Adult II Exam 2
1/71
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
72 Terms
what is anemia?
a decrease in the oxygen-carrying ability of the blood (low Hgb/RBCs)
what are the general s/s of anemia?
-pallor (low hgb levels and decreased BF to skin)
-jaundice (r/t Hgb breakdown → increased bilirubin concentration)
-fatigue, weakness
-pruritus (increased serum and skin bile concentrations)
-inc HR/palpitations, low blood viscosity → murmurs/bruits
-SOB
-HA, dizziness
-mild anemia (10-12)→ palpitations, dyspnea, and mild fatigue (due to underlying disease or compensatory response to exercise)
-moderate anemia (6-10) → increase in cardiopulmonary sx, may have them at rest and with activity
-severe anemia (<6) → involves multiple body systems
which lab tests are monitored and associated with anemia?
-hemoglobin (low)
-hematocrit (low) → volume of cells in 100 mL of blood
-MCV (size of RBCs) + MCHC (coloring of RBCs)
-reticulocytes (high) → immature RBCs
-serum B12/folate (low) → nutrients required for DNA synthesis/RBC development
-iron labs → TIBC (high), ferritin (low), serum iron (low)
-stool guaiac test → blood in stool
what is iron-deficiency anemia? what are the causes? what are the s/s?
-lack of iron → impaired RBC synthesis
-causes: blood loss**, lack of intake, malabsorption, hemolysis, pregnancy, GI/GU blood loss, hemodialysis
-s/s: general s/s of anemia + brittle nails, swollen tongue, cracked corners of mouth
how is iron-deficiency anemia treated?
-iron supplements (ferrous sulfate): take with vitamin C to increase absorption, black stools expected, may cause constipation/diarrhea/heartburn (take w/ stool softener)
-increased dietary intake: liver, muscle meats (liver beef, turkey, pork), fish, legumes, eggs, some dried fruits (raisins, apricots, peaches, prunes), beans, dark green/leafy veggie, whole grains, enriched bread and cereals, baked potatoes
Parenteral Iron
Indications: malabsorption, oral iron intolerance, need for iron beyond parenteral limits, poor patient adherence
what is cobalamin deficiency anemia? what are the causes? what are the s/s?
-lack of cobalamin (vitamin B12) → impaired RBC synthesis (macrocytic)
-causes: no intrinsic factor for B12 absorption (pernicious anemia), decreased intrinsic factor (alcoholism, medications, GI surgeries, old age), lack of dietary intake (vegans/vegetarians), smoking, long-term use of h2blockers/ppi’s
-s/s: general symptoms of anemia, neurologic symptoms (numbness/tingling, ataxia, confusion), abdominal pain
how is cobalamin deficiency anemia treated?
-B12 injections (usually for life)
-increase dietary intake: red meats, liver, eggs, enriched grain products, milk and dairy foods, fish
what is sickle cell disease?
-genetic, autosomal recessive disorder
-causes RBCs to lose round, concave shape and instead become sickle-shaped
-genetic mutation: normal hemoglobin (HbA) replaced by abnormal sickle cell hemoglobin (HbS)
what are the clinical manifestations/complications of sickle cell disease?
-pain → tissue hypoxia and damage
-pale mucous membranes
-jaundice → hemolysis of sickled RBCs
-complications → organ hypoxia, infection
what is a sickle cell episode vs. sickle cell crisis?
-episodes: triggered by low oxygenation (infection, stress, high altitude, blood loss, dehydration); sickling is initially reversible with re-oxygenation
-crisis: severe, painful, acute exacerbation of sickling leads to vaso-occlusive crisis; severe capillary hypoxia and eventual tissue necrosis, life threatening shock
how is a sickling episode/crisis treated?
-oxygen therapy
-IVF and electrolyte replacement
-blood transfusion
-close monitoring for respiratory failure
-pain management: PCA, heat packs (vasodilate), pain medication (continuous and breakthrough, patients often have developed tolerance to pain meds)
-elevate extremities → increase blood flow
-promote rest
-DVT prophylaxis
what things would a nurse teach a sickle cell patient about crisis prevention?
-prevent infection: vaccination, masks, avoidance, treat infections promptly
-stay hydrated
-avoid high altitudes
-receive prompt medical attention if an episode arises
-pain management
-medications: chelation therapy (helps remove excess iron), folic acid (inc RBC production), hydrea (antisickling agent)
what is thrombocytopenia?
-reduction of platelets (< 150,000)
-results in abnormal hemostasis (prolonged or spontaneous bleeding)
-primarily an acquired disorder (heparin, aspirin, malignancy)
what are the the possible complications a patient with thrombocytopenia might have?
-prolonged bleeding, especially when platelets are < 50,000
-hemorrhage risk (external or internal) when PLTs < 20,000
What is immune Thrombocytopenia Purpura?
most common acquired thrombocyotpenia
syndrome of abnormal destruction of platelets by spleen
primarily an autoimmune disease
live with platelets <100,000)=
what things would a nurse teach a patient with thrombocytopenia?
-avoid SQ/IM injections; if injection is necessary, apply pressure or ice packs
-teach s/s of bleeding so pt receives prompt treatment: mucosal or cutaneous bleeding, petechiae/purpura
-teach self-care measures to reduce risks for bleeding
-teach medication risks: cancer chemotherapy drugs, heparin, OTC meds that can cause blood thinning ( aspirin, NSAIDS, plavix, Coumadin)
-limit alcohol
-splenectomy → indicate if pts do not respond to other txs
-platelet transfusion → <10,000 or prophylactically for planned procedure
-corticosteroids → increase lifespan of platelets
-avoid contact sports
what is CLL? what is the disease process? what are the s/s?
-chronic lymphocytic leukemia
-most common leukemia in adults
-slowly progressive disease in which there is a proliferation of functionally inactive but long-lived, mature-appearing lymphocytes (infiltrate BM, spleen, liver)
-s/s: weakness, fatigue, weight loss, fever/night sweats, swollen lymph nodes
what are possible complications of CLL?
-immunosuppression
-lymph node enlargement & pain
-paralysis from pressure
-bone marrow suppression
what is CML? what are the s/s?
-chronic myelogenous leukemia → overproduction of mature and immature WBCs → bone marrow suppression
-s/s: fatigue, pallor, unexplained weight loss, abnormal bleeding
what is AML?
-acute myelogenous leukemia
-proliferation of immature WBCs (myeloblasts)
-s/s very similar to CML
what are the nursing responsibilities when caring for a patient with AML?
-disease management: bone marrow suppression from overcrowding of cancerous cells → anemia, thrombocytopenia, dec WBCs, infiltration into other organs (spleen, liver, lymph nodes, etc.)'
-Bone pain
-Meningeal irritation
-Oral lesions
-monitor labs: hematology, WBCs
-Dx: blood counts, bone biopsy
-manage side effects of drugs/treatment
-support psychosocial needs: patient education, stress management, reproductive concerns
-Chemotherapy
Other therapies
Corticosteroids
Radiation therapy - targeted or total body
Hematopoietic stem cell transplant
what is the difference between benign and malignant tumors?
benign:
-tumor that is not cancerous and does not spread to other areas of the body
-encpsulated
-slow, progressive growth
-rare recurrence
-typically good prognosis
malignant:
-tumor containing cancerous cells that spreads to other areas of the body
-undifferentiated, abnormal structure, not capsulated
-accelerated growth
-infiltrates/invades other tissues
-higher rate of recurrence
-prognosis depends on success of treatment
what is staging & grading of cancer?
-grading: classifies tumors by cellular changes (severity)
-staging: TNM (tumor size/invasiveness, nodular involvement (spread to regional lymph nodes), metastases)
what is the goal of chemotherapy?
-eliminate or reduce the number of malignant cells present in the primary tumor and metastatic tumor site(s); destroy rapidly growing/dividing cells
what is extravasation? what should the nurse do if this occurs?
-the leakage of chemotherapy drugs into the skin and surrounding tissue
-administration preferred through CVAD (implanted port)
-chemo is very toxic, causes skin break down and possible necrosis; swelling is first sign
-nurse management: immediately discontinue the infusion, cooling/diluting/elevating the site, extravasation kits on the unit (contain antidotes and flushes)
what is the goal of radiation?
causes cell death:
-kill or reduce tumor
-control: limit tumor growth, control symptoms
-provide comfort/palliation in metastatic disease
-prophylaxis: prevent further spread
what is brachytherapy? what are the nursing precautions for a patient undergoing bradytherapy?
-internal radiation
-radioactive seeds are implanted directly into the tumor/involved tissues or in close proximity adjacent to the tumor; may be permanent or temporary
-nursing precautions: ALARA principles (as low as reasonably achievable; avoiding exposure to radiation); limit time near radioactive source, increase distance between you and radioactive source, shield yourself from the source using a barrier (TDS); wear film badge (measures level of exposure)
what are the common side effects of chemotherapy & radiation?
-bone marrow suppression/hematologic: anemia, thrombocytopenia, infections
-fatigue
-GI effects: nausea, diarrhea, mouth sores; intenstinal mucosa is one of the most sensitive tissues
-pulmonary: toxicity and irreversible tissue damage
-cardiovascular: cardiotoxicity, HF
-skin effects: desquamation, rashes, skin redness, hair loss
-NS and cognitive: peripheral neuropathy, CNS edema, "chemo brain" (fogginess, forgetfulness)
-genitourinary: reproductive dysfunction, nephrotoxicity
what would be the patient teachings for someone who is neutropenic?
-monitor for s/s of infection
-prevent infections: avoid fresh flowers, cannot clean up after dog/cat, cannot have raw veggies/fruit/seafood/eggs, cannot drink well water; all nurses/visitors must wear masks in the room; hand hygiene
-meds to increase the WBCs may be scheduled prior to chemo (Neupogen - filgrastim; Neulasta - pegfilgrastim)
-a neutropenic emergency includes fever > 100.4 & neutrophil count < 500; call provider
-chemotherapy may be stopped until neutrophils levels rise again
what is superior vena cava syndrome? what are the s/s? what is the treatment?
-obstruction of the SVC by tumor or thrombosis
-commonly seen with lung cancers, breast tumors, and non-hodgkin's lymphoma
-s/s: facial/upper extremity edema, distended neck veins, HA, seizures
-tx: emergent radiation
what is spinal cord compression? what are the s/s? what is the treatment?
-compression of the spinal cord r/t malignant tumor in the epidural space
-commonly seen with breast, lung, prostate, GI, and renal tumors
-s/s: sudden intense back pain, new loss of bladder or bowel function
-tx: radiation and corticosteroids
what are the metabolic oncologic emergencies? what are the s/s and treatments of each?
SIADH (excessive ADH secretion; lung cancer)
-s/s: weight gain without edema, weakness, anorexia, N/V, severe hyponatremia
-tx: fluid restriction, hypertonic NS, lasix
hypercalcemia (metastatic bone cancer)
-s/s: depression, fatigue, muscle weakness, elevated serum Ca2+ levels
-tx: hydration (IVF) and diuretics, calcitonin
what is cardiac tamponade? what are the s/s? what is the treatment?
-fluid accumulation in the pericardial sac (pericardial effusion) + constriction of the pericardium or pericarditis (d/t radiation)
-s/s: heavy chest, dyspnea, tachycardia, cough
-tx: emergent fluid removal (pericardiocentesis)
what are the priority nursing interventions when caring for cancer patients?
-symptom management: antiemetics (especially on chemo days), pain medication/relief, energy conservation/light exercise (walking), skin care
-safety: neutropenic precautions, PPE for chemo administration
-monitor weight, small/frequent meals high in protein/calories, inc fluid intake
-monitor ECG, pay attention to sx of HF
-monitor neuro status
-monitor kidney function, avoid nephrotoxic drugs
what is an HLA screen?
human leukocyte antigens:
-determines tissue type
-HLA system is responsible for rejection of genetically unlike tissues
-HLAs of donor have to be matched to HLAs of recipient
what is a PRA screen?
panel of reactive antibodies:
-determines whether prospective crossmatch is needed
-high/positive PRA: indicates there are a lot of cytotoxic antibodies and the patient will most likely reject the new organ
-low/negative PRA: indicates a crossmatch will most likely be successful
what are the three types of organ rejection and what characterizes each?
hyperacute
-occurs in OR/first 24 hours
-blood vessels rapidly destroyed r/t antibodies (high PRA)
-no treatment
-organ must be retrieved
-patient death
acute
-occurs in first 6 months after transplant
-T-lymphocytes attack the organ
-usually reversible via high doses of immunosuppressive medications
chronic
-occurs over the lifespan of the transplanted organ
-fibrosis, scarring of the organ, irreversible damage/organ failure
-poor prognosis
-either need another transplant or they die from organ failure
what are the s/s of organ rejection?
-fever
-malaise
-body aches
-pain at transplant site
-signs of the transplanted organ failing
what is the action of calcineurin inhibitors? which are commonly used? what are potential side effects?
-suppress activation of cytotoxic T-cells
-cyclosporine, tacrolimus (Prograf)
-SE: nephrotoxicity (monitor BUN/creatinine), hypertension
what is the action of cytotoxic (antiproliferative) drugs? which are commonly used? what are common side effects?
-inhibit T and B cell proliferation
-sirolimus (rapamycin), azathioprine (imurman), mycophenolate mofetil (cellcept)
-SE: GI toxicity (N/V, diarrhea)
what is the action of corticosteroids (for immunosuppression)? which are commonly used?
-impair antigen recognition
-prednisone, methylprednisolone
-not used long-term; tapered off
what is the action of monoclonal antibodies? which are commonly used?
-decrease immunoreactivity by inhibiting t-cell proliferation
-received 2 hours prior to transplant
-Basiliximab, muromonab-CD3
what are common long-term problems associated with organ transplant?
-hypertension
-renal insufficiency
-hyperlipidemia
-diabetes
-osteoporosis
-malignancy**: skin cancer, post-transplant lymphoproliferative disease, other tumors
-CV disease**
-infection**
-transplant patients require frequent follow ups for signs of infection/rejection
what is ICP? what is the normal value?
-measure of the total pressure exerted by the three components within the skull (brain tissue, blood, and CSF)
-5-15 mmHg
-a sustained ICP > 20 mmHg is considered above the upper limit and is abnormal
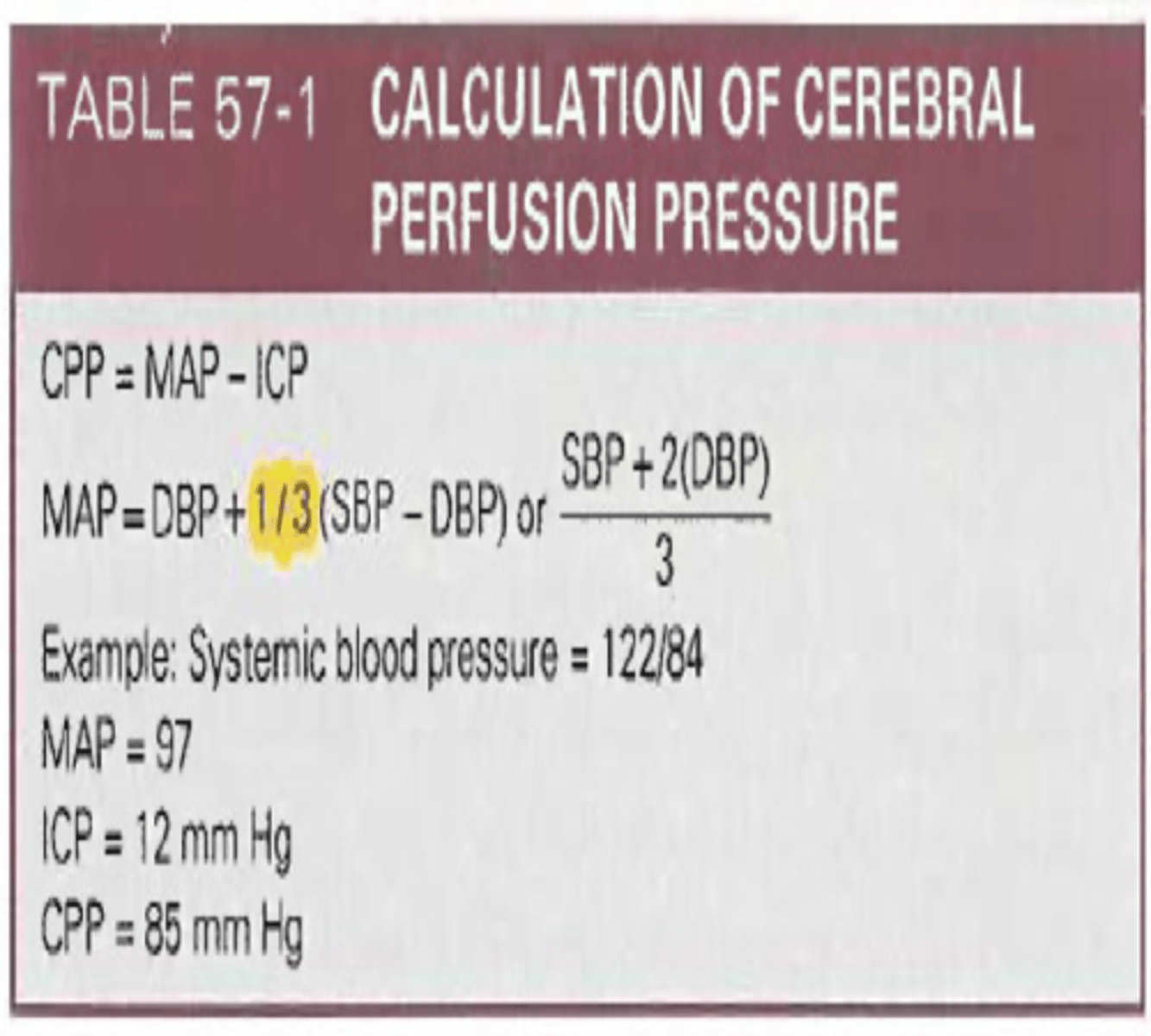
what is CPP? what is the normal value?
-the pressure needed to ensure blood flow to the brain.
-normal: 60-100 mmHg (MAP-ICP)
-CPP < 50 indicates ischemia and possible death
what is Cushing's triad?
vital sign changes related to increased ICP:
1) inc SBP and widening pulse pressure
2) decreased HR
3) irregular respirations
how do nurses assess for increased ICP? (clinical manifestations?)
-earliest sign is decreased LOC
-Cushing's triad
-ocular signs (cranial nerve III, brainstem reflexes)
-dilation of the pupils
-decline in motor function
-headache (often improves when sitting up)
-vomiting (projectile)
-posturing signs: decorticate (cortex of brain not communicating; fists clenched, arms flexed inward); decerebrate (midbrain/brain stem injury: arms extended down, fists faced away)
how is ICP measured/monitored?
-ventriculostomy → specialized catheter is inserted & coupled to external transducer
-device can also drain CSF to reduce pressure
what is the nursing care/treatment for increased ICP?
-maintenance of a patent airway**→ adequate oxygenation, ABGs, possible ventilation (to keep PaO2 at 100 mmHg)
-drug therapy (next card)
-nutritional therapy: patient is in hypermetabolic and hypercatabolic state; increased need for glucose, want to keep patient normovolemic
-frequent neurological assessments (Glasgow Coma Scale, cranial nerves, pupil evaluation, motor and sensory testing)
-positioning: increase head of bed (dec pressure/improve venous return), maintain good body alignment, turn q 2 hours
what are the drugs used to treat increased ICP?
-Mannitol (osmotic diuretic): reduces fluid volume
-hypertonic saline (3%): reduces edema by pulling fluid out of brain cells
-corticosteroids (dexamethasone/decadron): decrease inflammation
-barbiturates ("-barbital"): reduces cerebral metabolic demands and cerebral blood volume, sedates them/keeps them calm
-acetaminophen: fever reducer
-anti-seizure drugs: high ICP irritates brain and increases seizure risk
-stool softeners: prevent constipation to reduce abdominal pressure
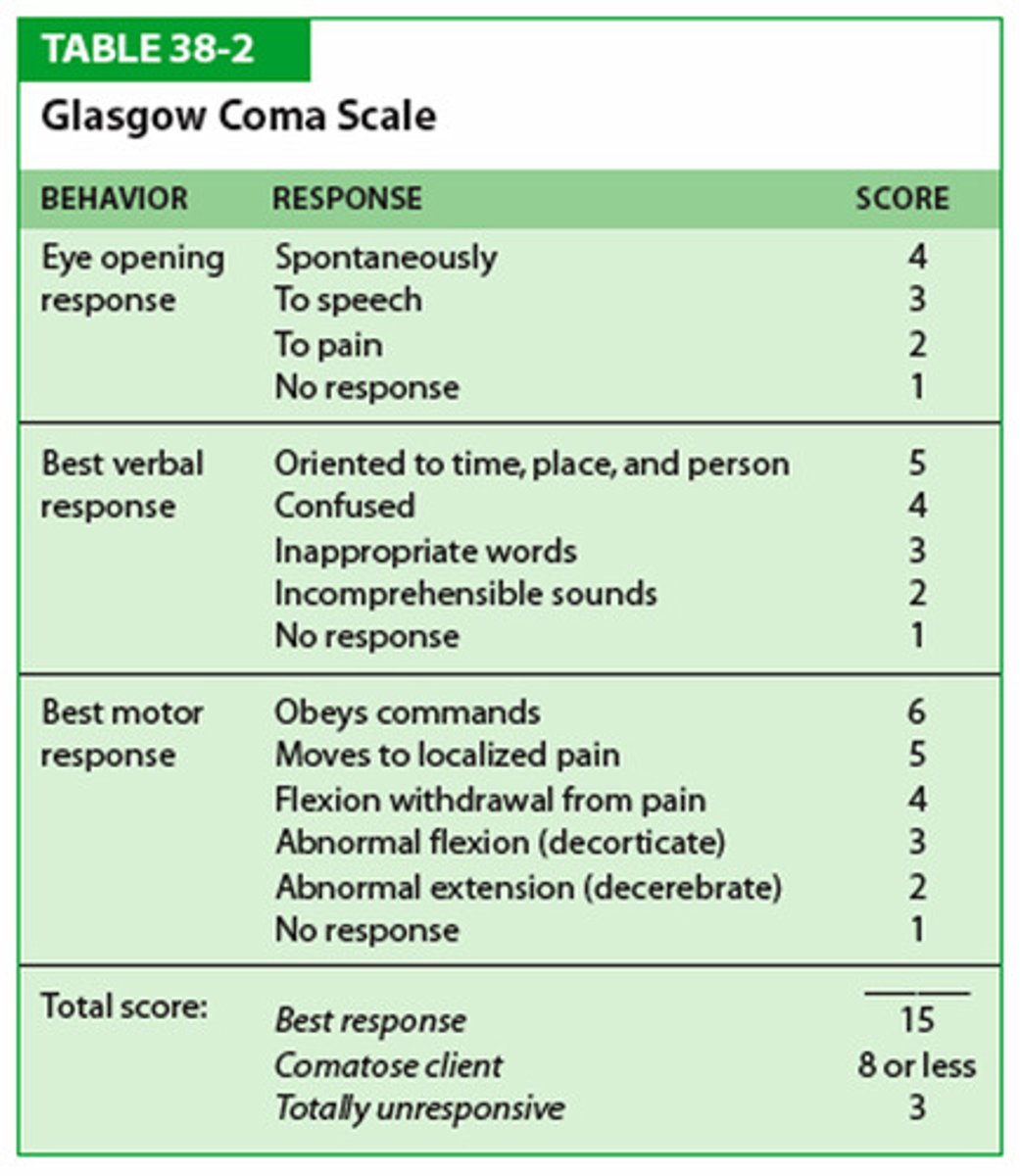
what is the Glasgow Coma Scale (GCS)?
-assessment tool measuring degree of impaired consciousness
-used in primary evaluation of traumatic brain injury
-looks at eye opening response, verbal response, and motor response
-the higher the score, the better (15 max)
what do Battle's sign, raccoon eyes, and halo sign indicate?
location of skull fracture alters the presentation of manifestations:
-Battle's sign: fracture to the temporal, parietal, or basilar region
-raccoon eyes: basilar or facial fracture
-halo sign: rhinorrhea/otorrhea produces ring of white/yellow around it → indicates drainage is CSF
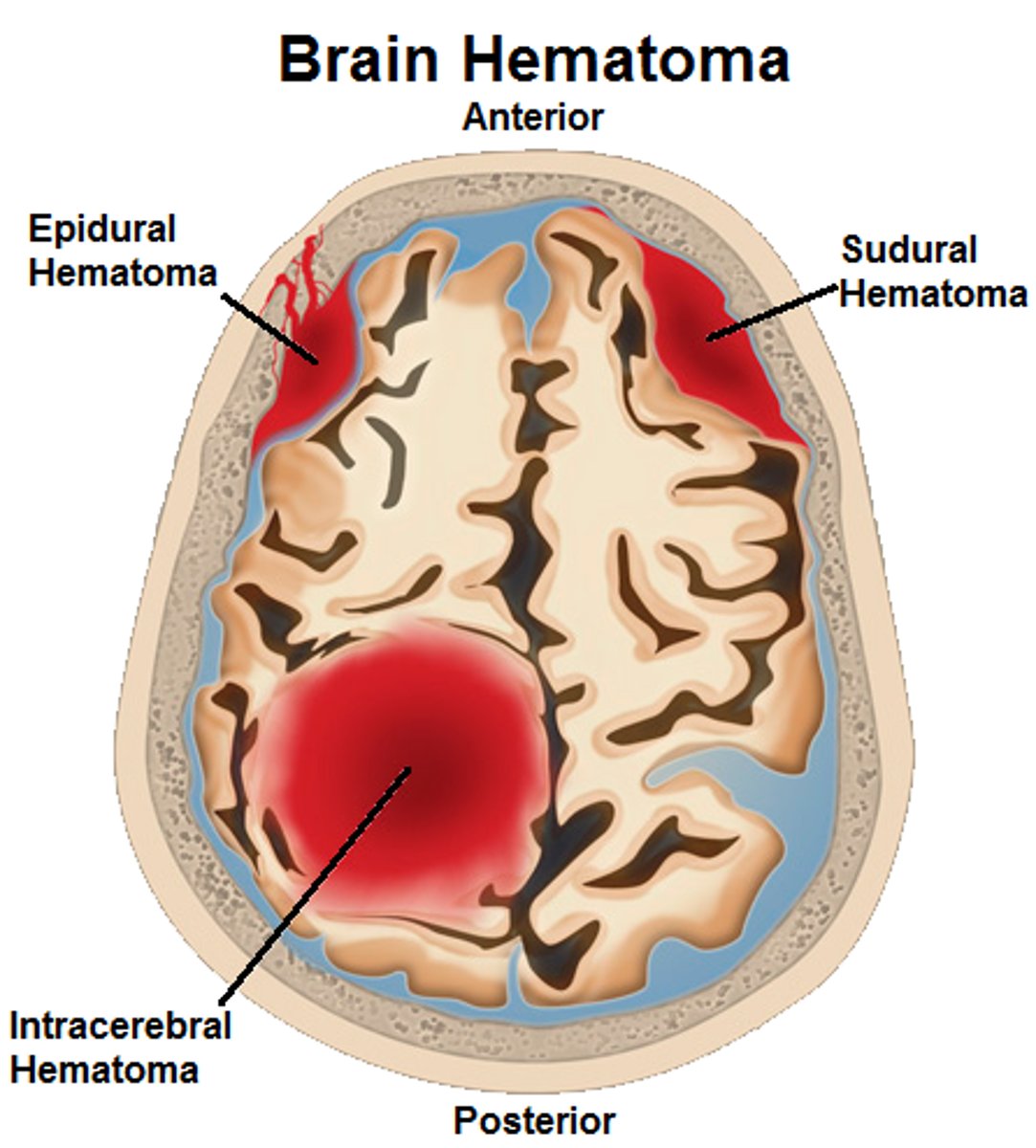
what is an epidural hematoma?
-bleeding between the dura and inner surface of the skull
-neurologic emergency
-usually arterial origin, resulting in very rapid bleeds
-classic signs: immediate loss of consciousness followed by lucid intervals; HA, nausea, vomiting; rapid deterioration
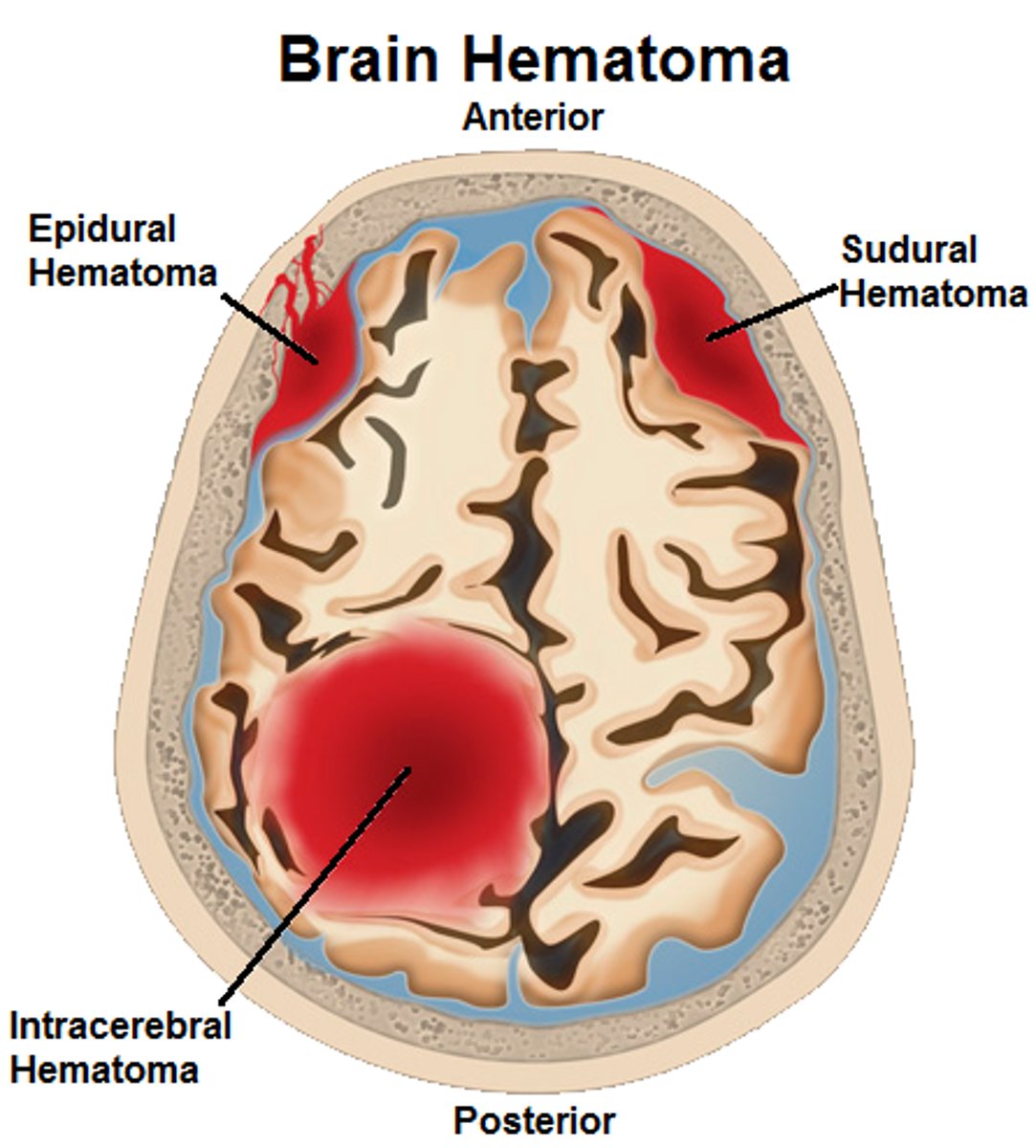
what is a subdural hematoma?
-bleeding between the dura and arachnoid layers
-usually venous in origin; slower appearance, develop mass large enough to produce symptoms
-elderly (medications, falls, veins more prone to injury) and alcoholics at increased risk
what is diffuse axonal injury? what is the result? what is the tx?
-twisting, shearing, rotational forces cause injury/tearing of axons and death of the neuron
-presence of petechiae (microhemorrhages) throughout the brain
-usually causes coma; disrupts normal brain communication and chemical processes → severe impairments
-tx: alleviate swelling/edema, control high ICP
what abnormal findings confirm meningitis?
-meningeal signs: Kernig's (lifting knee induces severe back pain), Brudzinski's (lifting head off pillow causes flexion of hip and knees)
-key signs: fever, severe headache, nausea, vomiting, photophobia and nuchal rigidity
-signs related to inflammation of the meninges
what test is performed for suspected meningitis?
-when patient presents with manifestations suggestive of bacterial meningitis → CT scan and a blood culture should be done
-diagnosis is usually verified by performing a lumbar puncture with analysis of the CSF (most definitive; cloudy, bloody, proteins, WBCs present; unable to perform if ICP is elevated)
what is the nursing care for patients with meningitis?
acute interventions:
-IV antibiotics (AFTER culture; bacterial meningitis)
-pain relief: positioning, analgesics (codeine)
-Tylenol to reduce fever
-photophobia: dark environment
-seizure precautions
-droplet precautions (airborne spread; private room, surgical mask)
-IVF
health promotion:
-vaccinations
-treatment of respiratory and ear infections
what is the nursing care for patients with encephalitis?
-symptomatic and supportive care; initial stages often require intensive care
-antivirals (herpes simplex virus), antibiotics
-fluids
-prevention: mosquito control, vaccinations
what are the risk factors for stroke:
non-modifiable
-age
-gender
-race/ethnicity
-heredity/family history
modifiable
-HTN (single most important modifiable risk factor)
-heart disease
-diabetes mellitus
-smoking
-obesity
-sleep apnea
-physical inactivity
-drug/alcohol abuse
-poor diet
what is an ischemic stroke and what are the types?
-87% of all strokes
-results from inadequate blood flow to the brain from partial or complete occlusion of an artery (plaques, clots)
-types: thrombotic (more common, r/t atherosclerosis of cerebral arteries) and embolic (ex: A-fib, MI), TIA (transient ischemic attack; mini-stroke, can be warning sign that larger thrombotic stroke is to come)
-symptoms are often rapid and severe
what is a hemorrhagic stroke?
-a stroke caused by bleeding into the brain tissue itself or into the subarachnoid space/ventricles (intracerebral or subarachnoid hemorrhage)
-can be torn artery or rupture of cerebral aneurysm
-main risk factor is HTN
-symptoms often have sudden onset, with progression over minutes to hours because of ongoing bleeding; "worst HA of life," altered LOC, vomiting, seizures
what are the clinical manifestations of stroke?
-motor/sensory changes: impaired mobility, respiratory function, swallowing and speech, gag reflex, and self-care abilities
-communication: aphasia, dysphasia, dysarthria
-personality/affect: difficulty controlling emotions, memory and judgement impaired
-intellectual function
-spatial-perceptual alterations
-bowel/bladder elimination
what does the acronym BEFAST stand for?
signs of stroke:
-balance: watch for sudden loss of balance
-eyes: check for vision loss
-face: look for an uneven smile
-arm: check if one arm is weak
-speech: listen for slurred speech
-time: call 911 right away
which diagnostics are used to confirm stroke?
MRI, non-contrast CT scan** (immediate; time = brain); indicate the size and location of the lesion and can differentiate between ischemic and hemorrhagic stroke
what are the preventive therapy measures for stroke?
-management of modifiable risk factors: healthy diet, weight control, regular exercise, no smoking, preventing or controlling hypertension, limiting alcohol consumption, and routine health assessments
-preventing clot formation: antiplatelet drugs, warfarin
-surgical interventions: carotid endarterectomy (plaque removal in carotids), stents
what is included in the emergency assessment of stroke?
-past medical history, current medications, family history
-neuro exam: altered LOC, motor/sensory/reflexes, weakness/numbness/paralysis, severe HA, unequal pupils, vertigo, seizures
-speech, swallow, or visual disturbances
-BP/HR/respiratory changes
-bladder incontinence, constipation
-nausea and vomiting
what deficits would likely be seen with a right-sided stroke?
-problems in spatial-perceptual orientation: agnosia (inability to interpret sensations and recognize things), apraxia (unable to perform tasks or movements when asked), unilateral neglect (difficulties in attending to stimuli in the left perceptual hemifield)
-left hemiplegia
-impaired judgement, impulsive
-impaired time concepts
-rapid performance, short attention span, impatient
-deny/minimize problems
what deficits would likely be seen with a left-sided stroke?
-right hemiplegia
-impaired speech/language (receptive/expressive aphasia)
-slow performance, cautious
-aware of deficits: depression, anxiety
-impaired comprehension related to language/math
-respond best to non-verbal (visual) cues
what are the emergency treatments for ischemic strokes?
-managing the airway, breathing, and circulation
-elevated BP is common immediately after a stroke; may be protective response to maintain cerebral perfusion
-baseline neurologic assessment; monitor closely for inc neurologic deficits/ICP
-careful fluid and electrolyte balance: maintain hydration to promote perfusion
-single most important point in the patient's history is the time of onset (determines eligibility for tPA)
-surgical interventions: endovascular clot retrieval
what medications are used for acute care of ischemic strokes?
-aspirin within 24-48 hours of stroke (reduces platelet aggregation)
-platelet inhibitors (Plavix) and anticoagulants (Heparin, Warfarin)
-tPA: clot buster; must be administered within 3 - 4.5 hours of the onset of clinical signs
what are the emergency treatments for hemorrhagic strokes?
-goals for managing airway, breathing, circulation, and intracranial pressure are the same as for ischemic stroke
-surgical: resection, clipping/coiling of aneurysm, evacuation of hematomas
-seizure prophylaxis
-drug therapy to manage HTN (beta blockers) and reduce incidence of cerebral vasospasms (calcium-channel blockers
"-dipine")