unit 7 lesson 3 blood vessels and circulation
1/140
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
141 Terms
What is interstitial fluid, what does it consist of
Fluid between the blood vessels and cells, consists of water, nutrients, hormones, enzymes, waste etc. 26% of human overall body fluid. Where blood and cells interactions MUST pass through

Systemic circulation pathway
Oxygenated blood is pumped from left side of heart throughout body via arteries, and further from heart become arterioles.
Arterioles branch out within capillary beds into capillaries. Oxygen leaves the capillaries and CO2 enters the capillaries to be carried back to heart
Deoxygenated blood travels in increasingly larger vessels back towards the right side of the heart. From the capillaries via venues then via the larger veins
Pulmonary circulation pathway
Deoxygenated blood leaves the right side of the heart en route to the lungs to exchange CO2 for oxygen
Oxygenated blood from lungs returns to left side of the heart
Necessary characteristics of all blood vessels
Must be flexible and resilient to withstand pressure and changes to it as well as flexibility to accommodate other tissues around them (organs, etc)
What is anastomosis
The joining of two vessels WITHOUT INTERVENING CAPILLARY BED (arterioles to venule) (connection between peripheral vessels)
What is collateral
More then one artery supplying an area (capillary beds needed), multiple arterioles vessels in one area
What is angiogenesis
Formation of new blood vessels- controlled by endothelial growth factor which tells body to make more
5 types of blood vessels
Artery, arterioles, capillary, venule, vein
What are characteristics and functions of arteries
ALWAYS CARRY BLOOD AWAY FROM THE HEART , initial vessel blood must pass through, highest pressure vessels. Thick walls that contain lots of elastic fibres
What are characteristics and functions of arterioles
Branches of arteries that deliver blood to capillary networks
What are capillary characteristics and functions
Smallest vessels with diameter if only 1 RBC, located between arterioles and venules, whose thin walls allow for the diffusion of gasses, nutrients and waste between plasma and intestinal fluid to cells (blood and tissue interaction)
Characteristics and functions of venules
Thin walled vein with lower pressure than even capillaries to carry blood away from capillaries back towards heart. Unite to form larger veins
Characteristics and functions of veins
Thin walls, Carries blood towards the heart and contains valves
Main differences between arteries and veins
Arteries carry blood away from heart while veins bring blood towards heart
Walls of arteries are thicker than veins
Endothelial lining of arteries have pleated folds (allows for contraction) while veins don’t
What are blood vessel lumens
Inside tube structure of blood vessels
Layers that make up blood vessels (innermost to outermost)
Tunica intima, tunica media, tunica externa or adventitia
What is the tunica intima of the blood vessel
Vessels endothelium (Inner most layer) of blood vessels composed of simple squamous epithelium, thin layer of connective tissue with elastic fibers.
In arteries this layer does not move but instead creates folds (pleated folds)
Tunica media of vessels
Middle layer→thickest layer in arteries, composed of elastic fibers and smooth muscles which causes vasoconstriction and vasodilatation
Adventitia of blood vessels
Tunica externa or outermost layer→ composed of connective tissue with elastic fibres which anchors vessel to surrounding tissues
What is vasa vasorum
Vessels within bigger vessels that supply them with blood flow
Types of arteries to know
Elastic arteries, muscular arteries, aterioles
What are elastic arteries
Largest arteries that transport heart away from heart (pulmonary, aorta). These arteries are rich in elastic fibres with relatively few smooth muscles to enable resiliency and ability to withstand the highest of pressures and decreasing pressures
What are muscular arteries
Most arteries, medium sized with thicker tunica media (more smooth muscles) allowing for vasoconstriction and vasodilatation
What are arterioles
Resistance vessels which are the smallest type. Carries blood from muscular arteries to capillaries. Tunica media has much less smooth muscles and less adventitia. These branch into metarterioles which connect to capillaries
What is vasodilation
An increase in the diameter of arterioles due to relaxation of smooth muscles which in tunica media. (Decreases blood pressure and resistance)
What is vasoconstriction
A reduction in the diameter of arterioles due to the constriction of smooth muscles in the tunica media
What causes vasodilation and vasoconstriction
Occurs in response to local factors, hormones or stimulation of the vasomotor centre in medulla oblongata
What factors will vasodilation and vasoconstriction effect in terms of blood flow
Impacts after load (directly related to resistance), peripheral blood pressure and capillary blood flow
Histology of capillaries
Single layer of simple squamous epithelium (endothelial tube) surrounded by a basement membrane. Known as exchange vessels hence the simple squamous allowing for efficient diffusion
How big are capillary diameters
Only the diameter of one red blood cell
Where are capillaries found
Throughout body, but more extensively in highly active tissues (muscle, brain, kidneys and liver)
Difference between highly vascular vs avascular tissue
Highly vascular tissues have more capillary networking where as avascular tissues have no capillaries
3 types of capillaries
Continuous, fenestrated and sinusoid capillaries
What are continous capillaries
Compared to a typical endothelial tube where there are no gaps in between cells (think blood brain barrier)
What are fenestrated capillaries
Pours capillaries with decent sized holes for rapid exchange of water, solutes, gases. Found in brain ventricles, GI tract
Sinusoid capillaries
Also known as discontinuous endothelium. Capillaries with massive gaps that allow for free movement of plasma proteins. Found in liver, bone marrow, spleen
What is a capillary bed
Network of capillaries connecting metarterioles to venules
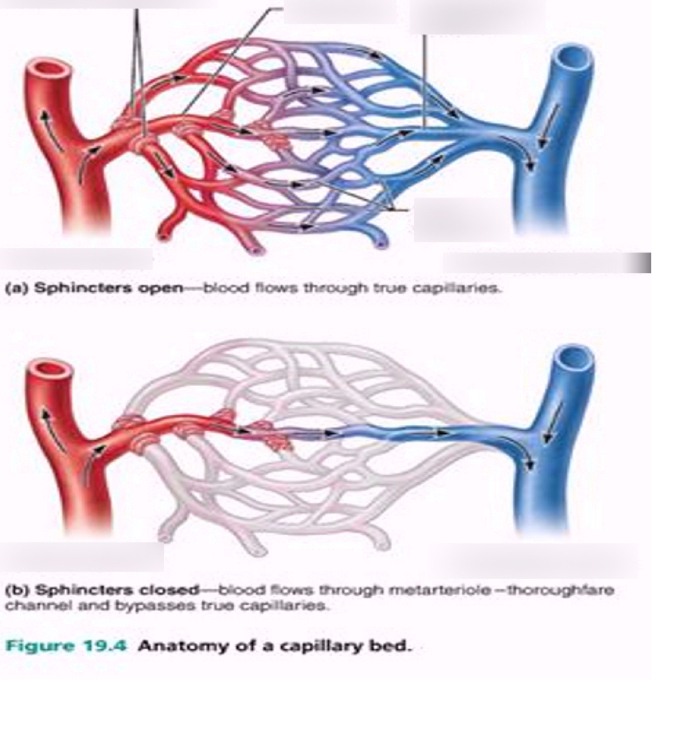
What does the opening of each capillary contain
A pre-capillary sphincter→controls amount of arterial blood flow through the capillary by relaxing and contracting several times a minute so that blood flows through in a pulsing fashion
How are pre—capillary sphincters controlled
Through auto regulation (no nervous system or endocrine involvement if working properly and controlled locally)
What is capillary exchange
Term used to describe all chemical and gaseous exchange from blood to body tissues that happens at capillary level. VITAL TO HOMEOSTASIS
How do materials move across capillary walls
Diffusion, filtration and reabsorption
Diffusion in capillaries
Net movement of ions across concentration gradient (higher to lower concentration) via channels (gaps in endothelium in fenestrated and sinusoid capillaries)
Filtration in capillaries
Removal of solutes as a solution flows across a porous membrane due to hydrostatic pressure
Reabsorption in capillaries
Opposite of filtration→As a result of osmosis in which water diffuses to follow solute, pulling extra water back into capillary
What layer of epithelium do venules tend to lack
Lack tunica media (no smooth muscle) except in larger venules
Main purpose of veins
Return blood back to heart
Thickness of layers in veins
Medium sized veins-Tunica media is thin with few smooth muscle, thickest layer is the tunica externa
Large veins (vena cavas)- all three layers are thickest
What type of pressure is found in veins
Very low pressure, has 10% that of arteries
What mechanisms aid blood flow back to heart in venules, medium sized veins
Venous valves and leg muscles
What are venous valves and their purpose, along with leg muscles in blood flow back to heart
Venous valves compartmentalize blood flow to eliminate backflow and blood pooling in the low pressure system. (Working against gravity)
Leg muscle movements push the valves open
Distribution of blood throughout vessels at any given time
30-35% in arteries and capillaries
65-70% found in Veins and venous system
Where and how much venous blood found in what organs
1/3 of venous blood in liver, bone marrow and skin
Vein advantage over arteries
Veins are more distensible due to less muscle with the ability to sustain greater volume without increasing pressure. Allows veins to act as blood reservoirs.
What is tissue perfusion?
Refers to adequate blood flow to the tissues, ensuring that the needs for oxygen and nutrients are being met
What factors influence tissue perfusion
Cardiac output, peripheral resistance and blood pressure (low BP=less tissue perfusion), activity of tissues (circulation and perfusion must increase to meet demands→in not, tissue death)
What mechanisms ensure adequate tissue perfusion
Auto regulation-capillary sphincters ensure perfusion
Vasomotion-changes in vessel diameter (constriction or dialation)
Correlation between blood flow and tissue perfusion
Adequate blood flow is needed to ensure adequate perfusion of tissues (oxygen supply)
What concept does blood flow often mirror
Cardiac output (CO=Heart Rate x Stroke volume) → decrease cardiac output= decreased capillary blood flow
What factors does capillary blood flow highly depend on
Directly proportional to pressure (more pressure=more flow)
Blood flow inversely proportional to resistance (more resistance=less flow)
What is blood pressure
Force exerted by blood against a vessel wall
What is necessary for blood pressure to overcome in order for adequate tissue perfusion
Must be enough to overcome resistance present in blood vessels (vascular resistance (general) and peripheral resistance (in systemic circuit))
Systolic blood pressure, what is it and average
Peak pressure exerted by ejected blood against vessel walls during cardiac systole
Average= 120 mmHg
Diastolic blood pressure
Minimum pressure in arteries when blood is draining off into vessels downstream
Average= 80 mmHg
Common average reading of blood pressure
120/80→ systolic blood pressure/ diastolic blood pressure
What is hypertension
When systolic blood pressure exceeds 140 mmHg (high blood pressure)
What is hypotension
When systolic blood pressure is below 90 mmHg (low blood pressure)
What is pulse pressure
Refers to the difference between systolic blood pressure and diastolic blood pressure and measures the strength of the pulse wave
120-80=40 mmHg
What happens when pulse pressure is too high vs low
If its too high→heart has to work harder to overcome peripheral resistance
If its too low→ heart doesn’t have time to relax (smaller difference)
What is mean arterial pressure
Refers to the average arterial pressure through one cardiac cycle, used to calculate overall blood flow and as a indicator of perfusion of tissues
Minimum mean arterial pressure to properly perfume tissue
In an adult MAP minimum is 65mmHg
Factors that affect blood pressure
Cardiac output and resistance
What is peripheral resistance
Resistance to the flow of blood through small vessels in systemic circuit (after load)
What is peripheral resistance determined by
Blood viscosity, blood vessel length, blood vessel diameter which all cause turbulence
What is total peripheral resistance impacted by
Vascular resistance, viscosity, turbulence
What is vascular resistance and how does it impact peripheral resistance
Determined mainly by FRICTION between blood and vessel wall (more friction, more slow), also impacted by vessel length and diameter (constriction, dilation, obstruction)
How does viscosity effect peripheral resistance
Refers to bloods thickness. The less viscous the blood the less resistance there is. In most cases one has normal blood viscosity except with disease (polycythemia (thick blood))
How does turbulence effect peripheral resistance
Altered blood flow during the swirling of blood, slows down blood and increases resistance.
What is stenosis
Abnormal narrowing of passageways (blood vessels)
Why are arterioles referred to as major resistance vessels
They are able to change diameter of vessels to distribute cardiac output and regulate arterial blood pressure
How do vasoconstriction and vasodilation affect resistance
Vasoconstriction→narrowing of vessel leads to increased resistance
Vasodilation→enlargement of inner diameter of vessel decreases resistance and increases flow through the vessel
Mechanisms to control blood flow and blow pressure classification
Auto-regulation→cause immediate, localized homeostatic adjustments (vasoconstriction and vasodialtion)
Central regulation→ neural and endocrine mechanisms when auto-regulation isn’t sufficient enough
What happens during dilation of pre capillary sphincters (vasomotion)
Local vasidilators that may cause dilation of precapillary sphincters include low O2 or elevated CO2, nitric oxide (NO), inflammatory meditators and increased tissue temperature
What happens during vasoconstriction
Often in response to vessel injury which causes endothelia release which stimulates vascular spasm to restrict blood flow and assemble platelets.
What is central regulation mainly in charge in
Controlling cardiac output and blood pressure through neural and endocrine controls
What type of changes do neural mechanisms detect?
Sense change in arterial pressure (baroreceptors) or blood gas level (chemoreceptors) at specific locations and adjust cardiac output and peripheral resistance to maintain blood flow to vital organs
What part of the brain contains cardiovascular centres? What are the centres referred to
Medulla oblongata;
Cardiac centres (cardioacceleratory, cardio inhibitory)
vasomotor centre
What do the cardiac dentures of the brain do?
Cardioacceleratory centre→sympathetic activation (increases cardiac output and increases blood pressure)
Cardio inhibitory centre→parasympathetic centre (decreases cardiac output and BP)
What does the vasomotor centre of the medulla oblongata do
Directs vasomotor responses in blood vessels; sympathetic input. Responsible for vasomotor tone (vessels never entirely relax). Change diameter and maintain pressure that way
2 groups of neurons tat control vasoconstriction and vasodilation
Vasoconstriction→adrenergic, NE secreted here, lots of neurons always active for tone
Vasodilation→smaller group of neurons, nitric oxide synthesis, chief vasodilator.
Baroreceptors reflex
These receptors are strategically located on carotid sinus, aortic arch and wall of right atrium to detect changes in stretch (related to blood pressure and communicate with CV centres to alter blood pressure
Effects of baroreceptors
1. Decreases cardiac output
2. Causes widespread peripheral vasodilation
Aiming to calm down sympathetic nervous system
STIMULATES VAGUS NURVE →vasovagal response drops blood pressure
VASODILATES TO DECREASE BLOOD PRESSURE
What is the chemoreceptors reflex
Involves a coordinated effort between cardiovascular and respiratory system.
Chemoreceptors respond to changes in the chemical composition/pH of fluid in arteriole blood and cerebrospinal fluid. (O2 level, CO2 level and pH levels) carotid sinuses and aortic bodies.
How do chemoreceptors respond to conditions?
Increased CO2 (decrease in O2 or pH) → stimulates cardioacceleratory and vasomotor centres→increased heart rate and cardiac output, increased blood pressure→stimulation of respiratory centres in medulla to increase BR and O2 intake
Type of changes make by endocrine mechanisms
While neural is immediate and short term, hormones can enhance direct longer term changes
Endocrine mechanisms to know
Adrenal medulla, ADH, aldosterone, angiotensin II, erythropoietin, natriuretic peptides
Adrenal medulla impact on cardiovascular system
Stimulated by the sympathetic nervous system→epinephrine and norepinephrine stimulate increased heart rate, cardiac output and blood pressure stimulate vasoconstriction
ADH or VASOPRESSIN effect on cardiovascular system
Released from Post.Pit in response to decreased blood pressure, increased solute concentration or increased angiotensin II
Stimulates conversation of water by kidneys to elevate blood pressure
Aldosterone effect on cardiovascular system
Released from adrenal cortex in response to low Na+ levels or increased angiotensin II→ stimulates conservation of Na+→water retention→increased blood pressure
Angiotensin II effect on cardiovascular system
In response to decreased blood flow, aims to increase blood pressure
What is renin-angiotensin-aldosterone system
Key regulator where renin released in kidneys causes inactive angiotensin→angiotensin I (still inactive)→angiotensin converting enzyme→angiotensin II (active)→stimulates aldosterone secretion→increases BP
Functions of angiotensin II
Stimulates aldosterone secretion (Na+ conservation)
Stimulates ADH secretion (water conversation)
Stimulates thirst
Stimulates increased cardiac output
Stimulates vasoconstriction (potent vasoconstriction)
Increases blood pressure