Pulm EXAM 1
1/118
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
119 Terms
State the four functions of the lungs
Exchange gases (“arteriolize” pulmonary venous blood)
Metabolize select compounds
a. Peptides (angiotensin I, bradykinin)
b. Amines (serotonin, norepinephrine)
c. Arachidonic acids (prostaglandins, leukotrienes)
Filter the circulation
Serve as a blood reservoir for left ventricle
~70-100 ml in pulmonary capillaries
~500 ml in bronchial circulation
2. Given a diagram of the human body, identify each of the following:
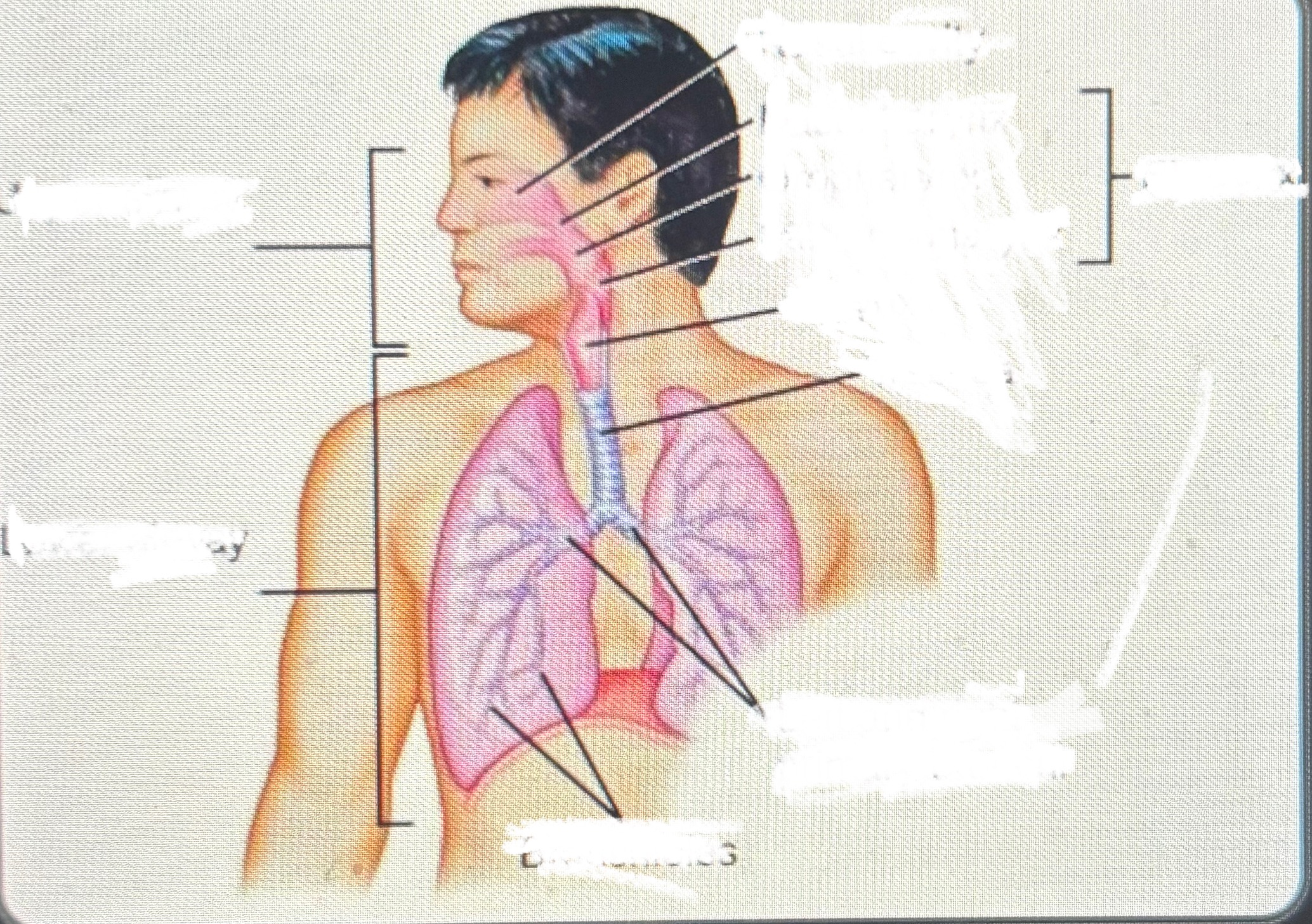
The five airway wall layers and their function
Epithelial - Pseudostratified ciliated epithelial cells
Basement membrane - Structural (support) function
Submucosal- contains submucosal glands that produce mucus and blood vessels
Smooth muscle
Cartilage - larger airways only; provides airway support with flexibility
Conducting Zone
The pathway for airflow, but not gas exchange
Respiratory Zone
Where the magic happens, gas exchange begins and occurs
principal muscles of inspiration
Accessory
Sternocleidomastoid
Scalene Groups
Pectoralis minor
Principal
External intercostals
Diaphragm
principal muscles of expiration
Quiet breathing
expiration results from passive, elastic recoil of the lungs, dip cage and diaphragm
Active breathing
Internal intercostals
Abdominals
Quadratus Lumborum
Epithelium type I pneumocytes function
Support
Epithelium type II pneumocytes function
metabolically active; secrete surfactant
Alveolar macrophage function
Clear the alveolar space of mucus and debris
Alert immune system
Lymphatics
Helps clear fluid, protects lungs from issues (particles)
Fluid balance
Phrenic Nerves
Motor innervation to the diagram, our principal muscle of respiration
6. State why ventilation and perfusion are greatest at the base of the lung.
gravity (closer to the earth)
7. State the role of the medullary respiratory control center, cortex and pons in the control of ventilation.
Medullary respiratory control center - “on/off” system
Cortex (voluntary)
Pons (controls the rate of involuntary respiration)
There are many sensors in this system to tell the control center how to regulate respiration
Describe the effect of changing area, thickness and diffusion capacity on the diffusion of oxygen and carbon dioxide.
Increase in area = Lower Vgas, Decrease in area = Higher Vgas
Increase in thickness = Lower Vgas, Decrease in thickness = Higher Vgas
Increase in diffusion capacity = Higher Vgas, Decrease in diffusion capacity = Lower Vgas
Cardiopulmonary circulation
Deoxygenated blood enters the right atrium from:
Superior vena cava (from upper body)
Inferior vena cava (from lower body)
Flows into the right ventricle
Pumped through the pulmonary artery → lungs
In the lungs:
CO₂ is exhaled
O₂ is absorbed into blood
Oxygenated blood returns to the left atrium via the pulmonary veins
Flows into the left ventricle, then pumped to the rest of the body via the aorta
Systemic circulation:
The pathway of blood from the left side of the heart to the body tissues and back to the right side of the heart
PaCO2
Respiratory alkalosis/acidosis
Bicarbonate
Metabolic Acidosis/Alkalosis
Hemoglobin Right Shift
CADET
C: CO2 increase
A: Acid increase (low pH)
D: DPG increase (2,3-BPG)
E: Exercise
T: Temperature increase
(hemoglobin less affinity for O2 release oxygen more quickly)
Hemoglobin left shift
- Body does not need as much oxygen, curve shifts to the left. (O2 conservation)
oral candidiasis - THRUSH
White slough on tongue
Looks like cottage cheese or milk curds
When the patches are wiped away, area underneath is red and may bleed
Edema
Swelling of throat and structures in mouth
Pharyngitis
“Group A Streptococcus”
White and Red splotches
Swollen Uvula
Viral
Redness in throat
Xerostomia
dry mouth bumpy tongue
Leukoplakia
white spilled paint
State the mechanism of action of antihistamine drugs.
H1 inverse agonist
Block the immediate hypersensitivity reaction: Anaphylaxis and Allergic reactions:
H1 antihistamines block the increased capillary permeability and formation of edema and swelling caused by histamine.
Explain two major pharmacological differences between 1st and 2nd generation antihistamines.
1st generation crosses BBB (causes sleepiness), while 2nd generation doesn’t
1st generation interacts with multiple other receptors causing a variety of unwanted effects, while 2nd generation specifically interact with peripheral H1 receptors
Polar groups
Do not cross BBB - 2nd gen
Allergic Rhinitis
Disease caused by an IgE-mediated inflammatory response of the nasal mucous membranes after exposure to inhaled allergens
seasonal allergic rhinitis
Occurs during different seasons
perennial allergic rhinitis:
Occurs from year round exposure (dust mites, mold, etc.)
intermittent allergic rhinitis:
Symptoms or exposure < 4 days per week OR < 4 weeks
persistent allergic rhinitis
Symptoms present >4 days per week AND >4 weeks
episodic allergic rhinitis
Not normally encountered in the individual’s usual environment (Episodic exposure, cat allergy)
rhinitis medicamentosa
Nasal mucosal inflammation caused by topical nasal decongestant overuse (greater than 7-10 days)
AR
allergic rhinitis
PAR
perennial allergic rhinitis
SAR
seasonal allergic rhinitis
OAH2G
oral antihistamines 2nd gen
INAH
intranasal antihistamine
PSE
pseudoephedrine
INCS
intranasal corticosteroid
IND
intranasal decongestant
INAC
intranasal anticholinergic
INC
intranasal cromolyn sodium
SLIT
sublingual immunotherapy
SCIT
subcutaneous immunotherapy
Describe the immune response to allergens.
Sensitization
IgE production
Arming of mast cells
Release of mediators
Clinical effects
Immediate vs. Delayed Reaction
Onset
Cellular involvement
Symptoms
Histamine action
Stimulates irritant receptors
Pruritis
Increased Vascular and mucosal permeability
Smooth muscle Contraction
Neutrophil Chemotactic factor Action
Inflammatory cell influx
Eosinophil Chemotactic factor Action
Inflammatory cell influx
Kinins
Increased vascular permeability
N-a-tosyl -arginine methylesterase action
Increased vascular permeability
Leukotrienes
Smooth muscle contraction
Increased vascular permeability
Thromboxanes
Smooth muscle spasm
Platelet Activation factor
Mucus Secretion
Increased Airway and vascular permeability
Chemotaxis
Heparin
Anti-inflammatory
Tryptase and kallikrien
Protein Hydrolysis
Allergic rhinitis
Bilateral
Frequent (Paroxysmal) Sneezing
Rhinorrhea Anterior and Watery
Frequent pruritis
Nasal obstruction variable
Non Allergic rhinitis
Unilateral
Infrequent Sneezing
Rhinorrhea Posterior and Watery and thick
Nasal obstruction usually present
Allergic shiners
swelling and darkening of circles under the eye due to nasal obstruction and venous congestion
Dennies lines
fold or crease of skin below the lower eyelid
Allergic crease/ allergic salute
visible line across the bridge of the nose due to repeated rubbing or pushing upwards of the nose
Allergic Gape
open mouth breathing due to allergic rhinitis and its long-term complications
Identify drugs that cause nonallergic rhinitis.
Local inflammatory
Acetyl salicylic acid
NSAIDs
Neurogenic
Alpha- and beta- adrenergic blockers (clonidine risperidone, methyldopa)
Ganglion blockers (trimethaphan)
Phosphodiesterase-5 inhibitors (sildenafil)
Calcium channel blockers
Angiotensin converting enzyme inhibitors (ACEi)
Gabapentin
Psychotropics
Rhinitis medicamentosa
Intranasal decongestant
Identify the medications that must be held prior to skin prick/puncture or intradermal allergy skin testing.
First generation antihistamines - at least 3 to 5 days before testing
Second generation antihistamines - at least 7 days before testing
Medications that interact with epinephrine (tricyclic antidepressants, beta-blockers)
Identify exclusions to self-care of allergic rhinitis.
Children ≤ 12 years old
Pregnant or lactating women
Symptoms of nonallergic rhinitis
Symptoms of otitis media, sinusitis, bronchitis, or other infection
Symptoms of undiagnosed or uncontrolled asthma (wheezing or shortness of breath)
Severe or unacceptable side effects of treatment
Identify adverse effects associated with antihistamines, decongestants, intranasal corticosteroids, cromolyn sodium and antileukotrienes.
Antihistamines: Drowsiness, anticholinergic, epigastric distress
Decongestants: Rhinitis medicamentosa (caused by intranasal decongestants), Contraindicated in pregnancy – risk of birth defects
Intranasal corticosteroids: sneezing, stinging, headache, epistaxis
Cromolyn sodium: Local irritation (sneezing and nasal stinging)
Antileukotrienes: BBW: behavioral changes and serious neuropsychiatric events
State the place in therapy of allergic rhinitis for nasal saline (nasal spray and nasal irrigation) and immunotherapy.
Nasal saline: removing mucus from the nose and clearing blocked nasal passages
Immunotherapy: considered for patients whose symptoms are not relieved with pharmacologic management and for those who are experiencing undesirable adverse effects
Differentiate between the advantages and disadvantages of subcutaneous and sublingual immunotherapy.
Subcutaneous immunotherapy
Earlier and more pronounced response
Local: redness and induration at site of injection
Systemic: urticaria, GI upset and wheezing
Provider administered
Sublingual immunotherapy
Safer
Self-administered tablet
Local: oral itching and discomfort
Nasal spray administration:
Clear nasal passages gently before administration
Wash hands before and after
Gently depress the other side of the nose with finger to close off the nostril not receiving medication
Aim tip of delivery device away from nasal septum to avoid accidental damage to the nasal septum
Activate the spray. Do not sniff
Breath through the mouth and wait a few minutes after using the medication before blowing the nose
Immunotherapy administration:
First dose to be given in providers office; monitor for 30 min at least
Always have epi-pen available
Instructions:
Handle with clean, dry hands
Remove from blister pack
Place under tongue
Hold under tongue and allow to dissolve completely
Wash hands after handling
Do not ingest food or beverages for 5 minutes after dose
State the black box warning for subcutaneous (SCIT) and sublingual immunotherapie (SLIT)
SCIT: uncontrolled asthma
SLIT: anaphylaxis (good for self administration)
Describe the management of rhinitis medicamentosa.
Discontinue nasal decongestant
May require intranasal corticosteroids or short course of oral corticosteroids
Mild Intermittent Allergic Rhinitis
1st- Oral Antihistamine (2ng gen) or INAH
Mild Persistent Allergic Rhinitis
INCS
Moderate/Severe Intermittent Allergic Rhinitis
1st- Oral Antihistamine (2ng gen) or INAH
Moderate/Severe Persistent
INAH and INCS
Mild Intermittent non allergic rhinitis
INAH
Mild Persistent non allergic rhinitis
INAH
Moderate/Severe Persistent non allergic rhinitis
INAH + INCS
Moderate/Severe Intermittent non allergic rhinitis
INAH
Common cold mechanism role of ICAM
cell surface protein involved in cell adhesion and inflammation of the airway that lead to symptoms like cough
Describe the mechanism of cough production and different types of cough
A cough is an innate primitive reflex and acts as part of the body’s immune system to protect against foreign materials
The most common causes of chronic cough are postnasal drip, asthma, and acid reflux from the stomach
Other causes of cough include smoking, infections (viral and bacterial), some medications and lung diseases
Pertussis, also known as whooping cough, is an illness with a classic clinical finding of paroxysmal episodes of intense coughing lasting up to several minutes followed by a loud gasp for air.
It is an infection of the respiratory tract by Bordetella pertussis, where the bacterium produces a toxin, pertussis toxin (PTx), that affects the cyclic AMP signaling through inhibition of Gi in many cell types including neutrophils and epithelial cells. The infection induces mucopurulent sanguineous exudate formation within the respiratory tract
PTx is extensively used in signal transduction studies in cell biology
Smokers cough: A tobacco smoking-induced cough can start off dry and hacky in the early stages and then become more phlegmy and productive as the cough progresses
Chronic cigarette smoke-induced desensitization of airway cough receptors and paralysis of the ciliated cells in the airway
Smoking cannabis also induces chronic cough
ACEI cough → bradykinin build up
Non Productive (Dry Cough):
Needs to be suppressed
Incessant non-productive cough leads to loss of sleep, rib fractures, pneumothorax, rupture of surgical wounds and syncope
Productive Cough (Wet Cough)
Needed to clear airways; dangerous to suppress
Beneficial as it expels irritating substances such as dust, pollen, fluids and inflammatory cells from the upper respiratory airways
Recall and describe the mechanism of cough suppression
General Mechanism of Cough Suppressants (Antitussives)
Via the CNS, by raising the threshold of cough centers
Via the periphery to reduce cough impulse
CNS acting cough suppressants
Opioids (cross BBB)
Suppress cough reflex on cough center (medulla)
Via mu and kappa opioid receptors
G protein coupled receptors
Moderate acting opioid agonist drugs
Codeine
Hydrocodone
Non-opioids (cross BBB)
Suppress cough reflex in cough center (medulla)
Via sigma receptors (and other receptors)
Drugs
Dextromethorphan (synthetic)
Sigma 1 receptor
Diphenhydramine (antihistamine)
Benzonatate
Peripheral acting cough suppressants
Antitussives & Demulcents
A demulcent (cough drop) is a high molecular weight compound that coats the skin surface
Peripheral acting agents work either by anesthetizing the local nerve endings or acting as demulcents
Demulcents have a soothing effect on the throat
Camphor, menthol, eucalyptus oil
Expectorants
Help thin and loosen mucus so you can cough it up more easily
Helps body get rid of excessive mucus more quickly
The active ingredient in OTC cough expectorants is guaifenesin
Found in mucinex, robitussin cough, and chest congestion DM
Used in patients who have thick, tenacious respiratory tract secretions and in sinusitis
Acute cough
less than 3 weeks
Subacute
Cough between 3-8 weeks
Chronic
more then 8 weeks
2. State common medical conditions associated with acute cough, subacute cough, and chronic cough.
Acute: Upper respiratory tract infection (dry), acute bronchitis (dry), pneumonia (dry or wet), GERD, asthma (wet or dry), HF (dry)
Subacute: Upper respiratory tract infection (dry), upper airway cough syndrome (dry)
Chronic: Chronic bronchitis (wet), upper airway cough syndrome (dry), GERD, asthma (wet or dry), HF (dry)
3. Identify the signs and symptoms of common medical conditions associated with cough.
Upper respiratory tract infection (URTI; “common cold”): Acute dry cough; rhinorrhea/nasal obstruction, sneezing, sore throat
Acute bronchitis: Acute dry cough; often follows viral URTI; ± wheezing, mild dyspnea, chest wall and substernal musculoskeletal pain
Chronic bronchitis: Chronic wet cough; COPD signs/symptoms/history
Pneumonia: Acute wet or dry cough; abnormal vital signs (fever, tachypnea, tachycardia), mental status changes especially in the elderly
Upper Airway Cough Syndrome (UACS): Acute or chronic dry cough; postnasal drip sensation, frequent throat clearing, ± rhinorrhea
Gastroesophageal reflux syndrome (GERD): Acute or chronic dry cough; heartburn, regurgitation, dysphagia
Asthma: Acute or chronic wet or dry cough; episodic wheezing and shortness of breath
Heart failure: Acute or chronic dry cough; cough with exertion or supine; heart failure signs (+S3, displaced apical pulse, increased jugular venous pressure, peripheral edema, weight gain)
Pulmonary emboli: Abrupt onset dry cough; dyspnea, pleuritic chest pain, hemoptysis, tachypnea, tachycardia, peripheral edema
Lung cancer: Persistent cough/worsening dry cough; acute changes in chronic “smokers cough”, hemoptysis, recurrent pulmonary infections, new onset wheezing
Common complications cough
Exhaustion
Sleep deprivation
Musculoskeletal pain
Hoarseness
Excessive perspiration
Social embarrassment
Urinary incontinence
less common
Syncope
Stridor
Pneumothorax
Rib fractures
Cardiac arrhythmias
Dextromethorphan MOA/dosage
Acts on the cough center in the brain to reduce the urge to cough, sigma
10-20 mg q4-6. max 120mg
Codeine MOA/ Dosage
Acts centrally on the cough center of the brain, reducing the sensitivity of the cough reflex, kappa mu
10-20mg q4-6h max 120mg
Guaifenisin MOA/ Dosage
involves increasing the volume and reducing the viscosity of respiratory tract secretion
Unknown; may increase respiratory tract hydration
200-400mg q4h max 2400mg
Benzonotate MOA/ Dosage
Anesthetic
Tetracaine congener; topical anesthetic action on respiratory stretch receptors (lung airways)
100-200mg TID max 600mg
Dextromethorphan Adverse effects
Dizziness, drowsiness, nausea, and gastrointestinal upset
Should not be take with monoamine oxidase inhibitors (MAOIs)/ medications that increase serotonin levels (serotonin syndrome)
Codeine Adverse Effects
dizziness, constipation, nausea, and respiratory depression, particularly at higher doses