Biol 417 Exam 1
1/107
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
108 Terms
neurons
Electrically excitable cells that transmit signals throughout the body
neurotransmitters
Chemical messengers that allow neurons to communicate with eachother
Diffuse across synapses (short distance)
Effects are rapid and short lived
hormone
Chemical messengers that travel in the bloodstream to act on target tissues
Travel long distances
Slower onset but longer lasting effects
neurosecretory neuron
A special type of neuron that produces and releases hormones instead of just neurotransmitters
Primarily located in the hypothalamus
autocrine signaling
Hormonal signaling
Signal targets the same cell that secreted it
Paracrine signaling
Hormonal signaling
Signaling affects nearby cells
Endocrine signaling
Hormonal signaling
Signal travels long distances vis the bloodstream to reach target cells throughout the body
macrolecithal eggs
Eggs characterized by having a large amount of yolk
Primary food source for the developing embryo
Ancestral trait
Most vertebrates
mesolecithal eggs
Eggs characterized by having a moderate amount of yolk
Concentrated in one hemisphere (vegetal pole)
Has a larval stage, the limited yolk can’t support full development inside the egg
Amphibians and Lampreys
microlecithal
Eggs that contain a very small amount of yolk
The devleloping embryo gets nutrients from another source like a placenta
Mammals
lecithotrophy
A developmental strategy where an embryo obtains its nutrition soley from the yolk contained within its egg
matrophy
A mode of embryonic development in which the mother provides nutrients directly to the developing embryo (e.g. placenta)
oviparity + lecithotrophy
The female lays eggs and embryonic development occurs outside the mother
Nutrients come from yolk inside the egg
viviparity + matrophy
The embryo develops inside the mother’s body, live birth
Nutrients come from the mother (placenta)
Internal fertilization
Benefits: embryo protection, higher survivial rate, stable developmental environment
Costs: high energetic demands, reduced mobility, fewer reproductive events (longer gestation)
viviparity + lecithotrophy (ovoviviparity)
Eggs are retained inside the body
Embryos get their nutrients only from the yolk
Live birth, but from hatched eggs
oviparity + matrophy
Monotremes, mammals that lay eggs
Embryos recieve additional nutrients (milk) from the mother after hatching
Platypus
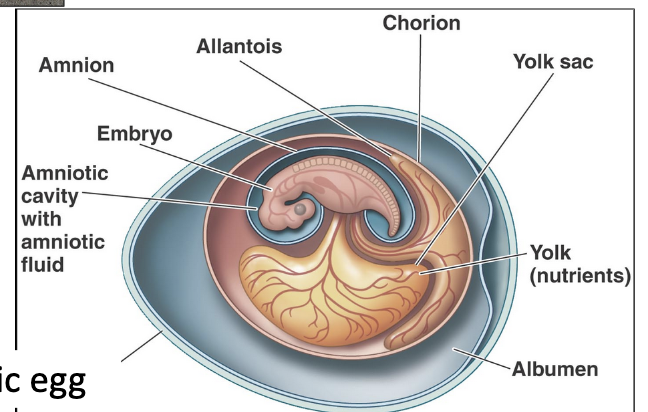
amniotes
An animal whose embryo developes in an amnion
An amnion is a membrane that encloses the embryo in a fluid filled cavity, used for protection
Lizards, snakes, turtles, crocodiles, birds, mammals
Advantages:
sturdy and porous eggshell
eggs can “breathe” and handle waste
ability to lay eggs on land or give live birth
free from dependence on water for reproduction in fish and amphibians
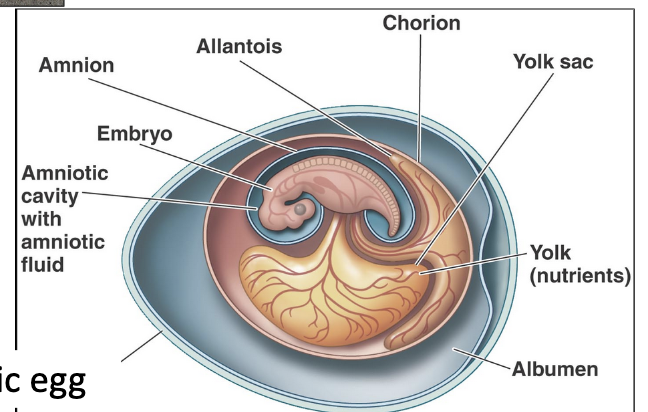
yolk sac
Present in all vertebrates
Extraembryonic membrane that provides the embryo with nutrients
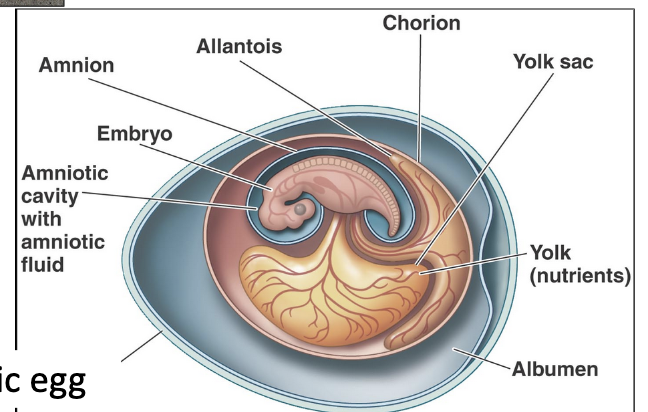
chorion
Present in amniotes
The outermost membrane surrounding the embryo
Good for protection and gas exchange
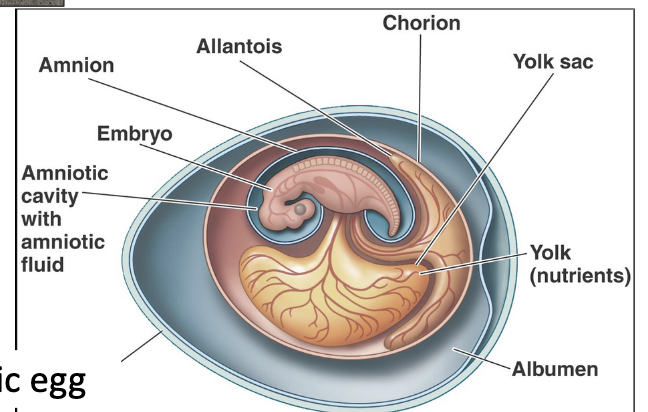
allantois
Extraembryonic membrane found in amniotes that aids in gas exchange and waste handling during embryonic development
placenta
An organ that develops in the uterus during pregnancy
Provides oxygen and nutrients to the developing embryo
Mammals, lizards, snakes
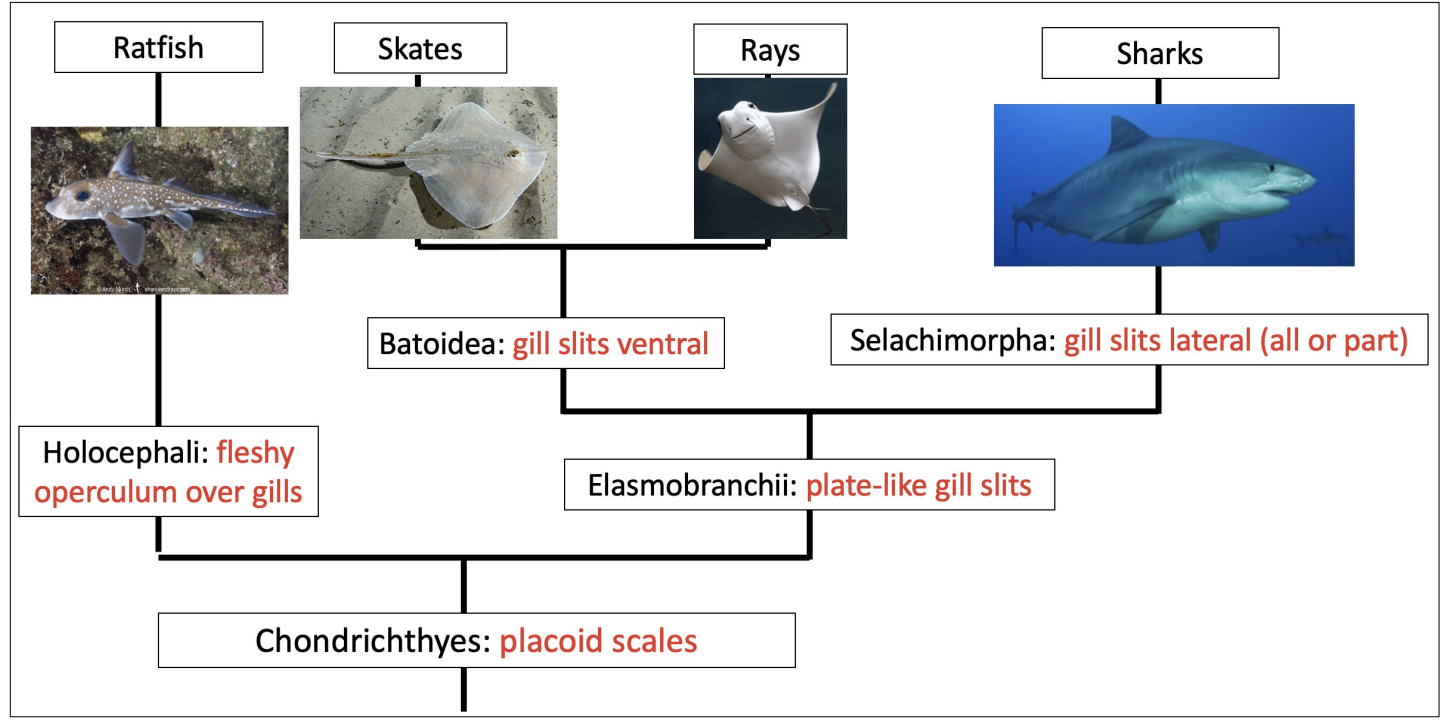
chondrichthyes phylogeny
traits shared by mammalian carnivores and elasmobranchs
Internal fertilization
Direct development (no metamorphosis)
Viviparity (live birth)
Long gestation
Larger and fewer offspring
Long-lived
viviparity in chondrichthyes
Viviparity is widespread in chondrichthyes
Viviparity evolved more than once in the chondricthyes
Oviparity never evolved from a viviparous ancestor
Co-evolved with increasing body size, shallower depth, and tropical distribution
Benefits:
Protection and increased embryo survival
Well developed offspring, more likely to survive on their own after birth
aplacental viviparity
51% of chondrichthyes use this mode of reproduction
Development of unattached embryos within the uterus
Three modes:
Oophagy/Adelphophagy
Lipid histotroph viviparity
Yolk-sac viviparity
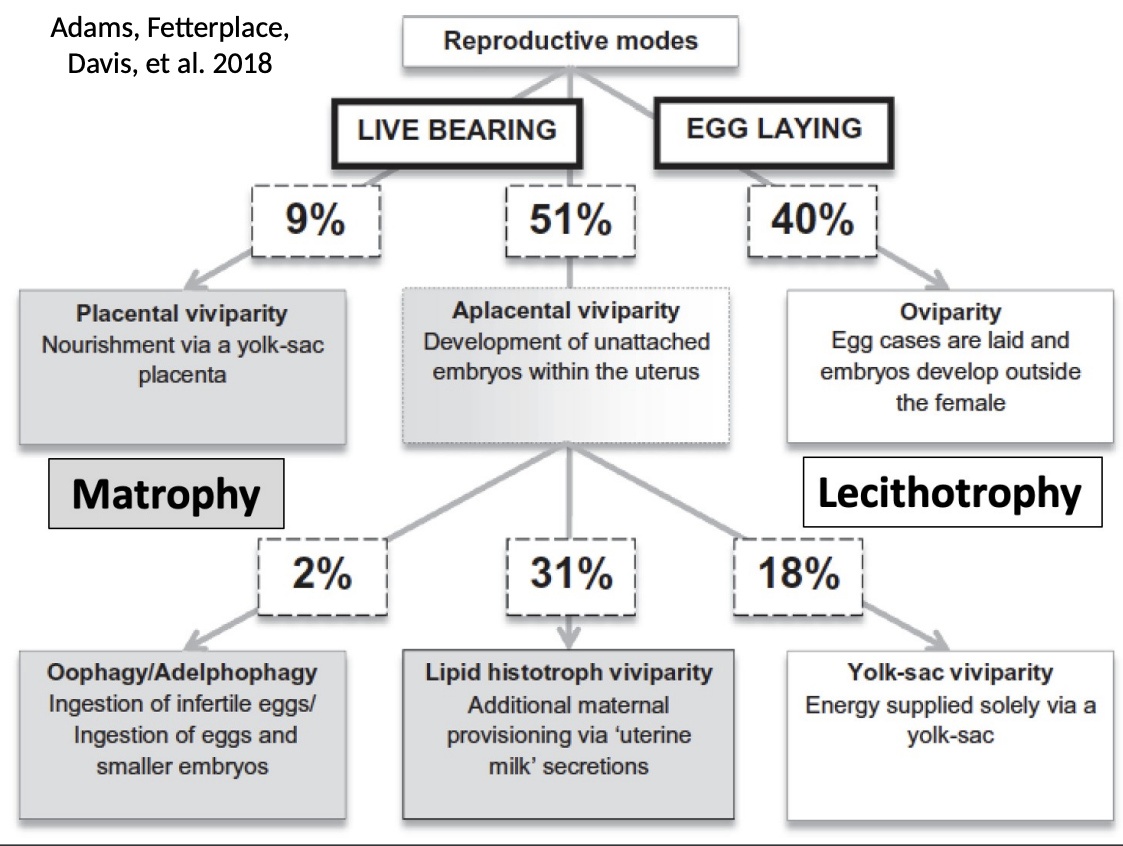
lecithotrophic oviparity in chondrichthyes
Ancestral trait
Egg laying reproduction, embryo nourished by yolk
The developing embryo and yolk are surrounded by a tough, protective egg case
Outer surface of egg cases are keratinized
Deep cold-water species lay eggs near hydrothermal vents

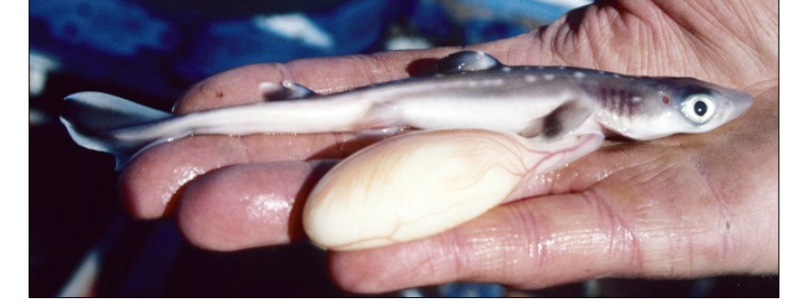
Yolk sac (lecithotrophic) viviparity
A mode of aplacental viviparity
Observed in guitarfish and dogfish sharks
Energy supplied soley via a yolk sac
Embryos develop inside the mother, live birth
Lipid histotroph viviparity
A mode of aplacental viviparity
Embryo starts out with a yolk sac but recieves extra nutrition via uterine milk secretions (matrophy)
The trophonemata (uterine villi) secretes uterine milk (lipid histotrophy)
California butterfly ray and stingrays
oophagy/adelphophagy
A mode of aplacental viviparity
Matrophy
Developing embryos feed on unfertilized eggs that are released from the ovaries (oophagy)
Ingestion of smaller embryos (adelphophagy)
uterine lamellae
Folds in the lining of the uterus that increases the surface area for gas exchange
Allows the mother to efficiently supply oxygen and remove CO2 from the uterine environment
Help non placental sharks like the great white efficiently deliver oxygen to their pups
placental viviparity in sharks
Nourishment via a yolk sac placenta
Once the yolk sac has been depleted, it attaches to the uterine wall acting as a pseudoplacenta that provides the embryo with nutrients from the mother (matrophy)
Blacktip shark
What is the goal of sexual reproduction?
Making a diploid zygote
Increasing the genetic variation within a population (benefit over asexual reproduction)
anisogamy
A form of sexual reproduction where males and females produce gametes of different sizes
Unequal investment in offspring
Males produce small gametes, females produce large gametes
gonads
Testes and ovaries
The organs that produce gametes
Where meiosis occurs to produce haploid gametes
spermatogenesis
The process of producing sperm in the testes
Takes place inside the seminiferous tubules
Males can produce up to a trillion gametes in their lifetime
4 gametes are produced by a single spermatogonium
Begins after the onset of puberty and continues throughout life
spermatogonia
Germ cells that undergo meiotic divisions to become sperm
Divides by mitosis to produce one cell that remains a spermatogonium (self-renewal) and another that differentiates into a primary spermatocyte which will enter meiosis to eventually form sperm
Present at birth
primary spermatocyte
Spermatocyte that has duplicated its DNA but not undergone a meiotic division
Diploid cell (2n)
secondary spermatocyte
Spermatocyte that has gone through the first meiotic division
Chromosome number reduced by half
Produces two haploid (n) daughter cells
Divides into spermatids in second meiotic division
spermatids
An immature sex cell formed from a secondary spermatocyte
Mature into sperm
Second meiotic division produces four haploid gametes (n)
seminiferous tubules
Region of the testes where sperm and hormones are produced
Contain two types of cells:
Spermatogonia
Sertoli cells
epididymis
Duct from seminiferous tubules to vas deferens where sperm complete their maturation and are stored
Sperm become motile and gain the ability to recognize and fertilize the egg
vas deferens
Tube that carries sperm from the epididymis to the urethra
Smooth muscle
ejaculatory duct
Formed by the union of the vas deferens and seminal vesicle duct
Sperm from the vas deferens and fluid from the seminal vesicles mix together to form semen
Passes through the prostate gland before it opens into the urethra, prostatic gland adds prostatic fluid to the mixture
Propels semen into the prostatic urethra during ejaculation
pathway of sperm
seminiferous tubules —> epididymis —> vas deferens —> ejaculatory duct —> urethra —> penis
seminal vesicle
Male accessory glands that contribute enzymes and other secretions to semen
prostate gland
Male accessory organ that contributes enzymes, nutrients, and other secretions to semen
Surrounds the urethra
Activates sperm
Enlarges with age
bulbourethral gland
Male accessory gland that produces components of semen
Located below the prostate
Contribute <5% of semen volume
Secrete a small amount of thick, alkaline mucus prior to ejaculation (pre-ejaculate)
Helps neutralize the acidic environment of the vaginal canal to protect the sperm
Lubricates the urethra to reduce friction during ejaculation
acrosome
Lysosome-like vesicle of sperm that contains powerful enzymes essential for fertilization
midpiece of sperm
Mitochondria to produce energy for sperm movement concentrates in the midpiece of the sperm body, along with microtubules that extend into the tail
flagellum
Tail-like structure that is used for swimming
Flagellum uses dynein to move
sertoli cells (nurse cells)
Testicular cells that support sperm production
Provide nourishment for the developing spermatogonia
Located inside the seminiferous tubules
blood testes barrier
tight junctions between Sertoli cells that prevent free exchange between the extracellular fluid and the lumen of the seminiferous tubules
interstitial (Leydig) cells
Cells in the testes that produce testosterone
Found between the seminiferous tubules
oogenesis
The process of forming female gametes (eggs)
At birth, the normal female ovary contains about 1-2 million oocytes
1 functional gamete is produced from a primary oocyte
Oogonia are produced during fetal development
ampulla
The widest part of the fallopian tube
Site of fertilization (sperm cell penetrates oocyte)
endometrium
The secretory inner lining of the uterus
Functional layer (stratum functionalis): the superficial layer shed during menstruation
Basal layer (stratum basalis): deeper, more stable layer that remains during menstruation
Contains glands that secrete nutrient-rich fluid to nourish a potential embryo after ovulation
Goes through cyclic changes each month as a part of the menstrual cycle
menstruation
a process that occurs when the body sheds the endometrial lining
proliferative/follicular phase
Phase of the menstrual cycle when the endometrium thickens and the ovarian follicles grow
Occurs before ovulation in anticipation of pregnancy
Estrogen levels rise as the dominant follicle in the ovary matures
Rising estrogen levels stimulate the endometrium to proliferate and thicken
luteal phase
Postovulatory phase of the uterus when it develops into a secretory structure
If no pregnancy occurs, the superficial layers of the endometrium are lost during menstruation
Ideal time for embryo implantation when the endometrium is thick and nutrient rich
ovulation
the release of an egg from the ovaries
primordial follicles
Consists of a primary oocyte in early meiosis surrounded by a single layer of granulosa cells
Present at birth and remain dormant until they begin to grow in reponse to hormonal signals during puberty
primary follicle
An undeveloped primary oocyte and its outer layer of granulosa cells
Oocyte begins to grow, number of granulosa cells increases
mature follicle
Follicle selected for ovulation
Meiosis resumes to form secondary oocyte
Large fluid-filled follicle that ruptures during ovulation to release the secondary oocyte
primary oocyte
Oocyte that has duplicated its DNA but not undergone a meiotic division
Females are born with all of their primary oocytes
Meiosis I begins during embryonic development and is arrested in prophase I
secondary oocyte
The ovulated egg which has gone through the first meiotic division
Meiosis I resumes in the dominant follicle that is selected for ovulation to produce a secondary oocyte and a polar body
Meiosis II begins (only completed if sperm penetration occurs)
corpus luteum
Ovarian structure that produces estrogen and progesterone after ovulation
Formed from the ruptured follicle
No pregnancy = degenerates into corpus albicans
Pregnancy = hormones sustain pregnancy
scrotum
The external sac into which the testes descend so that they can stay cooler than body temperature
dartos muscle
Smooth muscle that contracts to cause scrotal wrinkling
Reduces the surface area available for heat loss
Important for regulating the temperature of the testes
cremaster muscle
Skeletal muscle that contracts to pull the testes closer to the body, increasing their temperature
When it relaxes, the testicles hang lower, decreasing their temperature
pampiniform (venous) plexus
A network of veins arising from the testicular venous outflow
A key part of the countercurrent heat exchange system in the testes
Absorbs heat from the warmer arterial blood as it travels toward the testes
Cools the arterial blood before it reaches the testes, helping to maintain the lower temperature (2 degrees cooler than body temp) needed for sperm production
varicocele
Veins of the pampiniform plexus are enlarged
Dilated veins cause blood to pool and move more slowly, reducing the temperature difference between the venous and arterial blood, weakening heat exchange
Heat has more time to transfer into the slow moving venous blood
Venous blood becomes less cool by the time it reaches the artery
Smaller temperature difference between the artery and vein reduces efficiency of heat exchange
Results in higher testicular temperatures which negatively impacts sperm motility and production
path the egg takes to leave the body
Egg is released from the ovary during ovulation
Fimbriae at the entrance of the fallopian tube catch and transport the egg into the tube
The egg travels through the fallopian tube where fertilization can occur if sperm are present
If not fertilized, the egg enters the uterus and is eventually broken down
The egg and the uterine lining pass through the cervix
The unfertilized egg and uterine lining exit the body through the vagina during menstruation
vestibular glands
Female accessory sex glands
Produces a mucus-like secretion that lubricates the vagina during sexual intercourse
male and female parts with the same developmental origins
The clitoris is homologous to the penis
The labia is homologous to the scrotum
The vestibular glands are homologous to the bulbourethral glands
female external genitalia
Labia majora - outer folds of skin
Labia minora - inner folds that surround the vaginal and urethral openings
Clitoris
Urethral opening
Vaginal opening
male external genitalia
Penis
Scrotum
uterus
A hollow, muscular organ
Structure in which fertilized eggs implant and develop during pregnancy
Myometrium - middle layer made of smooth muscle, produces uterine contractions during labor
Contains more muscle than epithelium in comparison to the vagina
cervix
Neck of the uterus that opens into the vagina
Lined with mucous glands whose secretions create a protective barrier between the vagina and the uterus, can block or allow sperm to pass depending on the time in the menstrual cycle
Creates mucous plugs that forms in the cervical canal during pregnancy and seals off the uterus to protect the fetus from infection
Dilates during childbirth
clitoris
Female external genitalia important for sexual arousal
Has more than 10,000 nerve fibers
Clitoral stimulation leads to increased vaginal blood flow, lubrication, and temperature. It also neutralizes the vaginal acidicity and increases the chances of conception.
fallopian tube
Tube that transports eggs from the ovary to the uterus
Ciliated cells actively beat to propel the ovum (egg) from the ovary towards the uterus
Microvilli secrete nutrients
What signals do sperm move in response to?
Rheotaxis - movement in response to fluid flow, they swim against the flow of fluid which helps guide them toward the uterus and fallopian tubes
Thermotaxis - movement in response to temperature differences, sperm are attracted to the slightly warmer temp of the area near the ovulated egg
Chemotaxis - movement in response to chemical signals, the egg secretes chemical attractants
vaginal epithelium
The vagina is lined with stratified squamous epithelium, protects against abrasion
Prior to menopause, the high estrogen levels stimulate the vaginal epithelium to thicken and maintain an acidic pH that protects against infection. The epithelium is thick, moist, and elastic.
After menopause, the decline in estrogen causes the epithelium to become thinner and the vaginal pH to become more alkaline. This leads to increased dryness, reduced elasticity, and a higher risk of infection.
factors that may contribute to earlier onset of puberty and menstruation (menarche)
Improved nutrition and higher body fat
Exposure to endocrine-disrupting chemicals (interferes with hormonal signaling)
HPG axis
Hypothalamus → Pituitary Gland → Gonad
The hypothalamus contains neurosecretory cells that secrete releasing hormones (GnRH) into the portal system.
GnRH stimulates the anterior pituitary to release tropic hormones (LH and FSH) that target the gonads
The gonads (endocrine organ) produce sex hormones in response to tropic hormones (testosterone, estrogen)
tropic hormone
A hormone that has an endocrine gland as their target
FSH and LH
short-loop negative feedback
A pituitary hormone feeds back to decrease hormone secretion by the hypothalamus
long-loop negative feedback
Negative feedback from an endocrine gland hormone to the hypothalamus and anterior pituitary
gonadotropin-releasing hormone (GnRH)
Hypothalamic hormone that stimulates release of FSH and LH from the anterior pituitary
Release from the hypothalamus occurs in small pulses every 1-3 hours
Continuous administration of GnRH fails to stimulates secretion of FSH and LH (receptors become desensitized and downregulated)
luteinizing hormone (LH)
Anterior pituitary hormone that acts on the gonads to influence hormone production
Stimulates the Leydig (interstital) cells to produce testosterone from cholesterol
Stimulates theca cells to produce androgens
Levels are low during the follicular phase, rise dramatically just before ovulation, and then decline in the luteal phase
LH surge triggers ovulation
follicle-stimulating hormone (FSH)
Anterior pituitary hormone that stimulates gamete production in the gonads
Stimulates sertoli cells resulting in:
Synthesis of ABP
Stimulation of spermatogenesis
Secretion of inhibin
Induces aromatase expression so granulosa cells can convert androgens into estrogens
Stimulates the growth of follicles
FSH levels rise at the very beginning of the cycle (due to drop in estrogen and progesterone), rising estrogen levels from the follicles inhibits FSH secretion causing levels to decline, levels rise right before ovulation, high progesterone after ovulation causes levels to drop
testosterone
Sex hormone dominant in males
Secreted by Leydig (interstitial) cells and diffuses into nearby seminiferous tubules where sertoli cells help maintain a high local concentration of testosterone by binding it to ABP
Long loop negative feedback: inhibits the release of GnRH, FSH, and LH
androgen-binding protein
Sertoli cell protein that binds testosterone to keep it in the lumen of the seminiferous tubule
inhibin
Peptide hormone from the gonads that inhibits FSH secretion from the anterior pituitary
Secreted by sertoli and granulosa cells in response to FSH
aromatase
Convert androgens (testosterone) into estrogens
theca cell
The outermost layer of the ovarian follicle
Stimulated by LH to produce androgens (e.g. testosterone)
No aromatase activity
Androgens diffuse into granulosa cells
Progesterone made in granulosa cells acts as a precursor that diffuses to theca cells, where it is converted into androgens
granulosa cell
Innermost layer of the ovarian follicle
Stimulated by FSH to secrete estrogens and inhibin
FSH stimulates granulosa cells to convert androgens recieved from theca cells into estrogen using the enzyme aromatase
estrogen
Steroid hormone associated with female reproductive organs
Estrogen levels rise during the mid-follicular phase and then drop after ovulation. This is followed by a secondary rise in estrogen during the mid-luteal phase with a decrease at the end of the menstrual cycle.
progesterone
Primarily produced after ovulation during the luteal phase
After the mature follicle releases the egg, the granulosa and theca cells of the ruptured follicle transform into luteal cells, forming the corpus luteum
These luteual cells are now specialized to produce large amounts of progesterone
hormonal control of the menstrual cycle
The hypothalamus releases GnRH, which stimulates the anterior pituitary to secrete FSH and LH
FSH promotes the growth and maturation of follicles in the ovary. Granulosa cells are stimulated by FSH to secrete estrogen and inhibin.
Estrogen and inhibin act on the hypothalamus and pituitary gland to reduce the release of GnRH and FSH. This causes a decline in FSH levels which causes smaller follicles to degenerate, resulting in the emergence of a single dominant follicle
As the dominant follicle grows, it produces more estrogen which triggers a positive feedback loop that stimulates a surge of LH (and FSH).
This rise in LH leads causes ovulation
The ruptured follicle transforms into the corpus luteum which produces high levels of progesterone (also produces estrogen)
Progesterone inhibits GnRH, FSH, and LH secretion through negative feedback (inhibin also exerting negative feedback)
If pregnancy does not occur, the corpus luteum degenerates and progesterone levels fall, removing the inhibition on GnRH and allowing FSH levels to rise again to trigger the next cycle
kisspeptin
Hypothalamic neuropeptide that acts upstream of GnRH
Stimulates the release of GnRH
Released by KNDy neurons in pulses
Sensitive to feedback from low levels of sex steroids
Factors that may impact release:
Day length
Food intake/body fat
Stress level
Environmental estrogens