Basic of Immunology
1/94
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
95 Terms
What is immunity?
Immunity, also called resistance, is the ability to ward off disease caused by microbes or their products and to protect against environmental agents such as pollen, chemicals, and animal dander.
What is lack of immunity referred to as?
Susceptibility
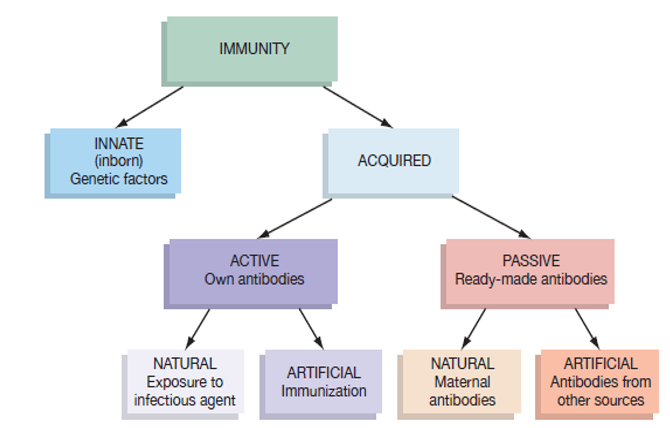
Differentiate between innate and acquired immunity.
Innate immunity is non-specific and does not involve the production of antibodies, while acquired immunity is specific and involves the production of antibodies after exposure to antigens.
What are antigens?
Antigens are foreign substances that provoke an immune response, leading to the production of antibodies. They are typically proteins or large polysaccharides.
Explain the roles of B cells in humoral immunity.
B cells are responsible for producing antibodies in response to specific antigens. They undergo clonal expansion and differentiate into plasma cells that synthesize antibodies.
Compare the primary and secondary responses of the adaptive immune system.
The primary response occurs when the immune system first encounters an antigen, leading to slower antibody production. The secondary response, facilitated by memory cells, is faster and more robust due to prior exposure.
What are the two main types of immunity?
The two main types of immunity are innate (non-specific) immunity and acquired (specific) immunity.
Describe innate immunity.
Innate immunity is a non-specific defense mechanism that includes physical barriers (like skin and mucous membranes) and chemical barriers (like saliva and gastric juices) that protect the body from pathogens.
Compare active and passive immunity.
Active immunity involves the body's own immune response to an antigen, leading to the production of antibodies (e.g., from infection or vaccination), while passive immunity involves the transfer of antibodies from another source (e.g., mother to infant through breast milk).
What is acquired immunity and how does it differ from innate immunity?
Acquired immunity is a specific defense mechanism that develops over time through exposure to pathogens, involving the production of antibodies and memory cells, while innate immunity is a non-specific, immediate response that does not involve memory.
What are the forms of acquired immunity?
Acquired immunity can be naturally acquired (through infection or maternal antibodies) or artificially acquired (through vaccination or antibody injection). It can further be classified as active (body produces antibodies) or passive (antibodies are transferred).
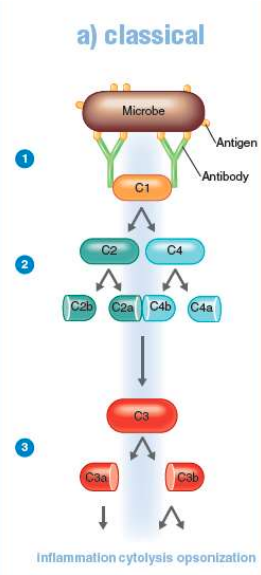
What is the complement system?
The complement system is a series of over 30 proteins produced by the liver that enhance immune functions through cytolysis, opsonization, and inflammation, aiding in the destruction of microbes.
Describe the classical pathway of complement activation.
The classical pathway is initiated when antibodies bind to antigens, forming antigen-antibody complexes that activate C1, which then activates C2 and C4, ultimately leading to the activation of C3, resulting in inflammation and opsonization.
What are the main outcomes of complement activation?
The activation of complement proteins leads to three main outcomes: cytolysis (via the membrane attack complex), opsonization (enhancing phagocytosis), and inflammation (through the release of inflammatory mediators).
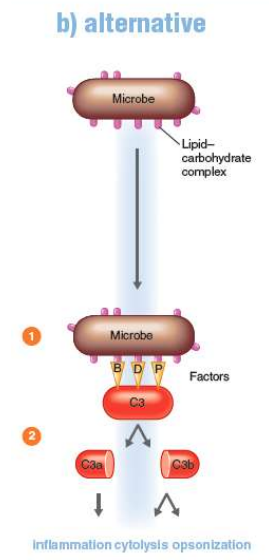
Compare the alternative pathway and the classical pathway of complement activation
The alternative pathway does not require antibodies and is activated by C3 binding directly to microbial surfaces, while the classical pathway requires antibody-antigen complexes to initiate the activation process.
What role do activated fragments C3a and C3b play in the complement system?
C3a is involved in promoting inflammation, while C3b enhances opsonization, marking pathogens for destruction by phagocytes and contributing to cytolysis.
What is the structure of a typical antibody (immunoglobulin)?
A typical antibody (immunoglobulin) has a Y-shaped structure composed of four protein chains:two identical light chains and two identical heavy chains, joined by disulfide links. The ends of the Y arms are the variable (V) regions that bind to specific epitopes on antigens, while the lower parts are constant (C) regions, which are the same for a particular class of immunoglobulin.
Compare the five classes of immunoglobulins (IgG, IgM, IgA, IgD, IgE) in terms of structure and function.
IgG and IgE are Y-shaped monomers, while IgM is a pentamer and IgA can be a dimer. IgG is the most abundant in serum and provides long-term immunity; IgM is the first produced during an immune response; IgA is found in mucosal areas; IgD is involved in B cell activation; and IgE is associated with allergic reactions and protection against parasites.
What are the mechanisms by which antibodies protect the host after binding to antigens?
Antibodies protect the host through mechanisms such as agglutination, opsonization, neutralization, and antibody-dependent cell-mediated cytotoxicity. These processes enhance phagocytosis, block pathogen attachment, and activate the complement system, leading to inflammation and cell lysis.
Describe the relationship between B cells and antibodies in the immune response.
B cells produce antibodies in response to specific antigens. Upon encountering an antigen, B cells bind to it via their surface immunoglobulins, become activated, and proliferate into plasma cells that secrete large amounts of antibodies, which then target and neutralize the antigens.
What role do the variable and constant regions of antibodies play in their function?
The variable (V) regions of antibodies determine the specificity for binding to unique epitopes on antigens, enabling precise targeting. The constant (C) regions dictate the antibody's class and function, influencing how the immune response is activated and how the antibody interacts with other immune components.
What is the process of phagocytosis?
Phagocytosis involves four main phases:1) Chemotaxis - chemical attraction of phagocytes to microorganisms. 2) Adherence - phagocyte attachment to the microorganism. 3) Ingestion - engulfing the microorganism by extending pseudopods to form a phagosome. 4) Digestion - fusion of the phagosome with a lysosome to form a phagolysosome, where the pathogen is digested.
Compare the roles of neutrophils and macrophages in the immune response
Neutrophils are the first responders to microbial infection, active in the early stages and highly phagocytic. Macrophages, derived from monocytes, are present later and play a role in both phagocytosis and activating T cells, thus bridging innate and adaptive immunity.
Define chemotaxis in the context of phagocytosis.
Chemotaxis is the process where phagocytes are attracted to microorganisms through chemical signals, such as microbial products, cytokines from other white blood cells, and components of damaged tissues.
What are the phases of inflammation and their significance in the immune response?
The phases of inflammation include: 1) Vasodilation and increased permeability, allowing immune cells and proteins to reach the affected area. 2) Phagocyte migration, where phagocytes adhere to the endothelium and move to the site of injury. 3) Tissue repair, where damaged tissues are replaced or repaired. These phases help to contain and eliminate pathogens while facilitating healing.
What is the role of Toll-like receptors (TLRs) in the immune system?
Toll-like receptors (TLRs) are receptors on phagocytes that recognize pathogen-associated molecular patterns (PAMPs) and initiate immune responses by activating signaling pathways that lead to inflammation and the recruitment of immune cells
Define cellular immunity.
Cellular immunity, also known as cell-mediated immunity, is a type of immune response that involves T lymphocytes (T cells) which recognize and respond to antigens presented by antigen-presenting cells (APCs). This process primarily targets intracellular pathogens, such as viruses and certain bacteria.
What are the main types of T cells and their functions?
The main types of T cells include: 1. Helper T cells (CD4+):Activate other immune cells and enhance the immune response. 2. Cytotoxic T cells (CD8+):Kill infected or cancerous cells. 3. Suppressor T cells: Regulate and suppress immune responses to maintain homeostasis.
How do helper T cells (Th) activate macrophages?
Helper T cells (CD4+) activate macrophages by recognizing antigen fragments presented on MHC class II molecules. The interaction requires a second signal, the co-stimulatory signal from the APC, leading to enhanced phagocytosis and antigen presentation capabilities of the macrophage.
Compare the recognition mechanisms of helper T cells and cytotoxic T cells.
Helper T cells (CD4+) recognize antigens presented by MHC class II molecules on APCs, while cytotoxic T cells (CD8+) recognize antigens presented by MHC class I molecules on infected or cancerous cells. This distinction is crucial for their respective functions in immune response.
Describe the activation process of T cells.
The activation of T cells involves two signals:1. Recognition of the specific antigen presented on an MHC molecule by the T cell receptor (TCR). 2. A second co-stimulatory signal from the APC, which is essential for full activation and proliferation of the T cell.
What is antibody?
Proteins produced by the host B-lymphocytes that neutralize or destroy the antigens
What is pathogen?
•Organism capable of causing disease
Types of immunity
What type of immunity involves host defense that does not depend on antibody production?
Innate Immunity (non-specific): Host defense that does not involve the production of antibodies.
How is innate immunity acquired?
Acquired genetically or inborn.
What activates the responses of the innate immune system?
Responses of the innate system are activated by protein receptors in the plasma membranes of defensive cells.
What are Toll-like receptors (TLRs)?
Responses of the innate system are activated by protein receptors in the plasma membranes of defensive cells. Among these activators are Toll-like receptors (TLRs).
What do TLRs attach to?
TLRs attach to various components commonly found on pathogens that are called pathogen-associated molecular patterns (PAMPs).
What are some examples of PAMPs recognized by TLRs?
Examples include the lipopolysaccharide (LPS) of the outer membrane of gram-negative bacteria, the flagellin in the flagella of motile bacteria, the peptidoglycan in the cell wall of gram-positive bacteria, the DNA of bacteria, and the DNA and RNA of viruses.
What type of immunity involves host defense that includes antibody production?
Acquired/ Adaptive Immunity: Host defense involving the production of antibodies.
How does adaptive immunity develop?
Develops with exposure.
What is the term for the first time the adaptive immune system encounters a specific foreign substance?
The first time the adaptive immune system meets and combats a particular foreign substance is called the primary response.
What happens during later interactions with the same antigen in adaptive immunity?
Later interactions with that same cell or substance will cause a secondary response, which will be faster and more effective as a result of a “memory” of the first infection.
What is a key exclusive feature of the adaptive immune system?
The memory component is important and exclusive to the adaptive immune system.
What is another important ability of the adaptive immune system related to recognizing cells?
Another important element of the adaptive immune system is its ability to differentiate between normal “self ” cells and “nonself.”
First line defenses
SeconFirst-line defenses keep pathogens on the outside or neutralize them before infection begins. The skin, mucous membranes, and certain antimicrobial substances are part of these defenses.
Second-line defenses
Second-line defenses slow or contain infections when first-line defenses fail. They include proteins that produce inflammation, fever that enhances cytokine activity, and phagocytes and NK cells, which attack and destroy cancer cells and virus-infected cells.
Third-line defenses
Third-line defenses include lymphocytes, that target specific pathogens for destruction when the second-line defenses don’t contain infections. It includes a memory component that allows the body to more effectively respond to that same pathogen in the future.
Physical and chemical barriers of first line of defense
1. Physical barriers
•Skin
•Mucous membranes
2. Chemical barriers
•Sebum
•Saliva
•Mucus
•Gastric juices
Mechanism of innate immunity
-Host defense that does not involve the production of antibodies.
-Acquired genetically or inborn
-Responses of the innate system are activated by protein receptors in the plasma membranes of defensive cells. Among these activators are Toll-like receptors (TLRs).
-These TLRs attach to various components commonly found on pathogens that are called pathogen-associated molecular patterns (PAMPs).
Examples include the lipopolysaccharide (LPS) of the outer membrane of gram-negative bacteria, the flagellin in the flagella of motile bacteria, the peptidoglycan in the cell wall of gram-positive bacteria, the DNA of bacteria, and the DNA and RNA of viruses.
What happens the first and second exposure in adaptive immune system?
The first time the adaptive immune system meets and combats a particular foreign substance is called the primary response. Later interactions with that same cell or substance will cause a secondary response, which will be faster and more effective as a result of a “memory” of the first infection. This memory component is important and exclusive to the adaptive immune system.
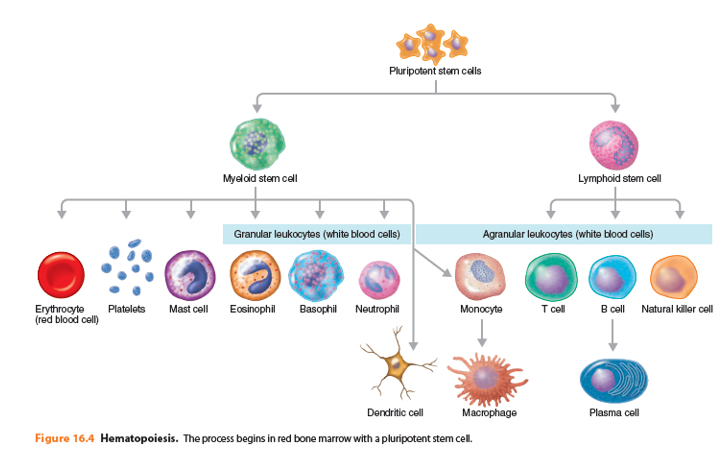
Granulocytes
Eosinophil, neutrophil, basophil
Agraulocytes
Monocyte (dendritic cell, macrophage)
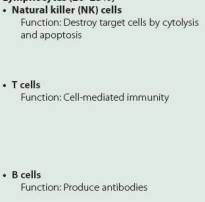
Lymphocyte (NK cell, T cell, B cell)
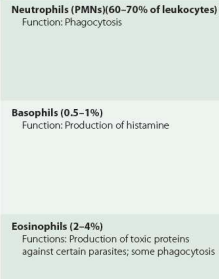
Function of neutrophils
highly phagocytic and motile, are active in the initial stages of an infection
Function of basophil
Basophils release substances, such as histamine, that are important in inflammation and allergic responses.
Function of eosinophil
Eosinophils are somewhat phagocytic and also have the ability to leave the blood. Their major function is to produce toxic proteins against certain parasites, such as helminths. Although eosinophils are physically too small to ingest and destroy helminths, they can attach to the outer surface of the parasites and discharge peroxide ions that destroy them. Their number increases significantly during certain parasitic worm infections and hypersensitivity (allergy) reactions.
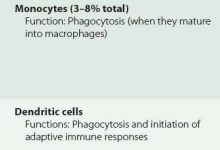
Function of monocyte
Monocytes are not actively phagocytic until they leave circulating blood, enter body tissues, and mature into macrophages. In fact, the proliferation of lymphocytes is one factor responsible for the swelling of lymph nodes during an infection.
Function of dendritic cell
Dendritic cells destroy microbes by phagocytosis and initiate adaptive immunity responses
Function of NK cells
NK cells attack any body cells that display abnormal or unusual plasma membrane proteins. The binding of NK cells to a target cell, such as an infected human cell, causes the release of vesicles containing toxic substances from NK cells. Some granules contain a protein called perforin, which inserts into the plasma membrane of the target cell and creates channels (perforations) in the membrane. As a result, extracellular fluid flows into the target cell and the cell bursts, a process called cytolysis. Other granules of NK cells release granzymes, which are protein-digesting enzymes that induce the target cell to undergo apoptosis, or self-destruction. This type of attack kills infected cells but not the microbes inside the cells; the released microbes, which may or may not be intact, can be destroyed by phagocytes.
What does perforin do?
inserts into the plasma membrane of the target cell and creates channels (perforations) in the membrane. As a result, extracellular fluid flows into the target cell and the cell bursts, a process called cytolysis.
What are granzymes and what do they do?
Granzymes are protein-digesting enzymes that induce the target cell to undergo apoptosis, or self-destruction
Functions of T cells and B cells
T cells and B cells are not usually phagocytic but play a key role in adaptive immunity. They occur in lymphoid tissues of the lymphatic system and also circulate in blood.
What is leukocytosis?
During many kinds of infections, especially bacterial infections, the total number of white blood cells increases as a protective response to combat the microbes; this increase is called leukocytosis
What is leukopenia?
salmonellosis and brucellosis, and some viral and rickettsial infections may cause a decrease in the leukocyte count, called leukopenia. Leukopenia may be related to either impaired white blood cell production or the effect of increased sensitivity of white blood cell membranes to damage by complement, antimicrobial serum proteins
Function of granulocytes
Function of agranulocytes
Function of lymphocytes
The lymphatic system
The lymphatic system consists of a fluid called lymph, vessels called lymphatic vessels, a number of structures and organs containing lymphoid tissue, and red bone marrow, where stem cells develop into blood cells, including lymphocytes. Lymphoid tissue contains large numbers of lymphocytes, including T cells, B cells, and phagocytic cells that participate in immune responses.
Lymph nodes
Lymph nodes are the sites of activation of T cells and B cells, which destroy microbes by immune responses. Also within lymph nodes are reticular fibers, which trap microbes, and macrophages and dendritic cells, which destroy microbes by phagocytosis
Lymphatic vessels
It begin as microscopic lymphatic capillaries located in spaces between cells. The lymphatic capillaries permit interstitial fluid derived from blood plasma to flow into them, but not out. Within the lymphatic capillaries, the fluid is called lymph. Lymphatic capillaries converge to form larger lymphatic vessels. These vessels, like veins, have one-way valves to keep lymph flowing in one direction only. All lymph eventually passes into the thoracic (left lymphatic) duct and right lymphatic duct and then into their respective subclavian veins, where the fluid is now called blood plasma. Lymphoid tissues and organs are scattered throughout the mucous membranes that line the gastrointestinal, respiratory, urinary, and reproductive tracts. Multiple large aggregations of lymphoid tissues are located in specific parts of the body. The spleen contains lymphocytes and macrophages that monitor the blood for microbes and secreted products such as toxins, much like lymph nodes monitor lymph. The thymus serves as a site for T cell maturation. It also contains dendritic cells and macrophages.
Phagocytosis
• Phagocytosis (from Greek words meaning eat and cell) is the ingestion of a microorganism or other substance by a cell.
• Cells that perform phagocytosis are collectively called phagocytes. All are types of white blood cells or white blood cell derivatives.
Mechanism of phagocytosis
phagocytosis can be divided into four main phases: chemotaxis, adherence, ingestion, and digestion
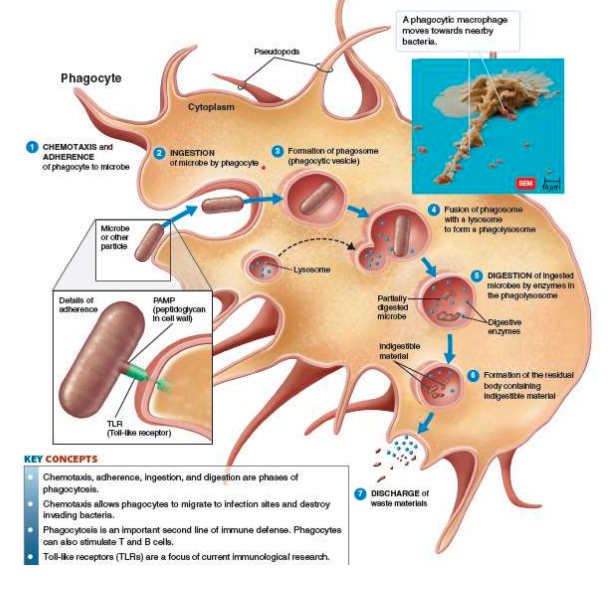
Chemotaxis and adherence
Chemotaxis is the chemical attraction of phagocytes to microorganisms. Among the chemotactic chemicals that attract phagocytes are microbial products, components of white blood cells and damaged tissue cells, cytokines released by other white blood cells, and, finally, peptides derived from complement. Adherence is the attachment of the phagocyte’s plasma membrane to the surface of the microorganism or other foreign material. Adherence is facilitated by the attachment of pathogen-associated molecular patterns (PAMPs) of microbes to receptors, such as Toll-like receptors (TLRs), on the surface of phagocytes
Ingestion
Following adherence, ingestion occurs. The plasma membrane of the phagocyte extends projections called pseudopods that engulf the microorganism. Once the microorganism is surrounded, the pseudopods meet and fuse, surrounding the microorganism with a sac called a phagosome, or phagocytic vesicle. The membrane of a phagosome has enzymes that pump protons (H+) into the phagosome, reducing the pH to about 4. At this pH, hydrolytic enzymes activate.
Digestion
On contact, the phagosome and lysosome membranes fuse to form a single, larger structure called a phagolysosome. The contents of the phagolysosome are digested in the phagolysosome. After enzymes have digested the contents of the phagolysosome brought into the cell by ingestion, the phagolysosome contains indigestible material and is called a residual body. This residual body then moves toward the cell boundary and discharges its wastes outside the cell.
Toll-like Receptors
Toll-like receptors (TLRs) are an important family of receptors that constitute the first line of defense system against microbes.
• They can recognize both the external pathogen-associated molecular patterns (PAMPs) and the internal damage-associated molecular patterns (DAMPs).
• TLR activation stimulates signaling cascades by the host as a defense mechanism against invaders and to repair the damaged tissue, leading to the release of various inflammatory cytokines and immune modulators.
• Excessive TLR activation disrupts the immune homeostasis by sustained proinflammatory cytokines and chemokine production and consequently contributes to the development and progression of many diseases.*
What is inflammation
Damage to the body’s tissues triggers a local defensive response called inflammation, another component of the second line of defense.
Signs and symptoms of inflammation
• Redness
• Pain
• Heat
• Swelling
• Loss of function
Functions of inflammation
1. To destroy the injurious agent, if possible, and to remove it and its byproducts from the body.
2. If destruction is not possible, to limit the effects on the body by confining or walling off the injurious agent and its by-products
3. To repair or replace tissue damaged by the injurious agent or its byproducts.
Types of inflammation
• Inflammation can be divided into acute and chronic inflammation.
• If the cause of an inflammation is removed in a relatively short period of time, the inflammatory response is intense and is referred to as an acute inflammation. An example is the response to a boil caused by S. aureus.
• If, instead, the cause of an inflammation is difficult or impossible to remove, the inflammatory response is longer lasting but less intense (although overall more destructive). This type of inflammation is referred to as a chronic inflammation. An example is the response to a chronic infection such as tuberculosis, caused by M. tuberculosis.
Stages of inflammation
Vasodilation and increased permeability of blood vessels
Phagocyte migration and phagocytosis
Tissue repair
Vasodilation and increased permeability of blood vessels
Vasodilation:
Vasodilation is the widening of blood vessels in the area of injury.
This allows more blood to flow to the damaged tissue.
The increased blood flow causes redness (erythema) and heat, two common signs of inflammation.
Increased Permeability:
The blood vessel walls become more permeable, meaning they allow fluids and immune cells to pass through more easily.
Defensive substances like antibodies, clotting factors, and phagocytes leave the bloodstream and enter the damaged area to fight infection and promote healing.
This movement of fluid into the tissues leads to swelling (edema).
Pain:
Inflammation can be painful due to:
Nerve damage,
Irritation by microbial toxins,
Pressure from the accumulation of fluid (edema).
Chemical Mediators:
Chemicals like histamine, kinins, prostaglandins, and leukotrienes are released by damaged cells.
These substances trigger vasodilation and increased permeability, amplifying the immune response.
Blood Clot Formation:
Clots may form around the affected area, helping to contain the infection and prevent it from spreading to other parts of the body.
Abscess Formation:
If tissue damage is extensive, dead cells and fluid may accumulate, forming a pus-filled cavity.
This localized collection of pus is called an abscess, a common result of severe infection.
Phagocyte migration and phagocytosis
Margination:
Blood flow slows down in the affected area.
In response to cytokines (chemical signals released by damaged tissues and immune cells), phagocytes begin to stick to the inner lining (endothelium) of blood vessels near the infection site.
This sticking process is called margination.
Diapedesis:
After margination, the phagocytes squeeze through the gaps between endothelial cells to exit the bloodstream.
This movement, similar to how an amoeba moves, is known as diapedesis.
It allows phagocytes to reach the damaged or infected tissue.
Phagocytosis:
Once at the site, phagocytes engulf and digest invading microorganisms such as bacteria.
This process, called phagocytosis, helps eliminate pathogens and begin the healing process.
Tissue repair
• The final stage of inflammation is tissue repair, the process by which tissues replace dead or damaged cells.
• Repair begins during the active phase of inflammation, but it cannot be completed until all harmful substances have been removed or neutralized at the site of injury.
• A tissue is repaired when its stroma or parenchyma produces new cells. The stroma is the supporting connective tissue, and the parenchyma is the functioning part of the tissue.
What is fever?
Fever is an abnormally high body temperature, typically above 37°C (98.6°F).
It is a natural response to infection, most commonly caused by bacteria, their toxins, or viruses
Role of hypothalamus in fever
The hypothalamus in the brain acts as the body’s thermostat, regulating body temperature.
Under normal conditions, it maintains the temperature around 37°C (98.6°F).
During infection, this set point is increased, leading to fever.
How fever is triggered
When phagocytes (like macrophages) ingest gram-negative bacteria, parts of the bacteria’s cell wall, called lipopolysaccharides (LPS), are released.
LPS is an endotoxin that stimulates immune cells to produce cytokines, specifically:
Interleukin-1 (IL-1)
Tumor Necrosis Factor-alpha (TNF-α)
These cytokines travel to the brain and act on the hypothalamus.
Resetting the thermostat (fever)
In response to IL-1 and TNF-α, the hypothalamus releases prostaglandins.
Prostaglandins reset the body’s thermostat to a higher temperature, causing the body to generate and retain more heat, which results in fever.
Purpose of fever
Fever can slow down the growth of some pathogens.
It also enhances immune functions, like increasing phagocyte activity and speeding up tissue repair.
The complement system
• The complement system consists of over 30 proteins produced by the liver that circulate in blood serum and within tissues throughout the body.
• The system is so named because it “completes,” or assists, cells of the immune system in destroying microbes.
• The complement system is not adaptable, never changing over a person’s lifetime. Therefore, it is considered part of the innate immune system.
• However, it can be recruited into action by the adaptive immune system. • Together, proteins of the complement system destroy microbes by cytolysis, opsonization, and inflammation.
The classical pathway
The alternative pathway
The lectin pathway
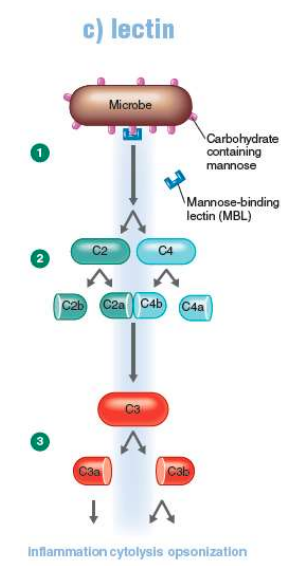
Outcomes of complement system
cytolysis, opsonization, and inflammation