45. Respiratory System I
1/141
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
142 Terms
What does the respiratory system consist of?
N
N
S
N
L
T
B
B
A
A
nostrils
nasal cavity
sinuses
nasopharynx
larynx
trachea
bronchi
bronchioles
alveolar ducts
alveoli
What aids in breathing?
diaphragm and intercostal muscles
What is the primary organ of the respiratory system?
the lung
What is the function of the lung?
facilitate O2 and CO2 exchange
What composes the conducting component of the respiratory system?
N
N
P
N
L
T
B
nostrils
nasal cavity
paranasal sinuses
nasopharynx
larynx
trachea
bronchi
What is the conducting component of the respiratory system largely lined by?
pseudo-stratified, ciliated columnar cells
The conducting component has a variable proportion of what?
secretory goblet (mucous) cells
What branches from the bronchi?
bronchioles
serve as a transition zone between the conducting component (ciliated) and the air exchange (alveolar) component
transitional component
Disappearance of cilia in the transitional component is ________ ________. The ciliated cells in the proximal bronchiolar region become ________ and progressively ________, until cilia eventually ________.
not abrupt; scarce; attenuated; disappear
What do normal bronchioles lack? What do they have?
goblet cells; other types of secretory cells such as club cells (aka Clara cells) and neuroendocrine cells
Club cells contain numerous biosynthetic organelles that play an active role in what?
the detoxification of xenobiotics (foreign substances)
Clubs cells act as ________ cells in the ________ and ________ of the respiratory system.
stem; repair; remodeling
Club cells contribute to the ________ immunity of the lung by secreting ________ ________ (________) and ________ ________.
innate; protective proteins (collectins); pulmonary surfactant
What is the air exchange component of the respiratory system in all mammals formed by?
alveoli
What is the surface of the alveoli lined by?
type I and type II pneumonocytes
type of epithelial cell that covers the majority of the alveolar wall and functions in gas exchange
type I (membranous) pneumonocytes
type of epithelial cell that is larger cuboidal cells and produces surfactant
type II (granular) pneumonocytes
supports both the alveolar epithelium and alveolar capillary endothelium
interstitium
What is the blood air barrier formed from?
V
B
A
vascular endothelium
basement membrane
alveolar epithelium lining cells
The alveolar walls are a ________ ________ ________.
thin delicate network
interconnecting network of interstitial stromal tissue supporting the blood and lymphatic vessels, nerves, bronchi, bronchioles. and alveoli
pulmonary interstitium
Into what compartments can the pulmonary interstitium be divided into?
B
I
A
bronchovascular interstitium
interlobular interstitium
alveolar interstitium
compartment of pulmonary interstitium where the main bronchi and pulmonary vessels are situated
bronchovascular interstitium
compartment of pulmonary interstitium separating the pulmonary lobules and supporting small blood and lymph vessels
interlobular interstitium
compartment of pulmonary interstitium supporting the alveolar walls that contain pulmonary capillaries and alveolar epithelial cells
alveolar interstitium
True or false: Pulmonary changes (edema, emphysema, and inflammation) may affect one or more of these interstitial compartments.
true
In all domestic species, what is the left lung composed of?
cranial and caudal lobes
Depending on species, what can the right lung be composed of?
cranial, middle, caudal, and accessory lobes
In what species is the right lung missing the middle lobe?
horses
What is each pulmonary lobe further subdivided by connective tissue into?
pulmonary lobules
What does the degree of lobulation determine?
the degree of air movement between the lobules
How is movement of air between the lobules in pigs and cattle described? Why?
practically absent; thick connective tissue of the interlobular septa separating individual lobules
movement of air between lobules and between adjacent alveoli
collateral ventilation
Collateral ventilation is poor in what species? It is good in what species?
cattle; dogs
single layer of mesothelial cells overlying multiple layers of connective tissue
pleurae
What lines the thoracic wall, diaphragm, and mediastinum?
parietal pleura
What lines the surface of the lungs?
visceral pleura
True or false: Between the parietal and visceral pleura is the pleural space separated by the mediastinum into left and right sides. The pleural space is minimal and under normal conditions contains only traces of clear fluid, which is a lubricant, and a few exfoliated cells.
true
In what species is the mediastinum complete? What does this mean?
cattle, goats, and pigs; no communication between the two sides
In what species are there fenestrations in the mediastinum? What does this allow?
horses and sheep; communication between these two spaces
True or false: In cats and dogs, whether the mediastinum is fenestrated or complete is controversial.
true
The microbiota (normal flora) of the respiratory system helps to do what?
prevent colonization of harmful bacteria (colonization resistance)
What is the resident microbiota present in the respiratory system of any healthy animal?
V
B
Y
F
viruses
bacteria
yeasts
fungi
The number of organisms in microbiota are more abundant in what parts of the respiratory system?
N
P
L
nasal cavity
pharynx
larynx
True or false: Some members of the nasal microbiota are pathogens that can cause important respiratory infections under some circumstances.
true
part of the bovine nasal flora but can cause pneumonia
mannheimia haemolytica
True or false: There are multiple routes to access the respiratory system. Inflammation can extend locally, regionally, or systemically. Laryngeal exudate from laryngitis can be aspirated to lungs. The large vascular bed present in the lung can allow for sepsis and septic shock.
true
What are the portals of entry into the respiratory system?
A
H
D
aerogenous
hematogenous
direct extension
True or false: Hematogenous dissemination of bacteria to this serosal surface occurs commonly, often as a component of polyserositis.
true
True or false: Microbes and foreign bodies may gain access to the pleura via direct extension through the thoracic body wall in association with penetrating thoracic injury (bites, gunshot wounds, and migrating grass awns). It can include rupture of the caudal esophagus, perforation of the diaphragm, and parapneumonic spread of infectious agents as a sequela of bronchopneumonia or when a lung abscess ruptures into the pleural space.
true
What is the defense system/barrier of the conducting and transitional components of the respiratory system?
mucociliary clearance
What is the defense system/barrier of the air exchange component of the respiratory system?
phagocytosis from pulmonary alveolar macrophages
physical unidirectional movement and removal of deposited particles and gases dissolved in the mucus
mucociliary clearance
What is mucociliary clearance provided by?
mucociliary blanket (mucociliary escalator)
What is the main defense mechanism of the conducting component (nasal cavity, trachea, and bronchi)?
mucociliary clearance
What does mucus primarily act as?
barrier and vehicle
What is mucus made up of?
W
G
I
L
E
water
glycoproteins
immunoglobulins
lipids
electrolytes
What is mucus produced by?
goblet cells, submucosal glands, and fluid from transepithelial ion and water transport
Where is serous fluid and mucus secreted? What is formed on top of cells?
onto the surface of the respiratory mucosa; a thin film of mucus
True or false: Rapid and powerful movement of cilia creates a series of synchronized waves that propels mucus, exfoliated cells, and entrapped particles to the pharynx.
true
Where does mucociliary clearance terminate at? What happens there?
the pharynx; mucus can be coughed
What will ciliary activity and mucus transport increase notably in response to?
stimuli such as in respiratory infections
Is the mucociliary apparatus available in the alveoli? Why or why not?
no; they lack ciliated and mucus-producing cells
What are the main defense mechanisms of the alveoli?
P
A
phagocytosis provided by the pulmonary alveolar macrophages
antimicrobial molecules of the alveolar lining fluid
Pulmonary alveolar macrophages are highly ________ cells.
phagocytic
How do pulmonary alveolar macrophages contribute to the immune system?
rapidly attaching and phagocytosing bacteria and any other particles reaching the alveolar lumens
What is the number of free macrophages in the alveolar space closely related to?
the number of inhaled particles reaching the lungs
True or false: This ability to increase, within hours, the number of available phagocytic cells is vital in protecting the distal lungs against foreign material, particularly when the inhaled particle load is high.
true
The lifespan of alveolar macrophages in the alveoli is notably ________, only a few ________. They are ________ being replaced by newly migrated blood ________.
short; days; continuously; monocytes
How do most alveolar macrophages leave the alveoli?
by migrating toward the bronchiolar (transitional) region until the mucociliary blanket is reached (via mucociliary apparatus to the pharynx)
What happens if the deposition of inhaled mineral dust exceeds removal?
particles accumulate in the lung
What is pneumoconiosis lung disease caused by?
deposition of dust
common finding in the lungs of dogs, particularly in animals living in polluted areas or households with smokers or fireplaces
carbon (anthracosis)
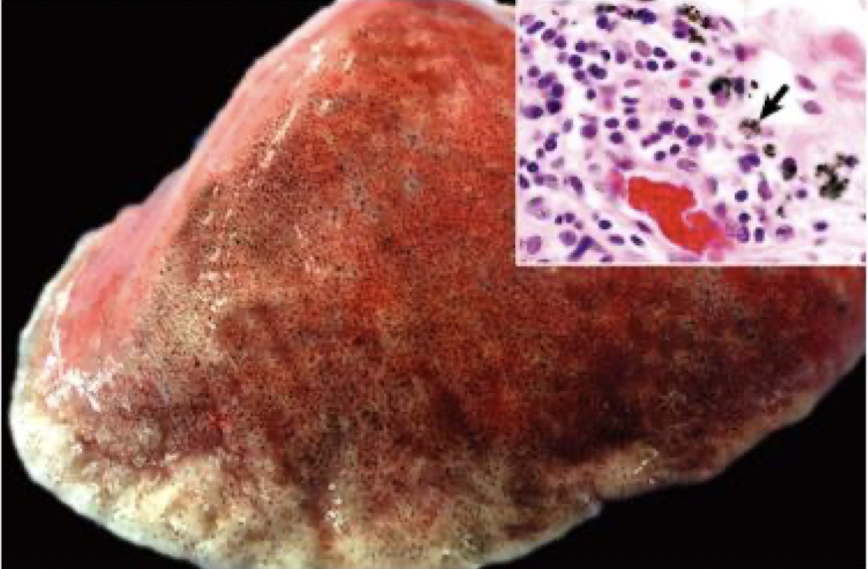
What is this showing?
anthracosis
particle, microbe, or toxic gas must first gain entry to a vulnerable region of the respiratory system before it can induce an effect
aerogenous
process by which particles of various sizes and shapes are trapped within specific regions of the respiratory system
deposition
process by which deposited particles are destroyed, neutralized, or removed from the mucosal surfaces
clearance
What are the main clearance mechanisms?
S
C
M
P
sneezing
coughing
mucociliary transport
phagocytosis
What is the underlying pathogenic mechanism in many pulmonary diseases?
abnormal retention of particles resulting from increased deposition, decreased clearance, or a combination of both
True or false: Anatomic configuration of the nasal cavity and bronchi plays a unique role in preventing or reducing the penetration of noxious material into the lungs.
true
What sized microbes will lodge in the nasal passage? What happens if they are smaller than this? Smaller than what size can progress to the bronchiole and alveoli?
10 um; can progress to tracheal and bronchial bifurcations; 2 um
True or false: The anatomic features of the nasal cavity and airways provide an effective barrier, preventing the penetration of most large particles into the lungs.
true
Particles longer than ________ may also reach the lower respiratory system provided their mean diameter is less than ________.
200 um; 1 um
What is an example of a large but slender fiber that can bypass the filtrating mechanisms by traveling parallel to the airstream?
asbestos
Lungs are also susceptible to hematogenous borne microbes, toxins, or emboli why?
large vascular bed
cell responsible for the removal of circulating particles, bacteria, and endotoxins from the blood of ruminants, cats, pigs, and horses
pulmonary intravascular macrophage
In pigs, what percent of the pulmonary capillary surface is lined by pulmonary intravascular macrophages? What about ruminants?
16%; 95%
In systemic conditions, excessive release of ________ by pulmonary intravascular macrophages may result in ________ lung injury.
cytokines; acute
True or false: Existing in an oxygen-rich environment and being the site of numerous metabolic reactions means the lungs require an efficient defense mechanism against oxidant-induced cellular damage (oxidative stress).
true
What are forms of damage caused by?
I
X
F
inhaled oxidant gases
xenobiotic toxic metabolites
free radicals released by phagocytic cells during inflammation
________ ________ and ________ ________ ________ (____) induce extensive pulmonary injury and impair repair.
free radicals; reactive oxygen species (ROS)
largely responsible for protecting pulmonary cells against damage
oxygen and free radical scavengers
What are examples of oxygen and free radical scavengers?
S
V
superoxide dismutase
vitamins E and C
Where are the scavengers present?
alveolar and bronchiolar epithelial cells and interstitium
True or false: Respiratory defense mechanisms are effective in trapping, destroying, and removing bacteria that, under normal conditions, animals can be exposed to aerosols containing massive numbers of bacteria without any ill effects. If defense mechanisms are impaired, the inhaled bacteria will colonize and multiply in bronchi, bronchioles, and alveoli, and they produce infection, which can result in fatal pneumonia. Blood borne pathogens, inhaled toxicants, or free radicals overwhelm the protective defense mechanisms, cells of the respiratory system are likely to be injured, often causing serious respiratory diseases.
true
There is ________ of viral and bacterial infections.
synergy
How long after a viral infection will the phagocytic function of pulmonary alveolar macrophages and the mucociliary clearance be impaired?
5-7 days
What viruses are known to predispose to secondary bacterial infections?
I
B
C
F
influenza virus in pigs and horses
bovine respiratory syncytial virus (BRSV) in cattle
canine distemper virus
felid herpesvirus 1 (FeHV-1) and feline calicivirus (FV)
True or false: Acquired or congenital immunodeficiencies can cause increased susceptibility to viral, bacterial, mycotic, and protozoal pneumonias, as can corticosteroids/chemotherapeutic drugs with immunosuppressive characteristics.
true