Y2 S2- CARDIO
1/47
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
48 Terms
label the following
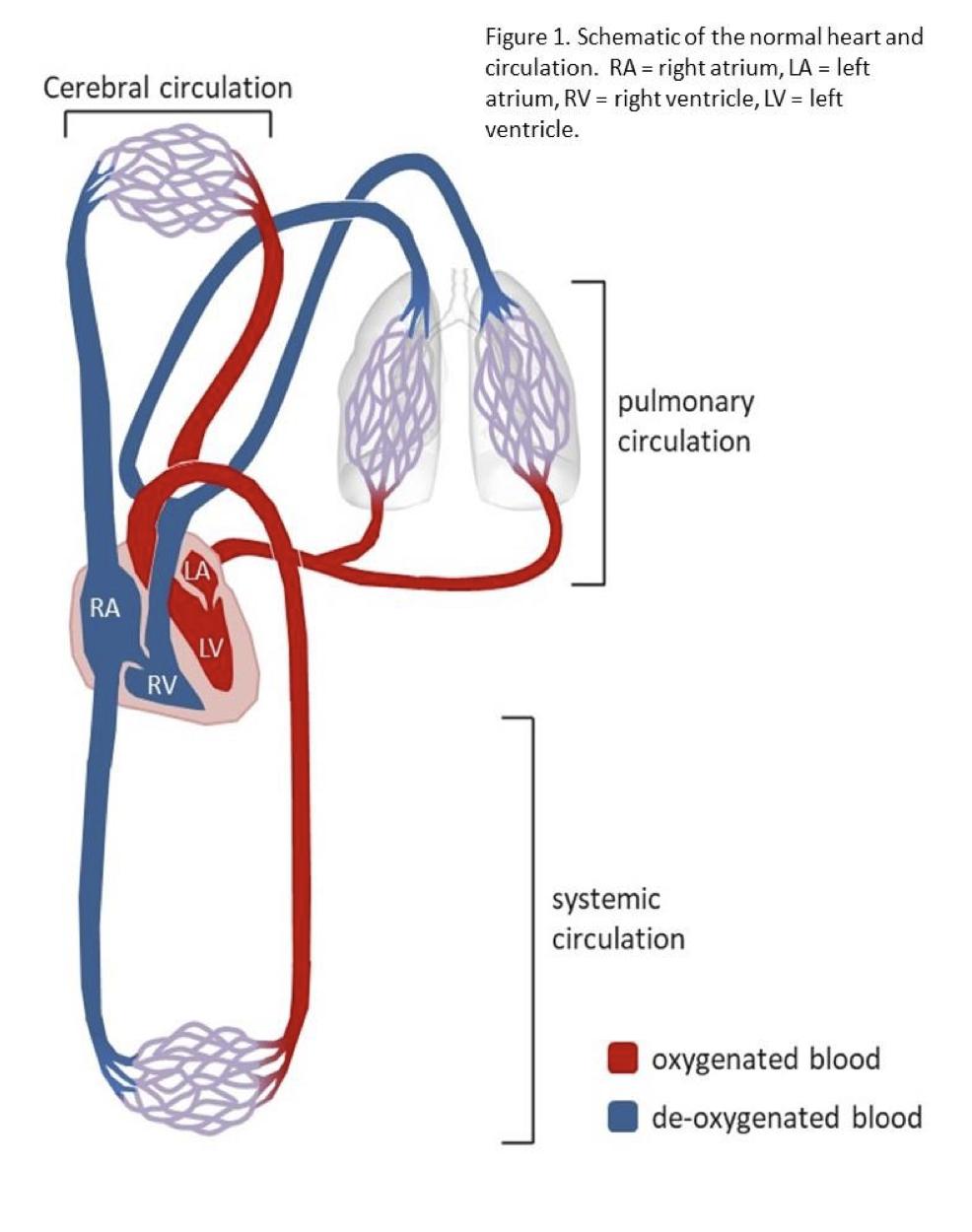
a) Where the cardiac cycle is initiated in a healthy heart
b) Where a diastolic blood pressure of approximately 80 mmHg is experienced in a healthy subject of AF’s age
c) Vessel carrying blood to the lungs
d) Where gas exchange takes place between blood and tissues
e) A valve that prevents backflow of oxygenated blood during ventricular systole
f) The largest capacitance vessel in the lower body (i.e., below the heart
g) cardiac conduction feutures
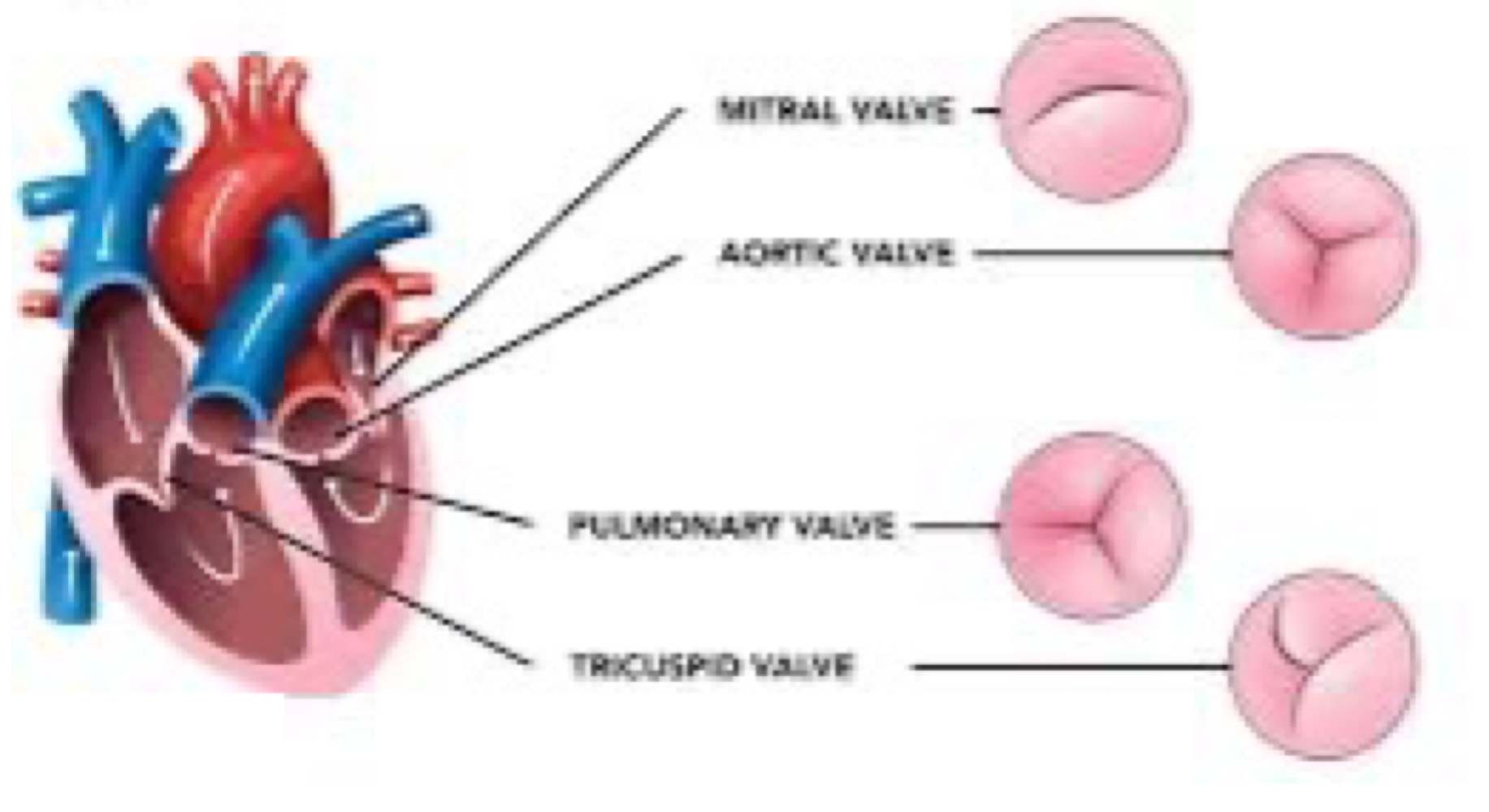
h) valves
A. Sino-atrial node
B. Aorta
C. pulmonary artery and pulmonary veins.
D. capillaries
E. Aortic valve-allows blood to flow from left ventricle to aorta, prevents backflow of blood.
F. venous system
g. SA node, AV node, Bach man bundle, pkunjie fibres, internal bands
effects on pt cardiovascular physiology if they run 3km every day. Consider:
(a) the immediate effects of running
(b) the long-term effects (i.e. if he continues running regularly every day).
a) increased HR + CO- As o2 demand inc = inc respiratory rate and tidal volume
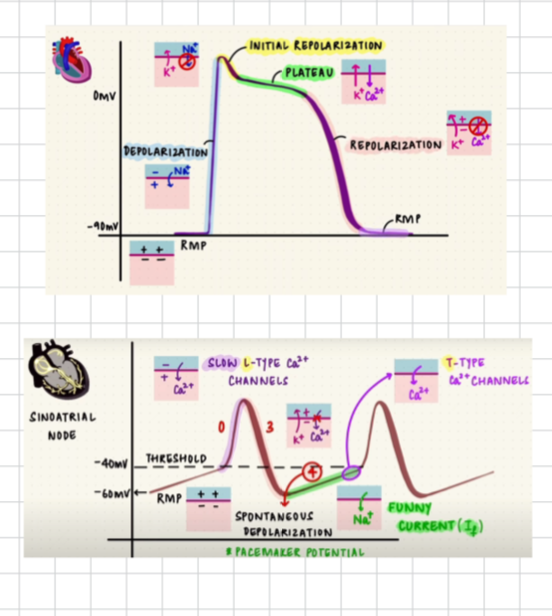
changes in blood (ph, co2 and o2 lvls) are detected by chemoreceptors in the carotid + activate + sends an AP to medulla = stimulates sympathetic ns = noradrenaline released + binds to SA node = beta-adrenergic receptors = inc CAMP = binds to funny channels = inc Na permeability = steeper depolarisation = faster heart rate
b) improved CO + more efficient heart
hypertrophy = inc heart muscle
what is an action potential + how do ap originate from the heart?
the rapid depolarization of a membrane that reaches a threshold level, it is always the same size (all or nothing ).
SA node has automacity (a cardiac cell ability to generate an AP) = has spontaneous depolarisation which creates an electrical impulse that spreads across atrial and initiates cardiac cycle
What two factors are responsible for changes in membrane potential during an action potential?
Ionic concntration gradient and Selective permeable ion channels in the membrane-
the opening close on of ion channels and flow following conc gradients controls the polarisation and depolarisation of the membrane
what are the homeostatic mechanisms to control high Bp
???
- baroreceptors in carotid sinus and aortic arch detect changes in pressure and signal to medulla oblongata’s CV centre
- activated parasympathetic system and release of acetylcholine. Sympathetic pathway effects are reduced so lower heart rate and cardiac output.
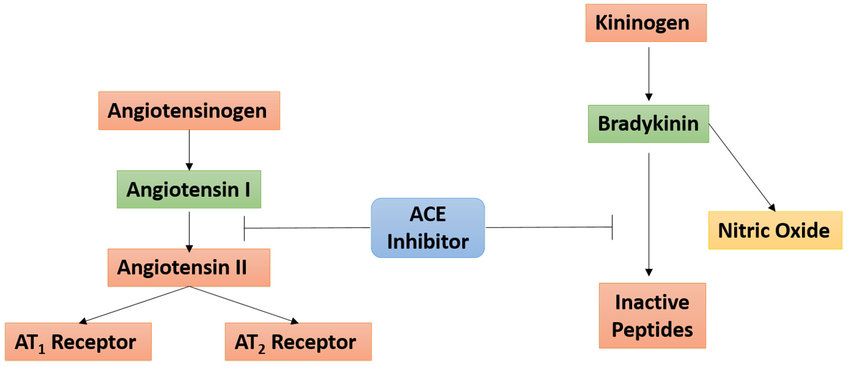
- RAAS - (1) reduced renin = less cleaving of Ang-1 into Ang-2 so less vasoconstriction, more dilation. (2) Less aldosterone release = lower blood volume due to less salt/water reabsorption and retention = lower preload
Why certain drugs are given with food.
Food delaying gastric emptying time, altering GI pH, stimulating bile flow, increasing splanchnic blood flow, or physically interacting with drugs.
In a fed state, gastric emptying is delayed, therefore drug delivery is delayed. However, food can increase the solubility of poorly soluble drugs allowing them to be better absorbed and drugs like NSAID which can stomach irritation food protects stomach.
fasted state- If gastric emptying increases the rate of absorption increases, therefore, taking medication in a fasted state increases the rate of absorption since the stomach transit time is lower, this is useful for enteric-coated formulations.
Describe the role of the bone marrow in the formation of blood cells. How does it differ between children and adults
the bone marrow is crucial for the production of blood cells through a process called hematopoiesis, which occurs within the bone cavities. In adults, there are two main types of bone marrow: red marrow, where hematopoiesis primarily occurs, and yellow marrow, which consists mainly of fat cells. Red marrow produces red blood cells (erythrocytes), white blood cells (leukocytes), and platelets (thrombocytes). White blood cells play a role in the immune system, while platelets are essential for blood clotting and wound healing.
In children, bone marrow plays a more significant role in hematopoiesis compared to adults. Initially, children have red marrow in their femur and long bones, but as they age, the amount of red marrow decreases, and it gradually converts to yellow marrow, which is less active in hematopoiesis. Despite this shift, certain bones in adults still contain red marrow and contribute to blood cell formation. Overall, bone marrow, especially in children, is vital for the continual production of blood cells necessary for various bodily functions.
/What sickle cell disease is and how is it caused?
Sickle cell disease (SCD) is a genetic condition affecting RBCs, usually flexible biconcave shape, to become rigid sickle / crescent shaped = harder for them to carry oxygen effectively = decreased O2 delivery to tissues and organs. Sickle-shaped cells are sticky + together, also reducing blood flow and increasing the risk of blockages in the vessels.
Caused by a genetic mutations that can cause sickle (crescent / c shaped) cell diseases.
HbSS SCD, also known as sickle cell anaemia, happens when an individual inherits two genes for haemoglobin ‘S’, resulting in the most severe form of the disease.
HbSC SCD happens when one inherits one haemoglobin ‘S’ and one haemoglobin ‘C’ gene, typically leading to a milder form of SCD compared to HbSS.
HbS beta thalassaemia arises when one inherits one ‘S’ gene and one beta thalassaemia gene, resulting in abnormal red blood cell shapes similar to other forms of SCD
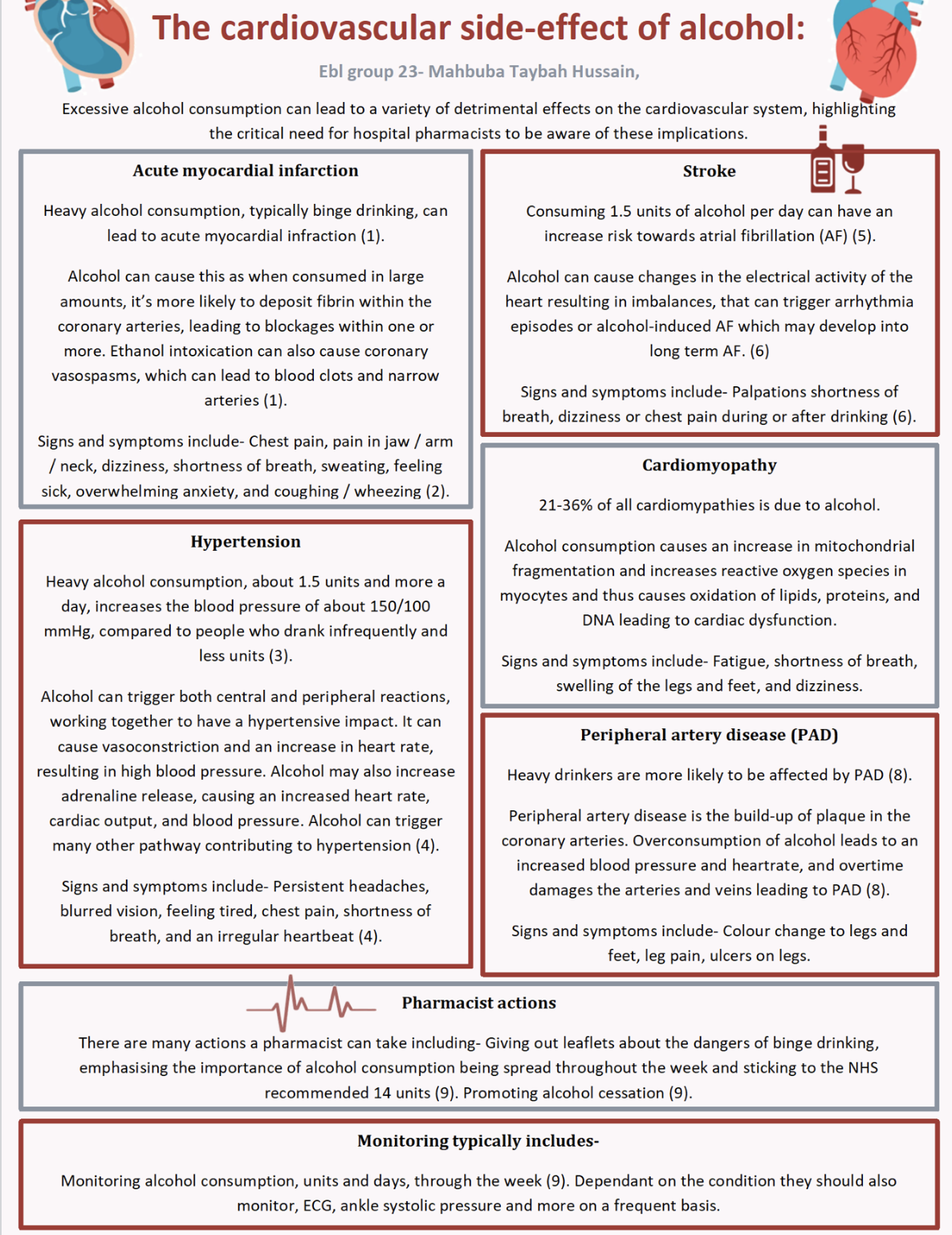
cardiovascular side-effects of alcohol.
direct and indirect costs
Direct Costs: Expenses directly associated with healthcare services, such as doctor visits, hospital stays, medications, medical procedures, and laboratory tests. Direct costs are typically paid for by NHS.
Indirect Costs: Financial impact of illness or health-related issues that extend beyond direct costs. These can include lost productivity due to illness, missing work, reduced quality of life, caregiver expenses, and long-term disability costs. Indirect costs are often paid by the individuals, employers and society as a whole.
(a) Why might the prescribing volumes go up?
(b) Why might the costs go down?
a) Increased demand for statin usage e.g. more patients with CVD and/or more preventative prescribing.
b) Generic alternatives are now available
Reduced demand requirement
Cheaper manufacturing
Government policy interventions
Explain how simvastatin converts into its active form.
Simvastatin is a prodrug which is used to lower the risk of cardiovascular disease and manage abnormal lipid levels by inhibiting the endogenous production of cholesterol in the liver. It is administered as the inactive lactone derivative.It is converted into its active form(simvastatin acid) by the hydrolysis of the lactone ring in the liver by the enzyme esterase
Simvastatin inhibits the enzyme HMG-CoA reductase to prevent it from converting to mevalonate, which is involved in the formation of cholesterol.
Through the inhibition of this enzyme,the production of cholesterol is reduced, lowering blood cholesterol levels.
Using your knowledge of cardiovascular physiology, suggest what changes in Mr. TD's circulation might have given rise to hypertension.
Smoking-
Smoking has a significant risk of increasing blood pressure. Nicotine, one of the active ingredients in cigarettes, stimulates the release of hormones like epinephrine and norepinephrine, which will increase the heart rate, and cardiac output, which will result in more blood going into the vessels per minute. This leads to the raise of blood pressure.
On the other hand, nicotine also has direct impacts on the blood vessels. It narrows the arteries, making them less flexible and more resistant to the blood flow, which increases the blood pressure.
Obesity-
Obesity triggers an overactive sympathetic nervous system, which plays a role in regulating blood pressure. This heightened activity can lead to elevated blood pressure
Also, obesity influences the RAAS system, a hormone system regulates blood pressure by increasing or decreasing the fluid into the bladder. Dysfunction of the RAAS system could contribute to high blood pressure.
Salty food-
When you consume excessive salt, your body retains more water to balance the concentration of salt in the blood. This increased water volume leads to a higher blood volume
Over time, excessive salt intake can lead to stiffened and narrowed blood vessels. These changes make it more difficult for blood to flow freely, contributing to hypertension
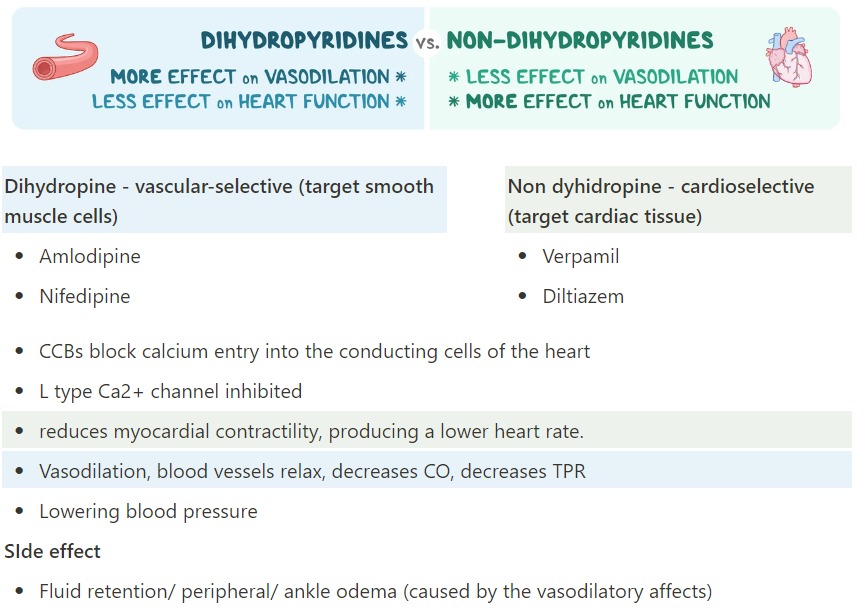
As part of your discussion with Mr TD, you will want to advise him not to drink grapefruit juice. Provide the rationale for discussing the impact of grapefruit juice on amlodipine clearance and bioavailability. Discuss whether this would be relevant to the other drugs that are prescribed for management of hypertension: atenolol, lisinopril and losartan.
Amlodipine is a dihydropyridines calcium channel blocker, which undergoes extensive first-pass metabolism and substances specific to grapefruit juice inhibit the primary oxidative step of the dihydropyridines to their dehydro-analogues by the hepatic enzyme CYP3A4.
Grapefruit juice reduces CYP3A4 activity by both reversible (competitive or non-competitive) and irreversible inhibition. This increases the drugs bioavailability therefore significantly increasing the plasma drug concentration.
An alternative mechanism by which grapefruit juice may alter the metabolism of co-administered drugs is by inhibiting P-glycoprotein activity.
Amlodipine has a lower hepatic extraction ratio than other Dihydropyridines, hence its higher oral bioavailability. With its high tissue affinity, oral amlodipine is taken up by hepatic tissue and then redistributed back into the systemic circulation. These properties result in a later time to peak plasma concentration and a longer plasma elimination half-life compared with other dihydropyridines.
Atenolol – no
Lisinopril – no
Losartan – yes, CYP 2C9 and CYP 3A4 are involved in losartan metabolism and are affected by grapefruit juice similar to amlodipine.
what is renal stenosis?
Renal stenosis is when the arteries taking blood to and from the kidneys get narrow and so not enough o2 rich blood can reach the kidneys appropriately.
It is mainly caused by atherosclerosis(build up of plaque- sticky substance made of cholesterol,calcium, fat in the inner walls of the arteries). It is also caused by fibromuscular dysplasia (FMD)—the abnormal development or growth of cells on the renal artery walls.
drugs mainly clreared by kidneys should be avoided or reduced dose.
KS is prescribed bisoprolol, lisinopril, digoxin and aspirin. For each of these medicines: (a) Explain its mechanism of action (b) Describe the indication for KS (i.e., why it is prescribed for KS) (c) Discuss its appropriateness for KS (including consideration of dosing) (d) Discuss any recommendations you may regarding any changes required (if applicable).
Two weeks after starting his digoxin, KS developed yellow vision, vomiting, nausea and skin rash. His digoxin trough level was 2 ng/ml (normal level:0.5-1.5 ng/ml). What is the likely cause and what would be the appropriate management?
The likely cause of these symptoms is digoxin toxicity due to above trough level value of it.
Hypokalemia predisposes the patient to digoxin toxicity; it is managed by giving a potassium-sparing diuretic(amiloride or spironolactone) or, if necessary, potassium supplementation.
Digoxin should be held and hydration with IV fluids, oxygenation and support of ventilatory function can be given.
With severe toxicity, ventricular tachycardia (which may be bidirectional) and ventricular fibrillation can occur. This is when we can give digoxin- specific antibody. But the indications for this is unclear. It is also very expensive per ampoule so cost-benfit analysis should also be done.
Considering Frank-Starling mechanism, impact on cardiac output, MAP, the sympathetic nervous system and the RAAS system Describe in detail why patients with heart failure develop oedema in their legs. In your answer you should consider both the immediate and long-term consequences of a failing left ventricle and describe the details of the underlying physiological processes.
The frank-starling mechanism states that the heart’s stroke volume increases in response to an increase in the volume of blood in the vent etricles.
This is because an increase in venous return increases the ventricular filling (end-diastolic volume) and therefore increases preload (the initial stretching of the cardiac myocytes before contraction). Myocyte stretching causes an increase in force generation. This mechanism enables the heart to eject the additional venous return, thereby increasing stroke volume.
In HF, the Frank–Starling curve is moved down (flattened) therefore a greater venous return and filling pressure is required to increase contractility and stroke volume. Mechanisms are activated to increase stroke volume and move the curve upwards.
In response to decreased cardiac output the sympathetic nervous system is activated by the carotid baroreceptor response. The SNS releases norepinephrine and adrenaline (epinephrine) from the adrenal cortex which promotes heart rate and cardiac contractility. This increases afterload and therefore increases venous hydrostatic pressure which forces more fluid into the interstitial space.
Activation of RAAS in response to low renal perfusion causes salt/water retention and increases preload (moving the curve left and up).
RASS activation increases angiotensin II, which leads to vasoconstriction and more salt and water retention, which further stress the ventricular wall and cause dilatation (remodelling) and worsening ventricular function. Angiotensin II also releases aldosterone which results in sodium reabsorption in the distal tubules of the kidney and promotes cardiac fibrosis.
These mechanisms increase water retention and increase venous hydrostatic pressure causing the accumulation of more tissue fluid. More fluid is forced out of the capillaries and less can be ‘drained’ back into circulation or the lymphatic system. This means fluid builds up within the interstitial spaces of the body. The legs are difficult to drain due to gravity further holding the fluid down.
In the short term, these neurohormonal systems induce many changes in the heart, kidneys, and vasculature that are designed to maintain cardiovascular homeostasis. However, with chronic activation, these responses result in haemodynamic stress and exert harmful effects on the heart and the circulation further progressing HF and producing symptoms such as oedema.
mechanism of action of furosemide + common side efs
monitoring
Loop diuretic
Acting upon the ascending limb of the loop of Henle loop diuretics inhibit the Na+/K+/2Cl- co transporter. This is responsible for the movement of ions from the tubular lumen to the epithelial cells. When salt enters, water follows by osmosis. Loop diuretics prevent salt reabsorption, so less water is reabsorbed. Loop diuretics also have a vasodilator effect on the veins.
Dizziness
· electrolyte imbalance e.g. hypokalaemia, hyponatraemia, metabolic alkalosis
· fatigue
· headache
· muscle spasms
· nausea
Efficacy: urine output should increase over a few days, weight loss (no more than 1kg/day) and symptom improvement.
Safety: serum electrolytes, renal function, blood pressure
LOST HEARING?
what red flag questions should the community pharmacist have asked the patient about pt “gord” symptoms and why?
Nature of pain:
-Angina often manifests as pressure, feeling tight, dull and heavy,, or squeezing in the chest, with possible radiation to the arm, neck, jaw, or back.
Onset and duration:
-Angina typically occurs during or after physical exertion / stress and lasts for a few minutes
-GORD symptoms may be after meals, night time and last longer.
Angina Symptoms:
-shortness of breath
-nausea
-sweating
-lightheadedness,
Medical history and family history: risk factors for cardiovascular disease such as hypertension, diabetes, smoking, or a family history of heart disease meaning angina is more likely to occur.
Glyceryl trinitrate (GTN) is an organic nitrate. Explain how organic nitrates can alleviate angina, highlighting the role and mechanism of action of nitric oxide (NO). Your answer should include details of the relevant enzyme and protein targets and the clinical implication
When Glyceryl trintrate ist aken, it is. metabolisedto nitric oxide (NO) within liver by CYP450. Nitric oxide (NO) then activates guanylate cyclase (GC) in smooth muscle cells. Activation of GC leads to the conversion of guanosine triphosphate (GTP) to cyclic guanosine monophosphate (CGMP). Elevated levels of GMP = dephosphorylation of myosin, leading to smooth muscle relaxation.
Vasodilation occurs primarily in the venous system, reducing preload on the heart, and to a lesser extent in the arterial system, reducing afterload.
By using Glyceryl trinitrate, this can relieve the symptoms of Angina by vasodilation.
GTN decreases myocardial oxygen demand by reducing preload and afterload, thereby alleviating angina symptoms such as chest pain or discomfort
Relaxation of veins: reduces cardiac preload.
Relaxation of large arteries: reduces cardiac afterload.
Relaxation of collateral vessels in the cardiac circulation: may improve perfusion of ischaemic tissue
ramipril MOA
rampiri = Angiotensis converting
enzyme inhilottor.
Reduce Agotensin I into angrotens II
reduced Aldosterone → reduced renin release in kidney (renin absorbs kidney reabsorption) → less water + ion reabsorption = less Blood volume = less CO= Lower BP
ALSO Aldosterone → cause vasodilation = decreased systematic ventricullaur resistance = lower bp.
metropolol moa
metropolol is a beta adrenoceptor antagonist with selectivity for β1-adrenoceptors (0.5 mark), which are found primarily in the heart (0.5 mark). Bisoprolol competitively inhibits/antagonises (0.5 mark) β1-adrenoceptors in the SA node, AV node and myocardium (0.5 mark – list at least two of these), reducing the effect of noradrenaline and other sympathetic neurotransmitters (0.5 mark). This reduces the contractility (or heart rate and force of contraction) (0.5 marks) therefore reducing overall cardiac workload (0.5 marks). This reduces risk of arrythmias and ischaemia (0.5 marks), improves diastolic filling time/systolic efficiency (0.5 marks) and reduces blood pressure (0.5 marks). Bisoprolol is also thought to reduce the output of renin in the kidneys, which reduces blood pressure (0.5 mark).
Simvastatin moa
Simvastatin is a prodrug when it is administered orally, undergoes metabolism in the liver and is transformed into its active form, by CYP3A4
Simvastatin acid enters the hepatocytes where it inhibits HMG-CoA reductase enzyme.
Simvastatin is a competitive inhibitor of HMG-CoA - an enzyme involved in synthesis of cholesterol in the liver. Statins block the action of the enzyme, which leads to a reduction in production of cholesterol in liver
Inhibiting HMG-CoA reductase results in reduced ability of the liver to produce cholesterol, which causes a decrease in LDL cholesterol levels.
The liver senses a decrease in cholesterol levels which leads to an increase in the number of LDL receptors on its surface - receptors bind to LDL particles circulating in blood - this promotes their uptake by the liver which results in further reduction in the amount of LDL cholesterol in blood.
secondary drug prevention of nstemi includes:
ACE inhibitor
Beta blocker
Dual-antiplatelet therapy
Statin (maximised)
Hyperlipidaemia
elevated LDL
the clinical indicator is the total cholesterol levels or HDL/LDL levels present in the patient’s blood and the relative change after treatment. Effective treatment should lower cholesterol levels back to a healthy range ideally a greater than 40% reduction.
What four main physiological events prevent blood loss from a damaged blood vessel? For each event, describe what initiates it and explain how it performs its role.
Constriction of the blood vessel-
within 30 mins of damage to the blood vessel, vascular spasm occurs which leads to vasoconstriction. It is initiated by chemicals called endothelins which are released by vessel-lining cells and by pain receptors in response to vessel injury.
Formation of a temporary “platelet plug." -
The ECM(extracellular matrix) /collagen fibres then become exposed to the blood components. The platelets become exposed to it and form a plug by sticking to it. This is assisted by a glycoprotein in the blood plasma called von Willebrand factor which stabilises the plug.
As they collect they release substances which further stop the bleeding . the substances are
ADP-adenosine diphosphate help in additional platelets to aggregate in the injury site.
Serotonin which maintains the vasoconstriction so blood flow gets constricted
prostaglandins(thromboxane A2) and phospholipids which also maintain vasoconstriction and help to activate further clotting chemicals.
Activation of the coagulation cascade-
This can be activated via extrinsic or intrinsic pathway. Injured vessels release thromboplastin and platelets release platelet factors which activate these pathways. The clotting factors convert prothrombin to thrombin and this helps in the conversion of fibrinogen into fibrin.
Formation of “fibrin plug” or the final clot-
The final steps in the coagulation cascade involve the conversion of fibrinogen to fibrin monomers which polymerizes and forms fibrin polymer mesh and result in a cross-linked fibrin clot. This reaction is catalysed by activated factor XIII (factor XIIIa) that stimulates the lysine and the glutamic acid side chains causing cross-linking of the fibrin molecules and formation of a stabilised clot.
Fibrinolysis is the gradual degradation of the clot-healing. There is a fairly complicated series of reactions that involves factor XII and protein-catabolizing enzymes. During this process, the inactive protein plasminogen is converted into the active plasmin, which gradually breaks down the fibrin of the clot. Additionally, bradykinin, a vasodilator, is released, reversing the effects of the serotonin and prostaglandins from the platelets. This allows the smooth muscle in the walls of the vessels to relax and helps to restore the circulation
intrinsic (continuing) and five temporary risk factors for the development of a DVT
Intrinsic factors:
-obesity
- Genetic predisposition-factor V leiden mutation
- Previous history of DVT or PE (Pulmonary Embolism)
-advanced age-over 60
- Family history of VTE
-cancer (some factors in cancer will also trigger thrombin cascade)
Temporary factors:
- pregnancy or postpartum
-surgery or trauma
-recent hospitalization
-long term immobilisation(prolonged travel)
-using oral contraceptive or HRT
Describe in detail the mechanism of action of warfarin, including details of the relevant protein (clotting factors) and enzyme targets. Considering its mechanism of action, explain why warfarin has a slow onset of action?
Warfarin competitively inhibits vitamin K epoxide Reductase complex -1 or Vitam§in-K Reductase. This enzyme is essential for the activation of Vitamin-K in the body.
Main role of vitamin-k is in the hepatic synthesis of active clotting factors as well as protein C and protein S which are also coagulation factors. Clotting factors II,VII,IX,X become mature or active by undoing gamma/y- carboxylation which is done by vitamin K. They then form a part of the coagulation cascade and form blood clots. This carboxylation reaction oxidises vitamin K which is then reduced by vitamin-k reductase enzyme back to its original form.
By inhibiting the enzyme warfarin stops the regeneration of vitamin k and in turn maturation of clotting factors.
Warfarin is metabolized by CYP450 enzymes so it has many drug-drug interactions due to inducers and inhibitors of the enzyme.
Slow onset of action- This is because the clotting factors which were pre-existing in the body must become depleted by natural turnover for the effect to be seen and this is very slow-takes days. The half-life of clotting factor II is very long -about 60-72 hours and we need its complete depletion before seeing full effects of warfarin which takes approx 6 days. The earliest changes in INR can be seem after 24-36 hours though.
Maturation means that the inactive enzymes or clotting factors are dominant when in blood but they are activated by vitamin K.
Patients should be advised not to take vitamin k rich foods with warfarin.
6. Explain the mechanism of warfarin interaction with St John’s wort (SJW). What are therapeutic consequences of this interaction? How would you manage a patient taking warfarin with SJW?
St John’s wort (SJW) - a traditional herbal remedy used to treat depression anxiety etc
warfarin - anticoagulant = prevent bloods clots = reducing risk stroke and heart attack
MOA- inhibits the synthesis of vitamin K-dependent clotting factors (II (prothrombin) , VII, IX, and X) in the liver and plays an important role in the coagulation cascade.
SJW induces CP450 enzymes (specifilly CYP3A4 + CYP2C9).
INCREASED ENZYMES = INCREASED METABOLISM
Warfarin is primarily metabolised by CYP2C9 = more enzyme in liver = increased and faster metabolism and decreased plasma conc.
Lower warfarin efficacy as subtherapeutic dose
more likely to form clot = more likely stroke, DVT, PE risk + increased bleeding risk
Educate the patient about the potential interaction between warfarin and St. John's wort, emphasizing the increased risk due to reduced warfarin efficacy.
Advise to stop SJW consumption and consider alternative medication including other herbal like ashwanda.
Monitor PT or INR to ensure warfarin is working as expected
Direct oral anticoagulants (DOACS) are another group of commonly used oral anticoagulants. Describe in detail the mechanism of action of DOACS including details of the relevant protein (clotting factors) and enzyme targets.
Direct oral anticoagulants (DOAC) act by directly inhibiting specific clotting factors in the blood, such as factor Xa and thrombin (factor IIa), unlike warfarin, which targets vitamin-K_dependant clotting factors.
It can be divided into two main groups:
Direct thrombin inhibitors: such as dabigatran, directly inhibits thrombin, which is a key enzyme involved in the coagulation cascade. Thrombin converts fibrinogen into fibrin, thereby preventing the formation of clots. Dabigatran binds direct;y to the active site of thrombin, preventing it from interacting with its substrate.
Factor Xa inhibitors: such as rivaroxaban, apixaban and edoxaban, it directly inhibits factor Xa, which is an essential enzyme in the coagulation cascade. Factor Xa converts prothrombin to thrombin, which then converts fibrinogen to fibrin, leading to clot formulation. By inhibiting factor Xa, these medications prevent the formation of thrombin and fibrin, thereby preventing clot formation. Factor Xa inhibitors bind directly to the active site of factor Xa, preventing it from interacting with its substrates
propose ways to alleviate the following problems in tablet formulation. Make sure to explain in detail the processes involved and possible excipients needed for each solution step.
a. High dose variation between tablets
b. Tablets sticking to the punches
c. Tablets not disintegrating in the appropriate time
d. Capping of tablets after compression
High dose variation between tablets Occurs because of- > uneven distribution of APIs during mixing > varying particle size of apis and excipients > inconsistent granule size or inconsistent density during granulation (in granulated formulations) Solutions- -mix properly to ensure homogeneity -control particle size distribution through milling -granulate through wet or dry granulation - improve flowability and uniformity - add flow enhancers such as silica, talc or magnesium stearate- acts as a lubricant or glidant and reduces segregation Talc is a useful lubricant because it has layers due to which they slide over each other. But it is quite hydrophobic so it can mess the physical properties and also affects the way the tablet dissolves. So we cant use too much of it. |
Tablets sticking to the punches = during tablet pressing tablet adheres to punch tip or walls > not enough or too much lubricant > puch surface rough causing it to stick? Solutions- > lubricate properly > add anti-adherent agent like silica or talc |
Tablets not disintegrating in the appropriate time >excessive compression- affecting porosity and density = affects water penetration >insufficient disintegrants Solutions- > add appropriate disintegrants such as >granulate (wet +/ dry) and compress properly- correct porosity and tablet struct |
Capping of tablets after compression > weak binding > uneven compression or over compression-energy build up which can cause capping. > weak tablet / elasticity Solutions- dont compress too hard. Add binders like microcrystalline cellulose (mcc) or excipients like magnesium stearate (lubricant), silica (gilidant), talc (anti-caking agent) |
. Briefly explain what a stroke is.
A stroke is when the blood supply to the brain is either blocked or cut off which prevents the brain getting enough oxygen and nutrients. It is a serious medical condition.It can be caused by a blood clot in the brain or by bleeding in the brain.
With reference to the underlying physiological processes describe why atrial fibrillation increases the risk of a person having a stroke.
Atrial fibrilation mainly causes irregular rate or rhythm in the heart.the sa node is firing action potentials irregularly. The atria doesn't contract fully. The blood is not being pumped out of the heart properly which leads to the blood being stagnant and blood pooling in the heart. This leads to the formation of blood clots which if leave the heart and form an emboli and that can go to the brain(cerebral arteries) and cause blockage and reduce blood and o2 supply which can cause stroke.it inc the risk of stroke by 5 times.
Using person centred language describes how you would explain to a person the symptoms of stroke and what they would need to do if they suspected someone was having a stroke.
Face – the face may have dropped on 1 side, the person may not be able to smile, or their mouth or eye may have dropped.
Arms – the person with suspected stroke may not be able to lift both arms and keep them there because of weakness or numbness in 1 arm.
Speech – their speech may be slurred or garbled, or the person may not be able to talk at all despite appearing to be awake; they may also have problems understanding what you're saying to them.
Time – it's time to dial 999 immediately if you see any of these signs or symptoms
amlodine moa
Amlodies is a calcium chanel blocker. CCBs disrupt the movement of Ca2+ through calcium channels.
MoA:
● Blocks L-type voltage gated calcium channels in cardiac muscle and blood vessels
● Decreases intracellular calcium, leading to decrease in muscle contraction – Negative inotropic effect on heart
● In blood vessels there is less contraction of vascular smooth muscle and larger diameter →Vasodilation
● Vasodilation decreases TPR and decreases cardiac contractility → Decreases CO → Decreasing BP
● Low BP means afterload increases → Decreases work of heart to eject blood into aorta → Oxygen demand on heart decreases → Improving symptoms of IHD
● Unlike Beta-Blockers CCBs do not decrease responsiveness of heart to input from SNS as BP regulation is carried out by SNS. CCBs allow more effective BP maintenance
● However, they cause a decrease in BP, therefore, baroreceptor reflex initiates a reflexive increase in SNS activity to increase HR and contractility. Effects can be minimised
a) Discuss the presence of pregelatinised starch in the capsule filling and which unit process you expect to have happened in the formulation of the capsule filling that makes this excipient necessary (3 marks)
(b) Why does the tablet formulation need two different excipients and which unit process you expect to have happened in the formulation of the tablet (2 mark)
(a) Pregelatinised starch is added to the capsules as a filler (0.5 mark). The low dose of ramipril (5 mg) (0.5 mark) and the use of pregelatinised starch in direct compression indicate that the formulation has acceptable powder flowability to be directly filled into the capsules (0.5 mark).
Pregelatinised starch has a moisture scavenger activity (0.5 mark); it is added to protect ramipril from hydrolysis during the formulation process and after capsule filling (0.5 mark).
(b) Pregelatinised starch is added to the tablet as a binder, disintegrant, and diluent for direct compression, in addition to its moisture scavenger activity (1 mark). The presence of pregelatinised starch suggest that the tablet can be prepared by direct compression (0.5 mark).
Unlike capsules, tablet formulation is a compressed dosage form, crospovidone is a superdisintegrant (0.5 mark) and it is added to the formulation to disintegrate the tablets into smaller particles and facilitate the dissolution (0.5 mark)
(Total - 5 marks)
HPLC
High Performance Liquid Chromatography (0.5 mark)
stationary phrase: C4, C8, C18 silica GEL (0.5)
Mobile phase: acetonitrile or mixture with water (0.5)
uv detection in 210 wavelength (0.5)
What direct medical costs could be generated in the future by the nos
hospital costs for acute management (examples could include A&E, ambulance, CCU, stroke unit, ward, interventions such as stent) (1 mark); secondary and primary care costs for rehabilitation and management afterwards (1 mark)
molecular mechanism of action of furosemide (including its site of action) and how it relieves oedema (4 marks)
Q4 (a) Furosemide blocks the Na+/K+/2CL- co-transporter (0.5 mark) in the thick ascending loop of Henle in the kidney nephron (0.5 mark). It inhibits the largest proportion of sodium and water reabsorption in the nephron (1 mark) and so is a potent diuretic in relieving oedema from the tissues (1 mark) as reduction of fluid in circulatory system allows tissue fluid to come into bloodstream and then removal by the kidneys (1 mark). (b) Furosemide has a fairly short half-life (0.5 mark), but if given later than lunchtime, risks the patient having to get up during the night to go to the toilet (0.5 mark) (Total - 5 marks) |
name the ethical principles
· Beneficence – to act in the patients best interests and prescribe the medication she needs or wants (1)
· Autonomy – the patient has a right to have a say in their care, so supply them with the medication they request (1)
· Justice – fairness to all, treat all patents equally – don’t supply the compound preparation, Otherwise this patient is requesting a more expensive formation without any justification (1).
Non-Maleficence: Pharmacists should avoid causing harm to patients and strive to minimize risks associated with drug therapy.
how kidneys play in regulating her plasma haemoglobin level.
Kidney’s release erythropoietin in response to hypoxaemia (0.5 mark), to stimulate erythropoiesis (red blood cell) in bone marrow (0.5 mark). (Total - 1 mark) |
The GP tells you he has read modified release iron preparations can effectively treat anaemia with lower risk of gastric upset. He asks you what you think about this and what you would recommend to reduce the risk of gastric upset. Briefly explain your answer (2 marks)
(a) It is claimed modified release preparations release iron slowly which can reduce gastric side effects (0.5 mark) but may carry iron past duodenum where most iron is absorbed (0.5 mark). It would be better to give a salt with less elemental iron (0.5 mark) and advise to take with food (0.5 mark)
how amlodipine’s mechanism of action causes oedema
Swollen ankles are due to peripheral oedema – this is caused because amlodipine causes vasodilation of resistance vessels – this increases blood flow in the resulting capillaries, increasing the hydrostatic pressure and hence forcing fluid into the interstitial fluid surrounding the peripheral tissues (especially in the lower limbs due to the effect of gravity)
(2 marks).
what is mona b
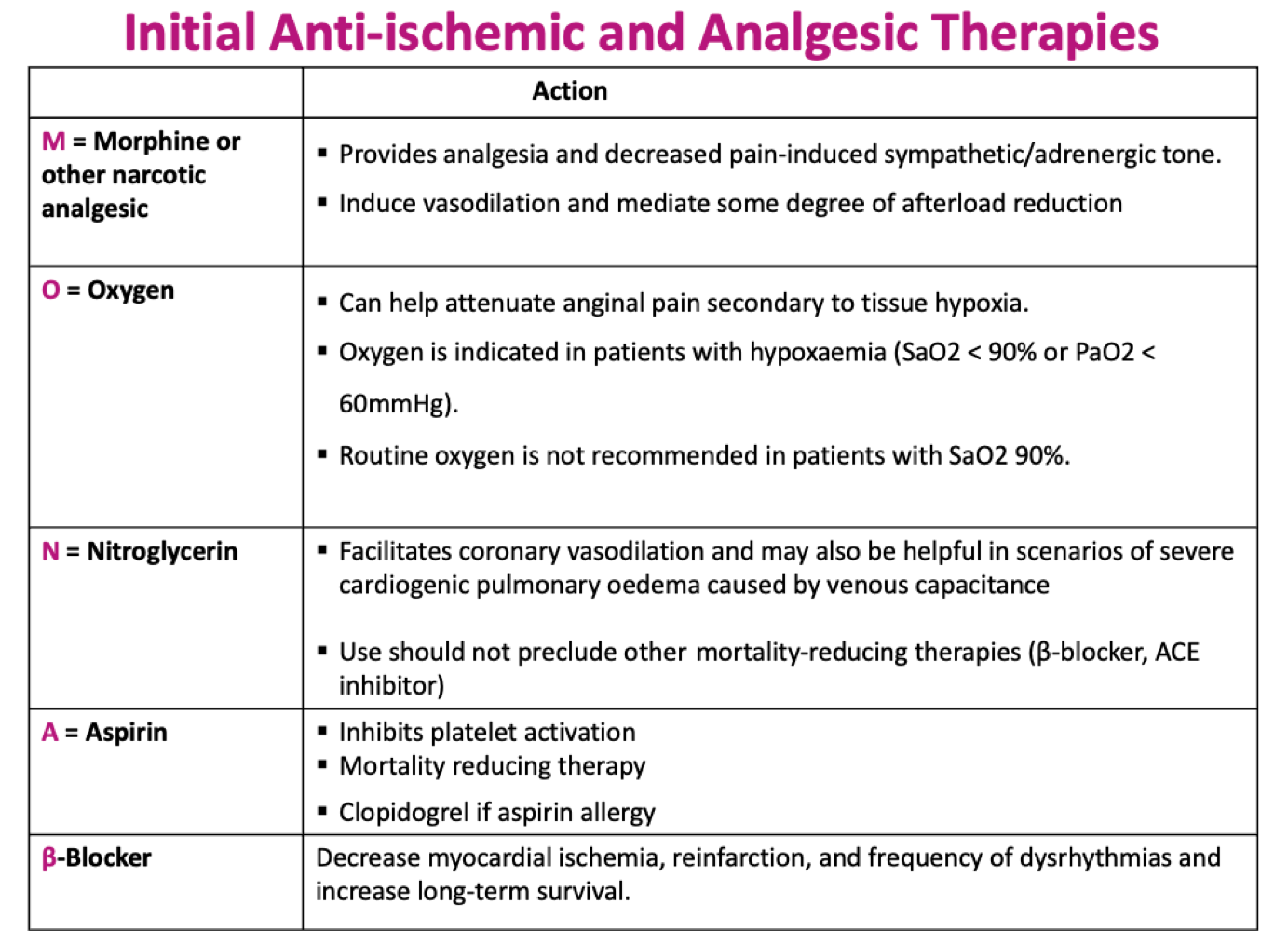
apirin moa
Acetylsalicylic acid is a non-steroid anti-inflammatory drugs (NSAIDs) (0 .5 mark). It works as an irreversible (0 .5 mark ) non-selective (0 .5 mark) cyclooxygenase enzyme inhibitor COX-1 & COX-2) (0 .5 mark). The acetyl group of acetylsalicylic acid binds with a serine residue of the cyclooxygenase-1 (COX-1) enzyme (0 mark ). This process stops the conversion of arachidonic acid to thromboxane A2 (TXA2) (0 potent inducer of platelet aggregation (0 .5 mark). Inhibition of COX-1 results in the inhibition of platelet aggregation for about 7-10 days (0 average platelet lifespan (0 .5 .5 mark), which is a .5 mark) which is the .5 mark). Inhibition of platelet aggregation prevents several cardiovascular complications such as the formation of venous or arterial thromboembolism, stroke or pulmonary embolism (0 .5 mark), which is essential as a secondary preventive measure in stable angina patients (0.5 mark).
Describe in detail how electrical activity is disrupted in atrial fibrillation and what are the key ECG features of atrial fibrillation.
The pathogenesis of AF involves initiating triggers, often in the form of rapidly firing ectopic foci (0.5 mark) located inside one or more pulmonary veins (0.5 mark) or in the atria (0.5 mark). The ectopic action potentials caused directly by multiple functional re-entry circuits (0.5 mark) varying in time, space and are not co-ordinated (0.5 mark). The AV node is then bombarded with signals trying to get through to the ventricles. This causes a fast and irregular heart rate (0.5 mark) and a ventricular rate ~ 110 – 160 (0.5 mark).
The main ECG Features of Atrial Fibrillation are Irregularly irregular rhythm (0.5 mark) , the absence of P wave (0.5 mark) and rapid ventricular rate (0.5 mark) .