts blood vessels
Sodium Bicarbonate
maintains pH balance
Atropine
indicated for cardiac arrest patients suffering from bradycardia or worst case, asystole.
Lidocaine
used for V-Tach, PVCs.
Dopamine
vasodilator, increases contractility and blood flow.
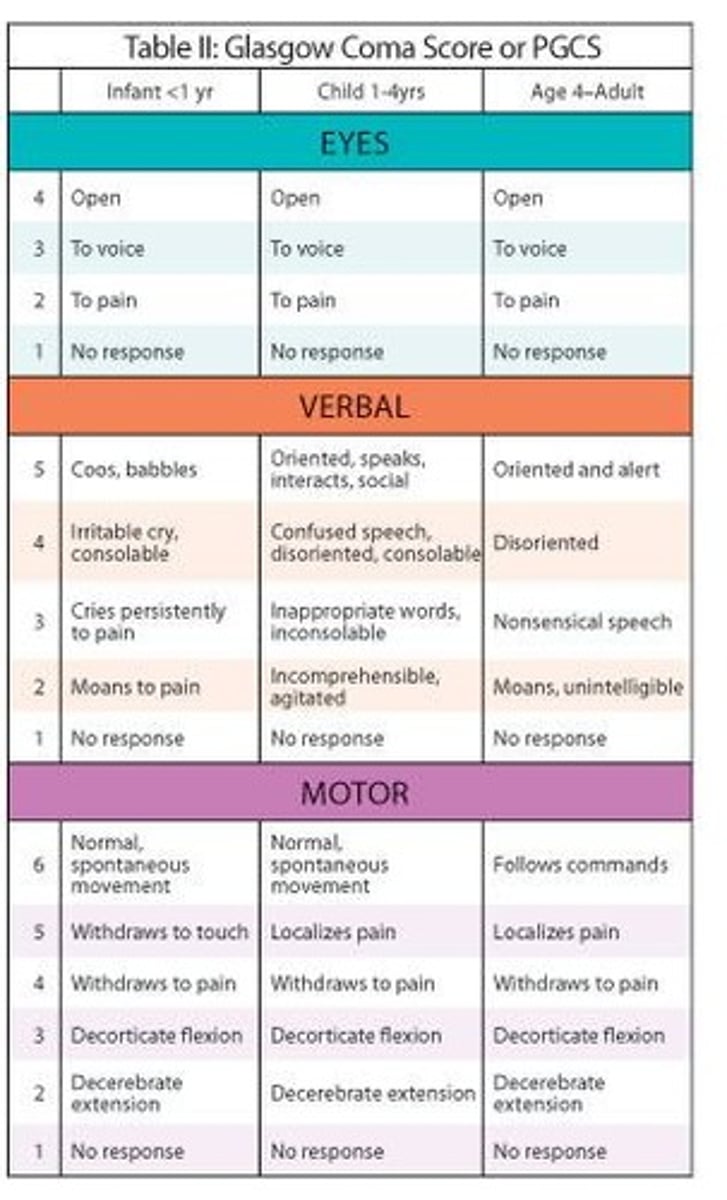
Glasgow Coma Scale
Three areas can be readily observed, each work 1-6 points for total of 15. Score 7 points or less is dangerous
1. Eyes opening
2. Motor response
3. Verbal response
Loss of Consciousness
Ask the patient to state his/her name, date, address, & the reason for coming to the radiology department to learn if he/she responds to verbal stimuli, & that he/she is oriented to time, place, person & situation.
Shock
An acute medical condition associated with a fall in blood presure
Stages of Shock
Compensatory, Progressive, Irreversible
Compensatory symptoms of Shock
-Skin is cold and clammy
-Nausea and Dizziness
-increased respirations
-Anxiety level increases; patient may begin to be unco-operative
-BP is decreased and pulse rate is increased
Progressive symptons of shock
-Significantly decreased blood pressure with an increase in pulse rate
-respirations are rapid and shallow
-pulmonary capillaries leak fluid into the lungs, causing severe pulmonary edema, known as acute respiratory distress or shock lung
-Tachycardia results and may be as rapid as 150 bpm
-chest pain
-mental status begins to change, confusion, progression to lethargy and loc
-renal, hepatic, gastrointestinal, and hematologic problems occur
Irreversible symptoms of shock
-Blood pressure remains low
-renal & liver failure results
-release of necrotic tissue toxins & an overwhelming lactic acidosis.
Causes of shock
-Bleeding
-Under physical or emotional stress
-Has a serious injury or infection
-Is vomiting or has diarrhea
-Has any form of diabetes
-Is very young or very old
-Is experiencing severe pain
-Has a bowel obstruction
-Is undergoing any procedure that causes rapid decompression of an organ or rapid fluid loss from a body cavity
-Has undergone anesthesia.
Types of Shock
-Hypovolemic shock
-Cardiogenic shock
-Distributive shock
-Neurogenic shock
-Septic shock
-Anaphylactic shock
-Obstructive shock.
Hypovolemic shock
Caused by an abnormally low volume of circulating blood in the body. If intravascular fluid decreases by 15 to 25% or by loss of 750 to 1,300 milliliters
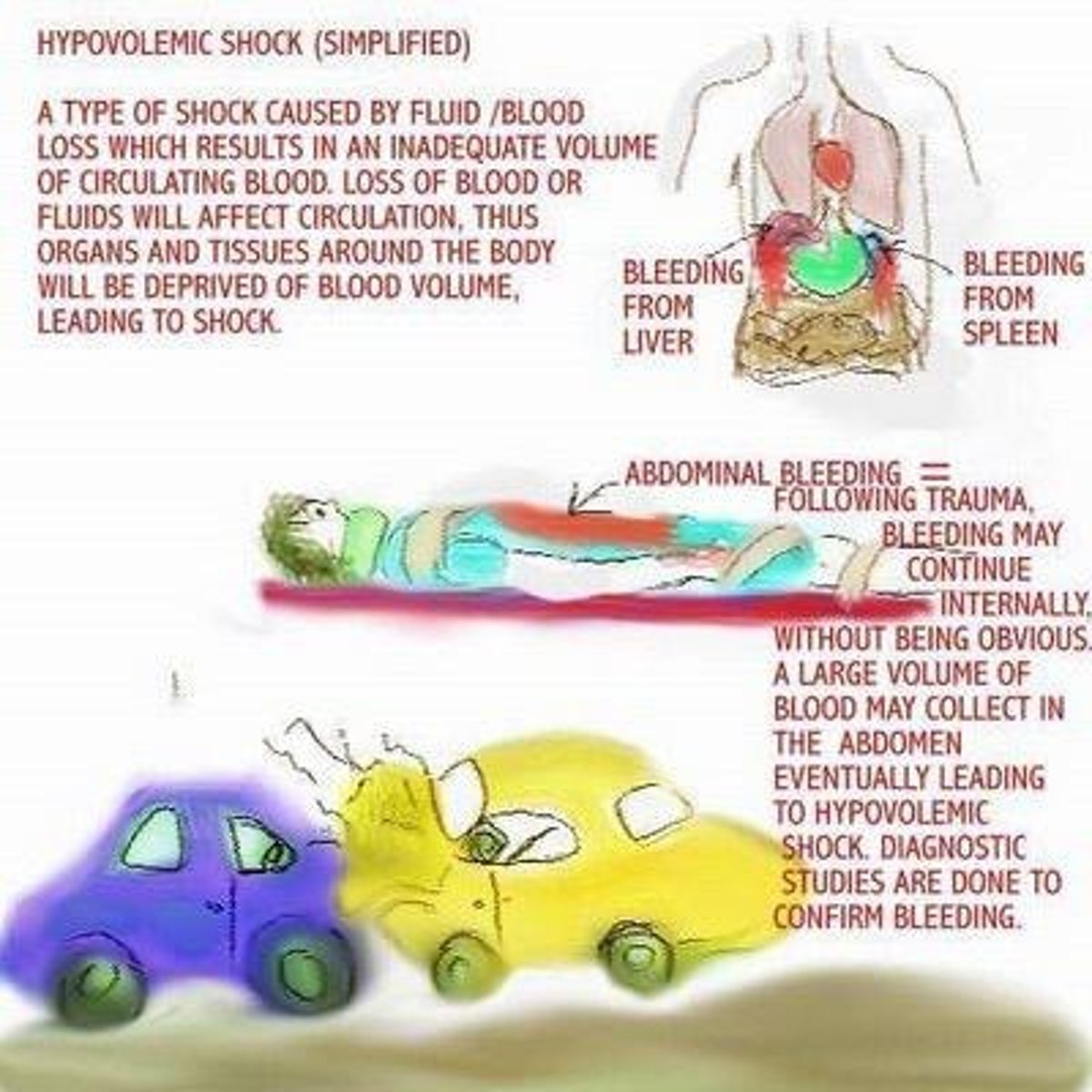
Causes of hypovolemic shock
-May be due to internal or external hemorrhage
-loss of plasma from burns
-fluid loss from prolonged vomiting
-diarrhea, medications or heat prostration (stroke).
Class I hypovolemic shock
-Blood loss of 15%
-BP is within normal limits
-HR is less than 100 bpm
-Respiration ranges from 14 to 20 per minute
Class II hypovolemic shock
-Blood loss of 15%-30%
-BP is within normal limits
-HR is greater than 100 bpm
-Respiration ranges from 20 to 30 per minute
Class III hypovolemic shock
-Blood loss of 30% to 40%
-BP begins to decrease to below normal limits
-HR is greater than 120 bpm
-Respiration increases to 30 to 40 per minute
Class IV hypovolemic shock
-Blood loss of 40% or more
-systolic BP decreases from 90 to 60 mm Hg
-HR is now tachycardia with a weak and thready pulse
-Respiration is greater than 40 per minute
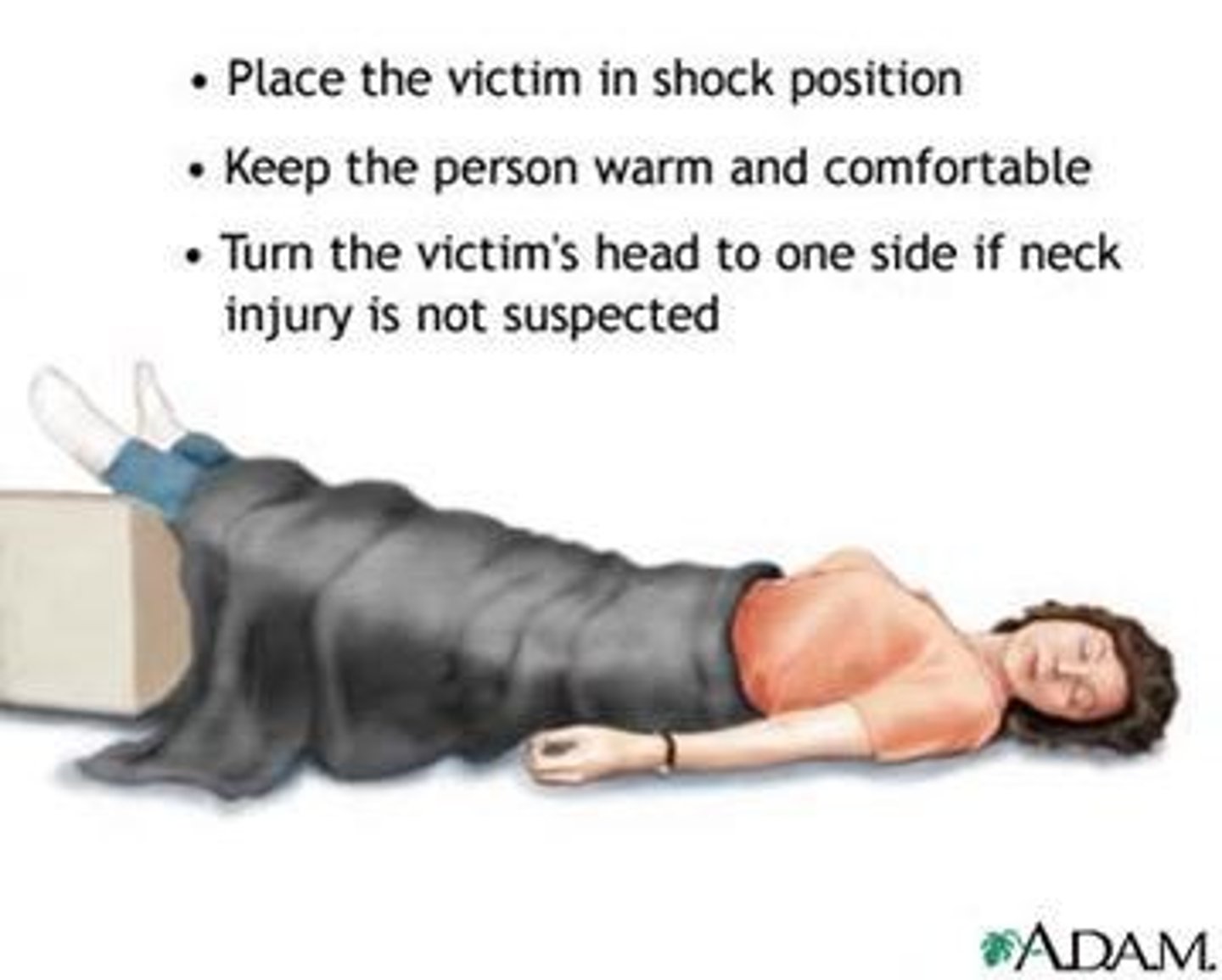
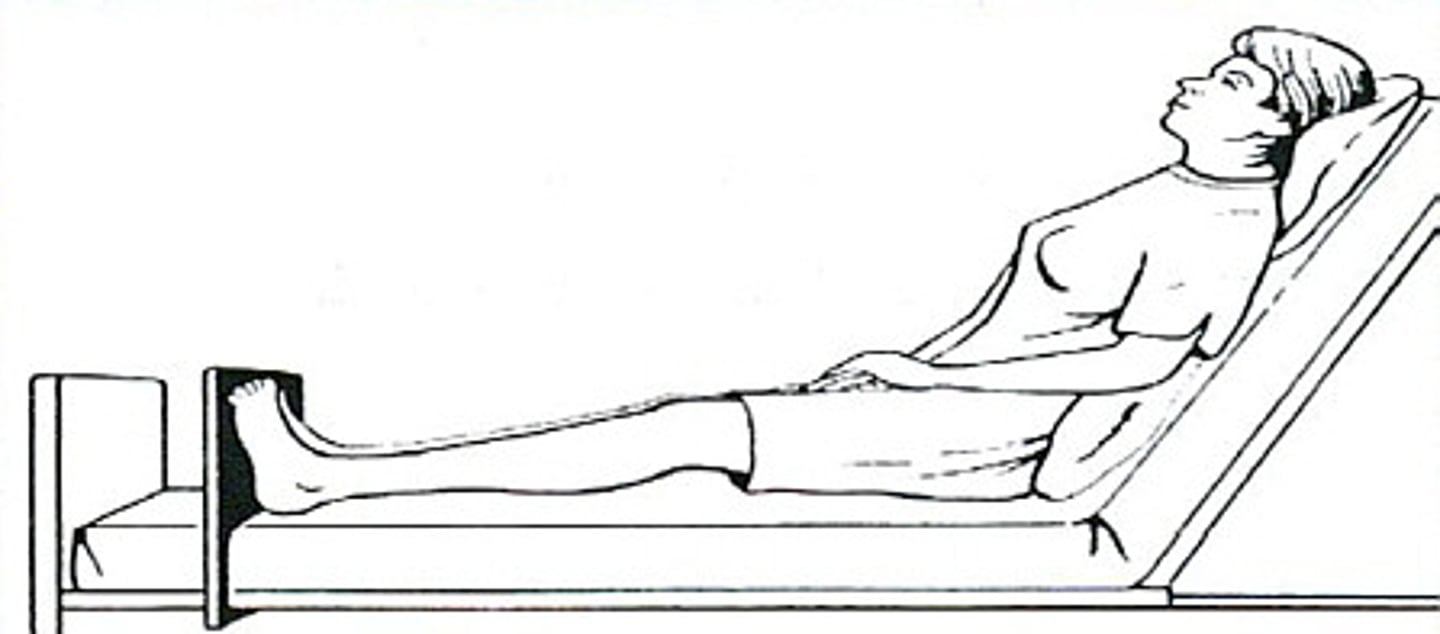
RT Actions for hypovolemic shock
-Stop the procedure
-place the patient in a supine position with legs elevated 30 degrees (unless there is a spinal cord injury). Do not place the patient in a Trendelenburg position
-notify the physician & call for emergency action
-make certain that the patient is breathing without airway being obstructed by position, blood or mucus
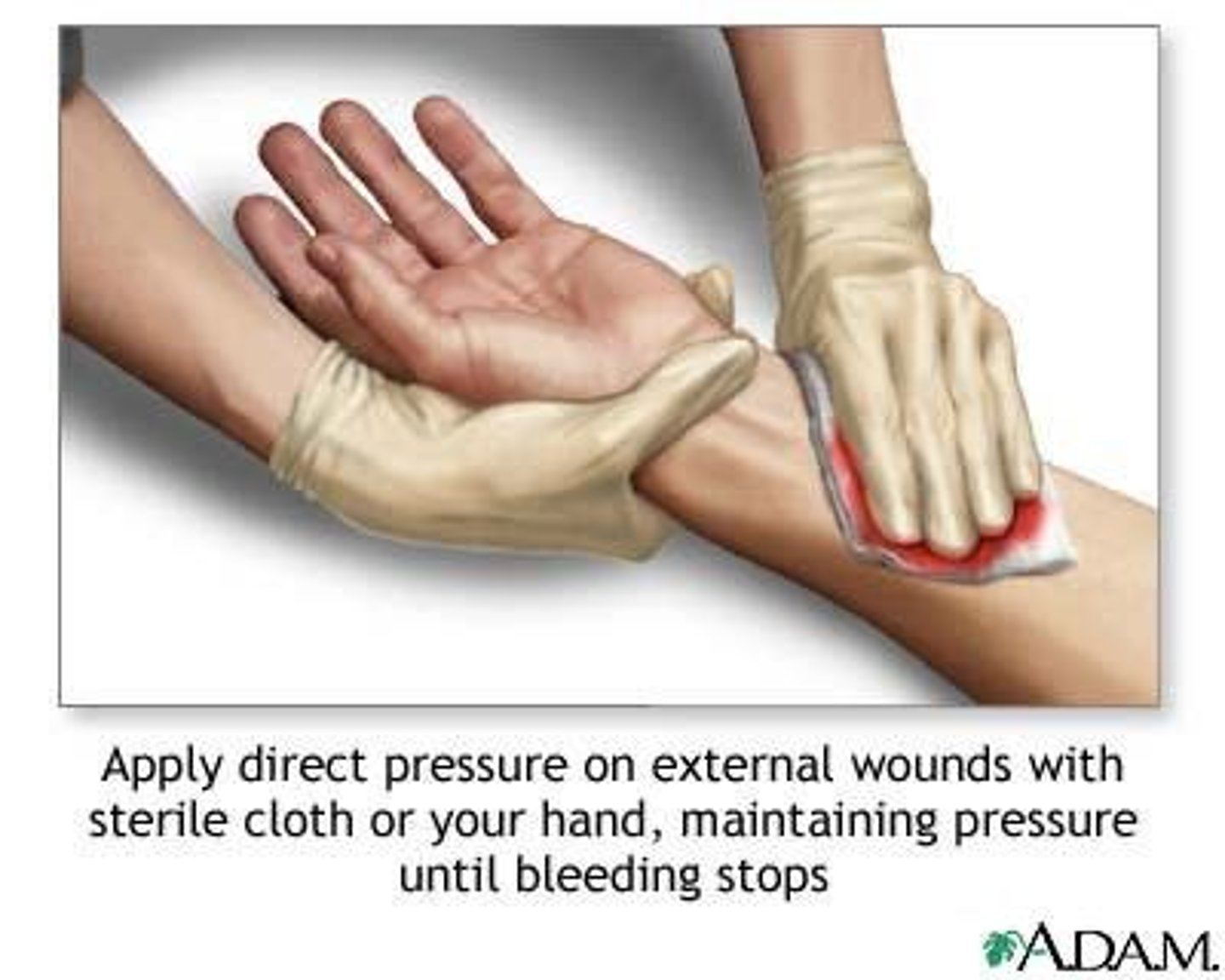
-if patient is bleeding apply direct pressure to the wound with sterile dressing
-get the crash cart.
Preparation for hypovolemic shock
-Prepare to assist with oxygen, IV fluids & meds.
-Have a large gauge IV catheter on hand
-keep the patient warm & dry.
-Do not overheat because it causes increased metabolism (need O2)
-take vital signs every 5 minutes
-do not leave the patient unattended.
-Keep them informed to prevent anxiety
-do not offer fluids to the patient.
Cardiogenic shock
Caused by a failure of the heart to pump adequate amounts of blood to vital organs.
Causes of cardiogenic shock
Patient hospitalized by myocardial infarction, cardiac dysrhythmias or other cardiac pathology.
Clinical manifestations of cardiogenic shock
-Complaint of chest pain that radiates to jaws & arms
-dizziness & respiratory distress
-Cyanosis
-restlessness & anxiety
-rapid change in LOC
-irregular & slow pulse
-tachycardia & tachypnea
-hard to evaluate carotid pulse
-decreasing blood pressure
-decreasing urinary output
-cool
-clammy skin
RT Actions for cardiogenic shock
-Call a Code & get the crash cart
-notify patient's physician
-place the patient in Semi-Fowler's position
-prepare to assist with oxygen
-IV fluids and meds
-do not leave patient alone-
-assess vital signs every 5 minutes
-do not offer fluids
-be prepared to administer CPR.
Distributive shock
Occurs when a pooling of blood in the peripheral vessels results in decreased venous return of blood to the heart, decreased blood pressure, & decreased tissue perfusion.
Types of distributive shock
Neurogenic and septic.
Neurogenic shock
Results from loss of sympathetic tone causing vasodilation of peripheral vessels.
Causes of neurogenic shock
-Spinal cord injuries
-severe pain
-neurologic damage
-depressant action of medication
-lack of glucose
-adverse effects of anesthesia.
Clinical manifestations of neurogenic shock
-Hypotension
-bradycardia
-warm
-dry skin
-initial alertness if not unconscious
-cool extremities & diminishing peripheral pulses.
RT Actions for neurogenic shock
-Summon emergency assistance
-notify the MD in charge
-keep the patient in supine position
-have emergency cart brought to the patient's side,
-do not move the patient if spinal cord injury is possible
-stay with the patient and offer support
-monitor vital signs every 5 minutes
-prepare to assist with oxygen
-IV fluids and medications.
Septic shock
Has a 40-50% mortality rate for its victims, and occurs within 12 hours. Least likely to be observed by RT
Septic Shock
A condition resulting from systemic infection by bacteria leading to shock syndrome characterized by increased capillary permeability and vasodilatation.
Clinical Manifestations of Septic Shock - First Phase
-Hot, dry, & flushed skin
-increased heart rate & respiratory rate
-fever (possibly absent in elderly)
-nausea, vomiting & diarrhea
-normal-to-excessive urine output
-possible confusion.
Clinical Manifestations of Septic Shock - Second Phase
-Cool, pale skin
-normal or subnormal temperature
-drop in blood pressure
-rapid heart rate & respiratory rate
-oliguria or anuria
-seizures & organ failure if syndrome is not reversed.
RT Actions for Septic Shock
-Stop the procedure
-notify the MD
-notify the ER team & get the crash cart
-place the patient in supine position
-keep the patient calm & quiet
-monitor vital signs every 5 minutes.
Risks for Septic Shock
-Advanced age/very young
-recent surgery
-reinsertion of a urinary catheter
-chronic diseases (diabetes, COPD, renal failure)
-immunosuppressed patients
-malnutrition
-massive burns or traumatic injuries
-indwelling catheter or prosthesis
-GU tract or biliary tree surgery.
Obstructive Shock
Shock resulting from pathologic conditions that interfere with the normal pumping action of the heart, unrelated to heart pathologies.
Pulmonary Embolism
A blockage in one or more pulmonary arteries caused by blood clots that usually originate in the venous circulation.
Anaphylactic Shock
An exaggerated hypersensitivity reaction to an antigen previously encountered by the immune system, causing vasodilatation and dyspnea.
Causes of Obstructive Shock
Includes pulmonary embolism, pulmonary hypertension, arterial stenosis, constrictive pericarditis, and tumors that interfere with blood flow through the heart.
symptoms of pulmonary embolism
-Chest pain
-rapid weak pulse
-hyperventilation
-dyspnea & tachypnea
-tachycardia, apprehension
-cough & hemoptysis
-diaphoresis, syncope
-hypotension
-cyanosis
-rapidly changing levels of consciousness
-coma.
RT Actions for Pulmonary Embolism
-Stop the procedure immediately
-notify the physician
-monitor vital signs
-do not leave the patient alone
-prepare to assist with oxygen, IV fluids, and medication administration.
Causes of Anaphylactic Shock
Includes medications, iodinated contrast, insect venoms, and requires pre-procedure checks for allergies and stocking of emergency medications.
Questions to Ask Patients Before Iodinated Contrast
Are you allergic to any food or medicine?
Which ones?
Do you have asthma or hay fever?
Have you ever had hives or other allergic skin reactions?
Have you ever had an exam using contrast media?
Did you have a reaction during/following that exam?
Vital Signs Monitoring Frequency in Septic Shock
Monitor vital signs every 5 minutes.
Immediate Actions for Anaphylactic Shock
-Stop the procedure immediately
-call for help, notify the physician
-monitor vital signs
-do not leave the patient alone
-prepare to assist with oxygen
-IV fluids
-medication administration.
Effects of Histamine in Anaphylactic Shock
Causes vasodilatation, dyspnea, hypotension, increased permeability of small blood capillaries, and incites pain.
Effects of Bradykinin in Anaphylactic Shock
Influences smooth muscle contraction in the respiratory tract, inducing hypotension and increasing permeability of small blood capillaries.
Anaphylactic Shock Mild Systemic Reaction
Symptoms beginning within 2 hours of exposure to antigen including nasal congestion, periorbital swelling, itching, sneezing & tearing of eyes, peripheral tingling or itching at the site of injection, and feeling of fullness or tightness of the chest, mouth, or throat.
Anaphylactic Shock Moderate Systemic Reaction
All symptoms listed in mild systemic reaction with rapid onset, including flushing, feeling of warmth, itching, urticaria, anxiety, bronchospasms & edema of the airways of larynx, dyspnea, cough & wheezing.
Anaphylactic Shock Severe Systemic Reaction
All symptoms listed in previous reactions with an abrupt onset, including decreasing BP, weak, thready pulse either rapid or shallow, rapid progression to bronchospasm, laryngeal edema, severe dyspnea & cyanosis, dysphasia, abdominal cramping, vomiting & diarrhea, seizures, respiratory and cardiac arrest.
Anaphylactic Shock Timeframe for Reaction
Any mild reaction can become a major reaction within 2 - 3 minutes.
RT Actions to Anaphylactic Shock
-Do not leave the patient alone
-Stop the injection or infusion immediately
-notify a radiologist if the patient complains of itching, redness, or swelling of the skin, or seems unduly anxious.
-If the patient complains of respiratory distress or has any symptoms, call the emergency team.
-Place the patient in Semi-Fowler's position or in a sitting position to facilitate respiration.
-Monitor vital signs every 5 minutes until the emergency team arrives.
-Prepare to assist with oxygen, IV fluid and medication administration. Have large gauge venous catheter available.
-Prepare to call a CODE BLUE
-Prepare to administer CPR
Anaphylactic Shock Emergancy Management
Establish airway and start:
- Epinephrine/adrenaline- vasopressor: increases BP, heart rate -cardiac output
-Oxygen therapy
-IV saline 0.9 %
-Tourniquet above injection site to prevent absorption
-Antihistamines- Benadryl
-Aminophylline -IV slowly for patients with severe bronchospasms &
asthmatic symptoms only - respiratory stimulant, myocardial stimulant
-Vasoconstrictors- raise BP
-Drugs for reduced cardiac output
-Watch for arrhythmias and arrest
-Convulsions- give IV short acting barbiturate
-Prolonged reaction- corticosteroids (Solu-cortef) suppresses immune response, decreases inflammation
Observation Period
The patient remains in the department for 30 minutes for observation if not an in-patient.
Iodine Reaction Definition
Contrast agents are categorized as drugs because they can be absorbed into the systemic circulation & may affect a physiologic response.
Transient Response Symptoms
A warm flushed feeling from a rapid bolus injection, nausea &/or vomiting usually passes quickly, headache, pain or burning at injection site, metallic taste.
Iodine Reaction Severity Levels
Reactions can be classified as Mild, Moderate (intermediate), or Severe.
Iodine overdose symptoms
80 to 90g of iodine may produce symptoms of tremors, irritability, & tachycardia.
General contrast procedures average
.05 to 0.2g of iodine.
Contrast administration temperature
All contrast should be administered at body temperature.
Contrast solution clarity
All solutions administered should be clear.
Iodinated contrast protection
Protect iodinated contrast from exposure to light.
Discard unused contrast
Discard all unused contrast that has been opened.
Mixing contrast
Do not mix contrast with other drugs or other contrast.
Diabetes mellitus
A disorder of carbohydrate, protein, & fat metabolism affecting blood vessels.
Normal adult blood glucose level
Should range from 80 to 115 mg/dL.
Type 1 Diabetes Mellitus
Insulin dependent; body stops producing insulin, abrupt onset, under age 30.
Type 2 Diabetes Mellitus
Gradual onset, over 40 who are obese; may be controlled by weight loss, dietary control, and exercise.
Ketoacidosis
Diabetic ketoacidosis (DKA) is a serious condition that can lead to diabetic coma or even death. It occurs when cells don't get the glucose they need for energy, causing the body to burn fat for energy, producing ketones.
Type 2 Diabetes
A condition where the body isn't able to use insulin properly, leading to insulin resistance and possibly insulin deficiency as the pancreas produces less insulin.
Insulin Resistance
A condition where the body's cells do not respond effectively to insulin, making it difficult for the body to use glucose.
Insulin Deficiency
A condition where the pancreas produces less insulin, which can worsen as type 2 diabetes progresses.
Gestational Diabetes
A type of diabetes that occurs in the later months of pregnancy, caused by hormones from the placenta that prevent the action of insulin.
Hyperglycemia
A condition characterized by high blood glucose levels, often greater than 600 mg/dL, which can lead to complications such as coma.
Three Major types of diabetes mellitus
-Type 1 diabetes mellitus (insulin dependent)
-Type 2 diabetes mellitus
-Gestational diabetes
Normal Blood Glucose Levels
Normal blood glucose levels range from 80 to 115 mg/dL.
Clinical Manifestations of Hyperglycemia
Symptoms include extreme dehydration, dry skin, sunken eyes, hypotension, tachycardia, increased body temperature, extreme thirst, muscle twitching, slurred speech, mental confusion, seizures, hemiparesis, and coma.
Ketoacidosis Clinical Manifestations
Symptoms include weakness, drowsiness, headache, blurred vision, abdominal pain, nausea, vomiting, sweet odor to the breath, orthostatic hypotension, warm dry skin, parched tongue, dry mucous membranes, extreme thirst, polyuria, general weakness, lethargy, flushed face, deep rapid respirations, tachycardia, and coma.
Hypoglycemia
A condition that occurs when there is an excess amount of insulin or oral hypoglycemic drug in the bloodstream, an increased rate of glucose use, or inadequate food intake, leading to blood glucose levels falling below 50 to 60 mg/dL.
RT Response for Hyperglycemia
Call for emergency assistance, notify the physician, monitor vital signs, and prepare to administer IV fluids, medications, and oxygen.
RT Response for Ketoacidosis
Check patient's chart or ID bracelet, stop treatment, notify MD, call for help, do not leave patient unattended, monitor vital signs, and prepare to assist with IV fluids, medications, and oxygen.
Diabetes Mellitus
A group of diseases that result in high blood sugar (too much glucose) due to insulin resistance, insulin deficiency, or both.
Diabetic Coma
A serious condition resulting from uncontrolled diabetes, where a person becomes unconscious for an extended period.