Week 1 - Pacemaker and conduction of the heart
1/81
Earn XP
Description and Tags
Pacemaker and Conduction SDL, preload, afterload and contraction and finally cardiac output
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
82 Terms
what is the annulus fibrosis
4 interconnected rings of fibrous connective tissue b/w atria and ventricles
acts as an electrical insulator
what does the annulus fibrosis ensure?
AP from the SAN only reach the ventricles via the AVN
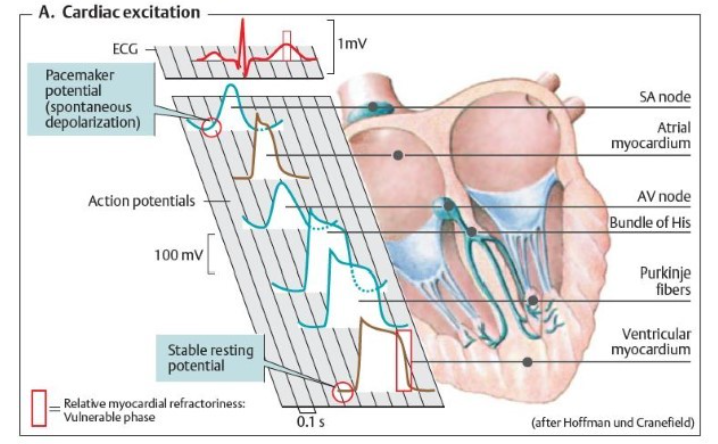
How does conduction of the myocardium work?
SAN cells depolarise by themselves = automaticity
Myocytes are connected via gap junctions so more depolarise and they take a ‘highway’ which sends this electrical impulse to the left atrium = Bachmann’s bundle
atrial systole
Wave of depolarisation reaches the AVN
travels down bundle of His, through a left and right bundle down the septum
fibres branch from the apex of the heart through the Purkinje fibres
Via what tracts does the wave of depolarisation reach the AVN?
intranodal: 3 of them
What causes the ventricles to contract after the atria and why?
AVN causes a delay of around 0.1 seconds
This ensures the atria empty fully and if it wasn’t delayed it would cause the atria and ventricles to push blood against each other
what is function the SAN
Initiation of the depolarisation of the atria
what is the function of the AVN
delaying the wave of depolarisation to ensure complete contraction of the atria and that blood flows in the same direction
what is the function of the bundle of His
where the wave of depolarisation travels down to ensure contraction of the ventricles starts at the apex of the heart
What is the function of the purkinje fibres
ensure complete contraction of the ventricles from the apex of the heart
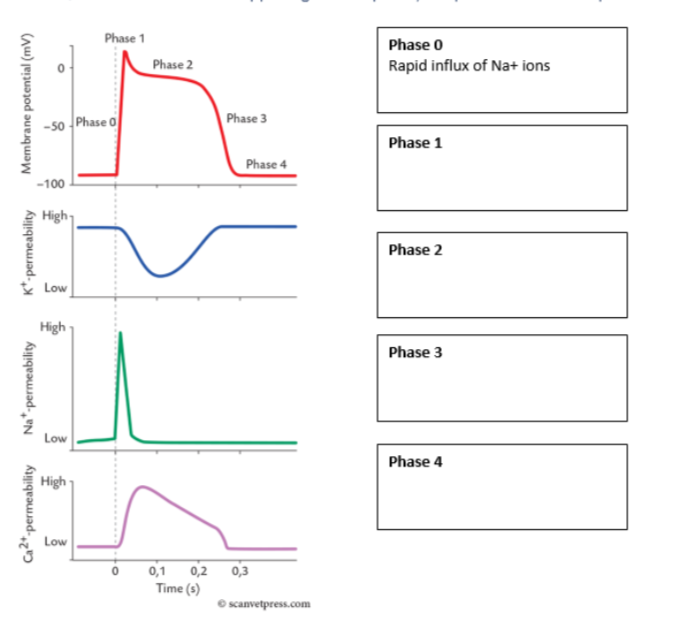
How many phases of AP in cardiomyocytes are there?
5 (phase 0-4)
What are the stages of AP generation in cardiomyocytes
0 = influx of Na+ ions
1 = potassium channels first open up, decrease in mV due to outflux
2 = Ca2+ influx is balanced with K+ outflux, stays balanced
3 = Ca2+ influx stops, only K+ outflux, decrease in mV
4 = resting potential, ~-90mV
what kind of cells are in the SAN, AVN, Bundle of His and Purkinje fibres?
autorhythmic cells
this means they have automaticity
what can autorhythmic cells do?
spontaneously generate AP
how do autorhythmic cells generate AP
undergo slow depolarisations until a threshold potential is reached
most rapid in the SAN
Outline the 5 stages of AP generation in the SAN
ion channels open that are permeable to both Na+ and K+ which causes a small influx of Na+ ions = If current
Ca2+ channels begin to open
further Ca2+ channels open
K+ channels activated allowing efflux of K+
K+ channels close and If channels open
Like a normal AP generation but with more involvement Ca2+ ions
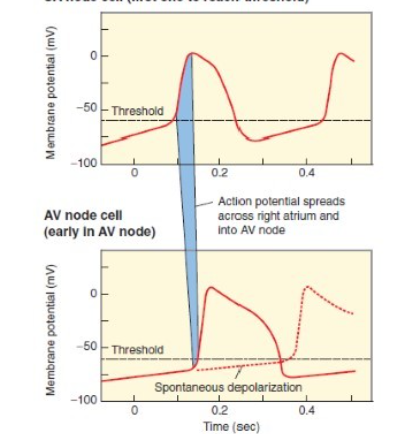
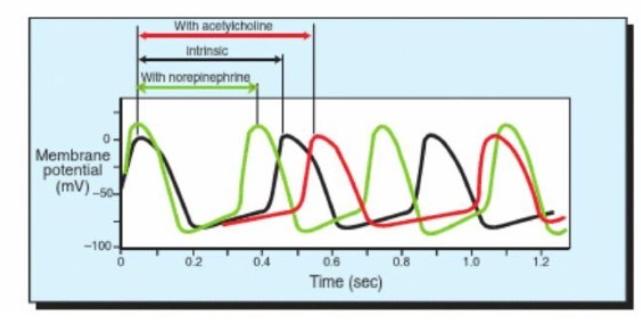
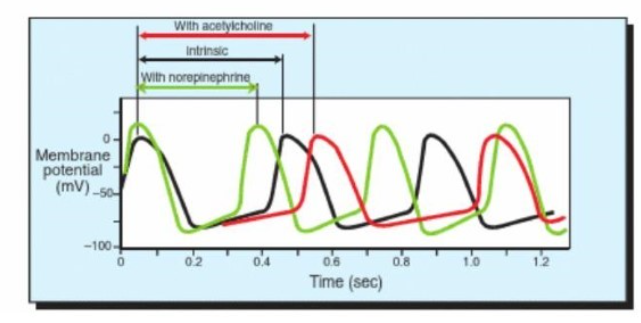
Explain what this diagram represents
The SAN reaches the threshold before AVN
arrival of AP from the SAN speed up the cells of the AVN into reaching the threshold
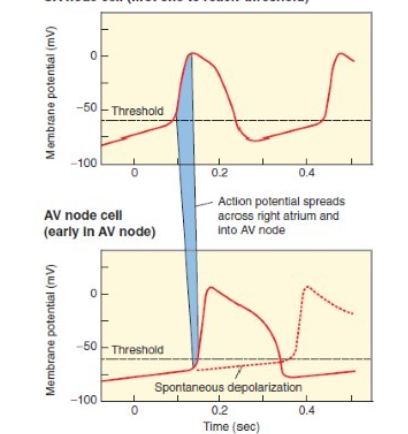
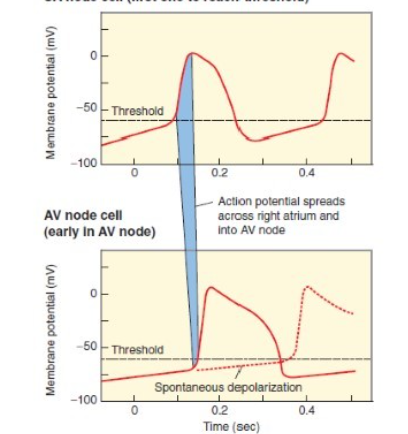
if the SAN wasn’t working, what would happen to AVN?
would eventually spontaneously depolarise but at a slower rate
Describe the effects of the parasympathetic nervous system on the SAN and AVN
ACh decreases rate of depolarisation, lengthening the intervals b/w action potentials = parasympathetic NS decreases heart rate
activates muscarinic cholinergic receptors on the pacemaker cells
slows ion channel changes
takes longer for the cells to reach the threshold → longer interval b/w heartbeats
heart rate is decreased below its intrinsic or spontaneous level
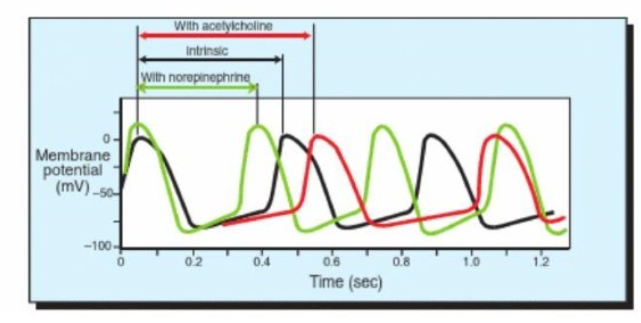
Describe the effects of the sympathetic nervous system on the SAN and AVN
NE/NA increases the rate of depolarisation and therefore shortens the interval b/w AP = sympathetic nervous system increases HR above intrinsic spontaneous level
activates Beta-adrenergic receptors
speeds up ion channel changes
enables SAN cells to reach threshold more quickly therefore there’s a shorter interval b/w heartbeats
why is it important both nodes have automaticity?
if one is damaged/doesn’t depolarise to threshold, the other can still propagate
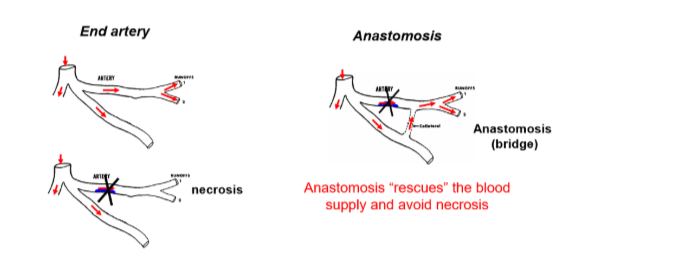
why does the AVN have a longer refractory period?
helps protect the ventricles from being stimulated to contract at rates that are too rapid for efficient contraction
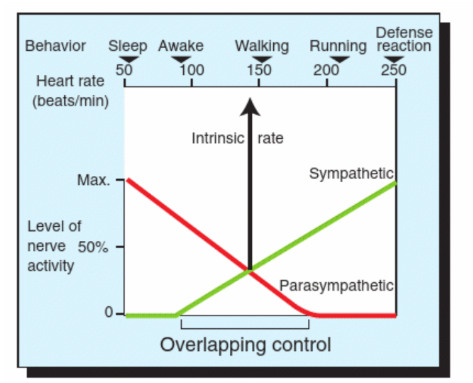
How are heart rates below the intrinsic rate achieved
by the parasympathetic neurones
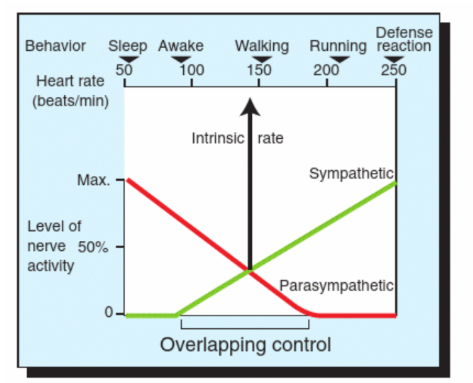
how are heart beats above the intrinsic rate able to occur?
during exercise or emotional arousal due to the sympathetic nervous system
why does the parasympathetic nervous system not influence the ventricular muscle cells?
less innervation in the ventricles
how can the parasympathetic nervous system have an effect on the ventricular myocytes
inhibits NE release from the sympathetic neurone terminals by releasing ACh
what is an ECG used for?
summarising the depolarisation spread through the heart
what lead type is being used to produce the rest ECG
lead II
What is stroke volume
the volume of blood pumped by the heart for each cardiac cycle
what affects the amount of blood delivered to the tissues?
stroke volume
heart rate
vascular tone
what makes up cardiac output
stroke volume
heart rate
what affects blood pressure
vascular tone
what is cardiac output
CO (ml/min) = HR(bpm) x SV (ml/beat)
the volume of blood pumped by the heart in one minute
Does the CO from the LV and RV differ?
no they’re matched
the heart automatically pumps whatever volume of blood is put into it
stroke volume must be matched, therefore vol entering lungs = vol entering systemic circulation
why can’t we have different SV from each ventricle?
increase in P in venous side
leads to oedema (pulmonary or peripheral)
CO is tightly regulated by a range of mechanisms as a result
how is CO regulated?
Cardiac output: heart rate and stroke volume
stroke volume is regulated by preload, afterload and contractility
what is preload
EDV: end diastolic volume (in the ventricles)
intrinsic regulation
what is contractility
ESV: end systolic volume
affected by SNS
extrinsic regulation of stroke volume
what is afterload
resistance to ventricular ejection
what is preload dependent on
dependent on venous return of blood i.e. central venous pressure
what happens if preload is low
ventricular filling is reduced, thus stroke volume is reduced
because preload is dependent on venous return of blood
what happens if preload is high
ventricular filling is increased, hence stroke volume increases
because preload is dependent on venous return
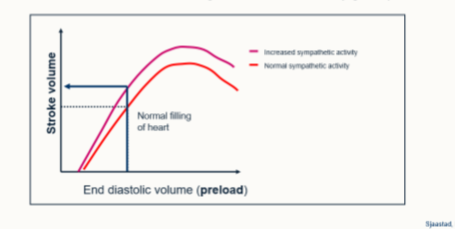
what is the Frank-starling mechanism
a linear relationship between preload and stroke volume
ventricular muscle stretching leads to a stronger contractile force
Outline the process of the length-tension relationship
increased preload
increased exposure of myosin to actin
increased cross-bridge formation
increased force of contraction
what are the 2 limits of the Frank-starling mechanism?
excessive stretching causes a decrease in cross-bridge formation
Laplace’s law: in a large sphere, more wall tension is required to generate the same internal P as it does in a small sphere as governed by:
Pressure = tension/radius
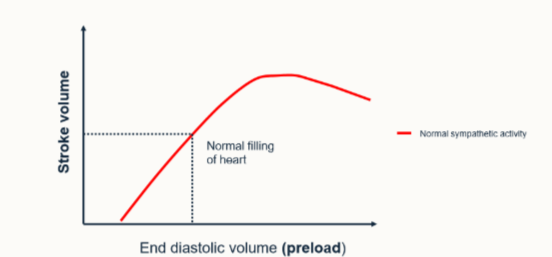
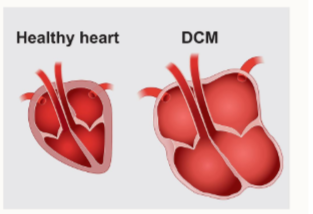
What are the clinical consequences of Laplace’s law
if the heart fills itself with more blood, it’s at an increasing mechanical disadvantage
chambers become more difficult to empty
e.g. dilated cardiomyopathy
What are 2 factors that influence preload
filling time of the heart:
low rates > longer period of ventricular filling → greater distension of the ventricle
venous return:
P difference b/w venous system and atrium:
skeletal muscle pump
respiratory pump
SNS activity
blood volume
how does the skeletal muscle pump work and how does it affect venous return
skeletal muscle contracts
veins are compressed
blood is forced to the heart
increased pre-load
increases venous return.
how does an increased respiratory pump increase venous return?
diaphragm moves caudally
increasing abdominal pressure
thorax pressure is reduced
INCREASED ABDOMINAL RETURN OF BLOOD
increases preload
outline the sympathetic control of venous return
venous system acts as a ‘reservoir’ of blood
the SNS stimulates the venous system causing:
venous vasoconstriction
increased venous pressure
increased preload (as a result)
Summaries how stroke volume is increased
Increases SNS → increased blood volume
Increased use of skeletal muscle pump → increased respiratory movements
BOTH:
increase venous pressure
increase venous return
increase EDV
what is the extrinsic regulation of stroke volume
The SNS activation → inotropy of the heart → increased contraction at any given preload
increasing stroke volume
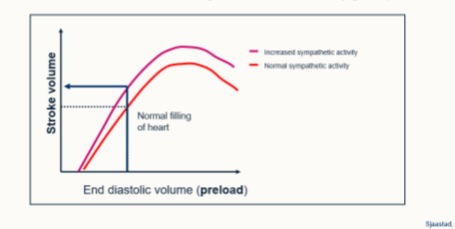
What is inotropy
increasing contractility of the heart
how does the SNS lead to increased ventricular contractility
empty more completely, thus reduced ESV
greater pre-load creating a greater filling volume
increased stroke volume → reduced ventricular filling time
afterload increases (increased aortic P)
what receptors are involved in increasing ventricular contractility caused by sympathetic stimulation
B1-adenoreceptory
How can contractility be manipulated pharmacologically
Positive inotropes:
phosphorylation of Ca2+ channels
faster calcium re-uptake
sensitisation of troponin C to calcium
increased contractility

what are some example clinical drugs that manipulate contractility
cardiac glycoside e.g. digoxin
Beta 1 - adrenoreceptor agonists e.g. dobutamine
How does the parasympathetic nervous system affect contractility
decreases force of contraction
inhibition of noradrenaline released from sympathetic NS
decreases heart rate
what receptors are involved in the parasympathetic stimulation of ventricular contractility
M2 muscarinic receptors
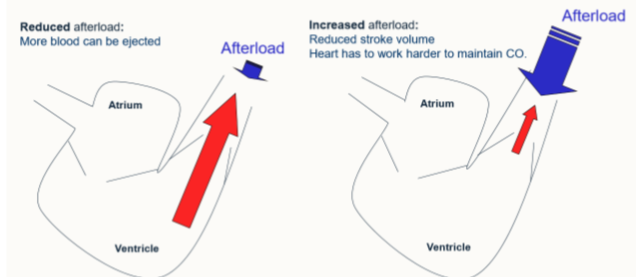
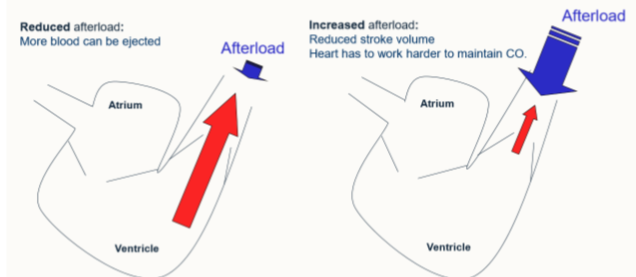
what is the effect of afterload on stroke volume
creates the resistance against which ventricle pumps
increased stroke volume → increased CO and thus increased afterload
apart from ventricular systole, what else effects afterload on stroke volume
pressure of blood in circulation
principally affected by vasomotor tone
primarily arteriolar tone
what is the normal situation of afterload
ejection pressure is greater than afterload, hence blood is ejected out of the heart
what is the effect of reducing afterload on stroke volume?
more blood can be ejected
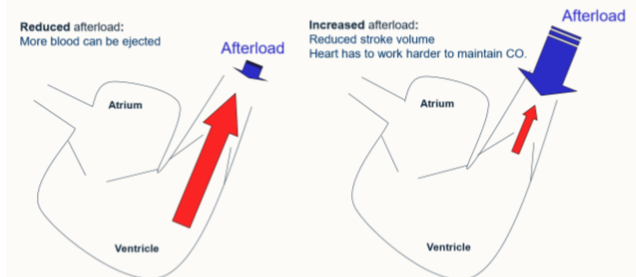
what is the effect of increasing afterload on stroke volume
reducing stroke volume
heart has to work harder to maintain CO
summarise stroke volume: 3 points
normal heart pumps venous return each cycle = intrinsic control
extrinsic mechanisms can overcome limits of intrinsic control → increased contractility at a given period
afterload is a limiting factor in stroke volume in diseased animals e.g. hypertensive animals
what does the ANS control of the heart rate enable
rapid response (increase of decreased)
tightly regulated to maintain blood P
How does Blood P influence heart rate and cardiac output?
Elevated BP (transient):
PSNS activation → reduced heart rate, reduced cardiac output, BP returns to normal
Low BP:
SNS activation → increased HR, increased vascular tone, increased CO, restores blood PS
What contributes to blood pressure?
vascular resistance
cardiac output (influence each other)
HR and SV impact CO
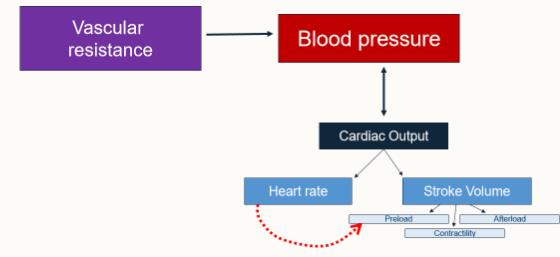
how do we calculate BP?
BP = MAP: mean arterial pressure
cardiac output x total peripheral resistance
what is total peripheral resistance (TPR)
arterial vascular resistance (tone)
what is TPR influenced by?
SNS (alpha and beta adrenoreceptors) in the vasculature
Renin-Angiotensin Aldosterone System (RAAS)
Local endothelial-derived factors
what do cardiac output and TPR affect
degree of afterload
how do we calculate blood flow
pressure difference/resistance
what is resistance proportional to?
Length/Radius4
How do we maintain blood flow if radius is halved
need to increase volume x 16
How do we calculate pulse pressure
Psystolic - Pdiastolic
how do we calculate mean arterial pressure
Systolic + 2(diastolic) / 3
what is pulse pressure influenced by
arterial compliance (aorta)
ability to accommodate the increase in pulse pressure
decreases with age
stroke volume
consistent high pulse pressure will ‘‘age’’ heart quicker
what does a greater stroke volume in relation to pressure
greater difference b//w systolic and diastolic pressure
When considering cardiac function, what is more important for perfusion of peripheral tissues - cardiac output or blood pressure
blood pressure is more important, as a decrease in BP will lead to lack of nutrients being delivered to tissues = cell death and organ failure. Too high = oedema
cardiac output is important as it generates blood P but not as important for perfusion
How does contractility of the heart change during physical exercise. How is this brought about?
EDV = lower
squeeze more blood out = stroke volume increases
SNS stimulates heart to contract with NA (conscious decision)
chemoreceptors haven’t kicked in yet
adrenaline will kick in ‘fight or flight’
What changes occur in HR, venous return, total peripheral resistance, tissue fluid volume and urine output after a major haemorrhage?
HR = increase - want to maintain cardiac output and correct pressure drop
venous return decreases
total peripheral resistance = decrease, constrict to maintain pressure
tissue fluid volume = decrease
urine output = decrease, want to conserve water as much as possiblt
what happens to cardiac output in heart failure
reduced BP
may have a miss-match in the L/R side of ventricles
exercise intolerant, particularly under stress
CO decreases for any given preload