Anxiety
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
42 Terms
Anxiety disorders and their treatment
Anxiety disorders are very common with lifetime prevalence rates as high as 31%, (12-month prevalence rates of about 18%)
Anxiety: emotion characterized by feelings of tension, worried thoughts and physical changes.
People with anxiety disorders usually have recurring intrusive thoughts or concerns.
They may avoid certain situations out of worry.
They may also have physical symptoms such as sweating, trembling, dizziness, rapid heartbeat, muscle tension.
Anxiety occurs in response to a specific stimulus (e.g. phobia) or unexpectedly.
Could it be distinguished from fear and phobia?
Phobia is persistent fear of clearly discernible, circumscribed objects or situations.
Exposure to the phobic stimulus invariably provokes an immediate anxiety response.
Critical when these conditions can negatively impact an individual’s quality of life and disrupt important activities of daily living.
Anxiety can be a normal part of everyday life,
Anxiety disorders are associated with functional impairment;
Needs to be treated when symptoms cause significant distress or impairment in social, occupational, or other important areas of functioning
Severe anxiety
Severe type of anxiety can be expressed in:
Phobia (extreme, irrational fear about a situation)
Panic attack (sudden episode of intense fear that triggers severe physical reactions)
General anxiety disorder (GAD).
Important facts
Treatable by pharmacotherapy or behavioural therapies or both (but treatment resistant patients)
Associated with an increased risk of developing a comorbid major depressive disorder
High levels of co-morbidity (Major depression, bipolar disorder, ADHD…) associated with poorer outcome
High economic impact, large proportion of sufferers not treated (misdiagnosis)
Moderate increase in suicide risk (higher in PTSD)
Sometimes young age of onset (varies with the type) />twice more common in women
Related disorders:
Post Traumatic stress disorders
Obsessive compulsive disorder (repetitive behaviors or mental acts performed as a result of anxiety and distress)
Factors associated
Gender (females >twice more affected), but women more likely to recover
Loneliness, Unmarried status,
Lower education level,
Poor health, chronic somatic illnesses, such as cardiovascular disease, diabetes, asthma, and obesity
Presence of life stressors.
Variable age of onset, with a median age of 30 years forGAD
Both environmental and genetic factors such as
History of stressful or traumatic experiences, such as domestic violence, Child abuse or bullying, adverse parenting, childhood trauma
Comorbidity, can precede
Comorbidities
Estimated:
52% of patients with bipolar disorder
60% of patients with MDD (Major depression may develop as a complication of GAD)
47% of patients with ADHD have a comorbid anxiety or related disorder
For practitioners or pharmacists
Check that anxiety is not:
Caused by another medical (eg some physical symptoms may occurs in other pathologies like hyperthyroidism, CPD),
Comorbid with another psychiatric condition
Medication-induced or drug-related (substance of abuse withdrawn)
Compassionate listening and education
Common lifestyle recommendations that may reduce anxiety-related symptoms:
Help to identifying and removing possible triggers (e.g., caffeine, stimulants, nicotine, dietary triggers, stress). Note that smoking cessation can trigger the symptoms
Help improving sleep quality/quantity
Encourage physical activity (associated with improved physical health, life satisfaction, cognitive functioning, and psychological well-being)
Provide education about their disorder, efficacy (including expected time to onset of therapeutic effects) and tolerability of treatment choices, aggravating factors, and signs of relapse
Key features of specific anxiety and related disorders
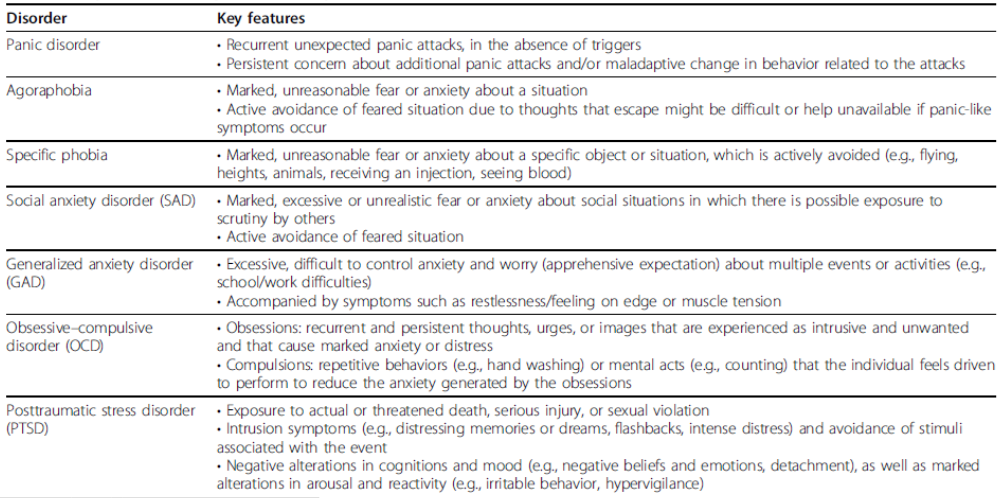
Anxiety disorders and related disorders
Main subtypes
7-9%: specific phobia
7%: social anxiety disorder
2-3%: panic disorder
2%: agoraphobia
5-6%: generalized anxiety disorder
1-2%: separation anxiety disorder (mainly children)
3-4%: posttraumatic stress disorder
Women are about twice more likely than men to experience anxiety disorders.

Animal models
Open field (anxious mice remain in a corner of a open arena)
Novelty Suppressed Feeding in the middl of the arena to (anxious mice will have more difficulty to venture in the middle of the arena to get some food)
Elevated plus Maze (anxious mice prefers to remain in a closed arm than in an open arm)
Social Approach (anxious mice will not approach new cage mate)
Light dark box (anxious mice prefer to stay in dark box)
Fear conditioning (anxious mice exhibit longer freezing behaviour when exposed to aconditioned stimulus)
Faecal dropping count: anxiety make bowel move faster
Biological markers
No clear structural brain abnormalities,
Possibly increase in some inflammatory markers in the brain (cytokine)
Amygdala (fear centre) dysfunction?
Increased grey matter (GM) volume in the amygdala (fear centre) has been repeatedly found in GAD patient
Over activation of the HPA axis (stress response)
Likely, a dysfunctional connection between several brain structure and an overactivation of the amygdala from functional imaging studies.
Other pathways involved:
Hippocampal pathways (learning and memory)
Dorsal raphe Serotonergic pathways (mood)
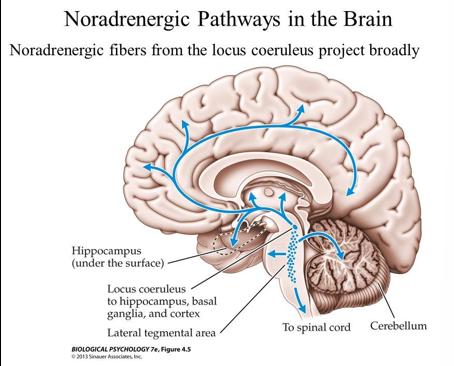
Locus coeruleus Noradrenergic pathways (attention vigilance, formation and retrieval of memory, stress response)
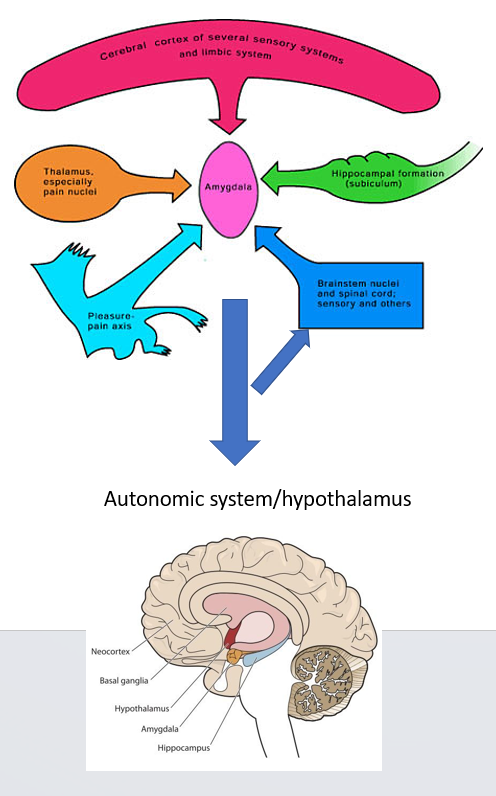
The amygdala
The amygdala couples a learned sensory stimulus (e.g. danger) to an adaptive response (e.g. fight or flight).
Inputs: the amygdala gets sensory input, (highly processed inputs from association areas of visual, auditory, and somatosensory cortices).
Sensory input from the cerebral cortex, the thalamus (involved in filtering of sensory information)
Outputs: the amygdala is able to control the autonomic system, to provoke an instant sympathetic response. The main outputs of the amygdala are to the hypothalamus and brainstem autonomic centres.
Monkeys with lesioned amygdalas are unable to recognize the emotional significance of objects, and for example, show no fear when presented with a snake or another aggressive monkey.
Involved in processing of fear
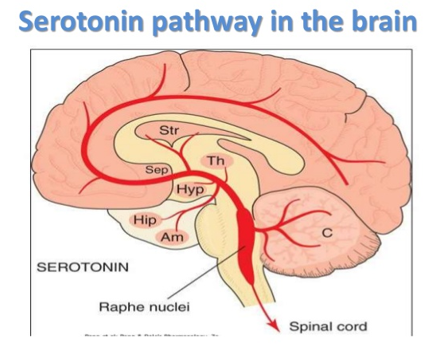
Role of serotonin
Raphe innervation of brain areas important for anxiety (amygdala, hippocampus)
Raphe stimulation evokes behavioural inhibition/ anxiety like behaviour
Stress/fearful situations increase 5-HT release
Giving animals the selective serotonin reuptake inhibitor (SSRI) or some serotonergic agonists provokes anxiety-like behaviors.
Selective chemical lesion that destroy serotonergic neurons reduce anxiety levels in animal model
Selective electrical activation of serotonin neurons improve ability to cope with stress and inactivation of these neurons increase anxiety like behaviour
Overall, manipulation of serotonergic neurotransmission and serotonergic neurons modulate stress and anxiety-related behaviour.
Serotonin: Pharmacological and clinical evidence:
Some serotonergic agents demonstrated anxiolytic effects (5HT1A agonists) other anxiogenic effects (5-HT2C agonists)
Partial agonists of 5HT1A receptor of the azapirones family (buspirone, gepirone, ipsapirone, tandospirone) have anxiolytic properties (some commonly used in clinic)
Usually have limited effect so are used with other drugs
Selective serotonin uptake inhibitors are the first line treatment
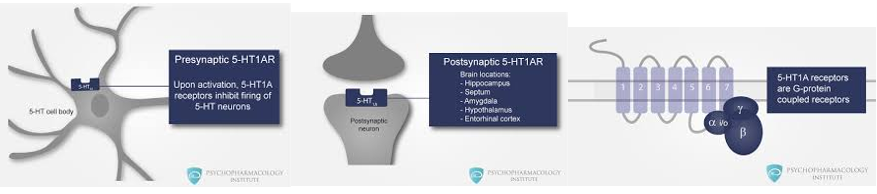
Why 5-HT1A receptor?
Abundant in areas linked to anxiety
Main function of 5-HT1A receptor:
Gprotein coupled receptor, inhibitory receptor (Gi protein coupled),
Presynaptic auto receptor inhibit activity of serotonergic neurons (negative feedback inhibition)
Postsynaptic receptor, reduce postsynaptic neurons excitability (abundant in hippocampus, prefrontal cortex and amygdala, activation of serotonin (5-HT) 1A receptors in the amygdala reduces anxiety-like behaviour
In Patients only efficient after 2-3 weeks administration
Treatment for long term-relief with serotonergic antidepressant
Selective serotonin uptake inhibitor:
First line treatment (other antidepressants may work), because of low side effects,
Act with a delay of generally 4 to eight weeks in onset of symptom relief, with full response taking up to 12 weeks or more.
Longer-term therapy associated with continued symptomatic improvement and the prevention of relapse,
First weeks of treatment maybe associated with increase in anxiety (transient combination with a benzodiazepine)
Therapy should be continued for at least 12-24 months for most patients
1st line= Sertraline
2nd line= Paroxetine or citalopram
Preferred drugs: fluoxetine, citalopram, escitalopram, sertraline
Selective serotonin and noradrenaline uptake inhibitor:
Similar effects as SSRI
Tricyclic antidepressants
Similar clinical effects as SSRI, but side effects, not first line therapy
Good clinical results obtained with clomipramine in clinical trial
Atypical antidepressants
Trazodone, targets various monoamine receptors, with 5-HT1A agonist properties
Role for noradrenaline
Role of locus coeruleus (LC) in arousal and attention and aversive memory
LC innervation of brain areas important for anxiety (amygdala, hippocampus)
LC stimulation evokes anxiety
Fearful situations increase LC firing and NA release
Strong link with hypothalamic- pituitary-adrenal (HPA) axis and autonomic centres (sympathetic system)
Stress is known to induce noradrenaline release in several brain regions associated to emotion and autonomic control
Extreme anxiety caused by drug of addiction associated with overactivation noradrenaline neurons during withdrawal
Pharmacological and clinical evidence for a role of NA neurotransmission
Clonidine and Alpha-2 receptor agonist
Clonidine may have proven anxiolytic effects but rarely used in clinic for treatment of anxiety (side effects)
Alpha-2 receptor agonist (noradrenergic counterpart of 5-HT1A agonist) clonidine
Alpha-2 receptor are inhibitory receptor; can decrease sympathetic outflow from the central nervous system
Presynaptic auto receptor inhibiting activity of noradrenergic neurons (negative feedback inhibition)
Postsynaptic receptor, reduce postsynaptic neurons excitability (abundant in hippocampus, prefrontal cortex and amygdala);
Activation of a2 receptors in the amygdala reduces neuronal activity and fear response to aversive stimuli
Anxiety associated with opiate-withdrawal (linked to overactivation of noradrenergic neurons) improved following a2 receptor agonist treatment
b antagonists (propranolol)
Disputable real anxiolytic effect, but very useful to reduce physical symptoms (eg tachycardia) and improve patients general state (symptomatic relief)
May have a positive effect on aversive learning (help to reduce impact of traumatic events on memory, tested in patients following a trauma experience (PTSD patients).
Selective noradrenaline uptake inhibitors likely efficient on anxiety disorders (but not first line treatment)
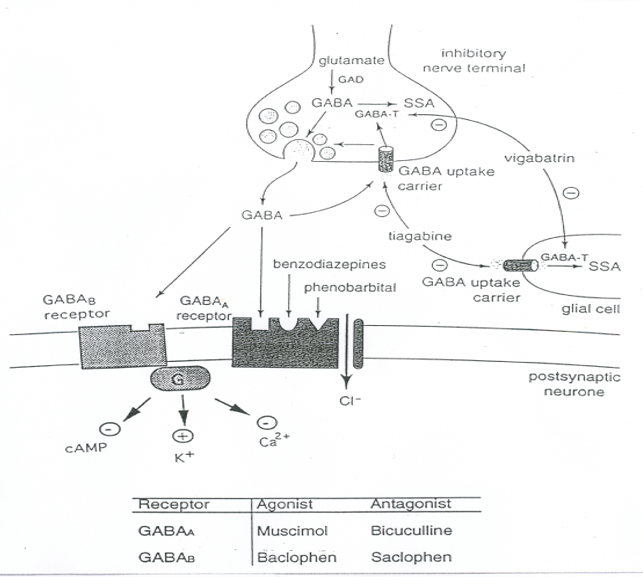
GABA receptor agents
GABAA receptor potentiators (benzodiazepines and related compounds) can be useful agents for the acute but not long-term treatment of anxiety.
Act mainly as tranquilizers (acute calming/sedative effect) and can help to improve sleeping problems
Ionotropic receptor:
ligand-gated Cl- channel
Mediates very fast inhibition
Major inhibitory mediator in the brain (should reduce neuronal overactivation)
GABAA receptor: Agonists and antagonists
Agonists and Antagonists:
The agonist activate GABAA receptor function causing calming effect and the antagonists block it increasing anxiety
Competitive (act at GABA binding site):
Agonists: GABA, muscimol
Antagonist: bicuculline/picrotoxin
Non-competitive (act at modulatory sites allosteric modulator). Potentiate receptor activity to make it more efficient
Agonists: benzodiazepines, z-drugs and related drugs, barbiturates, neurosteroids
Antagonists:
Flumazenil (inhibits benzodiazepines)
Picrotoxin (causes convulsions)
GABA-ergic neuron
Drugs work where you have over activation of neurones caused by anxiety
GABAA receptor
Five subunits composed of a combination of different subtypes of a (a1-5), β (β1-3) and γ (γ1-3) subunits
Located on post-synaptic terminals throughout CNS
GABA binding to alpha subunits opens Cl- channel, resulting in neuronal hyperpolarisation
Mediate early phase of IPSPs
GABAA receptors are the main mediator of inhibitory neurotransmission (every neurons in brain is equipped with GABAA receptors that can reduce its electrical activity (braking system) also very important function of GABAergic interneurons
GABAA receptor modulatory sites
Benzodiazepine, barbiturate, neurosteroid binding sites
E.g. benzodiazepines bind to alpha subunits
Binding facilitates GABA effects (enhanced Cl- entry into neuron)
Increased hyperpolarisation results in enhanced inhibition
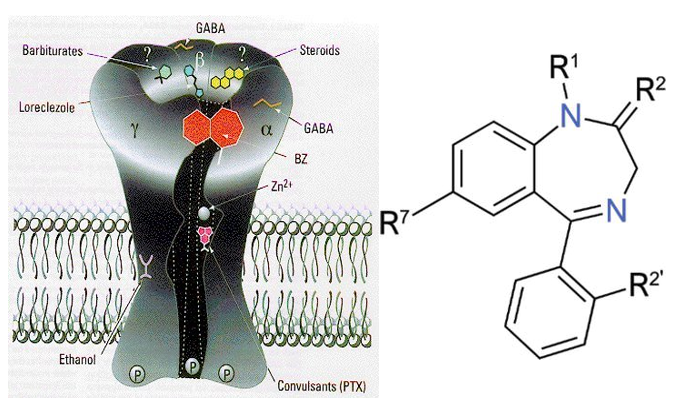
GABAA receptor a subunit types
Various a subunits are associated with different functions
Due to preferential localisation of certain subunit combinations in select brain regions
a1: hypnotic (sleep-inducing)
a2/3: anxiolytic (anti-anxiety)
a5: amnesic (inhibits memory)
GABA Receptors as Therapeutic Targets?
Little use for drugs acting competitively on GABAA receptors due to poor selectivity and side effect profile
Benzodiazepines (and barbiturates) used as hypnotics, muscle relaxants, anxiolytics, anti-convulsants.
Side effects and abuse potential limit their usefulness= Giving treatment for two long can cause addiction. Only treated for a short period of time
Targeting specific GABAA receptor subunits may have therapeutic uses and limited side effects
a1 agonists: sedative
a2/3 agonists: anxiety
a5 antagonists: cognitive enhancement (e.g. Alzheimer’s)
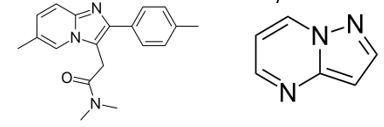
Drugs closely related to benzodiazepine
Looking for a compound producing a robust anxiolytic action comparable to benzodiazepines, but lacking these limiting side effects at therapeutic doses (an anxioselective agent), would represent an important advance in the treatment of generalized anxiety disorder, and perhaps other anxiety disorders.
Z-drugs:
zopiclone, zolpidem and zaleplon. Closely related to benzodiazepine, but some could be more subtype selective, most are hypnotic but possibly safer than BZP and barbiturate and less likely to cause dependence and addiction.
Pyrazolopyrimidine:
Ocinaplon mainly anxiolytic properties and relatively little sedative or amnestic effect (still not in the market (are alpha2/3 selective).
Use of benzodiazepine and related compounds in anxiety disorder
Useful for immediate calming effects, but potentially harmfull for long term teatment
Could be used temporary while waiting for clinical effects of SSRI
Most used: diazepam, alprazolam, temazepam, flurazepam
Adverse effects:
Sedative
Motor impairment
Memory deficit
Interaction with alcohol
Tolerance, dependence, withdrawal
Useful for associated sever insomnia
BDZs shortens the time it takes to go to sleep (good for sleep induction)
Little-no effect on the duration of sleep
BDZs shortens REM sleep (Rapid eye movement- dream sleep)
BDZs shortens deep sleep (slow wave sleep)
Z drugs (e.g. zopiclone and zolpidem) may be preferable as sleeping agents (lower risk of addiction, shorter half life, better for elderly people)
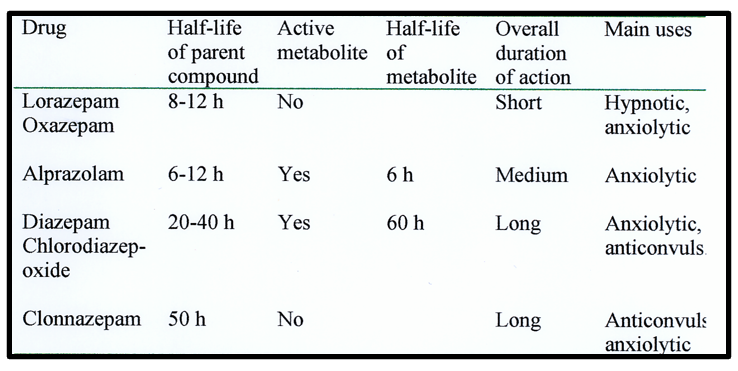
Half life of BDZs varies
Summary treatment for anxiety disorders
CBT usually can be the effective first-line option and can be as effective as pharmacotherapy.
When patients do not benefit from CBT, a trial of pharmacotherapy is advisable, and vice versa.
Pharmacotherapy:
SSRI as first line therapy
70% success rate, but
Long onset of action for SRRI (>4 weeks), SSRIs have the potential to exacerbate anxiety and panic early in the treatment course
Benzodiazepines (optional in combination):
Rapid onset of action but sedation, confusion (possible loss of memory), and increased mortality.
Can cause tolerance and dependence (should be used for short term relief (while waiting for effects of SSRI)
Most commonly used: alprazolam, temazepam, flurazepam
5-HT1A receptor partial agonists (more second line therapy).
Azapirones, such as buspirone (Buspar) work for GAD, but may not work for PD.
Takes 2-4 weeks for onset of action, recommended only for short term treatment, not as effective as benzodiazepine but no sedation and dizziness.
Common practice: to combine SSRIs with benzodiazepines to provide more rapid, and potentially additive, clinical efficacy.
Combining medication and psychotherapy may be even more effective for patients with moderate to severe symptoms
May reduce hyper arousal
If non responsive:
SNRI then TCA (clomipramine), other options: pregabalin (VDCa++ channel blocker) or second generation antispychotics (SGA)
If completely refractory: ketamine, vagus nerve stimulation (not in UK)
General anxiety disorder
Common anxiety disorder (1-4% among general population).
Very common in primary cares, Missed diagnoses and misdiagnosis (like for PD) are high, with symptoms often ascribed to physical causes.
GAD: Excessive out of control worries.
Excessive anxiety about ordinary, day-today situations. The anxiety is intrusive, causes distress or functional impairment, and often encompasses multiple domains (e.g., finances, work, health).
The anxiety is often associated with physical symptoms, such as sleep disturbance, restlessness, muscle tension, gastrointestinal symptoms, and chronic headaches.
Bimodal age of onset:
Children: 10-14 y; Adult: 30 y
Psychological treatment (CBT and ICBT) can be as effective as drug therapy
Benefits of psychological treatments are maintained at one to 3 years follow-up after treatment
No clear evidence that combination CBT/pharmacotherapy is better
Drug treatment:
First line SSRI (sertraline, escitalopram, citalopram), SNRI (duloxetine). BZD (Alprazolam, bromazepam, diazepam, and lorazepam for short-term use during crisis
Can give beta blockers for physical symptoms
Second/third line: SGA (quietapine) or pregabaline, buspirone
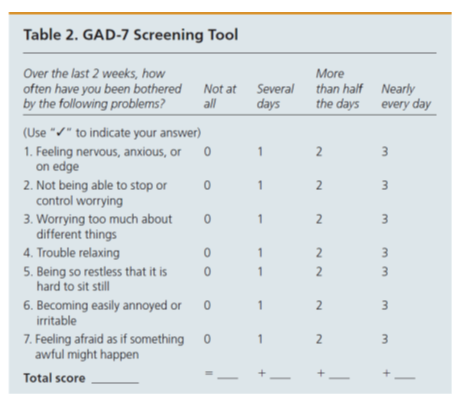
GAD-7 screening tool
Panic disorder
Recurrent unexpected panic attacks, in the absence of triggers
Persistent concern about additional panic attacks and/or maladaptive change in behaviour related to the attacks
Lifetime prevalence: 4-5% of PD, but28% for PA!
Age of onset: 20-24
Strong co-occurrence with agoraphobia and MDD and with other medical condition like thyroid disease, cancer, chronic pain, cardiac disease, irritable bowel syndrome, migraine, as well as allergic and respiratory diseases.
CBT is an efficacious psychological treatment for panic disorders
Combined psychological and pharmaco-therapy may be more effective that one of them alone
Firstline pharmacotherapy: SSRI, benzodiazepines (second-line options) may be useful at any time during therapy for the short-term management of acute or severe agitation or anxiety.
If treatment resistant (refractory) try first TCA or SGA as second or third line.
Buspirone, propranolol not recommended
Panic disorders: DSMV criteria
Characterized by recurrent and unexpected panic attacks, (abrupt surge of intense fear or intense discomfort that reaches a peak within minutes), and during which time four (or more) of the following symptoms occur:
Note: The abrupt surge can occur from a calm state or an anxious state.
1. Palpitations, pounding heart, or accelerated heart rate.
2. Sweating.
3. Trembling or shaking.
4. Sensations of shortness of breath or smothering.
5. Feelings of choking.
6. Chest pain or discomfort.
7. Nausea or abdominal distress.
8. Feeling dizzy, unsteady, light-headed, or faint.
9. Chills or heat sensations.
10. Paresthesias (numbness or tingling sensations).
11. Derealization (feelings of unreality) or depersonalization (being detached from oneself).
12. Fear of losing control or “going crazy.”
13. Fear of dying.
Agoraphobia
Fear of being in situations where escape might be difficult (not a simply fear abut open space)
Marked, unreasonable fear or anxiety about a situation (patient can develop panic like symptoms)
Active avoidance of feared situation due to thoughts that escape might be difficult or help unavailable
It can be fear of: travelling on public transport, visiting a shopping centre, leaving home usually experience physical symptoms of panic attack (can be a complication of PD)
Prevalence: 1-2 % (without panic)
Treatment: similar as PD
Specific phobia
Marked, unreasonable fear or anxiety about a specific object or situation, which is actively avoided (e.g., flying, heights, animals, receiving an injection, seeing blood)
Life time prevalence 10-13%
Much higher rate in adolescent (up to 30%??) and very early age of onset (5-12)
Can have very negative impact on social/occupational functioning and lead to restriction of usual daily activities, co-occur with other specific phobias, with less than 10% of patients having only one fear, strong cooccurrence with other anxiety disorders.
Psychosocial interventions, particularly exposure-based treatments, treatments of choice, associated with a high degree of success in providing remission
Minimal role for pharmacotherapy
Progressive exposures are generally more tolerable
Social anxiety disorder (SAD)
Marked, excessive or unrealistic fear or anxiety about social situations in which there is possible exposure to scrutiny by others
Active avoidance of feared situation
(fear that the individual will say or do something that will lead to humiliation, embarrassment, or negative evaluation by others)
Most common anxiety disorders, with lifetime prevalence estimates ranging from 8-12%
Early age of onset (12)
Associated with significant impairments including problems with educational performance, family functioning, and an overall reduced quality of life (QoL)
Large comorbidity with ADHD MDD and other anxiety and related disorders.
Psychological treatment, in the form of CBT, considered gold-standard Cognitive techniques include restructuring and challenging of maladaptive thoughts
Pharmacotherapy has not been shown to be of benefits over CBT
If not responding to BT, second line therapy: SSRI
Obsessive-compulsive disorder (OCD)
Obsessions: recurrent and persistent thoughts, urges, or images that are experienced as intrusive and unwanted and that cause marked anxiety or distress (Fear of being contaminated by germs or dirt, aggressive or disturbing thoughts, concern of causing injuries....)
Compulsions: repetitive behaviours (e.g., hand washing) or mental acts (e.g., counting) that the individual feels driven to perform to reduce the anxiety generated by the obsessions
Less common than other anxiety disorder 2-3 % life time prevalence
OCD is associated with a substantial negative impact on QoL for both patients and their caregivers
(can cause distress and disruption to all members of the family). Patients are usually aware that their obsessions and compulsions are irrational and excessive, but feel unable to control them.
60-90% of patients with OCD also have a comorbid disorder (anxiety, bipolar, psychosis)
Usually early onset (12) with fluctuating or episodic courses, relapse may occur after successful treatment.
Treatment:
CBT, generally including exposure with response prevention (ERP)
Pharmacotherapy (in combination with CBT )
SSRIs first-line pharmacological interventions in adult
SNRIs, TCA (clomipramine), and other antidepressants as second- and third-line treatments.
Children: Fluoxetine in combination with CBT (under careful monitoring)
SSRI/SGA when treatment resistant
Posttraumatic stress disorder (PTSD)
Major stress following exposure to traumatic events (death, death threatening), serious injury, or sexual violation
Intrusion symptoms (e.g., distressing memories or dreams, flashbacks, intense distress) and avoidance of stimuli associated with the event
Negative alterations in cognitions and mood (e.g., negative beliefs and emotions, detachment), as well as marked alterations in arousal and reactivity (e.g., irritable behaviour, hypervigilance)
Most common forms of trauma resulting in PTSD included unexpected death of someone close, sexual assault, serious illness or injury to someone close, having a child with serious illness, and being beaten by a partner or caregiver
Onset: 20-25
associated with significant QoL and functional impairments, estimate lifetime prevalence: 6-8%, somatic complaints, suicide risk, and comorbid psychiatric disorders.
Possible strong association with high suicide rates (conflicting results).
CBT effective first-line option
Pharmacotherapy includes mainly SSRIs
Associated symptoms may need some specific treatments (trauma nightmare, hyperarousal state) Possible beneficial effects of propranolol for decreasing physiological signs of hyperarousal when used shortly after patients with PTSD experience.
Screening questions for specific anxiety and related disorders

Generalised anxiety disorder: Diagnosis and assessment
There are various anxiety disorders. – different questionnaires apply to each
Ask Over the last 2 weeks, how often have you been bothered by the following problems?
Feeling nervous, anxious or on edge
Not being able to stop or control worrying
Screening tools: GAD-7
Carry out physical examinations – symptoms would exist in absence of co-existing medical problems/substances
Increased heart rate.
Shortness of breath.
Trembling.
Exaggerated startle response

DSM-5-TR
DSM-5-TR is the standard classification of mental disorders
Core symptoms
Excessive anxiety and worry occurring most days across at least 6 months
Difficultly controlling the worry.
Cause clinically significant distress or impacting social, occupational, or other functioning.
Accompanying Symptoms (3+ on most days)
Psychological symptoms
Restlessness,
Difficulty concentrating or mind going blank, irritability,
Physical symptoms
Easily fatigued,
Muscle tension,
Sleep disturbance
ICD-11
International Classification of Diseases 11th Revision
Core symptoms
Anxiety and general apprehensiveness or worry
Marked symptoms manifested by either general apprehensiveness (not restricted to particular circumstance).
Accompanying symptoms
Physical symptoms
muscle tension or motor restlessness;
sympathetic autonomic overactivity (e.g. frequent gastrointestinal symptoms, palpitations, sweating, trembling, shaking, and/or dry mouth);
Psychological symptoms
subjective experience of nervousness, restlessness, or being 'on edge’;
difficulty concentrating;
irritability;
sleep disturbances (difficulty falling or staying asleep, or restless, unsatisfying sleep).
Types of anxiety
Type | Incidence | Screening Tool | Definition & Details |
Generalised Anxiety Disorder | 5% | Generalised Anxiety Disorder 7 (GAD-7) | •Characterized by excessive worry about everyday issues that is disproportionate to any inherent risk. At least 3 symptoms present most of the time: restlessness or nervousness, being easily fatigued, poor concentration, irritability, muscle tension, or sleep disturbance. •Often co-exists with depression •6 months to several years |
Panic Disorder | 1% | •During an acute attack, at least 4 symptoms present: shortness of breath, palpitations, shakiness, nausea, hot or cold flushes, dizziness, and feeling of imminent death •Sudden onset •Months to a lifetime | |
Social Anxiety Disorders /Social phobias | 2% | 3-item Mini-Social Phobia Inventory (Mini-SPIN) | •Suggested by anxiety or persistent fear that is limited to social situations and fear of social scrutiny or embarrassment. Avoidance behaviour is commonly present. E.g. agoraphobia, claustrophobia, social phobia •Can be life-long |
Post traumatic Stress Disorder | <1% | Trauma Screening-Questionnaire (TSQ) | •Exposed to a traumatic event or situation and experience persistent remembering or 'reliving' the stressor in intrusive flashbacks, vivid memories, or recurring dreams, or experience distress, hypervigilance, avoidance of reminders. •Symptoms manifest within 6 months, although can have delayed onset. •Can be life-long |
Obsessive Compulsive Disorder | 2% | Yale–Brown Obsessive-Compulsive Scale (Y-BOCS) | •Characterized by recurrent obsessional thoughts or compulsive acts or, commonly, both, which may cause significant functional impairment and/or distress •Episodic •Anxiety if resist compulsion, ritualistic |