Bacteria and biofilms
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
34 Terms
How many microorganisms are in one gram of plaque?
4 × 10^10 microorganism
How many organisms are in 1 ml of saliva
10^8 organisms/ml
What are some oral habitats?
Lips, cheeks, palate
shedding surface
Keratinised
Tongue
highly papillated
Reservoir
Teeth
number of surfaces
Gingival crevice
Non-shedding surface
Plaque buildup
What are biofilms?
Free-floating bacteria attach to a solid surface
Multiple species
Embedded in extracellular slime layer
Antibiotic resistance
Latent state (nutritional needs)
E.g. plaque on teeth, dental implants, contaminated waterlines, indwelling prosthetic devices, ear infections, contact lenses
Dental unit water lines and biofilms
Form where water is left to sit e.g. tubing
DUWL contamination with biofilm poses two major issues
infection risk (e.g. pseudomonas)
Equipment breakdown from occluding the lines and also corroding metal compounds
The pellicle
Pellicle: Salivary glycoproteins that attach to tooth enamel
Adherence is essential for survival of bacteria
Pellicle formation occurs in seconds on cleaned enamel and reaches the maximum in 90-120min
Within a few mins pioneer bacteria will attach to pellicle
Initial adhesion involves salivary components adsorbed to the oral cavity surface (pellicle)
What are examples of pioneer species?
Strep. sanguinis, strep. Gordonii, strep. mutans
What are the stages in plaque development?
Attachment, initial colonisation, secondary colonisation, mature biofilm
What is calculus?
Calcified plaque
Calcium and phosphate salts in saliva - hard water areas
Rough porous surface - more plaque can form
Has to be removed by scaling instruments
What factors lead to caries?
mutans streptococci
Lactobacilli
Other acidogenic/aciduric streptococci
Frequent sugar/ low pH challenges low saliva flow
What factors lead to periodontal disease?
Gram-negative anaerobes
treponema denticola
Porphyromonas gingivalis
Tannarella forsythia
Aggregatibacter actinomycetemcomitans
Inflammation
Immune suppression
Increased gingival crevicular flow
Dental caries
Breakdown of the hard tissues of the teeth
acid environment → demineralisation → erodes enamel or dentin
Enamel caries
common in young children
Fissures most common site
Mutans streptococci, lactobacillus
Root surface caries
more common in older people
Thought to possibly be polymicrobial
Transmissible
What factors are needed for caries?
Tooth, bacteria, diet, time
How does bacterial metabolism contribute to the development of caries?
Cariogenic bacteria produce acids
glycolysis/fermentation
Dissolves some of the minerals in the adjacent enamel surface - calcium phosphate and carbonate salts are lost from hydroxyapatite crystals - demineralisation
Saliva can neutralise the acid
can enable repair of the enamel - remineralisation
The more fermentable carbohydrates are eaten, the more acid is produced, and the risk of caries increases
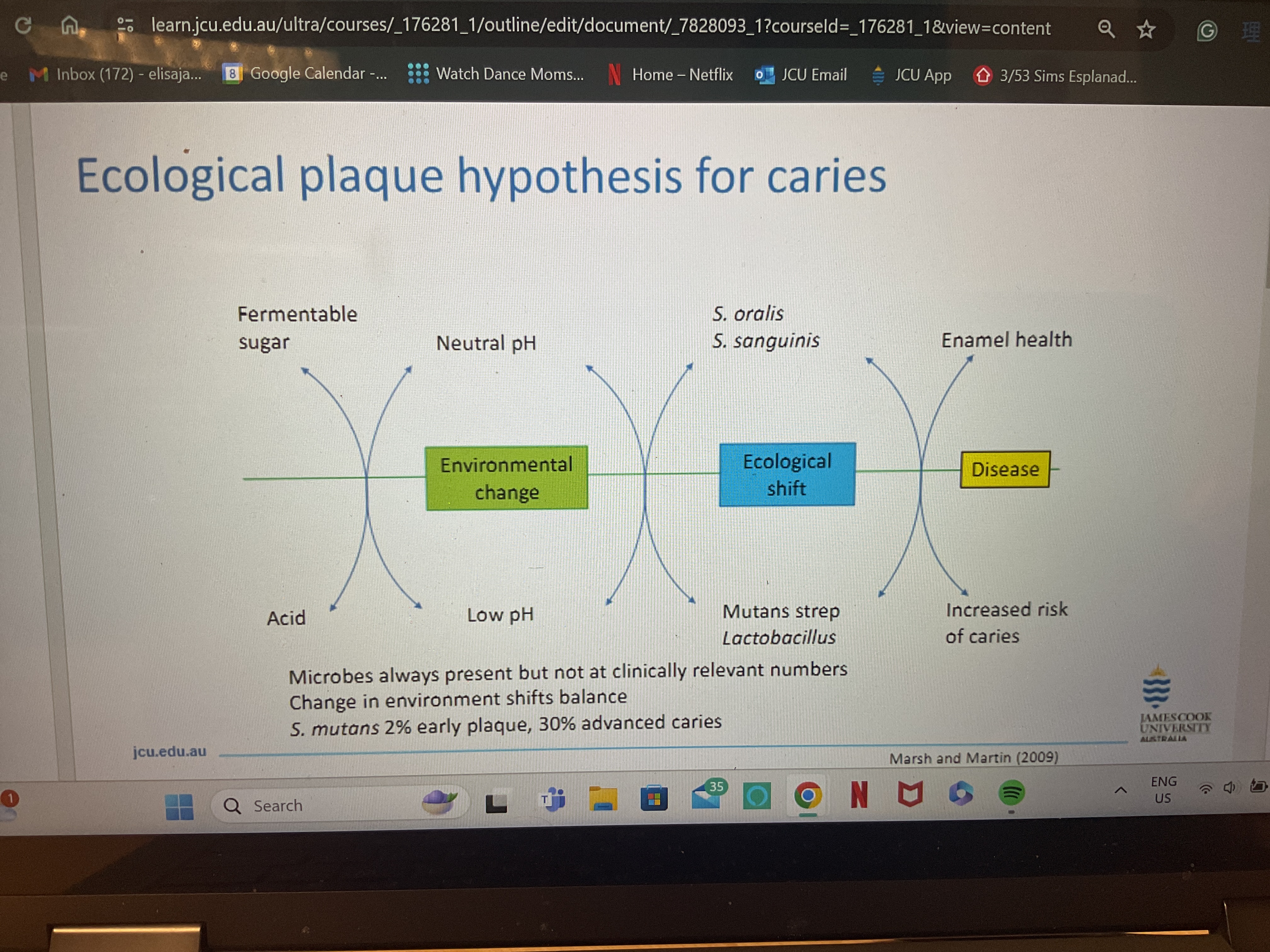
Ecological plaque hypothesis for caries
^^
How do lesions form?
S. Mutans attaches to the pellicle
Uses GTFs to produce glucans from sucrose
consolidates biofilm
Up-regulates CHO metabolism genes
ferments CHOs to lactic acid, acetate
Drops pH
Acid tolerance
expresses FoF1 ATPase to pump out protons
Lesion develops
What is saliva?
Complex secretion
99% water, 1% organic and inorganic molecules
Provides molecules for pellicle
Secreted from salivary glands located in the mouth
Secrete 500-700ml/day
average volume in mouth is 1.1 ml
Rate is 0.25-0.35 ml/min at rest; 1.5 ml/min when stimulated
Quality and quantity are important in maintaining oral health
What is the role of saliva?
Dilutes and eliminates sugars and other dietary components, microorganisms
patients with low flow rates (xerostomia) have increased risk of caries
Buffers pH changes produced by ingestion of foods with a low pH e.g. carbonated drinks, citrus fruit
Balances demineralisation/remineralisation
saturated with Ca²+, OH- and PO4
Periodontal diseases
Diseases where the supporting tissues of the teeth are attacked
Leading cause of tooth loss
Plaque accumulation + inflammatory response
Increase in gingival crevicular fluid
Periodontal pockets (anaerobic)
Selection for proteolytic, gram-negative bacteria
Germ-free animals
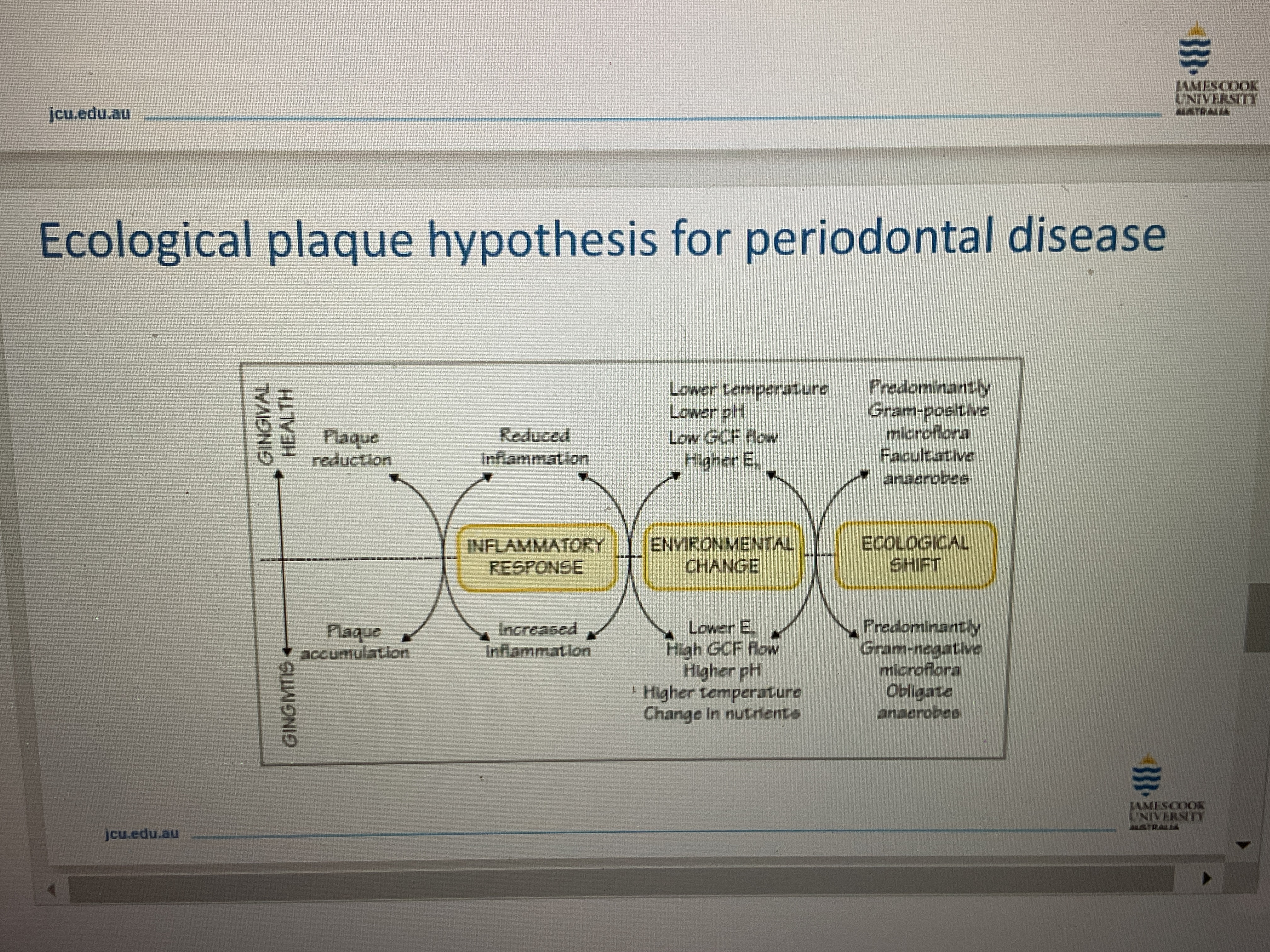
Ecological plaque hypothesis for periodontal disease
^^
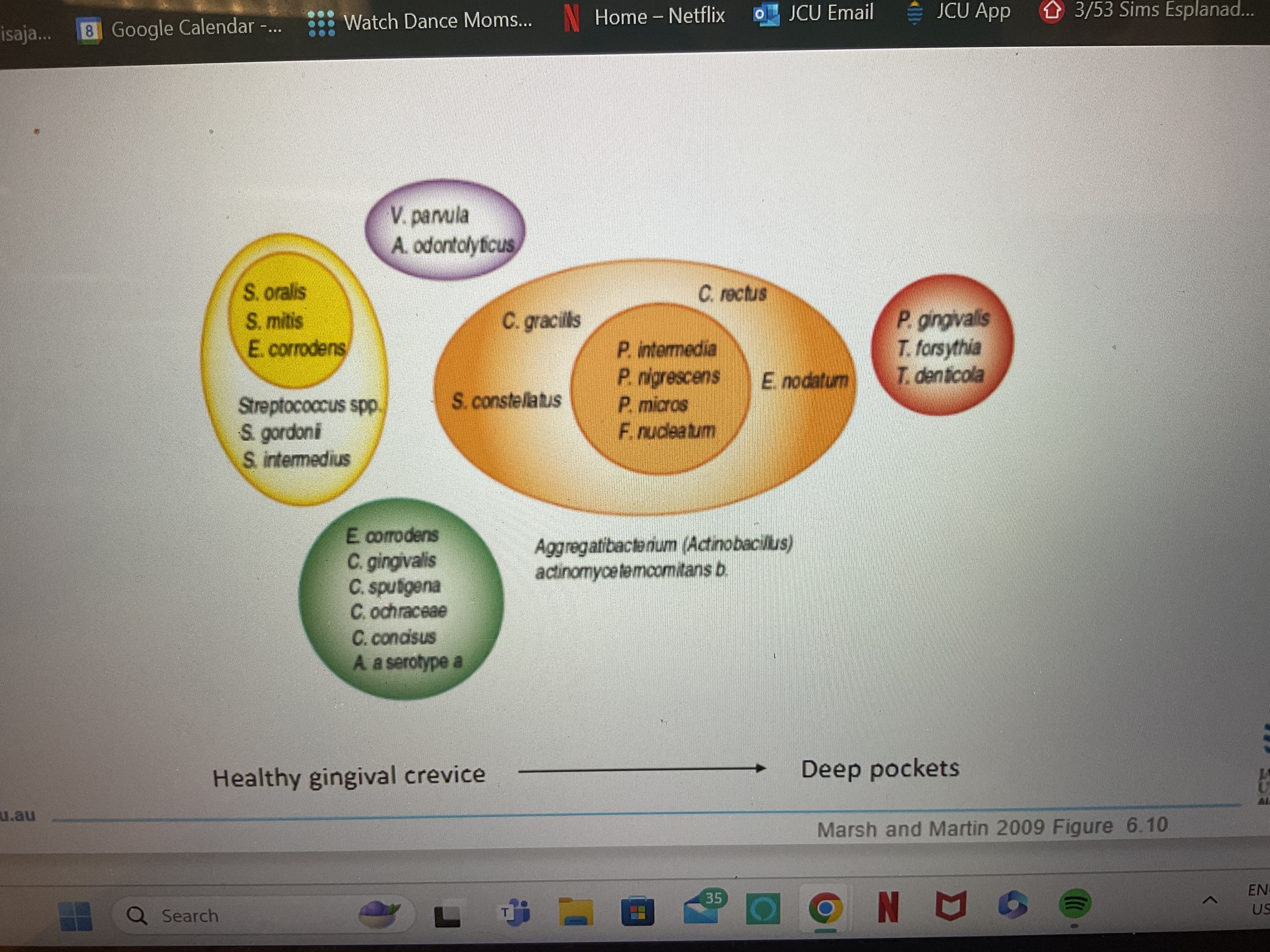
Microorganisms involved in the oral cavity
^^
Gingivitis
Early stages of periodontal disease
Inflammation of the gingiva in response to dental plaque
Host responses lead to destruction of gingival tissues
Periodontitis/periodontal disease
Fifth most prevalent health problem among Australians
Inflammation of the periodontium
Occurs when the gingivitis is untreated and inflammation spreads into ligaments and bones that support the teeth
Shift from gram-positive aerobes to gram-negative anaerobes (strong inflammatory response)
Periodontal pockets form creating an environment that is highly anaerobic, pH shifts to 7.7-7.8
proteilytic bacteria flourish
The common signs of periodontal disease (both gingivitis and periodontitis)are:
red, swollen or tender gingiva
Bleeding of the gingiva whilst brushing or flossing
Pus around the teeth or gingival tissues
As it progresses you will find
loose or separating teeth
Pain or pressure when chewing
Adherence to host surfaces
Adhesins and receptors usually interact in a complementary and fashion
Similar to interactions between enzymes/substrates
Usually many bonds form over area of contact
Oral cavity ligands
Pellicle contains mucins, salivary glycoproteins, minerals and immunoglobulins
proline-rich proteins (PRPs), statherin bind to enamel
Mucins, and agglutinins (e.g. gp340 glycoprotein) bind to enamel and epithelial surfaces
Attachment
Bacteria also attach to each other using adhesins
Some bacteria can’t attach directly to surface, need to attach to another species
can influence community structure
E.g. Porphyromonas gingivalis binding to streptococcus gordonii
What are the factors that affect adherence?
Host factors (ligands), saliva (suspending medium) and bacterial factors (adhesins)
Plaque maturation
As plaque matures on the tooth it increases in mass and thickness and the microbial composition also changes
After 7 days streptococci are still the main organisms on the tooth surface
After 14 days there is a shift to anaerobic rods
Climax community = situation where you have bacteria sloughing off and other bacteria attaching to the plaque, an equilibrium
Mature plaque is potentially more pathogenic
Subgingival plaque
Tooth attached plaque (detrimental to periodontal tissues)
Epithelial attached plaque (less risky)
Unattached plaque (bacteria not part of biofilm)
Calculus
Supragingival
above the gingival margin
Yellowish-white
Subgingival
tooth root surfaces below the gingival margin
Periodontal pocket
Black/ dark green
Mutans streptococci
Seven different species and 8 serotypes (a-h)
S. mutans serotypes c/e/f, S. sobrinus serotypes d/g most common in humans
Produces extracellular polysaccharides (glucans) from sucrose that help in colonisation
Can initiate and maintain growth, metabolism, acid production at low pH
Efficient and rapid metabolism of sugars to lactic acid
Lactobacillus spp.
Cariogenic qualities
increased numbers in most carious cavities affecting enamel enamel and tooth surfaces
Able to initiate and maintain growth at low pH
Produce lactic acid below pH 5
Some strains produce extracellular polysaccharides
Not involved in initiation but in progression of lesion deeper into enamel and dentine
Porphyromonas gingivalis
Obligate anaerobic Gram-negative bacillus
Found mostly in Subgingival plaque
Part of the red complex
Keystone species
present in low numbers but has huge influence on microbial community structure