01 Canine orbit, enucleation and Eyelids (part 1)
1/63
Earn XP
Description and Tags
LO: To be familiar with the clinical signs of orbital disease, and how clinical signs may be useful in distinguishing neoplastic from inflammatory causes LO: To be aware of how exophthalmos may be investigated further in first opinion practice, and treatment of retrobulbar bacterial infection LO: To recognise and treat traumatic proptosis in the dog LO: Know the common indications for enucleation in the dog LO: Be familiar with the trans-palpebral technique for enucleation LO: To have a basic knowledge of the anatomy and function of the external eyelids LO: Know how to examine the external eyelids in the first opinion practice setting LO: Be able to define distichiasis, conjunctival cilia, and trichiasis and understand how these conditions present
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
64 Terms
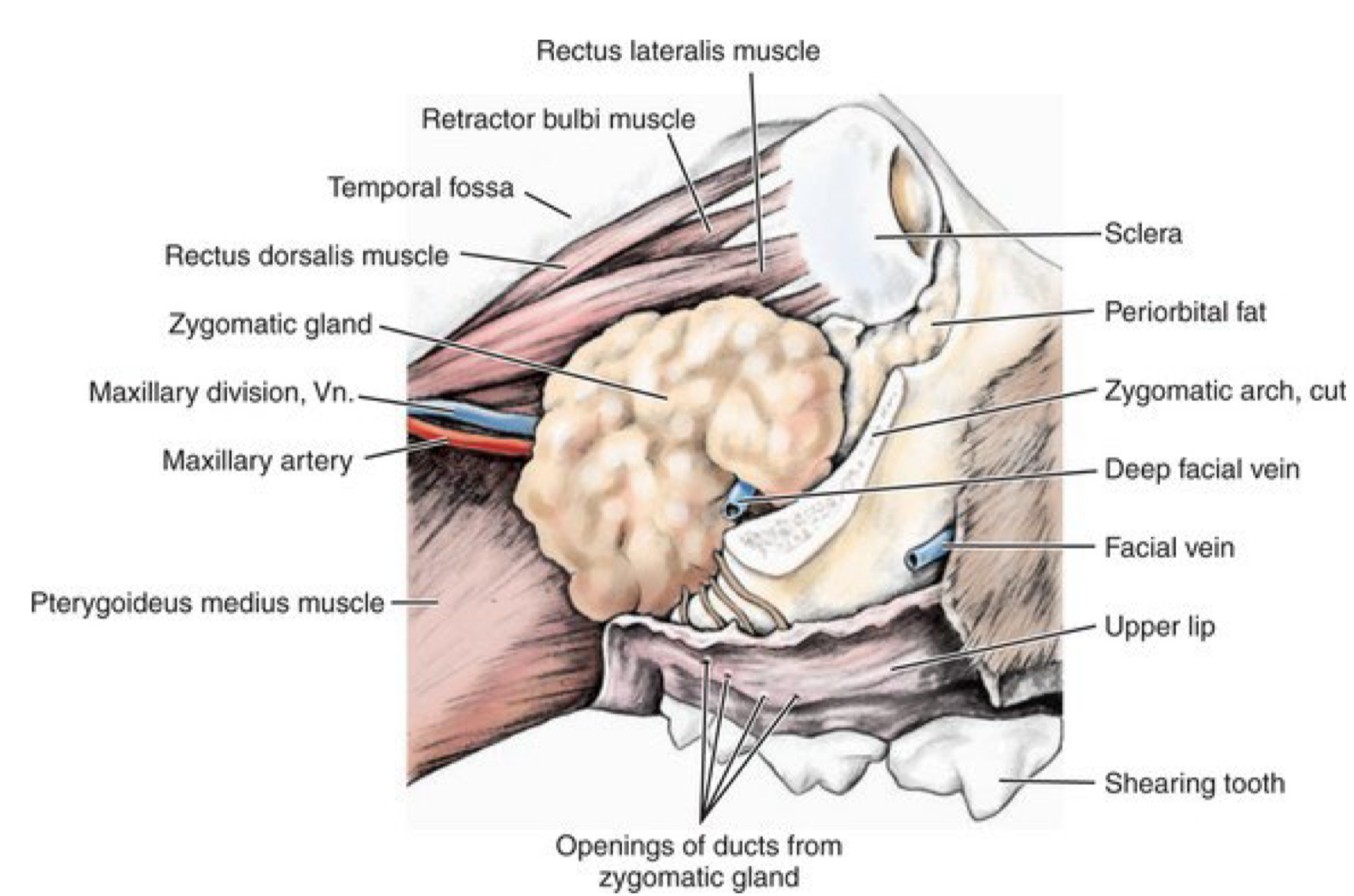
canine orbit typeexophthalmos
open
opent type orbit
Incomplete in the temporal or dorsal temporal region—> continuous with the temporal fossa
canine orbit is divided into
Intraconal space
extraocular muscles, CN II, III, IV, V(1), VI)
Extraconal space
neurovascular structures
nictitating membrane
zygomatic salivary gland
neighbouring structure of canine orbit?6 what is the significance?
caudal nasal cavity,
paranasal sinuses,
masticatory muscles,
caudal maxillary molar teeth,
pharynx
zygomatic salivary gland
diseas may extent into orbit
Hallmark clinical sing of orbital disease
exophthalmos
exophthalmos
anterior displacement of globr along orbital axis
how do you derernmine exophthalmos
viewing the patient from above
exopthalmos often associated with
increased resistance to digital retropulsion of the globe
Other Clinical signs of orbital disease
x increase resistnace
x exophthalmos
Strabismus: rotation of the globe away from the normal optical axis e.g. exotropia or esotropia
Pain on opening the mouth (esp. nflammatory conditions) or reluctance to eat and chew
Protrusion of the nictitating membrane
Periocular swelling
Chemosis (swelling) and conjunctival hyperaemia
Epiphoramucopurulent ocular discharge
Keratoconjunctivitis sicca
Visual and afferent pupillary defects
Decreased ocular motility
Decreased eyelid and periorbital sensation
Lagophthalmos +/- exposure keratopathy /corneal ulceration
Swelling, induration or fistula of the oral mucosa in the pterygopalatine fossa (caudal and medial to the
second maxillary molar tooth)Retinal folds / scleral indentation / tortuous engorged retinal blood vessels / papilloedema
Lagophthalmos
condition preventing eyelid from closing completely
common ddx diagnosis: exophthalmos
Retrobulbar cellulitis or abscess
Retrobulbar neoplasia
less common ddx: exophthalmos
Myositis of masticatory or extraocular muscles
Adenitis of the zygomatic salivary gland (sialoadenitis)
Retrobulbar haemorrhage
Cystic space-occupying lesions of the nictitans gland/ zygomatic mucocoele
Dacryops
Dermoid cyst
unilateral or bilateral orbital disase more comon
unilateral
bilateral involvement suggest
myositis
bilateral sialoadenitis
Retrobulbar abscess/cellulitis
aetiopathogenesis
inflammatory disease of neighouring periorbital structure or space
can be
direct inoculatoion
or secondary to orbital FB or septicaemia
Retrobulbar abscess/cellulitis
clinical sign
Acute onset / rapid progression
expophthalmos
Discomfort on opening the mouth + globe retropulsion
perorbital swelling sensiticity
marked conucntical hyperaemia
Pyrexia, anorexia and neutrophilia with left shift may be present
Retrobulbar abscess/cellulitis
investigation
Orbital ultrasonography
Radiographs of the caudal maxillary molar tooth roots
evidence of periodontal or endodontic disease
Examination of the oral cavity
particular attention to the pterygopalatine fossa and the maxillary molar teeth
may need GA
period of stabalisation may be needed in systemically unwell px
On ultrasound, retrobulbar abscesses often have
vs orbital cellulitis
a well-defined hyperechoic wall surrounding a uniformly
orbital cellulitis: subtle changes in the
normal retrobulbar space
distortion or obliteration of the normal retrobulbar architecture
retrabnormal mixed echogenicity
Retrobulbar abscess/cellulitis
SHOULD BE TREATED AS EMEGENCY
urgent investigation and instigation of
appropriate management to preserve the globe and its function
Retrobulbar abscess/cellulitis
management: emergency
if abscess is not seen on ultrasound
Initial treatment with a potentiated-
penicillin (amoxicillin/clavulanic acid) or cephalosporins while waiting on C+C resultusually mixed aerobic and anaerobic
empirical broad-spectrum antibiotics (3-4 weeks) and NSAIDS
generally results in rapid improvement.
Retrobulbar abscess/cellulitis
management: emergency
if lagophthalmos are apparent
Initial treatment with a potentiated-
penicillin (amoxicillin/clavulanic acid) or cephalosporins while waiting on C+C resultusually mixed aerobic and anaerobic
empirical broad-spectrum antibiotics (3-4 weeks) and NSAIDS
appropriate topical treatments to manage or prevent exposure keratitis are indicated
Retrobulbar abscess/cellulitis
management: emergency
if ultrasound indicate abscess
drain pus through oral approach (pterygopalatine fossa)
periapical( tooth root) abscessation:
extraction of tooth
Gentle probing of the alveolar bone may reveal direct communication with the orbit and allow drainage of the orbital abscess
if not then sx pterygopalatine fossa drainage
If radiographs of the maxillary dental arcade reveal evidence of periapical
abscessation
extraction of the affected tooth is indicated
entle probing of the alveolar bone may reveal a direct
communication with the orbit
allow drainage of the orbital abscess.
If drainage inadequate, surgical drainage via pterygopalatine fossa
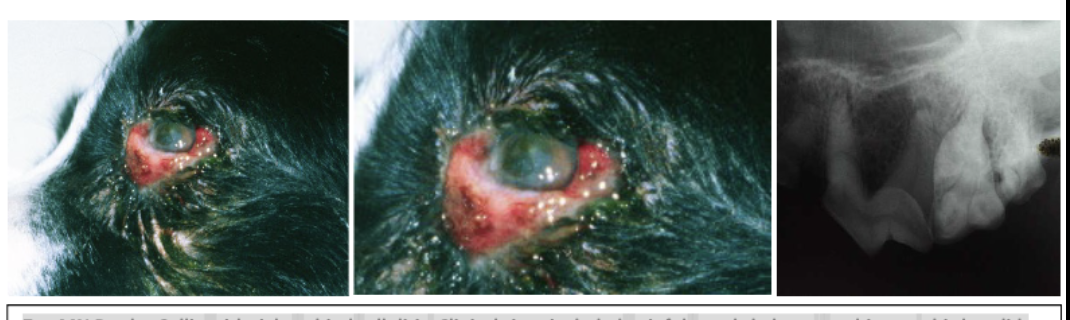
7yo MN Border Collie with right orbital cellulitis. Clinical signs included painful exophthalmos, strabismus, third eyelid protrusion and exposure keratitis
dental radiographs identified periapical abscesses of the maxillary molar teeth.
Retrobulbar abscess/cellulitis
prognosis
generally good,
rapid improvement on appropriate antibiotics
combined with orbital drainage when orbital abscessation is present.
If recurs on completing the course of treatment
foreign body may be implicated
referral for advancing imaging
surgery should be recommended
Retrobulbar neoplasia
aetiopathogenesis
primary
arises from orbital structures
secondary
local extension from
adjacent structures or metastasis from distant sites
generally affects older patients (> 8 years)
often follows a more insidious course
leading to a late presentation when tumours are well-advanced
most common orbital tumour
Nasal adenocarcinoma
Retrobulbar neoplasia prognosis
late presentaion, 90% malignant,
guarded or grave
Retrobulbar neoplasia
clinical sign
Hx:
slowly progressive
unilateral exophthalmosstrabismus
third eyelid protrusion
without pain on opening the mouth or on palpation of periocular tissues
reduced air flow through the nostril of the affected side (common originate from nsal cavity)
importance to check for disseminted diseas and sample non orbital diseae
Retrobulbar neoplasia
Investigaton
Physical exam importatnt
Lymphadenomegaly or organomegaly —> increase suspicion of disseminated disease
Sampling of more accessible non-orbital tissues may be more appropriate
orbital US (most tumours appear variably hyperecoic)
plain film radiography : abd and thorax
extension from the nasal cavity, loss of orbital bone
both are poor prognostic indicators.
Sample: FNA/ US biopsy
typing tumor
grading needs: Rx thorax and abdo, abdo ultrasound
(if tx considered)
CT or MRI
demonstrate the extent of the neoplasia more fully, and frequently indicate the origin of the tumour.
Retrobulbar neoplasia
pronosis
generally guarded
unless advance img suggest sx can be curative
Traumatic proptosis
Protrusion of the globe with eyelids behind equator of globe
only occurs as a result of trauma where it often becomes entrapped
orbicularis oculi muscl spasm—> exaccerbated
minor trauma posisble in brachy: better chance retain vision
evaluateion of concurrent craniofacial and CNS injury
Traumatic proptosis
evaluateion of concurrent craniofacial and CNS injury
Strabismus from torn extraocular muscles is common (medial rectus typically affected)
lateral strabismus.
Chemosis and corneal ulceration
uveitis,
glaucoma or
hypotony and hyphaema.
Neuro-ophthalmic examination
visual deficits
pupillary abnormalities
prognostic indicator for cision
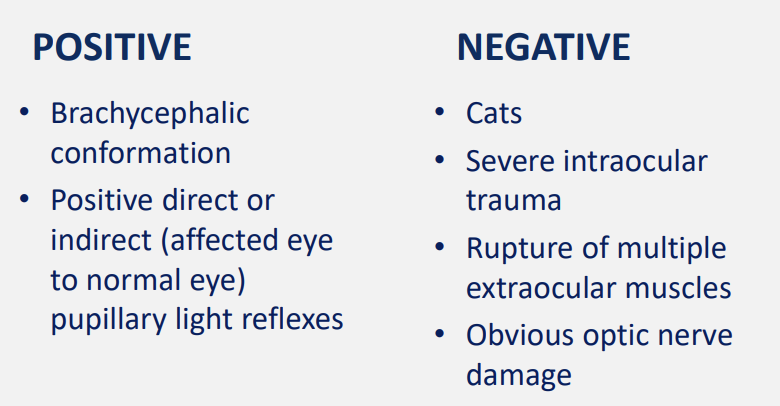
when is enucleation indicatied in traumatic proptosis
damage to the globe, extraocular muscles and / or optic nerve is severe
prognosis for salvaging even a non-functional globe is poor
Replacement of proptosed globe sx steps
GA, clean ocular surface with povidone iodine (1:50 solution), fluorescein, flush again
gentle forward traction applied to the eyelids, lateral canthotomy —> tension release
eyelids drawn forward over the ocular surface
protect the cornea as the sutures are tightened.
tissue swelling— not possible to return globe to normal position in whiere corneal surface will be protected—> Temporary tarsorrhaphy
Pass suture upper eyelid first ~ 5mm from lid margin exiting eyelid margin at level of meibomian gland openings
Direct needle through meibomian gland opening on opposite lid, exit through skin
routinely closed (figure 8), eyelids sutured together for 14 days
simple interrupted
partial thickness horizontal mattress sutures emerging through the lid margins
ensure suture material not contacting the cornea
Replacement of proptosed globe sx
aftercare
how long does the suture have to stay in?
B/S systemic antibiotics if wound open and contaminated
nsaids & analgesia
Appropriate topical antibiotics applied via small gap left open at medial canthus
Leave sutures in place at least 2 weeks
prolapse globe treatment complicaion
long term complications leading to patient morbidity
permanent blindness
lagophthaalmos
neurotrophic keraitits
KCS
permanent strbismus
phthis bulbi
indications for enucleation
Unmanageable ocular disease associated with pain or risk to the patient
Intraocular neoplasia/neoplasia— cannot be removedc without sacrificing globe
Non visual eye + intractable pain
Chronic glaucoma, irreversible loss of vision + evidence of discomfort
Panophthalmitis (inflammation of all intraocular structures and sclera) refractory to treatment
Severe ocular trauma – e.g. proptosis with ON transection
importance: enucleation post op care
often best welfare option for O with money contraint
what to do post enucleatiokn
access demeaanour following removal
histo assessment
store glbe in formalin in case later prob
enucleation
Magnification and lighting
Magnification ranging from ____ Working distance of_____
Magnification: 1.5 to 8x;
Working distance: ~ 20 - 50 cm
Major disadvantages of loupes include: (4L)
lack of variability in magnification
limited magnification
limited field of view (smaller at higher mag)
limited depth of field
enucleatio pre op prep
instrument set: personal pref. bishop harmon forcep; 4/0 monocryl 6/0 vicryl)
meticulous haemostasis: Clamp bleeding vessels Ligate larger vessels Thermal cautery Bipolar cautery Care with monopolar cautery – esp in orbit
px postition: vacuum positioning. px insulatied from cold table, resistant to infectant
hair clipping: avoid rash, prep aseoptically (1:50 ocular serviei; 1:10neyelid)
enucleation anaesthesia
retrobulbar nerve block prior to enucleation reduce postoperative pain and anaesthetic requirements.
cureved retrobulbar needle
Alternatively, a splash block of the orbit once the eye has been removed can help with post-operative discomfort
enucleation species and breed consideration
CATs
Short optic nerve
Tractional injury to contralateral Optic nerve via chiasm
DO NOT clamp or ligate the ON
Rabbit
Large orbital venous sinus
Retrobulbar lobes of tear glands
Risk for haemorrhage
goal of transpalpebral enuceleation
Removal of globe, eyelids and conj sacs in one unit
Not entering conj sac (Infectious/neoplastic contamination of orbit)
Eyelids sutured together or held by Allis tissue forecps
Transpalpebral enucleation technique
The eyelids are held together with Allis tissue forceps and the skin incised around
them.
• Use scissors to section the lateral canthal tendon, and dissect back to the
conjunctival reflection.
• Once posterior to this, work as close to the globe as possible, sectioning each of
the rectus and oblique muscles in turn at their tendons of insertion (this will
drastically reduce haemorrhage as the muscle bellies are very vascular). The retractor
bulbi muscles surround the optic nerve and usually obscure it
• Continue the plane of dissection medially, sectioning the short tight medial canthal
tendon to free up the outer surface of the third eyelid
• Avoid at all costs applying tension to the optic nerve (ON), as this may damage the
chiasm and blind the patient in the remaining eye (traumatic optic neuropathy).
Rotate the globe medially to expose the retractor bulbi muscles surrounding the
optic nerve rather than using traction. Section the retractor bulbi muscles and optic
nerve without clamping them first. Clamping the ON increases the risk of
contralateral traumatic optic neuropathy
• If there is any residual bleeding apply digital pressure with a gauze swab (for 5
mins). Close deep orbital tissue, then place a continuous layer in the deep tissue
attached to the lids (try to make this layer watertight). Finish with skin sutures.
• Maintaining even pressure over the closed wound with an ice pack (covered by a
cloth moistened with sterile saline) for 10-20 minutes during the recovery period
will reduce haemorrhage into the orbit/eyelids and subsequent swelling.
• Provide good post-operative analgesia and systemic NSAIDs