PATHO CH. 42 Clinical Manifestations of Gastrointestinal Dysfunction
1/236
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
237 Terms
anorexia
Loss of appetite despite physiological stimuli that would normally produce hunger.

What is the vomiting reflex and which part of the brain is responsible for it?
Forceful emptying of the stomach and intestinal contents through the mouth, initiated by the vomiting center in the medulla oblongata.

What are some common antiemetic medications used for nausea and vomiting?
Serotonin and neurokinin-1 antagonists, metoclopramide, domperidone, olanzapine, corticosteroids, apomorphine, levodopa, and bromocriptine.
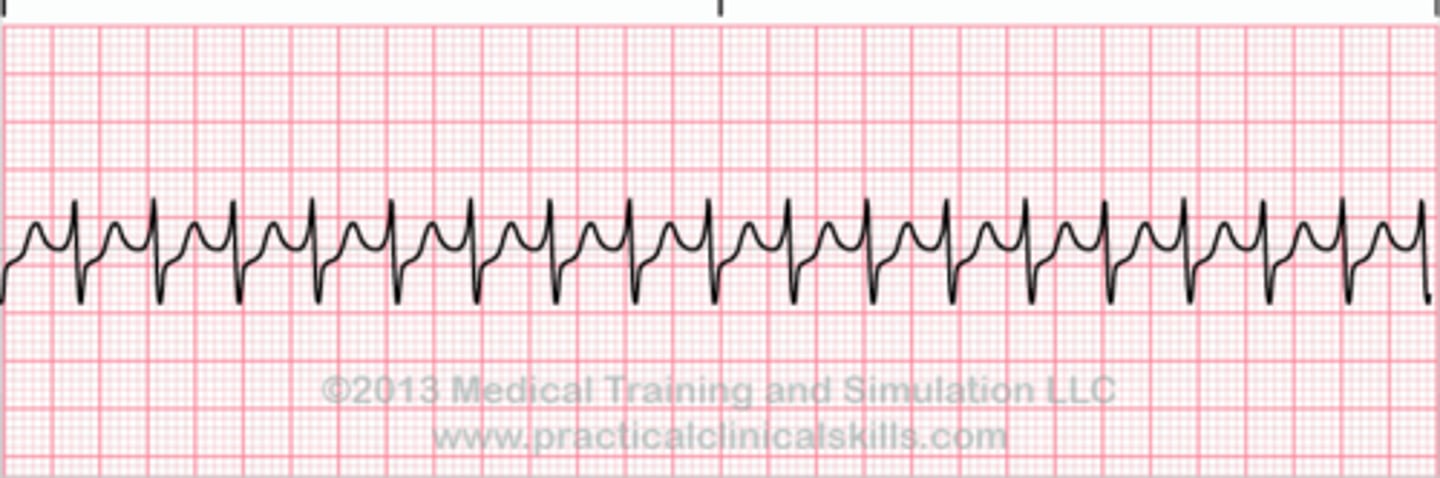
What is nausea and what are its common symptoms?
A subjective experience associated with various conditions, commonly accompanied by hypersalivation and tachycardia.
What is retching?
Vomiting without the expulsion of vomitus.

What are the types of constipation based on pathophysiology?
Normal transit (functional), slow-transit, pelvic floor dysfunction, and secondary constipation.

What are some treatments for constipation?
Bowel retraining, moderate exercise, increased fluid and fiber intake, enemas, biofeedback for dyssynergic defecation, and medications like colonic secretagogues and laxatives.
What defines diarrhea in terms of bowel movement frequency?
Increased frequency of bowel movements, defined as three or more per day.

What are the clinical manifestations of diarrhea?
Dehydration, electrolyte imbalance (hyponatremia, hypokalemia), metabolic acidosis, and weight loss.

What is the primary treatment for diarrhea?
Restoring fluid and electrolyte balance, along with medications such as antimotility agents and water absorbents.

What is the role of loperamide in diarrhea treatment?
It is an antimotility medication used to reduce the frequency of bowel movements.

What dietary recommendations can help with mild diarrhea?
Natural bran and psyllium.

What is the significance of biofeedback in treating dyssynergic defecation?
It helps patients learn to coordinate pelvic floor muscle relaxation during defecation.
What is the normal range for bowel movements per week?
Two to three per day to one per week.
What is the difference between normal transit constipation and slow-transit constipation?
Normal transit constipation has a normal rate of stool passage but difficulty with evacuation, while slow-transit constipation involves impaired colonic motor activity.
What are systemic manifestations of diarrhea?
Fever, with or without vomiting or cramping pain.

What are the manifestations of inflammatory bowel disease?
Fever, cramping pain, and bloody stools.

What are the signs of malabsorption syndromes?
Steatorrhea (fat in the stools), bloating, and diarrhea.

What are the types of abdominal pain associated with gastrointestinal disorders?
Mechanical, inflammatory, or ischemic.
What is parietal (somatic) pain?
Pain felt in the peritoneum.
What is visceral pain?
Pain felt in the organs themselves.
What is referred pain?
Pain felt in another area of the body.
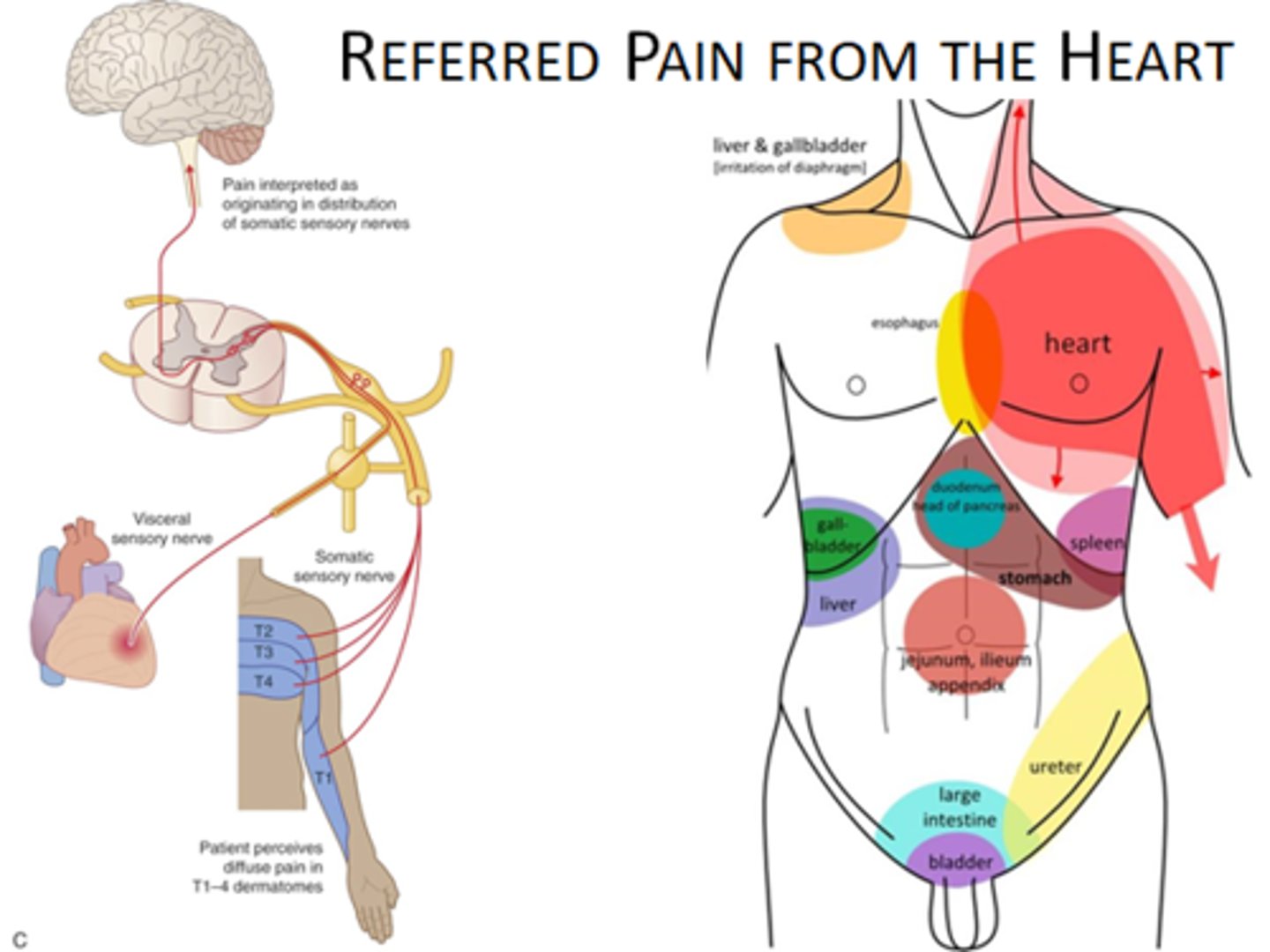
What biochemical mediators stimulate pain nerve endings in the abdomen?
Histamine, bradykinin, and serotonin.
What are the characteristics of upper GI bleeding?
Frank, bright red bleeding in emesis or dark, grainy digested blood (coffee grounds) in stool.
What is hematemesis?
Bloody vomit.
What is hematochezia?
Bloody stools.
What is melena?
Black, tarry stools.

What is occult bleeding?
Bleeding that is not visible.
What is dysphagia?
Difficulty swallowing.

What are the types of dysphagia?
Mechanical obstructions (intrinsic vs. extrinsic) and functional obstructions of esophageal motility.
What is achalasia?
Denervation of smooth muscle in the esophagus and lack of lower esophageal sphincter relaxation.
What are the clinical manifestations of upper esophageal obstruction?
Discomfort occurring 2-4 seconds after swallowing.

What are the clinical manifestations of lower esophageal obstruction?
Discomfort occurring 10-15 seconds after swallowing.
What are common symptoms of dysphagia?
Retrosternal pain, regurgitation of undigested food, unpleasant taste, vomiting, and weight loss.
What are some treatments for dysphagia?
Eating slowly, small meals, taking fluids with meals, elevating the head of the bed, oral medications, tube feedings, dilation, or surgical myomotomy.

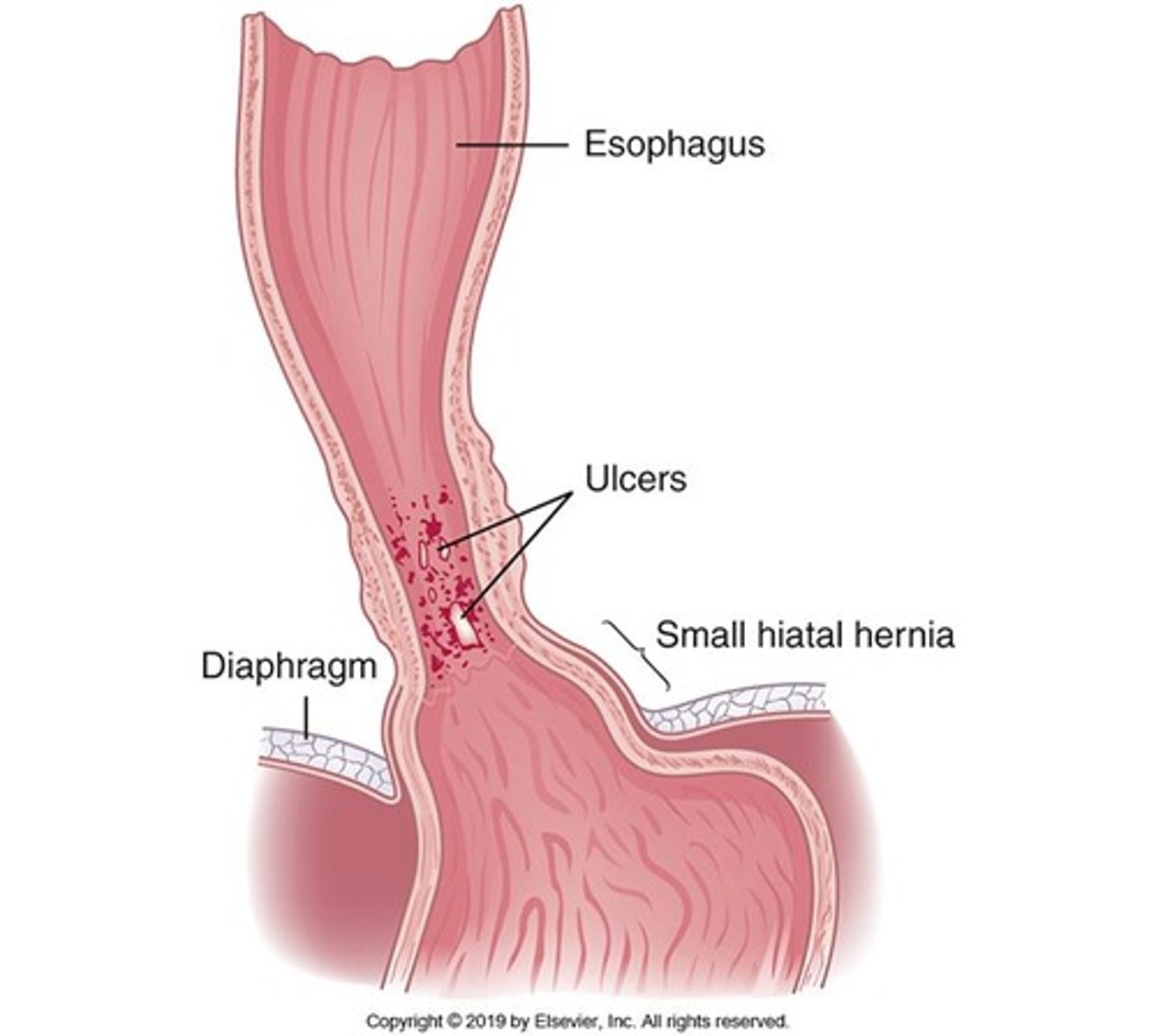
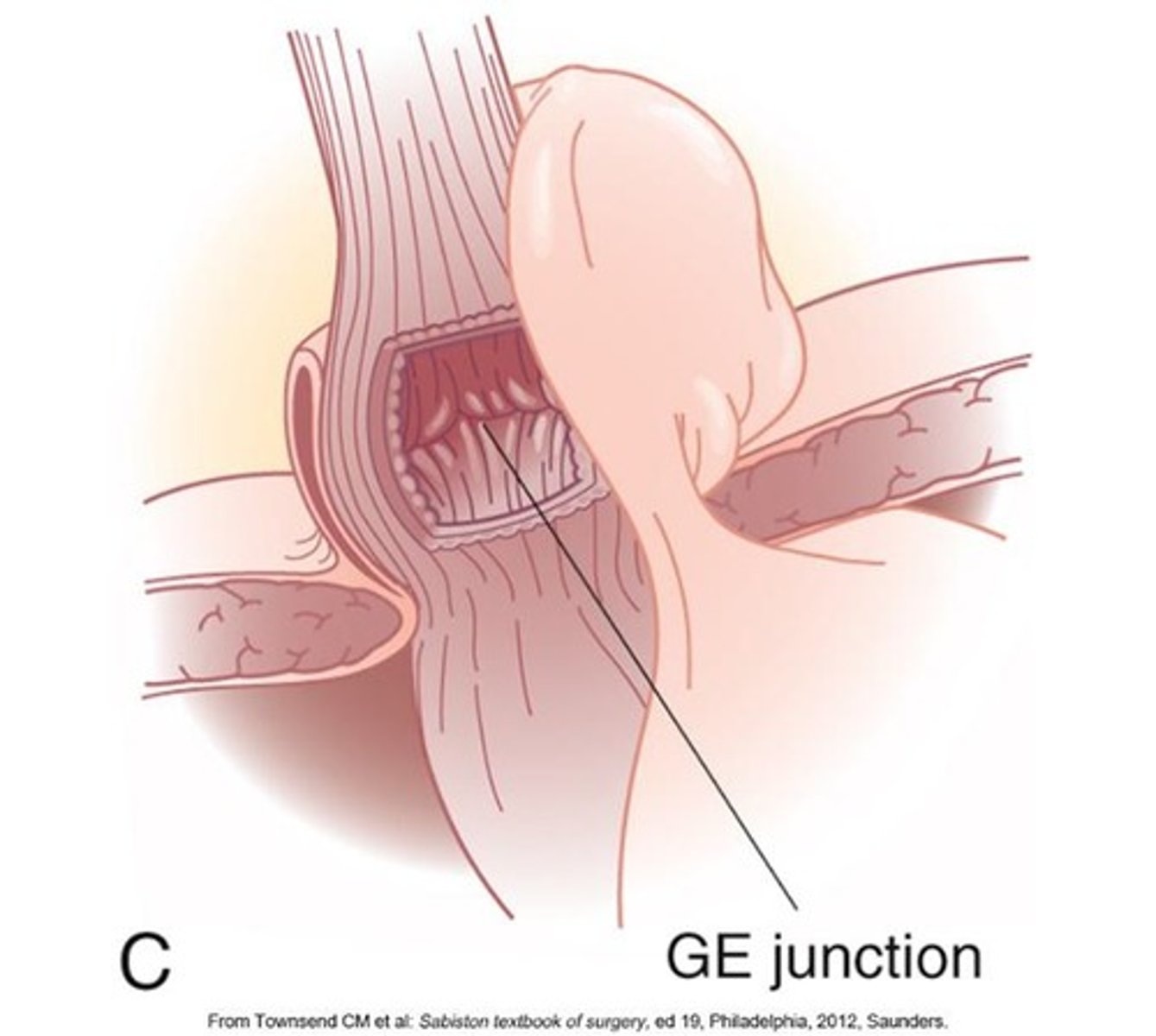
What causes gastroesophageal reflux disease (GERD)?
Acid and pepsin reflux from the stomach into the esophagus, often due to lower resting tone of the lower esophageal sphincter.
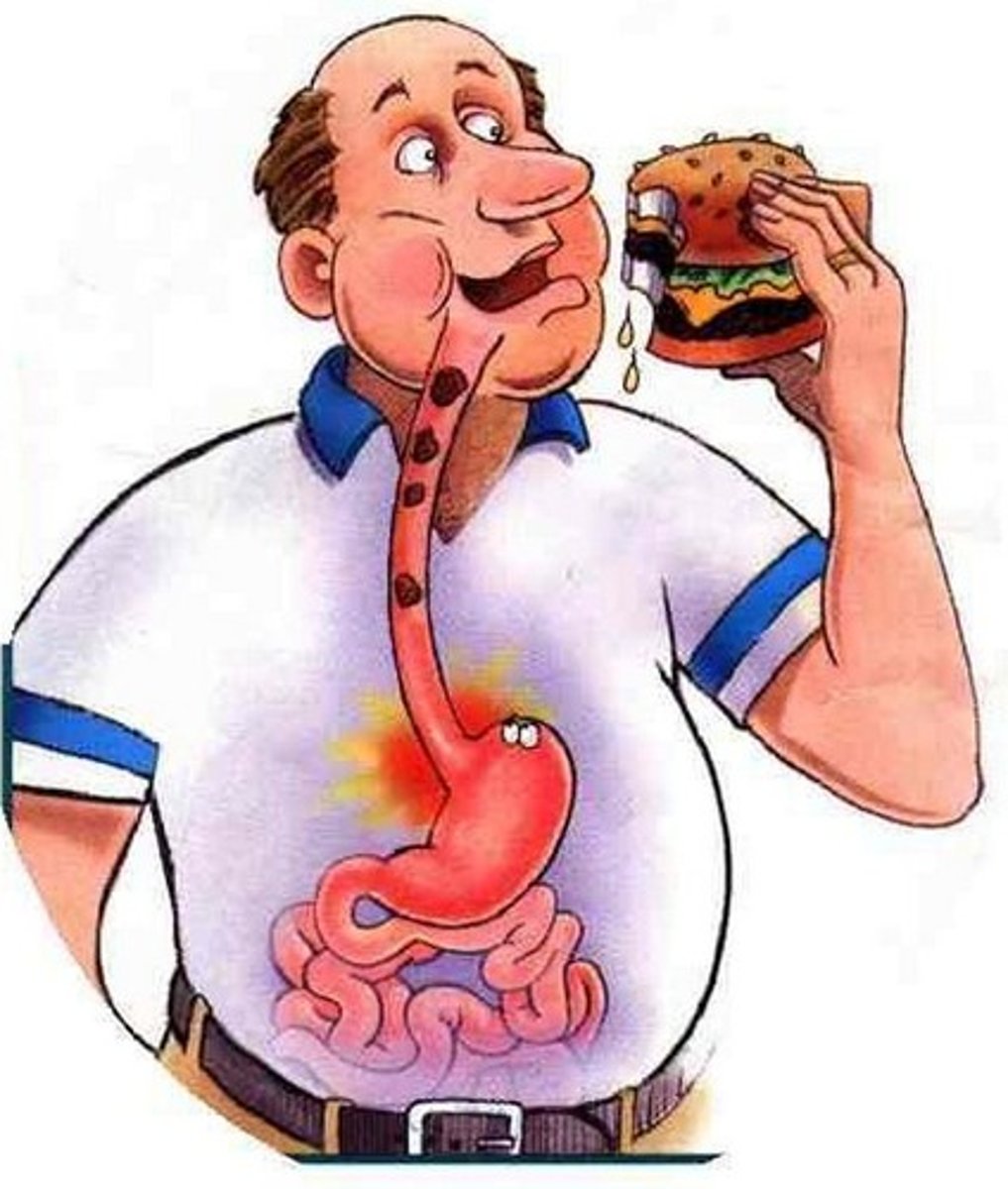
What are the clinical manifestations of GERD?
Heartburn from acid regurgitation, chronic cough, laryngitis, asthma attacks, sinusitis, and upper abdominal pain within 1 hour of eating.

What is the most effective treatment for GERD?
Proton pump inhibitors.
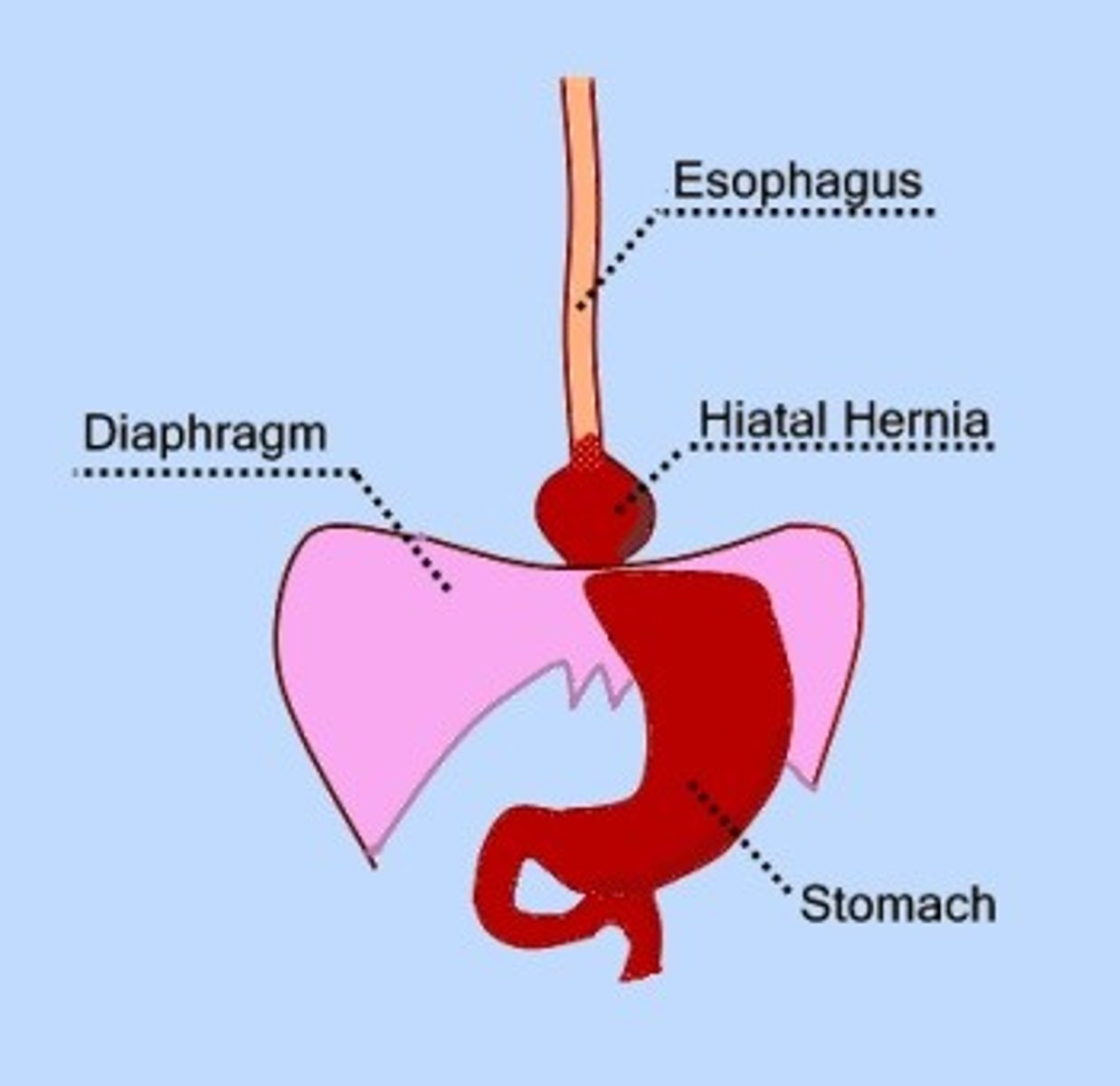
What is a hiatal hernia?
Protrusion of the upper part of the stomach through the diaphragm and into the thorax.
- type 1-3
- Asymptomatic, heartburn, regurgitation, dysphagia, and epigastric pain.
- Small, frequent meals; to treat or Laparoscopic surgery (fundoplication).
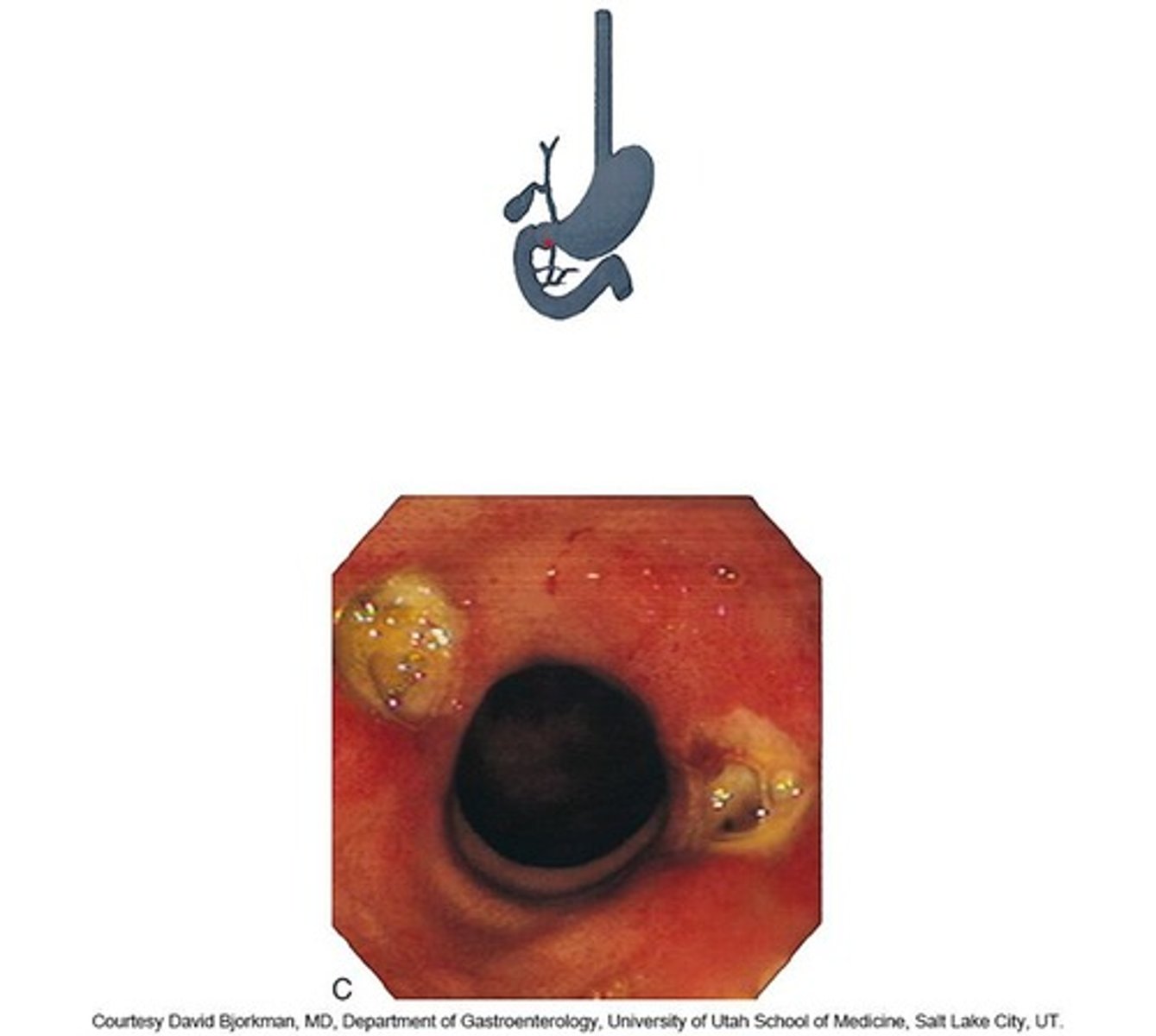
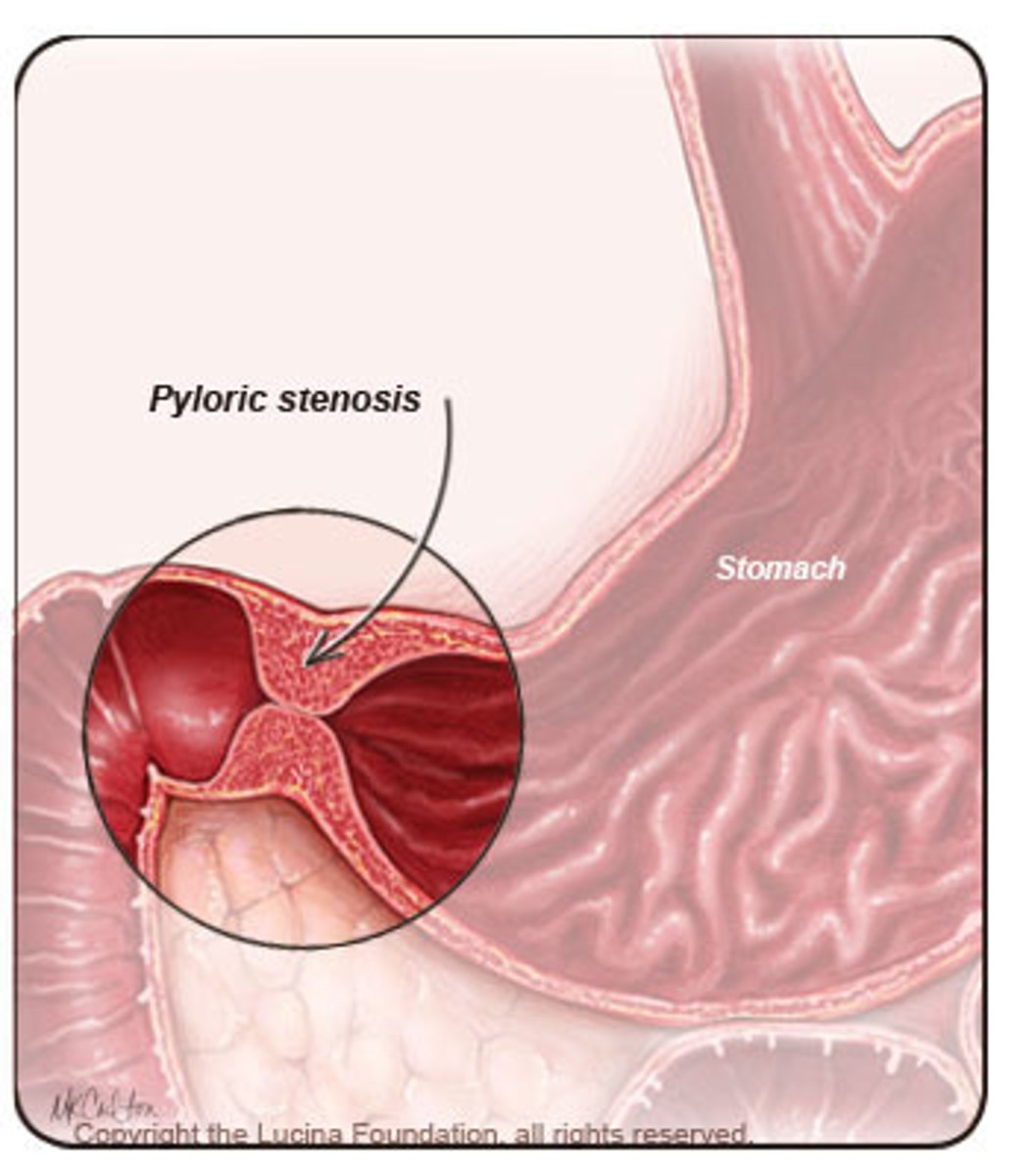
pyloric obstruction
Blocking or narrowing of the opening between the stomach and duodenum, which can be acquired or congenital.
- Epigastric pain and fullness, nausea, succussion splash, vomiting; prolonged cases can lead to malnutrition and dehydration.
- Gastric drainage; intravenous (IV) fluid and electrolytes; IV nutrition; proton pump inhibitors or H2 receptor antagonists; surgery or stenting.
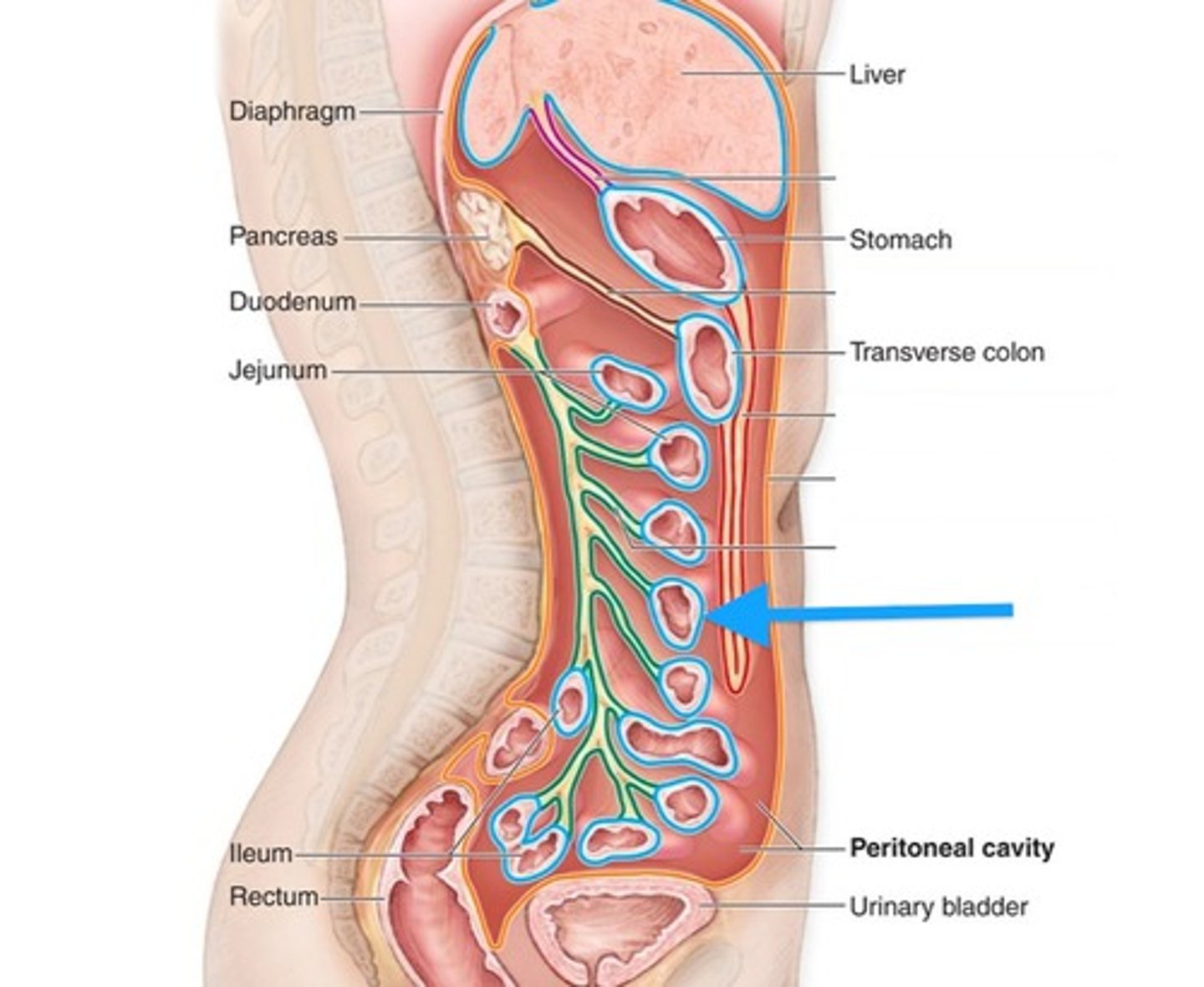
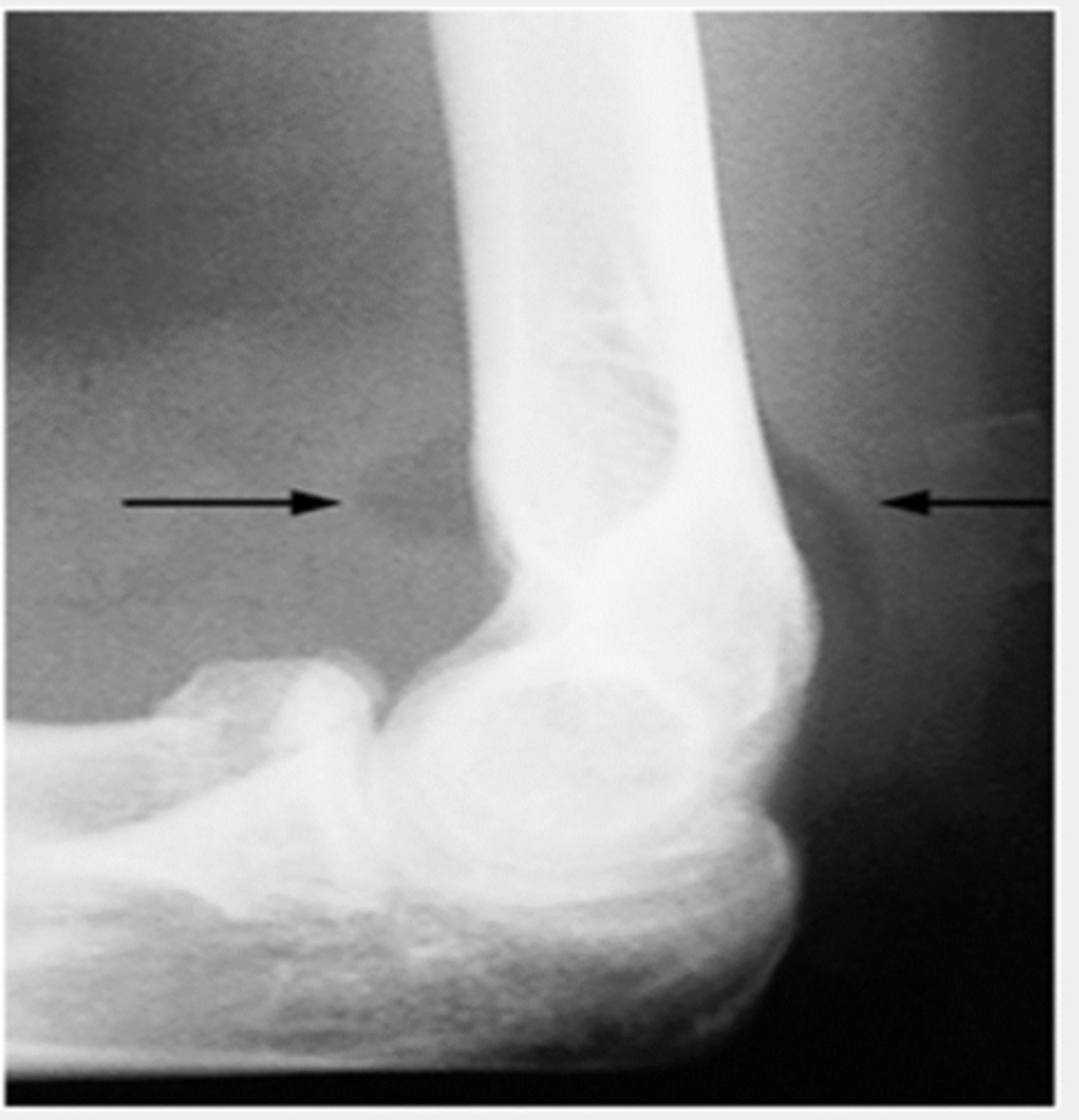
What defines intestinal obstruction?
Any condition that prevents the flow of chyme through the intestinal lumen or failure of normal intestinal motility in the absence of an obstructing lesion.
What are the clinical manifestations of small intestine obstruction?
Colicky pains caused by intestinal distention, followed by nausea and vomiting.
What are the clinical manifestations of large intestine obstruction?
Hypogastric pain and abdominal distention.
What are the general treatment approaches for intestinal obstruction?
Replacement of fluid and electrolytes; gastric or intestinal suction; laparoscopic procedures for adhesions; immediate surgical intervention for strangulation and complete obstruction; colonic stent for malignant obstruction; neostigmine for colonic pseudo-obstruction; IV antibiotics and fluid resuscitation for intestinal perforation.
What can the type of vomitus indicate in cases of intestinal obstruction?
It can indicate the location of the obstruction.
What is a simple obstruction?
Presence of a lesion.
What is a functional obstruction?
Paralytic ileus, characterized by failure of motility, especially after surgery.
What is the most common cause of small intestinal obstruction?
Fibrous adhesions.
What are the most common causes of large bowel obstruction?
Colorectal cancer, volvulus (twisting), and strictures related to diverticulitis.
What is Ogilvie syndrome?
Acute colonic pseudo-obstruction characterized by massive dilation of the large bowel, typically in critically ill patients and older adults who are immobilized.
What is acute gastritis?
An inflammatory disorder of the gastric mucosa associated with Helicobacter pylori, NSAIDs, drugs, chemicals, and metabolic disorders.
What are the clinical manifestations of acute gastritis?
Vague abdominal discomfort, epigastric tenderness, and bleeding.
What is the typical treatment for acute gastritis?
Healing usually occurs spontaneously within a few days; discontinue injurious drugs; administer antacids.
Which statement is correct regarding disorders of motility?
A succussion splash from jarring of the abdomen occurs in pyloric obstruction.
What are the two types of chronic gastritis?
Chronic Antral Gastritis (Type B) and Chronic Fundal Gastritis (Type A).
What is Chronic Antral Gastritis associated with?
H. pylori, NSAIDs, alcohol, and tobacco.
What is Chronic Fundal Gastritis associated with?
Autoantibodies to parietal cells and intrinsic factor, resulting in gastric atrophy and pernicious anemia.
What are common clinical manifestations of chronic gastritis?
Anorexia, fullness, nausea, vomiting, epigastric pain, and gastric bleeding.
What are the treatment options for chronic gastritis?
Smaller meals, soft bland diet, avoidance of alcohol and NSAIDs, administration of combination antibiotics, and Vitamin B for pernicious anemia.
What causes Alkaline Reflux Gastritis?
Reflux of bile and alkaline pancreatic secretions.
What are the clinical manifestations of Alkaline Reflux Gastritis?
Nausea, bilious vomiting, and sustained epigastric pain that worsens after eating and is not relieved by antacids.
What is the treatment for Alkaline Reflux Gastritis?
Avoidance of aspirin and alcohol, low-fat diet, and possible surgical correction.
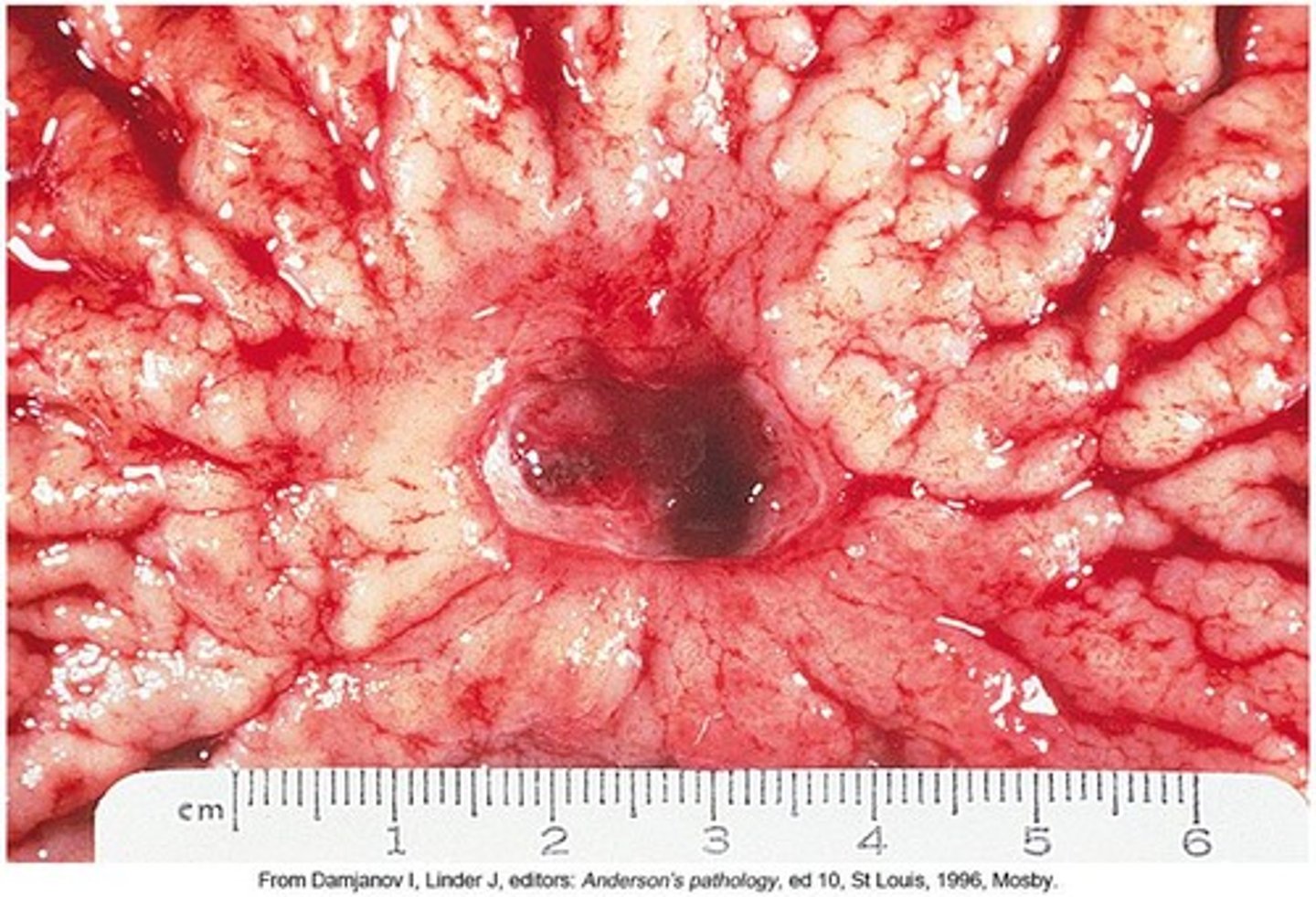
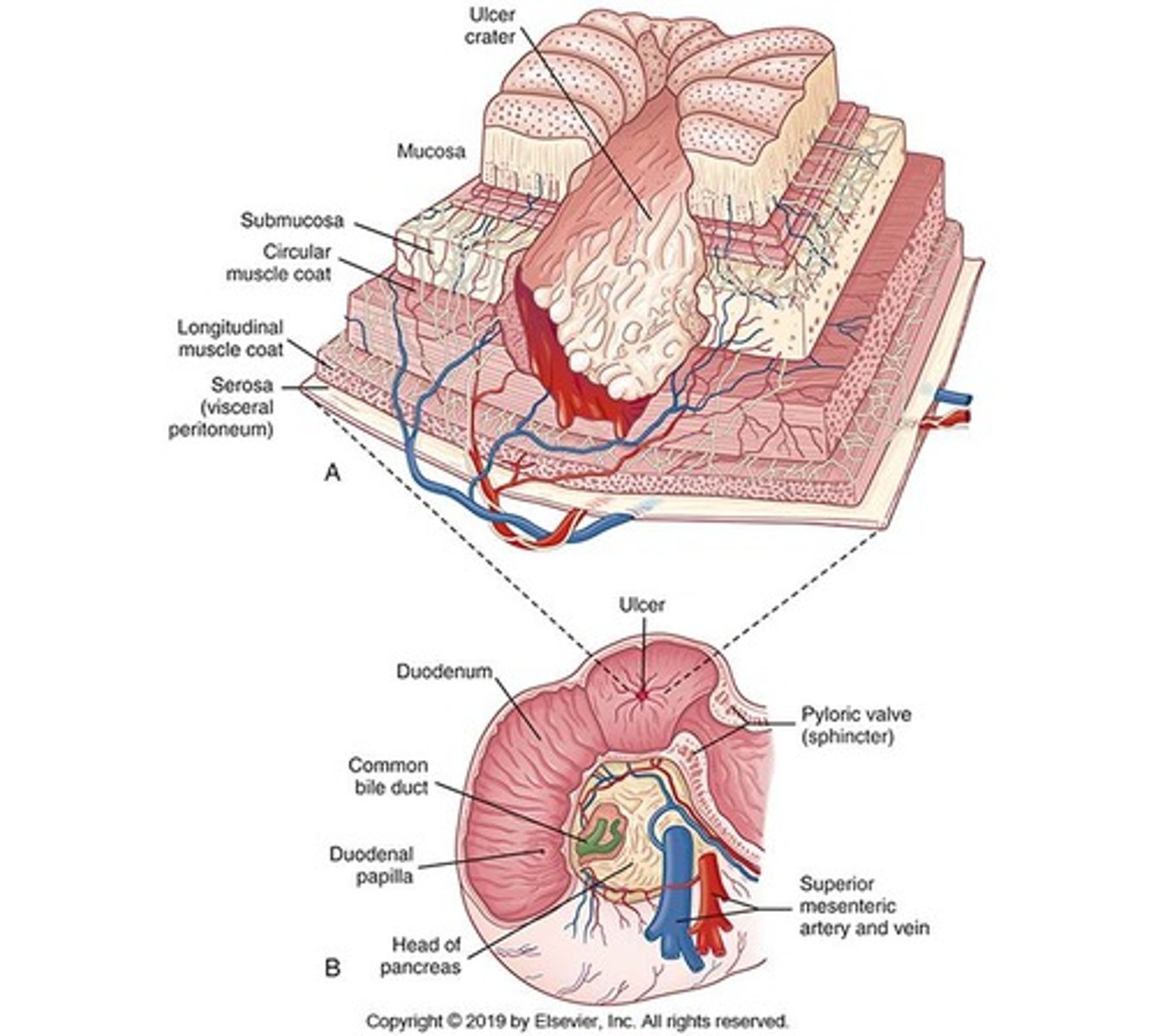
What is Peptic Ulcer Disease?
A break or ulceration in the protective mucosal lining of the lower esophagus, stomach, or duodenum.
What are the risk factors for Peptic Ulcer Disease?
Genetic predisposition, H. pylori infection, habitual use of NSAIDs and aspirin, excessive use of alcohol, smoking, acute pancreatitis, chronic obstructive pulmonary disease, obesity, cirrhosis, socioeconomic status, and being over 65 years of age.
What are the characteristics of duodenal ulcers?
Most common type of peptic ulcer, associated with altered mucosal defenses, high gastrin levels, rapid gastric emptying, and acid production from smoking.
What are the clinical manifestations of duodenal ulcers?
Chronic intermittent pain in the epigastric area, occurring 30 minutes to 2 hours after eating, relieved by food and antacids.
What treatments are available for duodenal ulcers?
Antacids, proton pump inhibitors, H-2 receptor blockers, anticholinergics, sucralfate, colloidal bismuth, and surgical resection.
What is the primary defect in gastric ulcers?
Increased mucosal permeability to hydrogen ions.
What are the clinical manifestations of gastric ulcers?
Pain occurs immediately after eating, along with anorexia, vomiting, and weight loss.
What is Zollinger-Ellison Syndrome?
A condition associated with a gastrinoma that causes chronic secretion of gastric acid, leading to gastric and duodenal ulcers.
What are the clinical manifestations of Zollinger-Ellison Syndrome?
Gastroesophageal reflux with abdominal pain and diarrhea.
What is the treatment for Zollinger-Ellison Syndrome?
Proton pump inhibitors to reduce gastric acid secretion and surgical removal of tumors to limit metastasis.
What is Stress-Related Mucosal Disease?
A peptic ulcer related to a severe illness, multisystem organ failure, or major trauma.
What is an ischemic ulcer?
An ulcer that develops within hours of an event.
What is a Curling ulcer?
An ulcer that develops after a burn injury.
What is a Cushing ulcer?
An ulcer that develops as a result of head trauma or brain surgery from hypersecretion of hydrochloric acid from the vagal nuclei.
What is the most common clinical manifestation of Stress-Related Mucosal Disease?
Bleeding.
What is the treatment approach for Stress-Related Mucosal Disease?
Prophylactic therapy.
What is Dumping Syndrome?
Rapid emptying of hypertonic chyme from the stomach into the small intestine.
What are common complications leading to Dumping Syndrome?
Partial gastrectomy, bariatric procedure, or pyloroplasty.
What are the developmental factors for early dumping syndrome?
Loss of gastric capacity, loss of emptying control, and loss of feedback control by the duodenum when it is removed.
What are the clinical manifestations of early dumping syndrome?
Diarrhea, cramping, feeling of epigastric fullness, pain, nausea, and vomiting.
What are the clinical manifestations of late dumping syndrome?
Weakness, diaphoresis, and confusion.
What are some treatment options for early and late dumping syndrome?
Consuming frequent small meals high in protein and low in carbohydrates, drinking fluids between meals, reclining on the left side after eating, reconstructing the pylorus or performing a gastrojejunostomy, and administering Octreotide.
What is malabsorption syndrome?
A condition that interferes with nutrient absorption.
What is maldigestion?
Failure of the chemical processes of digestion.
What is malabsorption?
Failure of the intestinal mucosa to absorb (transport) the digested nutrients.
What is pancreatic insufficiency?
Insufficient pancreatic enzyme production, leading to fat maldigestion.
What are the most common signs of pancreatic insufficiency?
Fatty stools (steatorrhea) and weight loss.
What is lactase deficiency?
A congenital defect in the lactase gene causing inability to breakdown lactose, leading to fermentation by bacteria.
What are the clinical manifestations of lactase deficiency?
Gas, cramping pain, flatulence, and osmotic diarrhea.
What is bile salt deficiency?
A condition where conjugated bile salts are insufficient to emulsify and absorb fats, often due to liver disease or intestinal issues.
What are the consequences of bile salt deficiency?
Fatty stools, diarrhea, decreased plasma proteins, and loss of fat-soluble vitamins (A, D, E, K).
What are the symptoms of fat-soluble vitamin deficiencies?
Vitamin A: Night blindness; Vitamin D: Decreased calcium absorption, bone pain; Vitamin K: Prolonged prothrombin time; Vitamin E: Testicular atrophy and neurologic defects in children.
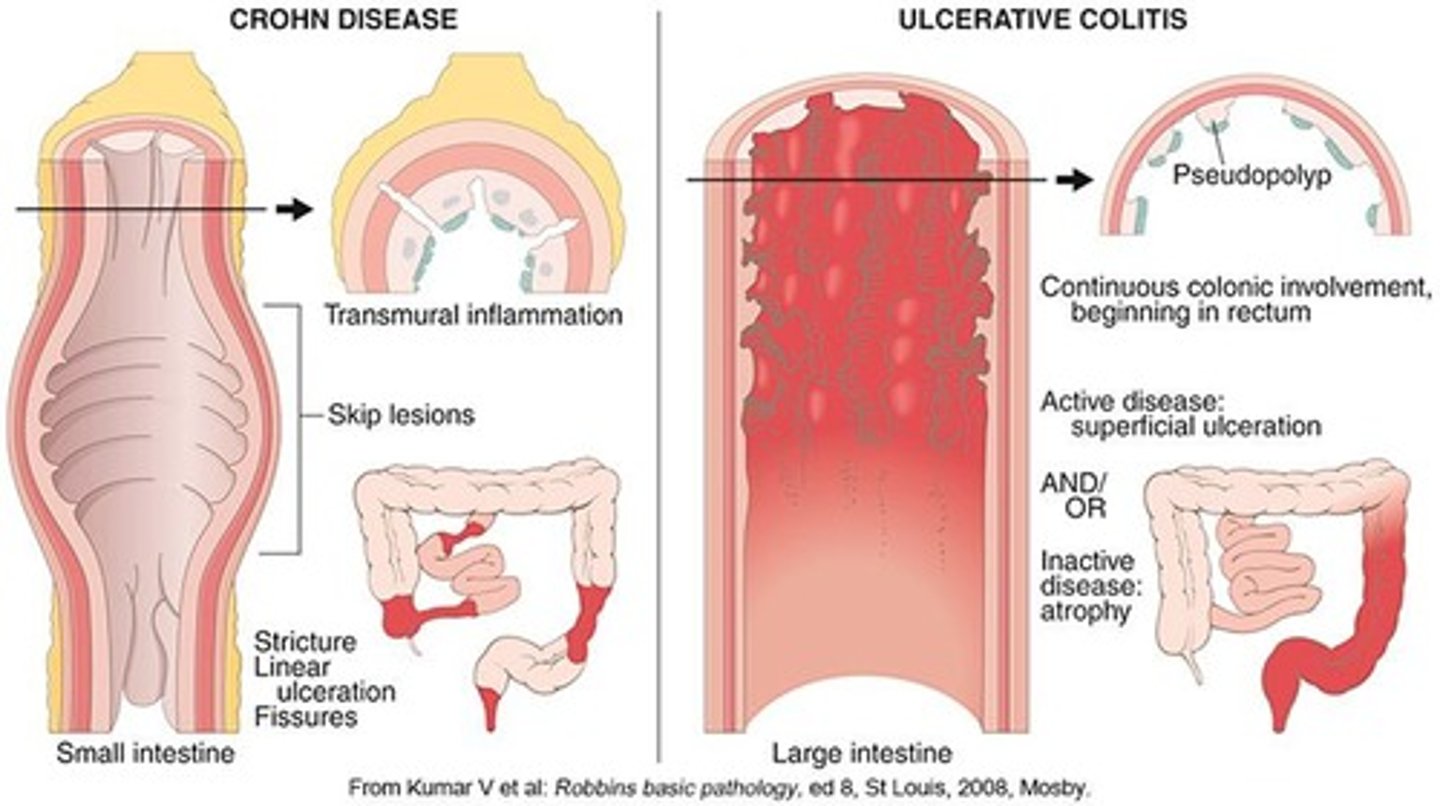
What are Inflammatory Bowel Diseases?
Chronic, relapsing inflammatory bowel disorders of unknown origin, influenced by genetics, environmental factors, and immune reactions.
What are two examples of Inflammatory Bowel Diseases?
Ulcerative colitis and Crohn's disease.
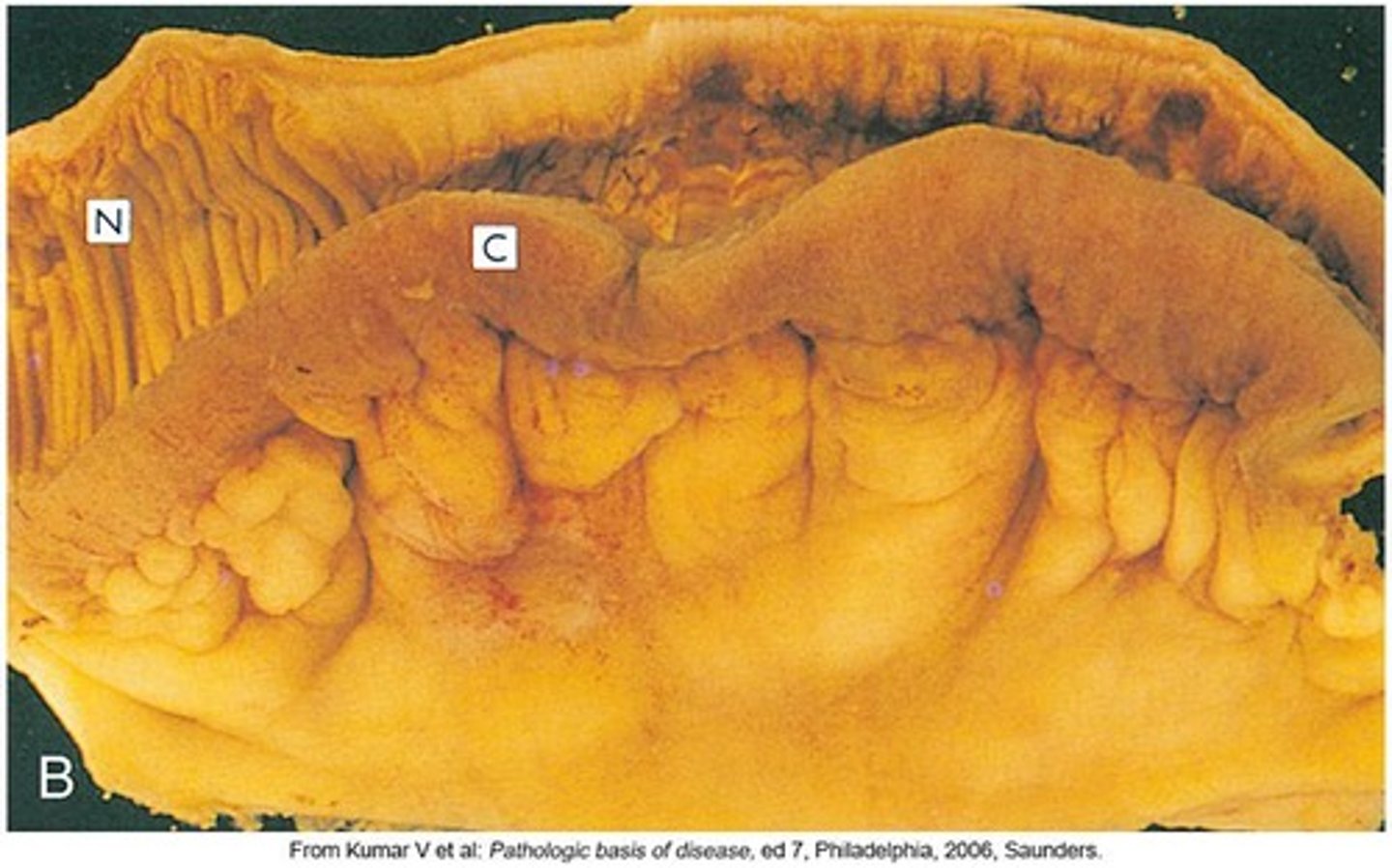
What is Ulcerative Colitis?
A chronic inflammatory disease that causes ulceration of the colonic mucosa, commonly affecting the sigmoid colon and rectum.
At what age is Ulcerative Colitis most common?
In individuals aged 20-40 years.
What are the characteristics of lesions in Ulcerative Colitis?
Lesions are continuous with no skipped lesions, limited to the mucosa, and not transmural.
What are the clinical manifestations of Ulcerative Colitis?
Large volumes of watery diarrhea, bloody stools, cramps, pain, and an urge to defecate.