B5: CMG Exam 3 pt 2
1/376
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
377 Terms
abdominal pain
acute (abdominal pain/abdomen):
-describes a Sx that can be caused by a long differential diagnosis
abdomen
acute (abdominal pain/abdomen):
-medical condition characterized by peritoneal sign that require immediate surgical intervention rather than waiting on labs and imaging
-acute mesenteric ischemia + bowel obstruction may present as this, but are typically late clinical presentations
small bowel obstruction
What disorder:
-caused by a variety of pathologic processes that obstruct the bowel
-mechanical or functional blockage of the small intestine preventing the normal transit of products of digestion
Types:
1. Simple Mechanical = obstruction occurs at a single point
2. Mechanical Closed-loop ("strangulation obstruction) = obstructed at 2 locations creating a segment of bowel w/ both proximal and distal blood flow compromise, can cause intestinal infarct + necrosis much quicker than simple obstruction
3. Functional = occurs due to disruption of normal coordinated peristaltic activity of the GI tract in absence of a physical blockage within the intestinal lumen (most commonly = adynamic ileus)
4. Pseudo-obstruction = due to chronic diseases --> disruption of nerves/innervations to peristaltic mm. (Ex = Hirschsprung disease)
bowel obstruction
What is a mechanical or functional blockage of the intestine preventing the normal transit of products of digestion?
post-operative adhesion
What is the most common extrinsic cause of a small bowel obstruction/ileus?
1. post-operative adhesions
2. compressing masses (e.g., tumors, abscesses, hematomas)
3. hernias
4. volvulus
What are the extrinsic causes of a small bowel obstruction/ileus?
1. primary neoplasms
2. inflammation (e.g., CD, radiation enteritis)
3. infection (e.g., intestinal TB)
4. intussusception
5. trauma (intestinal wall hematoma)
What are the intrinisic causes of a small bowel obstruction/ileus?
1. bezoars (a tightly packed collection of partially digested or undigested material)
2. foreign bodies
3. gallstones
4. ascaris infestation
What are the intraluminal causes of a small bowel obstruction/ileus?
post-operative adhesions
What is the most common cause of small bowel obstruction in the developed world?
post-operative adhesions
What disorder:
-#1 cause of SBO in developed world
-develop due to a process involving the interaction among many cells, cytokines, and coagulation factors caused by damage to peritoneal surfaces (93-100% of pts undergoing trans-peritoneal surgery will develop post-op adhesions, and of these, 25% will develop SBO)
neoplasms
What is the second most common cause of small bowel obstruction?
neoplasms
What disorder:
-#2 most common cause of small bowel obstruction
-caused both by malignancies + benign conditions
Malignancies = adenocarcinomas, carcinoid tumors, lymphomas, and sarcomas
Benign = adenomas, leiomyomas, and lipomas
-gynecologic cancers, esp. ovarian cancer, are a very common cause
-metastatic disease can also cause SBO (including breast, skin, and testicular cancers)
hernias
What is the third most common cause of small bowel obstruction?
hernias
What disorder:
-#3 most common cause of small bowel obstruction
-can be internal or external
External involve the abdominal wall (e.g., inguinal, femoral, or incisional)
Internal typically involve mesenteric defects from prior surgery
-important to recognize due to higher incidence of strangulation which is a surgical emergency b/c blood supply is compromised
functional
What type/cause of SBO involves:
-metabolic disease (esp. hypokalemia and hypocalcemia)
-medications (E.g., narcotics, anti-cholinergics, CCBs)
-infection (retroperitoneal, pelvic, intrathoracic)
-abdominal trauma
-laparotomy
-most often occurs in pts who have undergone abdominal surgery, transient in nature
-some degree of this type of obstruction is considered normal after surgery (post-op ileus)
small bowel obstruction
What disorder's pathophysiology:
-due to interruption of normal flow through the intestinal lumen triggering a cascade of physiologic changes:
1. bowel proximal to obstruction first becomes mildly dilated by the accumulation of partially digested food and normal intestinal secretions (succus entericus -- secreted by cells lining intestinal wall in response to mechanical stimulation)
2. increased intestinal dilation causes an increase in peristalsis throughout the intestines, which can trigger frequent and loose bowel movements early in progression of the obstruction + n/v
3. as process continues, bowel wall becomes edematous and the normal absorptive function of intestinal wall decreases, leading to further accumulation of contents in the intestinal lumen proximal to obstruction
4. with the loss of normal intestinal motility, bacterial overgrowth begins to occur in proximal bowel (E. Coli, Strep Faecalis, Klebsiella)
5. As obstruction continues, transudative fluid loss occurs in peritoneal cavity, leading to worsening hypovolemia and dehydration
6. if obstruction is proximal in location, continued bouts of emesis can lead to electrolyte abnormalities, metabolic alkalosis, and severe hypo
small bowel obstruction
What Disorder:
-S/Sx = crampy abdominal pain, abdominal distention, n/v/d or constipation or inability to pass gas
-PE = ABCs first! evaluate hemodynamics, degree of distress, etc., fully expose the abdomen to observe abdominal distention, surgical sears and hernias (including genitals), hyperactive bowel sounds w/ rushes and high pitched tinkles on auscultation (hypoactive sounds late), possibly tympani on percussion, diffuse tenderness w/ palpation, peritoneal signs if late/complicated or strangulated, rebound tenderness, guarding, rigidity, and/or distention, fecal blood or impaction on digital rectal exam
-Labs = CBC, CMP to assess level of dehydration/metabolic disruption/infection (elevated lactate a late and ominous finding)
-Imaging = acute abdominal series --> CXR, supine and upright abdominal views, CT abdomen/pelvis w/ IV and oral contrast is 96% specific and helps to rule out most other acute abdominal diagnoses
small bowel obstruction
ID

small bowel obstruction
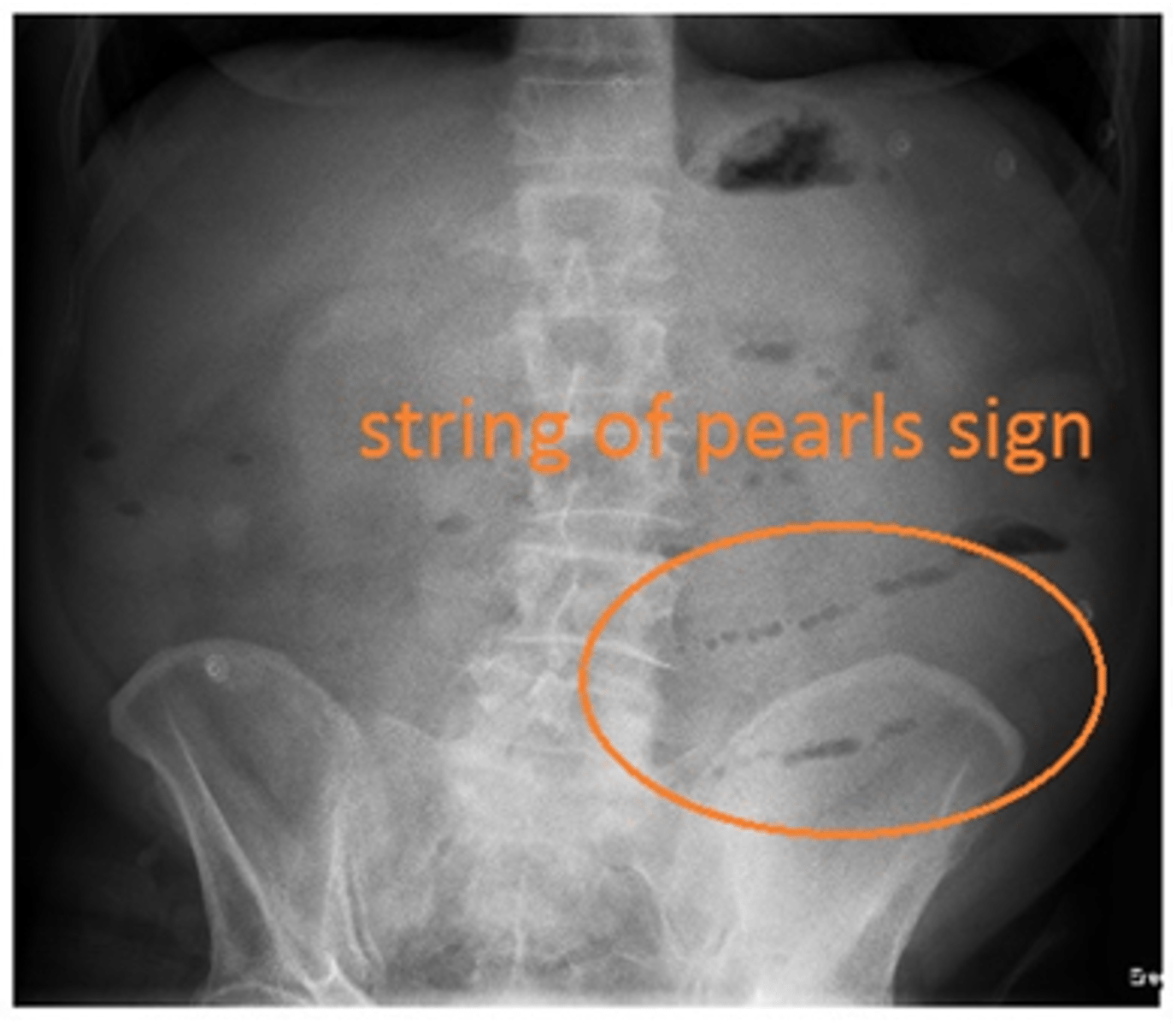
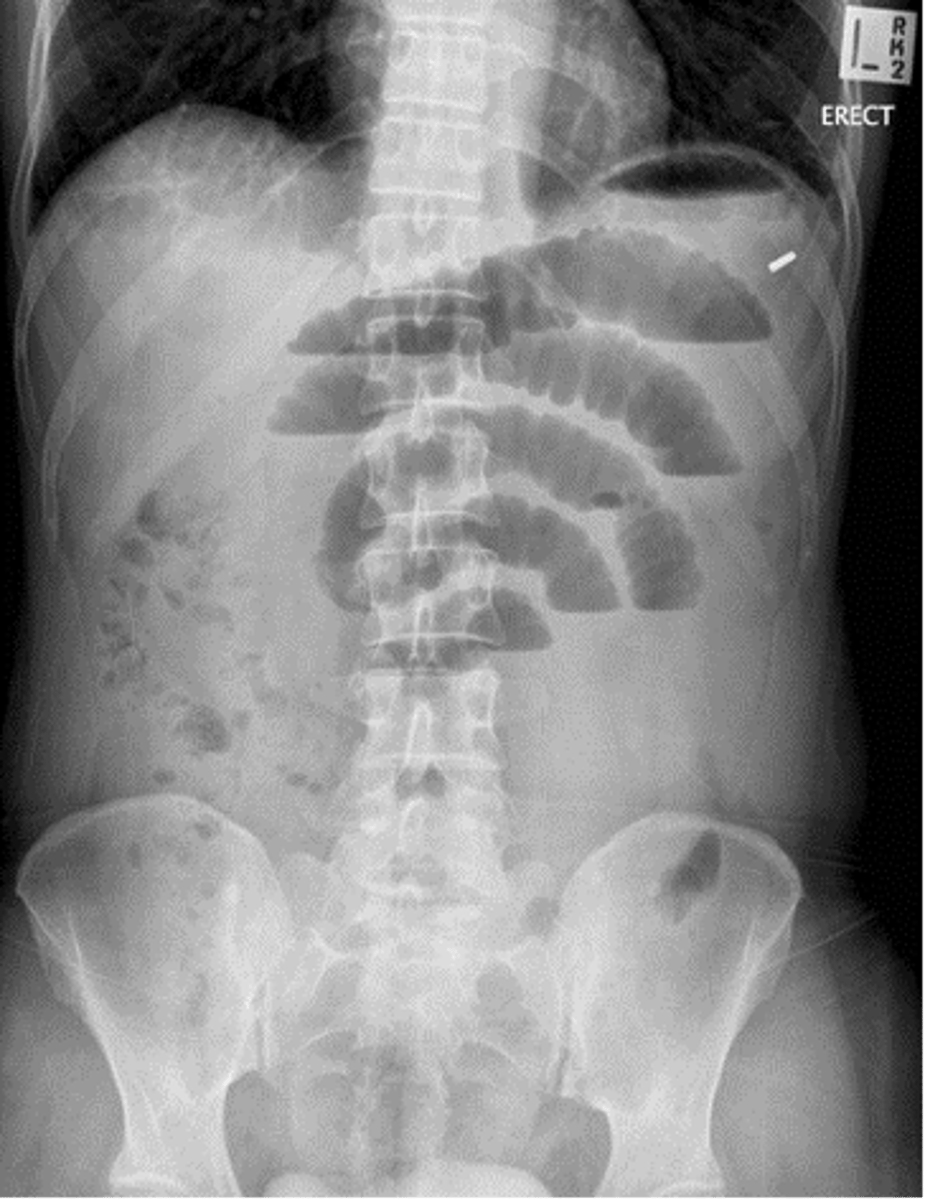
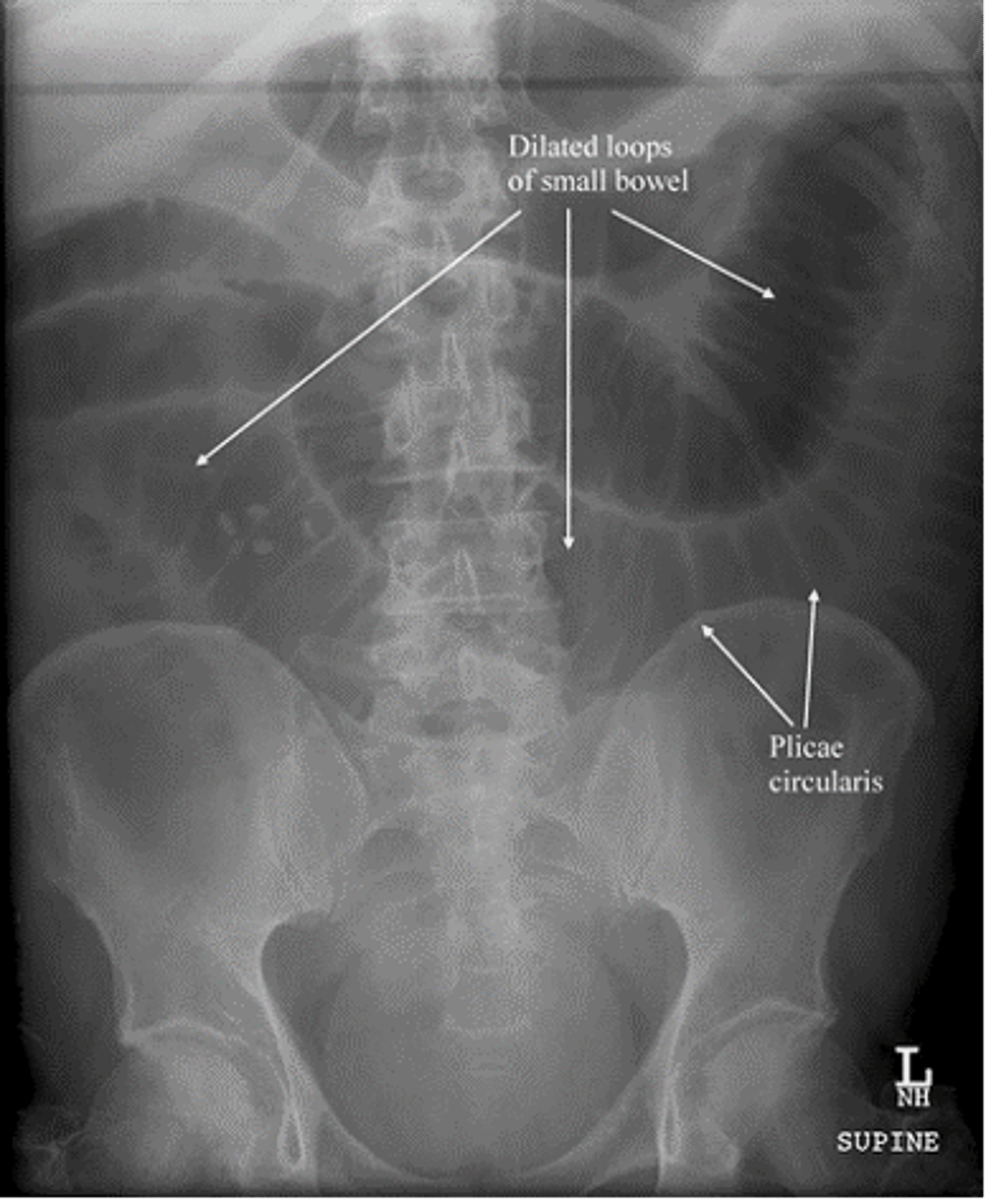
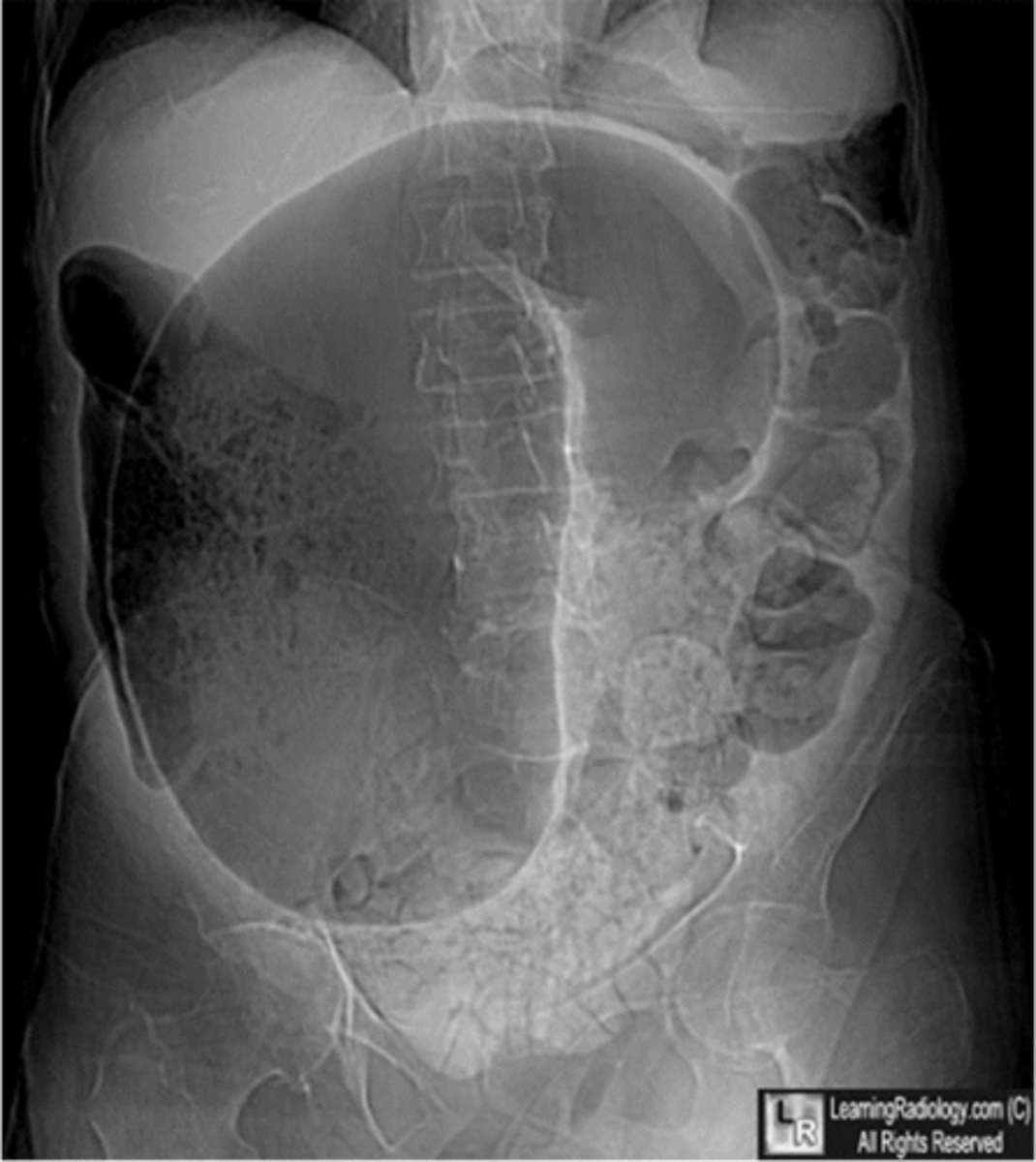
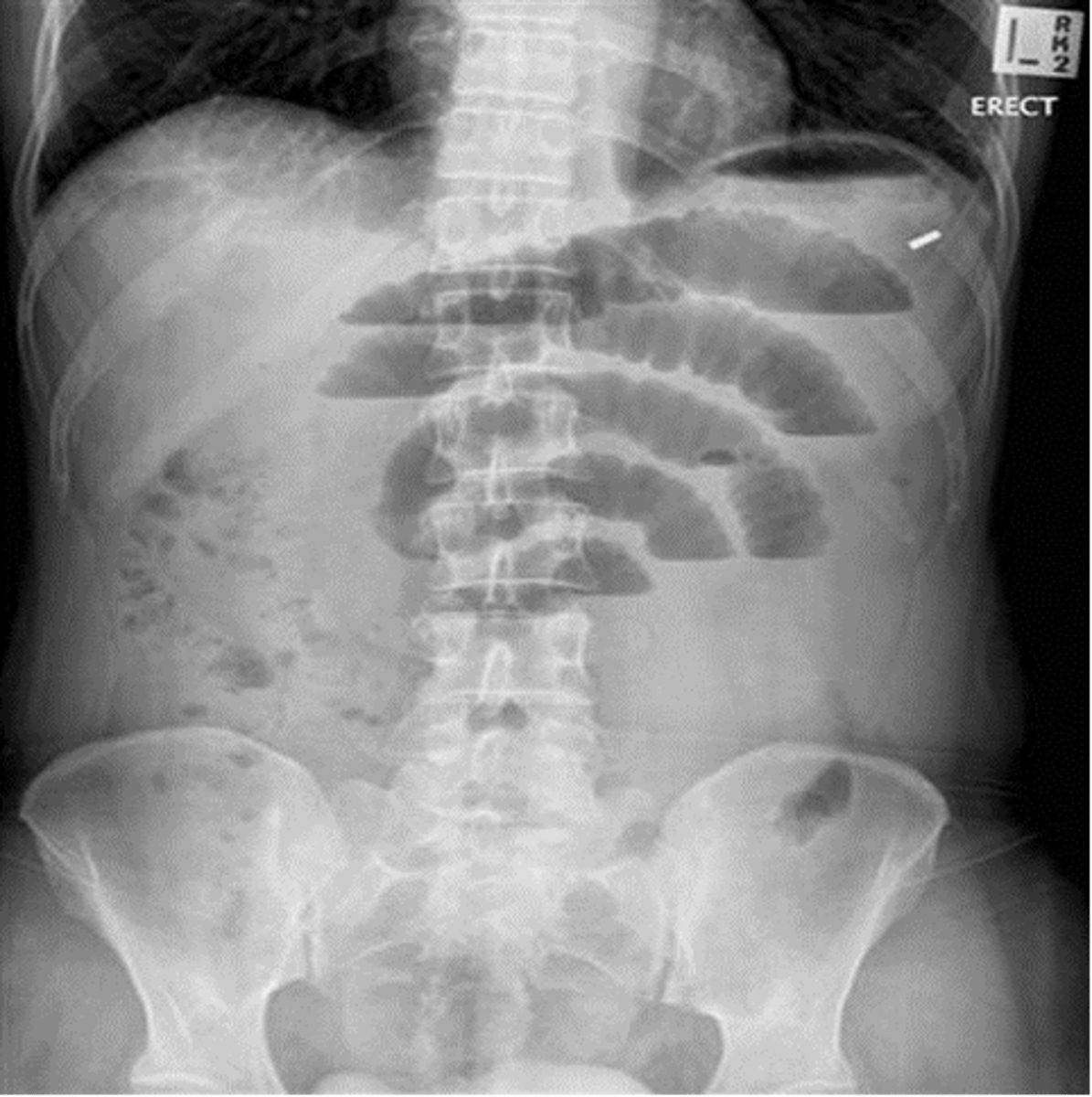
What disorder on XRAY:
-typically see distended loops of bowel, normally >3 cm in diameter, air fluid levels, and "string of pearls/beads" sign from trapped gas between intraluminal fluid
-the valvulae conniventes (plica circulares) cross the entire lumen of the small intestine
-greater # of distended loops, more distal the obstruction
small bowel obstruction (string of pearls sign)
ID
small bowel obstruction
ID
small bowel obstruction
ID
small bowel obstruction
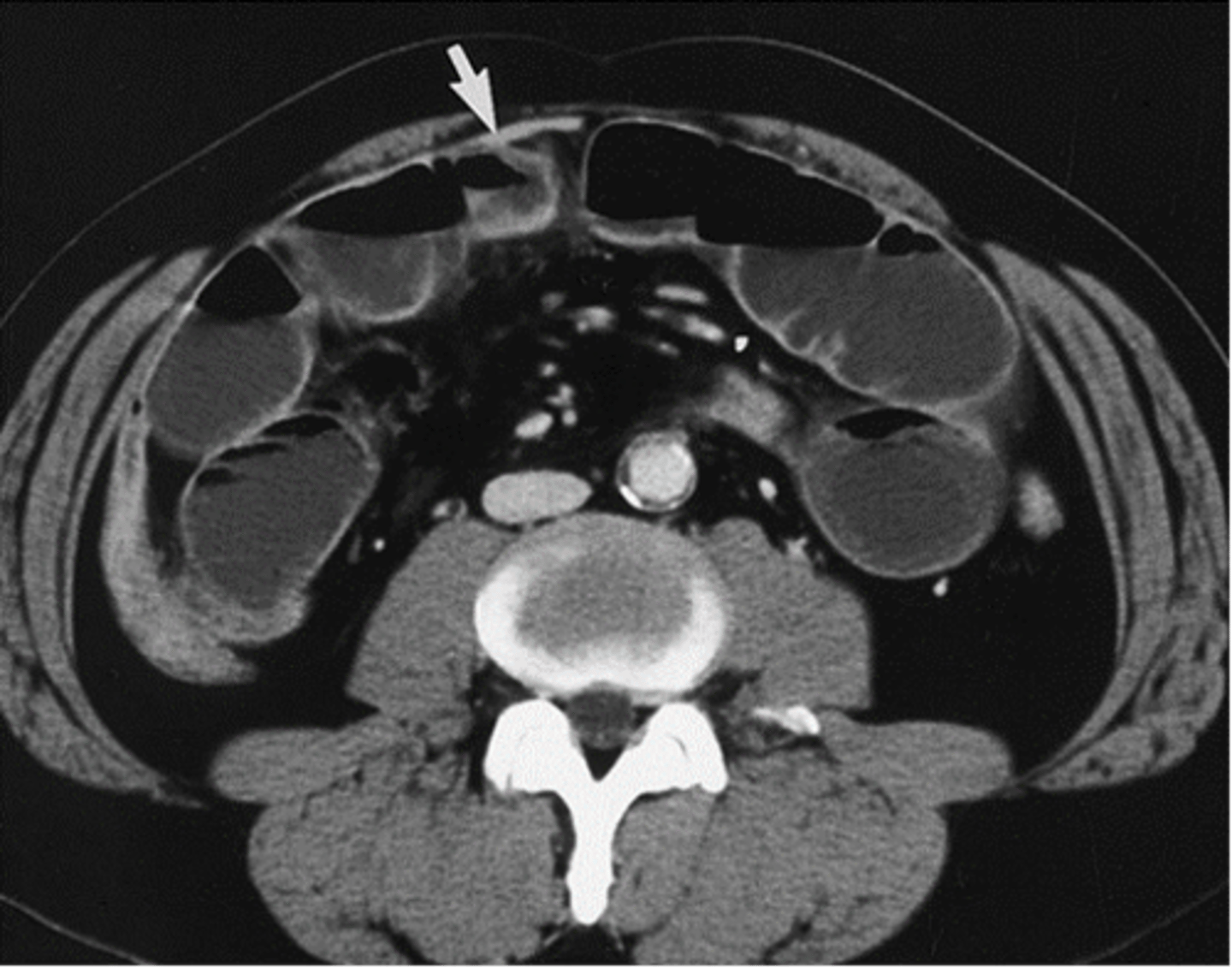
What disorder on CT:
-typically see distended loops of bowel, normally >3 cm diameter, air-fluid levels, "string of pearls/beads" sign, trapped gas between intraluminal fluid, transition point of strangulation
small bowel obstruction
ID
small bowel obstruction
ID
small bowel obstruction
Treatment for __________ involves:
-aggressive fluid resuscitation (IV NS)
-control n/v/pain
-reduce hernias (if possible)
-bowel decompression w/ NG tubes (delay if the pts n/v can be controlled w/ medication)
-timely surgical consultation of lysis of adhesions, surgical bowel resection, and bowel rest
1. hypovolemia
2. oliguria
3. renal failure
4. peritonitis
5. sepsis
6. surgical complications = hemorrhage, wound infection, abscess formation, short bowel syndrome
What are some complications of SBO?
reducible
What type of hernia:
-reducible w/ manual pressure
incarcerated
What type of hernia:
-non-reducible
-still has good blood supply but if it remains, it will worsen
strangulated
What type of hernia:
-surgical emergency
-blood supply to tissue/bowel compromised/cut off
colorectal carcinoma or malignancies
What is the most common cause of a large bowel obstruction?
diverticular disease
What is the second most common cause of a large bowel obstruction?
large bowel obstruction
What disorder:
-#1 cause = colorectal carcinoma or malignancy
-#2 cause = diverticular disease
-5% are due to sigmoid/cecal volvulus, many of rest are hernias
-prevalence of mechanical type increase w/ age as does its main causes (colorectal cancer + diverticulitis)
-Pathophysiology (similar to SBO):
1. mechanical obstruction or twisting (volvulus) causes dilation above obstruction --> mucosal edema and impaired venous + arterial blood flow to bowel
2. bowel edema + ischemia increases mucosal permeability of the bowel --> bacterial translocation, systemic toxicity, dehydration, and electrolyte abnormalities
3. bowel ischemia can lead to perforation and fecal soilage of peritoneal cavity
-sepsis + death common
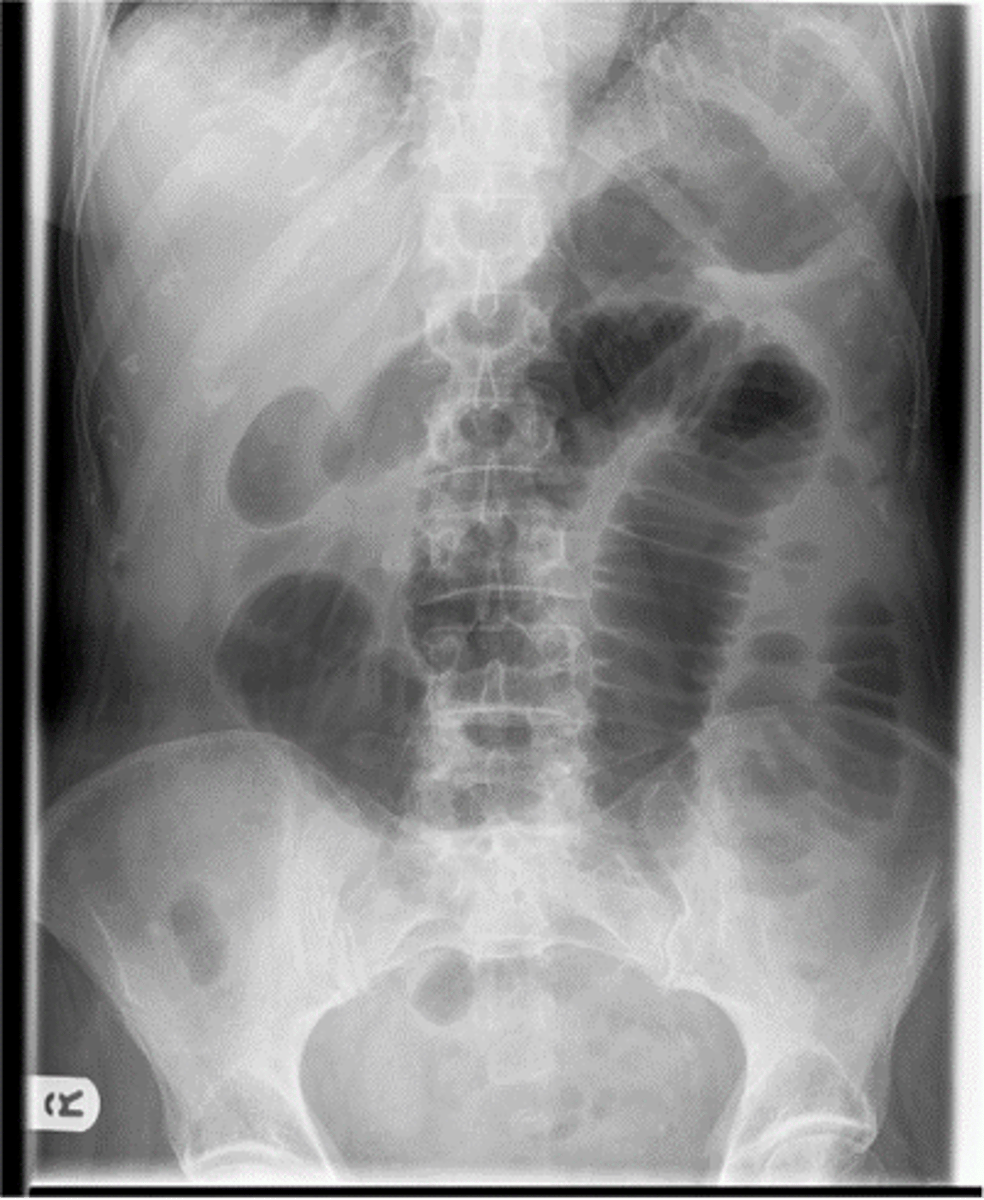
large bowel obstruction
ID
large bowel obstruction
ID

large bowel obstruction
What disorder on imaging:
-look for extremely dilated loops of bowel, typically following periphery
-haustra typically do not connect across diameter of bowel and spaced far apart
diverticula
What disorder:
-presence of diverticula in the colon (mostly asymptomatic)
-can become inflammed --> usually painful
-Sx believed to develop when diverticula become obstructed, presumable w/ inpissated stool --> inflammation sets in and micro-perforations of sac develop
uncomplicated
(uncomplicated/complicated) diverticulitis:
-only peri colonic fat is inflamed
-w/ time, a phlegmon, abscess, or gross perforation may develop
complicated
(uncomplicated/complicated) diverticulitis:
-extension of disease beyond peri colonic fat
-involved colonic segment may fistulize to any adjacent organ, most commonly the bladdy
-adjacent bowel may become obstructed by mass effect from abscess or may incur an inflammatory ileus
-recurrent episodes of diverticulitis can lead to strictures in the colon w/ subsequent obstruction
volvulus
What disorder:
-can be cecal or sigmoid
-twisting of the bowel that may compromise the vascular supply to a loop of the colon
-more common in older adults (60-70)
left
In regard to LBO, treatment of colon cancer involving the (left/right) colon involves:
-surgical Tx = resection w/o primary anastomosis or resection w/ primary anastomosis + intra-operative lavage (NOT EMERGENT)
-endoscopically placed expandable metal stents can be used to relieve the LBO, thus allowing for a primary colorectal anastomosis
right
In regard to LBO, treatment of colon cancer involving the (left/right) colon involves:
-palliative colorectal stents option for pts who are poor surgical candidates or have advanced cancer
-R obstructions treated w/ right colectomy and a primary anastomosis between ileum and transverse colon OR colostomy + hartmann's procedure
diverticulitis
Treatment of __________ causing a LBO involves:
-similar to SBO: IV fluids, Abx, and n/v/pain control/bowel rest
-pts w/ persistent obstruction despite appropriate medical management go to surgery --> resection follows same principles as treatment of carcinomas
-elective colonic resection is offered to pts w/ recurrent disease
sigmoid
Treatment of (sigmoid/cecal) volvulus causing LBO involves:
1st choice = sigmoidoscopy w/ volvulus reduction
2nd choice = sigmoid colectomy w/ hartmann's procedure
cecal
Treatment of (sigmoid/cecal) volvulus causing LBO involves:
1st choice = surgical cecostomy, often a cecopexy needs to be performed to prevent recurrence
2nd choice = colonoscopy due to high risk of colonic perforation
acute mesenteric ischemia
What disorder:
- caused by reduction of intestinal blood flow, commonly arising from occlusion, vasospasm, and/or hypoperfusion of mesenteric vasculature
-rare but life-threatening w/ high mortality --> REQUIRES EARLY DIAGNOSIS
->50 y/o, often w/ underlying CVD
4 Categories:
1. arterial embolus (most common)
2. arterial thrombosis
3. non-occlusive (arterial) mesenteric ischemia (intestinal angina)
4. mesenteric venous thrombosis
-mortality rates climb to 70% once infarct has occurred
MANY causes = virchow's triad, alterations in blood flow (e.g., stasis), vascular endothelial injury, alterations in constituents of blood, inherited hypercoagulable disorders, factor V leiden mutation, prothrombin gene mutation, Protein S/C deficiency, anti-thrombin deficiency, dysfribinogenemia, acquired hypercoagulability disorders, infection, hospitalization, recent surgery, AFib
acute mesenteric ischemia
What disorder:
-PAIN OUT OF PROPORTION TO PE!!!!!!!!!
4 types:
1. arterial embolus (most common) = 25% of CO goes to small and large bowel w/ 2/3 going to SMA and 1/3 IMA --> SMA most susceptible to embolism due to large caliber and narrow angle of origin to aorta in which the emboli lodge 3-10 cm distal to origin in tapered segment distal to take off of middle colic artery --> middle segment of jejunum most often ischemic b/c most distal from collateral circulation
2. arterial thrombosis = acute thrombosis w/ patients w/ chronic intestinal ischemia from progressive stenosis due to atherosclerotic plaque @ celiac or SMA origin
3. non-occlusive (arterial) mesenteric ischemia (intestinal angina) = splanchnic hypoperfusion and vasoconstriction (tends to occur in pts w/ atherosclerotic plaque), typical pt is older w/ CVD who sustained life-threatening event (e.g., CHF/MI) or treated w/ drugs that reduce perfusion (e.g., diuretics) or have other events (e.g., sepsis, aortic insufficiency (dissecting aneurysm), cardiac arrhythmias, or from medications (digoxin, alpha adrenergic agonist -- epi, norepi, dopamine)
4. mesenteric venous thrombosis = young pt, 70% hypercoagulable states
mesenteric arterial embolism
Which type of acute mesenteric ischemia is associated w/ the following factors:
-coronary artery disease: post-MI or CHF
-valvular disease: mitral valve disease, non-bacterial endocarditis
-dysrhythmias: chronic Afib
-aortic aneurysm and dissections
mesenteric arterial thrombosis
Which type of acute mesenteric ischemia is associated w/ the following factors:
-celiac and SMA usually involved, esp. in pts w/ chronic severe visceral atherosclerosis
-50% of these pts have a Hx of "abdominal angina" or abdominal pain after meals
-RFs = older age, diffuse atherosclerosis, HTN
non-occlusive mesenteric ischemia (intestinal angina)
Which type of acute mesenteric ischemia is associated w/ the following factors:
-CVD low flow states --> CHF, dysrhythmia, cardiogenic shock, post-cardiopulm bypass
-preceding hypotensive episode -- sepsi
-drug-induced splanchnic vasoconstriction --> digoxin, vasopressors, cocaine, methamphetamines
mesenteric venous thrombosis
Which type of acute mesenteric ischemia is associated w/ the following factors:
-hypercoagulable states = polycythemia, sickle cell, anti-thrombin III deficiency, protein C/S deficiency, malignancy, myeloproliferative disorders, estrogen therapy/OCP, prgenancy
-inflammatory conditions = pancreatitis, diverticulitis, appendicitis, cholangitis
-trauma = post-op, post-splenectomy
-Misc = CHF, renal failure, decompression sickness, portal HTN
Virchow's Triad = hypercoagulable, endothelial injury, stasis
acute mesenteric ischemia
What disorder presents as:
Traditional Historical Triad:
1. sudden onset of poorly localized abdominal pain
2. gastric emptying (v/d) in acute setting
3. pts w/ cardiac disease or arrhythmia (1/3 - 1/2 pts have Hx of embolic event like PE, DVT, or CVA)
PE: pain out of proportion to PE -- pt may be writhing in pain but have a soft abdomen w/o guarding
-as ischemia progresses, s/sx of acute abdomen/peritonitis set in --> heme (+) stools, rebound/guarding/rigidity, and hypotension/tachycardia/shock
Labs = can be normal, leukocytosis >15k in 75%, anion gapped metabolic acidosis, elevated serum lactate (90% sensitive)
acute mesenteric ischemia
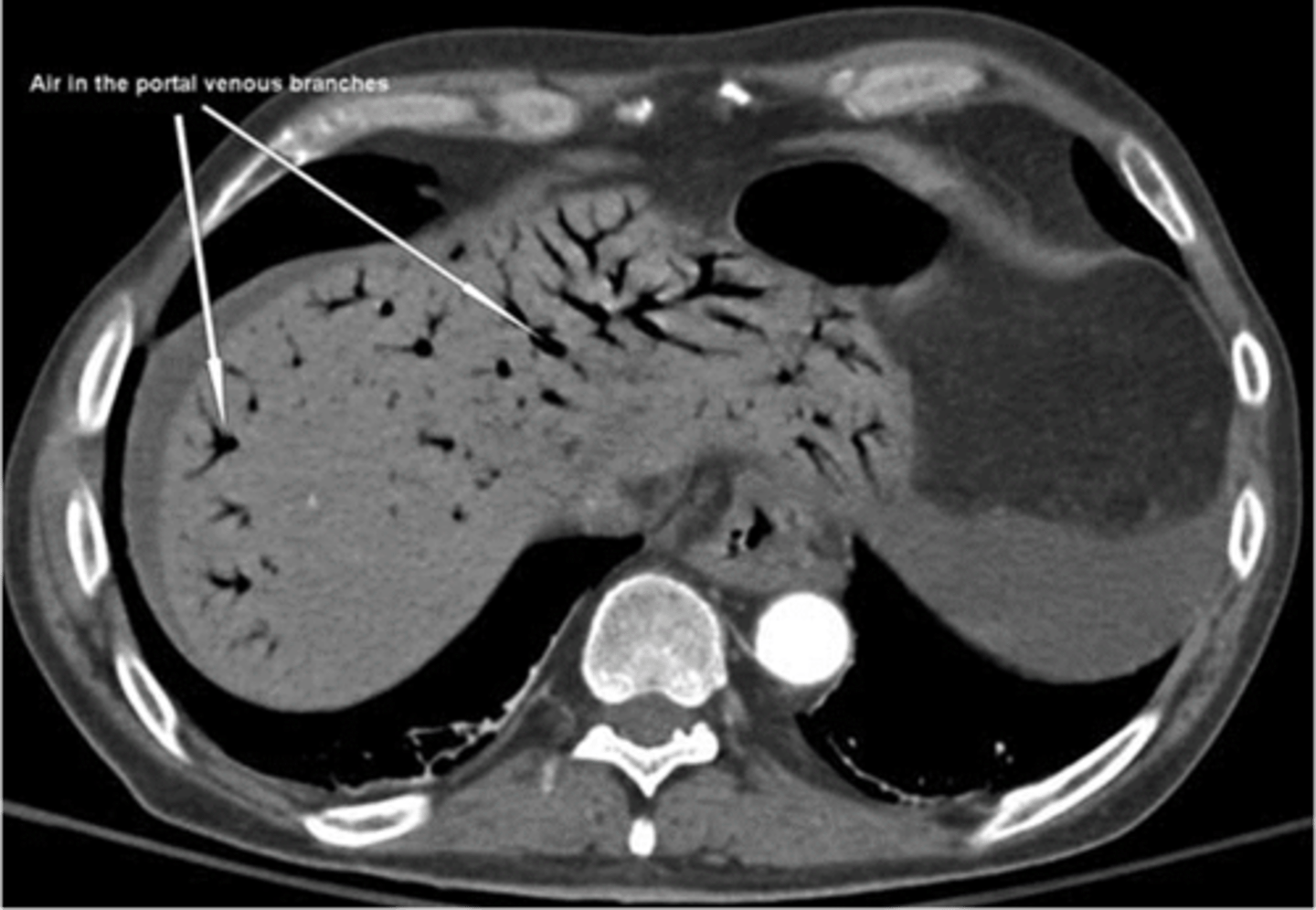
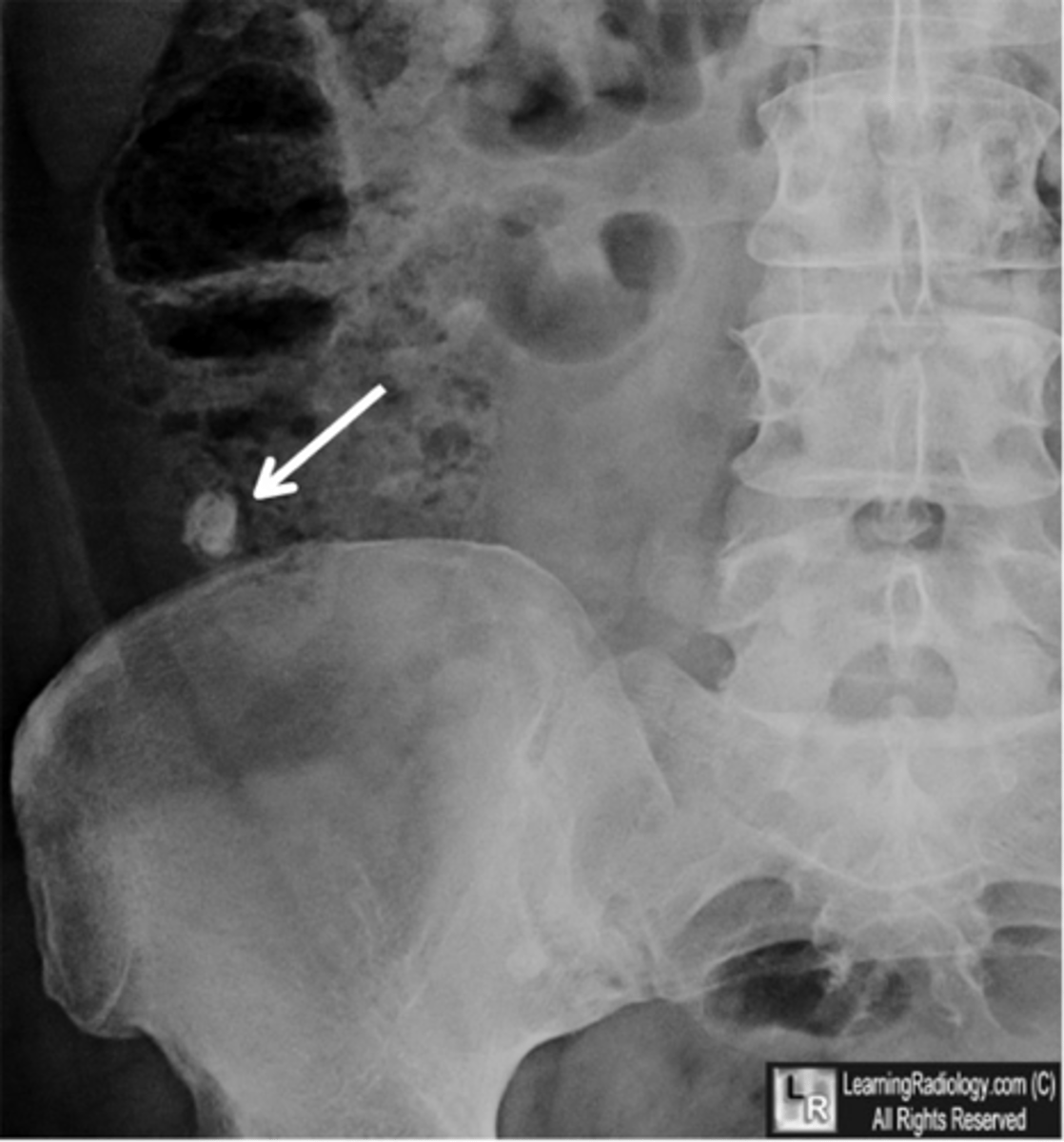
What disorder has imaging that involves:
XRAYs = "thumb printing" --> edema in bowel wall, as the disease progresses to transmural, often creates an adynamic ileus, distended loops of small bowel w/ air-fluid levels, and advanced cases may have pneumatosis intestinalis (air in bowel wall -- very ominous)
CTA Abd/pelvis w/ IV contrast: arterial or venous thrombosis, intramural gas (pneumatosis interstinalis), portal venous gas, focal lack of bowel-wall enhancement (infarcted tissue) --> normal/negative doesn't rule out --> go-to choice for rapid diagnosis in modern ED
GOLD STANDARD = Mesenteric Angiography --> can diagnose and possibly treat @ same time
mesenteric angiography
What is the gold standard for diagnosis of acute mesenteric ischemia?
CTA abdomen/pelvis
What is the go-to choice for rapid diagnosis of mesenteric angiography in a modern ED?
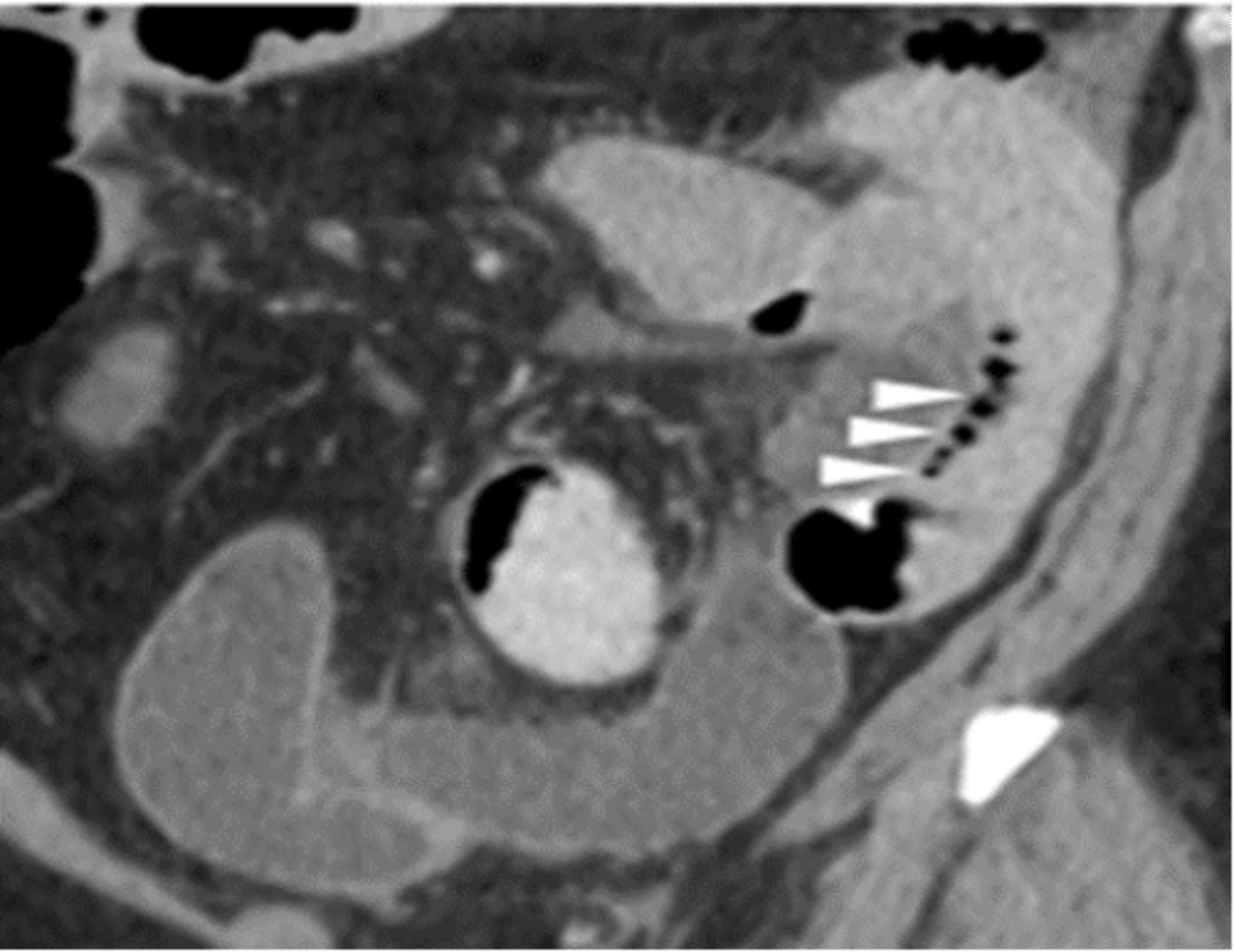
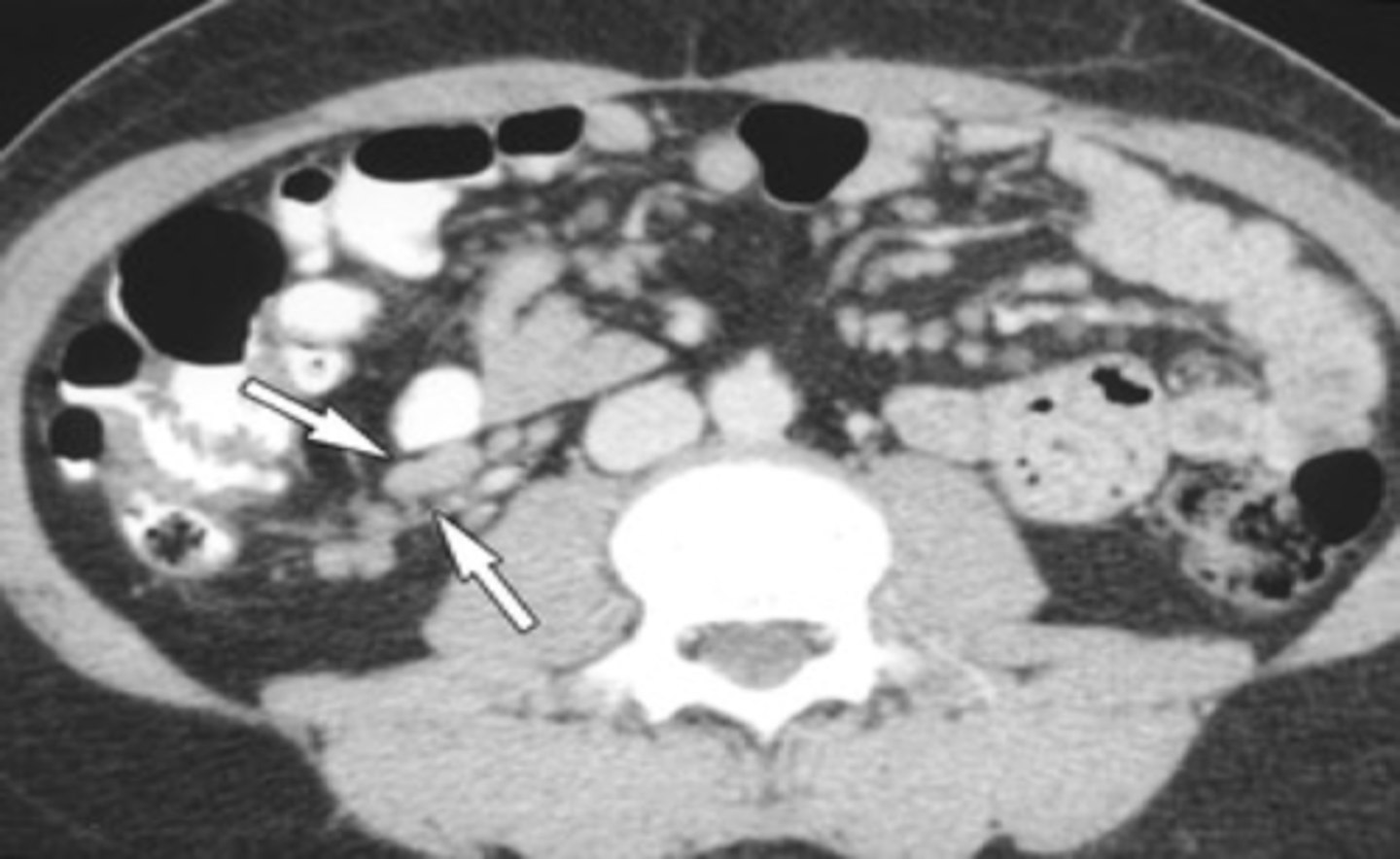
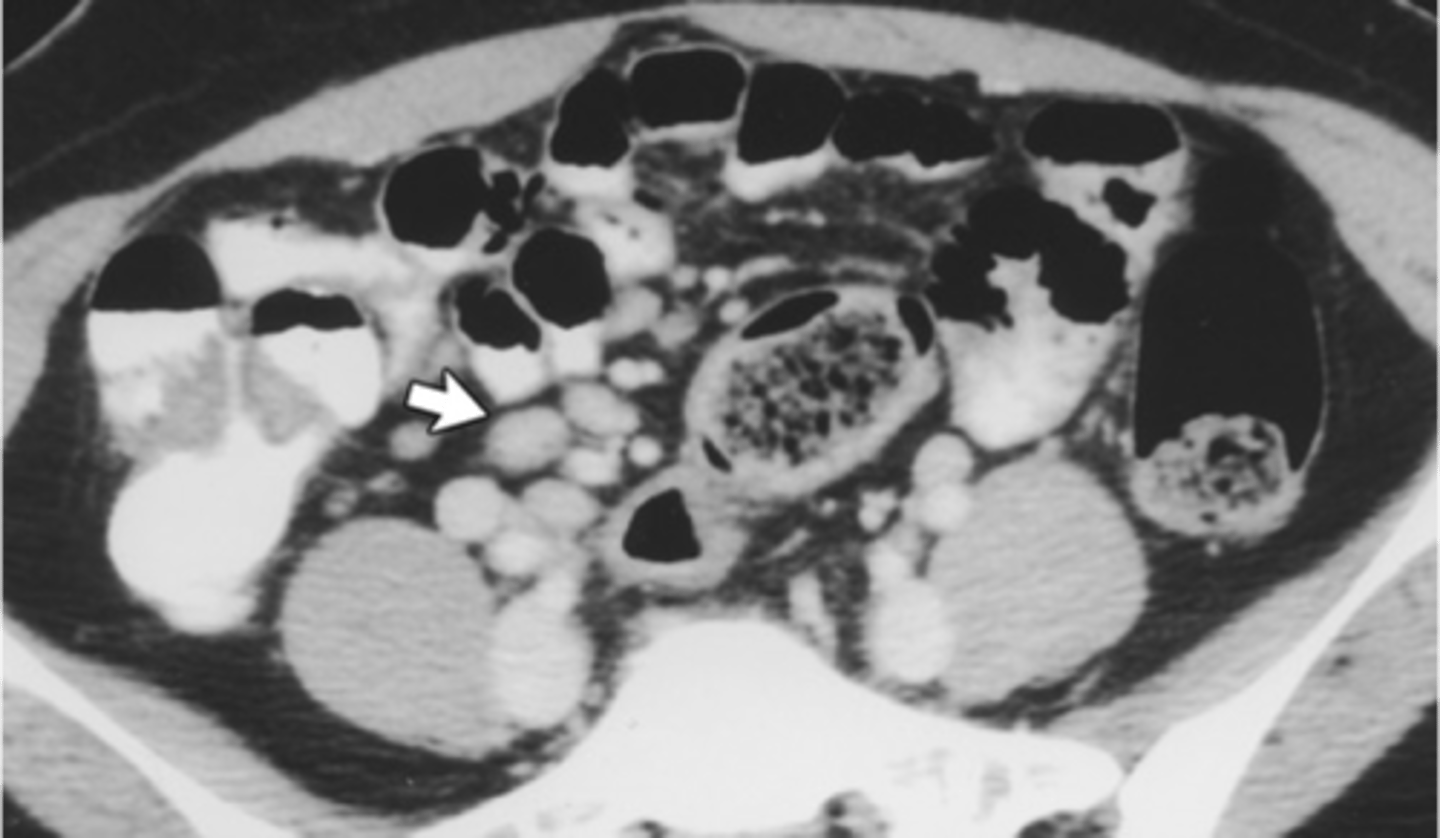
acute mesenteric ischemia (celiac artery cut off/occluded)
ID

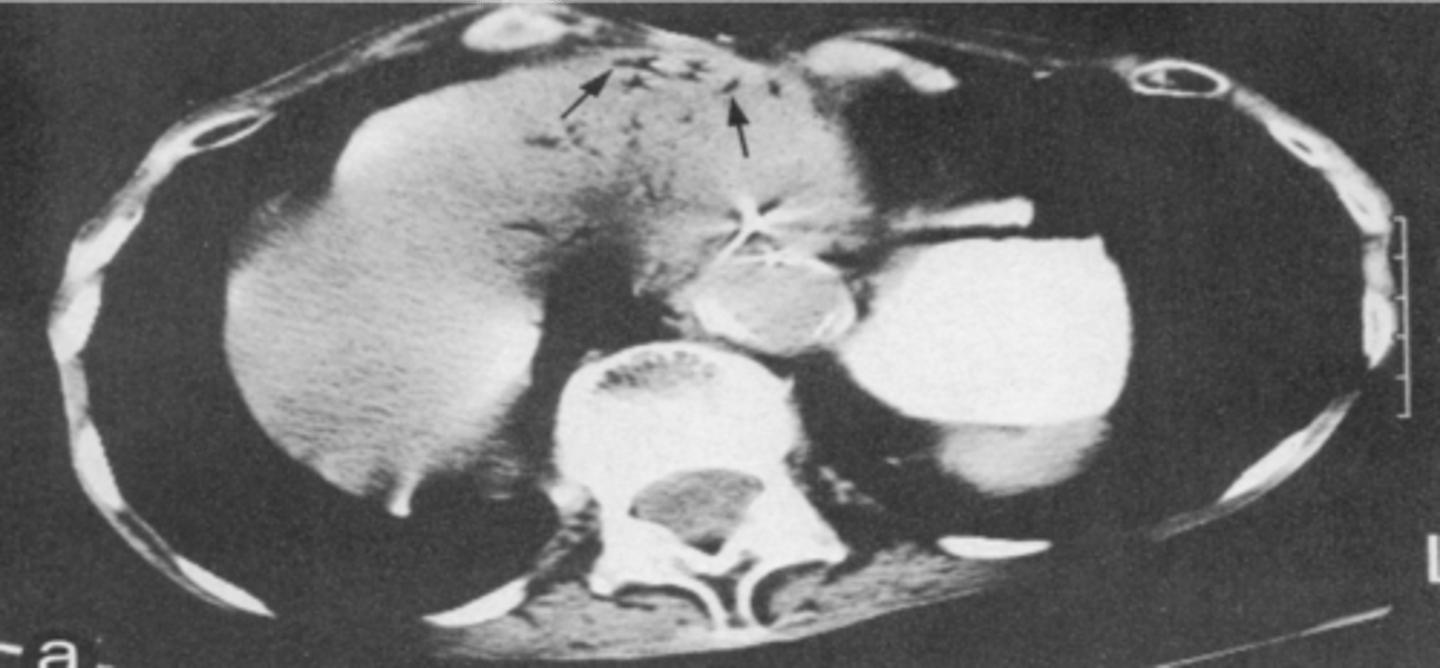
acute mesenteric ischemia (air in hepatic and portal system)
ID
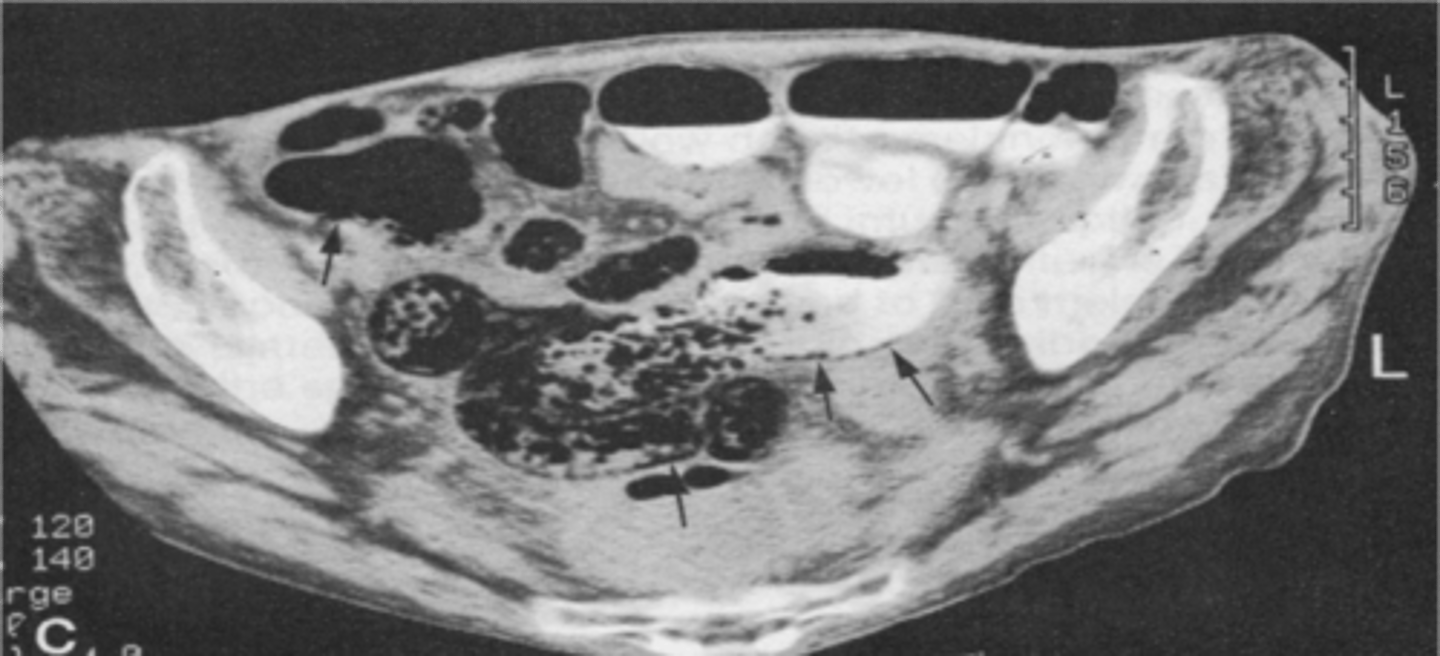
acute mesenteric ischemia (pneumatosis intestinalis)
ID
acute mesenteric ischemia
Treatment of __________ involves:
Aggressive hemodynamic support and restore intestinal blood flow ASAP with anti-coagulation/interventional angiography/surgery!!
• Restore intestinal blood flow ASAP
• Aggressive hemodynamic monitoring
• IV fluid support
• Correction of metabolic acidosis
• Broad spectrum antibiotics
• NG tube for gastric decompression
• Avoid vasoconstrictors (Levophed)
• Systemic anticoagulation with Heparin or LMWH unless patient activity bleeding
• Surgery - No delay if intestinal infarction or perforation
• Arteriography – intra-arterial vasodilators (papaverine), thrombolytics, angioplasty, stents, embolectomy
The patient has rebound tenderness
A 60-year-old woman presents with diffuse colicky abdominal pain, nausea and vomiting. The patient's past medical history is significant for hypertension and perforated appendicitis at age 25 that was managed surgically. Her physical exam reveals hyperactive bowel sounds, diffuse abdominal tenderness and distention. An abdominal x-ray is shown below. Which of the following additional features would result in the patient being managed surgically?
a. The patient has not passed gas
b. The patient has a reducible ventral hernia
c. The patient is volume depleted
d. The patient has rebound tenderness
e. The patient is a diabetic
Previous abdominal surgeries
A 47-year-old gentleman presents to the emergency department with a 3-4-day history of cramping abdominal pain, nausea, and vomiting. Physical examination reveals a normal cardiovascular assessment, but his abdomen is found to be distended, tender to palpation, and with high-pitched bowel sounds. An abdominal radiograph is shown in Figure A. Upon further questioning, what is most likely to be found in this patient's past history?
a. Psychological derangements
b. Gastroesophageal reflux disease
c. Irritable bowel syndrome
d. Previous abdominal surgeries
e. Intermittent appendicitis
Mesenteric ischemia
A 60-year-old male is brought to the ED by EMS complaining of severe abdominal pain that began suddenly 6 hours ago. His BP is 145/75, HR is 105 and irregular. On examination, your note mild abdominal distention and diffuse tenderness without guarding. Stool is heme+, lab results reveal WBC 12,500, Hct 48, lactate 4.2. ECG shows atrial fibrillation, rate 110. A CT scan is show below. Which of the following is the most likely dx?
a. AAA
b. Crohn's disease
c. Diverticulitis
d. Mesenteric ischemia
e. SBO
appendicitis
What disorder:
-peak incidence between 10-30 y/o
-most common general surgical emergency
Pathophysiology: obstruction of the lumen from 1) inpissated stool (fecalith or appendicolith), 2) lymphoid hyperplasia --> obstruction leads to bacterial overgrowth + continued secretion of mucus --> distention --> increased pressure + vascular compromise + necrosis --> increased pressure stops venous inflow, causes increased pressure + ultimately overcomes arterial circulation --> late you get necrosis + local inflammation --> irritation of peritoneum in RLQ
S/Sx: early distention causes visceral pain manifesting as peri-umbilical pain followed by loss of appetite + nausea (Sometimes 1-2 ep of vomiting) --> pain migrates to RLQ --> fever, tachycardia, leukocytosis
Labs: elevated WBC (>20k -- suspect perforation and abscess or other etiology)
Imaging: appendicolith on CXR (but don't order a CXR), US good but requires expertise, better for peds, MRI very good but time consuming, often used for pregnant women to avoid radiation to fetus, CT scan gold standard
Tx: surgery (open + laparoscopic appendectomy) or non-operative
appendicolith
ID
dunphy's sign
Which Physical Exam finding potentially indicating appendicitis:
-coughing exacerbates RLQ pain
rovsing's sign
Which Physical Exam finding potentially indicating appendicitis:
-pain in RLQ during palpation of LLQ
obturator sign
Which Physical Exam finding potentially indicating appendicitis:
-pain w/ internal rotation of hip
psoas sign
Which Physical Exam finding potentially indicating appendicitis:
-heel tap/walking posture/psoas m. stretch during extension of leg --> pain
mcburney's point
Which Physical Exam finding potentially indicating appendicitis:
-point located 1/3 of distance along a line drawn from ASIS to umbilicus
examine their tonsils and perform a rectal examination
What two physical exam procedures should you ALWAYS do when assessing possible appendicitis?
CT
What is the gold standard diagnostic tool for appenicitis?
in pts w/ prohibitive operative/anesthesia risk
When can you do non-operative treatment for appendicitis?
medical emergency
What type of emergency is a ruptured appendicitis?
1. admission, fluids, foley, Abx
2. drain abscess in OR or usually interventional radiologist can drain via CT guidance
3. may need interval appendectomy at later date
What is the treatment for ruptured appendicitis?
mesenteric lymphadenitis
What disorder:
-one of most common causes of acute abdominal pain in young adults + children
-lymph nodes involved drain the ileocecal region
-nodes are enlarged, discrete, soft + pink
-Histo: pattern of reactive hyperplasia
-S/Sx = recent illness (sore throat, URTI), first symptom usually pain located in RLQ but less focal and more diffuse than appendicitis, n/v in 1/3 of pts, enlarged lymphadenopathy elsewhere (20%), low grade fever and elevated WBCs common
-No specific Tx required
mesenteric lymphadenitis
ID
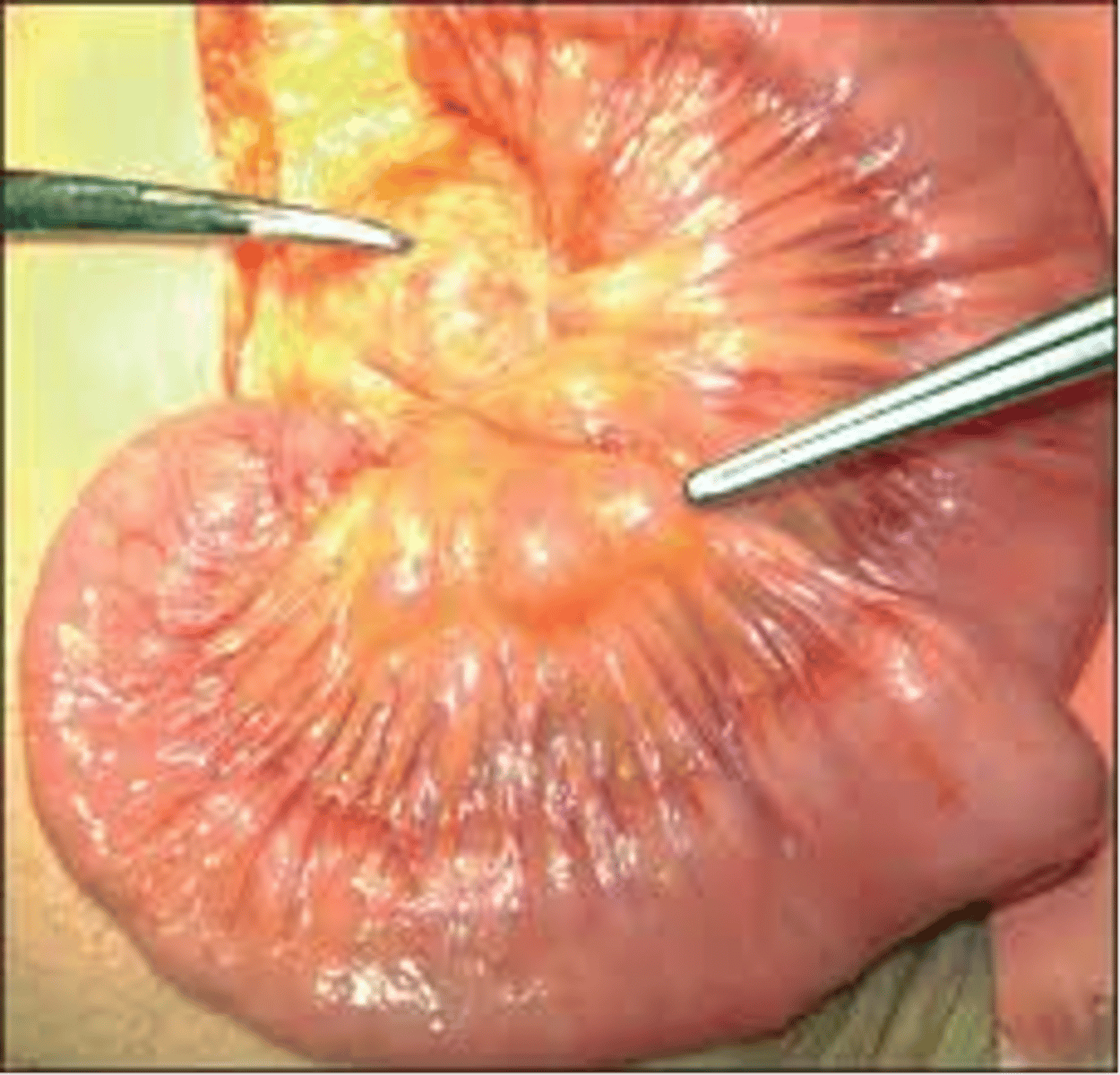
mesenteric lymphadenitis
ID
mesenteric lymphadenitis
ID
meckel's diverticulum
What disorder:
-most common true diverticulum of GI tract
-congenital diverticulum that results from incomplete closure of omphalo-mesenteric duct (vitelline duct)
-located near terminal ileum
-often contain heterotropic gastric (50%) or pancreatic tissue
-most remain asymptomatic and undetected
-can be incidentally discovered at laparotomy or laparoscopy
-no indication to remove an asymptomatic one
meckel's diverticulum
What disorder:
-Imaging: technetium-99m (99mTc) pertechnetate scan. This scan detects gastric mucosa. Would appear as a spot on the scan distant from stomach
-Rule of 2s:
•2% of the population
•2 ft from terminal ileum
•2% become symptomatic
•2 years old is the most common age of clinical presentation
•2 in in length
•2 types of ectopic tissue (Gastric/Pancreatic)
-S/Sx in children: bleeding (most common)
-S/Sx in adults: obstruction (most common) -- bowel volvulus around adhesive band from tip of diverticulum to umbilicus, abdominal wall, or mesentery
-Other S/Sx: mimic appendicitis, pain, fever, anorexia, elevated WBCs
-CT scan may help differentiate from appendicitis
-can be present as an indirect hernia (typically on R) --> "hernia of Littre"
-Tx: surgical removal (laparotomy or laparoscopy) + may need to remove segment of bowel connected (In adults with bleeding related to Meckel’s there is often an ulcer in the small bowel that is the source of blood loss)
dysentery
What describes blood and pus in the feces and often presents w/ pain, fever, and cramps?
enterocolitis
What is inflammation of the mucosa of the small and large intestine?
gastroenteritis
What is a syndrome w/ GI Sx including n/v/d and abdominal pain?
diarrhea
What describes >3-5 loose bowel movements per day and can be further classified into acute/chronic and non-inflammatory/inflammatory?
small
Infections of the (small/large) intestine will cause the following changes to stool:
-large volume, watery diarrhea
-no blood or WBC in stool
-cramps, bloating, gas, weight loss
large
Infections of the (small/large) intestine will cause the following changes to stool:
-frequent, regular, small volume, often painful bowel movements
-bloody or mucoid stools
food-associated infection
What disorder:
-consumption of contaminated food
-food is vehicle for pathogen
food poisoning
What disorder:
-consumption of food containing toxins (chemical or bacterial)
toxins
What pathological mechanism utilized by infectious pathogens to cause a food-associated infection:
-produced by S. aureus, B. cereus, C. botulinum
-Sx in 1-6 hrs
toxin production after ingestion
What pathological mechanism utilized by infectious pathogens to cause a food-associated infection:
-produced by Vibrio, Shigella, STEC
-Sx in ~24h after exposure
invasion of intestinal epithelium
What pathological mechanism utilized by infectious pathogens to cause a food-associated infection:
-produced by Viruses, Salmonella, EIEC, Campylobacter
-Sx last 1 day to weeks
food poisoning
clinical features of _____________ include:
-suspect when >2 people develop Sx at/near same onset time
-most common Sx = n/v/d, abdominal cramps
-Systemic Sx = fever, dehydration, malaise
-Hx = food, travel, childcare/long-term care facility, job, personal hygiene, PMHx
true
T/F: diagnosis of food poisoning is not required for testing b/c illness is usually self-limited (not necessary for uncomplicated, watery diarrhea)
true
T/F: you may need diagnostic testing in pts w/ systemic illness, prolonged Sx, or serious comorbid conditions w/ food poisoning
bacillus cereus
What pathogen:
-G(+), aerobic/facultatively anaerobic, motile, spore-forming rod
-Catalase (+), b-hemolytic
-2 types of toxin-mediated illness = diarrheal syndrome + emetic syndrome which both cause disease within 24h of ingestion
Virulence Factors:
1. diarrheal toxins -- heat labile, syndrome caused by ingested vegetative cells
2. emetic toxin (cereulide) -- heat stable, fried rice syndrome
S. aureus
What pathogen:
-produces MANY different enterotoxins
-food is contaminated by human carriers
Pathogenesis: act as superantigen, all are heat stable
-causes severe vomiting within 3-6 hrs, usually recover within 24 hours and NO DIARRHEA
clostridium perfringens
What pathogen:
-G(+) rod, anaerobic, spore forming
-ubiquitous, very short generation time
-causes extremely accelerated decomposition
-common cause of foodborne illness, spores survive cooking and germinate in improperly stored foods (meats, poultry, gravy) and is toxin-mediated from a heat labile toxin from type A stains
Presentation:
-incubation period of 6-24 hrs (usually 10-12)
-watery diarrhea, cramping w/ resolution of Sx in 24-48 hrs
-less common = enteritis necroticans (pigbel) --> abdominal distention, pain, dilated thickened loops of bowel w/ segmental necrosis usually in resource-limited countries associated w/ pork consumption caused by type C strains
Toxin Pathophysiology: GI Sx caused by enterotoxin (CPE), a pore forming toxin that binds to claudins; pore leads to Ca2+ influx → ↑ Ca2+ → calpain activation → caspase-3 mediated apoptosis
Histo: severe villous shortening w/ epithelial necrosis and desquamation
E. coli
What pathogen:
-G(-), facultative anaerobic, coliform rod
-readily cultured from stools in aerobic conditions
-ferments lactose, indole (+)
-very versatile and diverse, some strains are pathogenic while others are normal flora and virulence factors are encoded on accessory genetic elements
-Strains/Serotypes: O/K/H antigens
enterotoxigenic E. coli (ETEC)
What type of E. coli:
-WATERY diarrhea in children in developing nations, also seen in travelers exposed to contaminated food + water
Pathogenesis requires intestinal colonization and virulence factors:
1. colonization = fimbrial adhesions
2. secretory toxins encoded on plasmids = LT (heat labile, stimulates AC) and STa (heat stable, stimulates GC)
enteroaggregative E. Coli (EAEC)
What type of E. coli:
-emerging enteric pathogen, first found in children in poor resource countries, chronic infections in immunocompromised pts, and 2nd most common cause of traveler's diarrhea
-defined by "stacked brick" pattern of adhesion to Hep-2 cells via plasma-associated fimbriae
Pathogenesis:
-aggregation + adherence of bacteria to intestinal mucosa
-enterotoxins and cytotoxins damage host cells
-inflammation causes diarrhea