Electrical Activity of the Heart/Cardiac Action Potential Block 1
1/65
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
66 Terms
2 Parts of the Cardiovascular System
Heart: acts as a pump
Blood vessels: set of tubes connected to the pump
2 Parts of the Circulatory System
Pulmonary circulation: the right side of the heart pumps blood to the pulmonary circulation and the left side of the heart receives blood from the pulmonary circulation
Systemic circulation- the left side of the heart pumps blood to the systemic circulation and the right side of the heart receives blood from the systemic circulation
arterioles
these blood vessels are surrounded by smooth muscle. Contraction of the SM changes diameter of the blood vessel which affect blood pressure
these blood vessels are the site of nutrient and waste exchange
capillaries
systemic circulation contains a # of capillary beds arranged :parallel are found where?
most beds are arranged this way
just not kidneys and liver
capillary beds arranged in series are found where?
in the liver and kidneys
capillaries are found within______um of most cells in the body
50
this is important since O2 moves from blood into the interstitial compartment via diffusion
the veins contains how much of the blood? how about the arteries and arterioles?
vein- 64% (low P)
arteries and arterioles- 16% (high P)
Cardiovascular system: transports what INTO the body
-nutrients and water
-oxygen
Cardiovascular system: transports what OUT of the body
-CO2
-metabolic wastes
-heat
Cardiovascular system: transports what within the body
-hormones
-immune cells
-Abs
-clotting proteins
-stored nutrients
what generates the pulsitile pressure of the heart
the pulsitile property of the heart originates in specialized cells in the heart capable of generating periodic action potentials. These periodic APs spread throughout the heart, causing periodic contraction of the heart. This periodic contraction generates periodic, pulsitile pressure
a pulse of pressure is defined as
the difference between the highest pressure developed in a beat and the lowest pressure
the pressure pulse is largest in
the heart
before the heart contracts, the pressure is
close to zero
as the heart (left ventricle) ejects blood the pressure reaches
its maximum at about 120 mm Hg
by the time the pressure pulse reaches the the arterioles and the capillaries the pressure pule is
close to 0
this does NOT mean that the pressure in the arterioles and the capilarries is 0, but that there is no fluctuation in pressure from 1 heartbeat to the next. This insures a continuous flow of blood through the capillaries
the pressure in the veins and on the right side of the heart is what? then what would the pressure difference at the max pressure between the left side of the heart and right side of the heart be?
close to zero
so about 120 mm Hg
the biggest difference between the pressures in the pulmonary vs systemic
just lower in the pulmonary circulation
at resting heart rate what ANS exerts a stronger influence?
P-ANS
thus, severing P-ANS nerves to the heart will increase resting HR to a greater extent that severing sympathethic nerves would decrease HR
P-ANS control of the heart involves what NTs and what receptors?
ACh and M2
S-ANS control of the heart involves what NTs and what receptors?
NE; beta-1 (cardiomyocytes) and alpha-1 (smooth muscle)
the P-ANS innervates what of the heart?
only nodal regions of the heart
the heart's pump strength is controlled by what branch of the ANS?
S-ANS
There is some P-ANS control of ATRIAL muscles, but bc most of blood is pumped from heart as a result of ventricular contraction, there is little P-ANS effect on the strength of contraction of the ventricles
this is a collection of pacemaker cells near the right atrium
sino-atrial (SA) node
Electrical Activity in the Heart Pathway
SA node-->atrial muscle contracting--> AV node--> Bundle of His (AV bundle--conducting)--> Bundle Branches (Left/Right--conduction)--> Purkinje Fibers (conducting)--> Ventricular Muscle (contracting)
3 basic types of cells in the heart
-pacemaker
-conducting cells
-contracting cells
pacemaker cells
cells that set the automatic rhythm of the heart and allow it to beat contiunously throughout a lifetime. These cells are found in the SA and AV node.
These cells are electrically connected via gap junction--fire APs on their own
conducting cells
conduct the electrical signal (AP) from 1 part of the heart to another. These cells are found in the bundle His, the bundle branches and the Purkinje fiber networks
where are conducting cells found?
-bundle of His
-bundle branches
-Purkinje fiber network
contracting cells
generate P w/in the heart and pump blood out of the heart. These cells make up most of the cells in the walls of the atria and the ventricle. Contracting cells are called myocytes and make up about 75% of the total volume of the heart
contracting cells are aka? and make up what % of volume of heart?
myocytes; 75%
what are the 2 main types of action potentials in the heart?
-pacemaker AP
-AP in conducting and contracting cells
nodal/pacemaker APs
found in the SA and AV nodes. This type of AP is autorhythmic: these cells generate the same AP periodically for long periods of time
conducting/contracting APs
AP found in myocytes and conducting cells such as bundle of His, bundle branches, purkinje fibers
these cells either contract in response to an AP or conduct the AP to neighboring cells
the nernst potential for Na+ in the heart
+70
the Nernst potential for K+ in the heart
-94
the Nernst potential for Ca2+ in the heart
+132
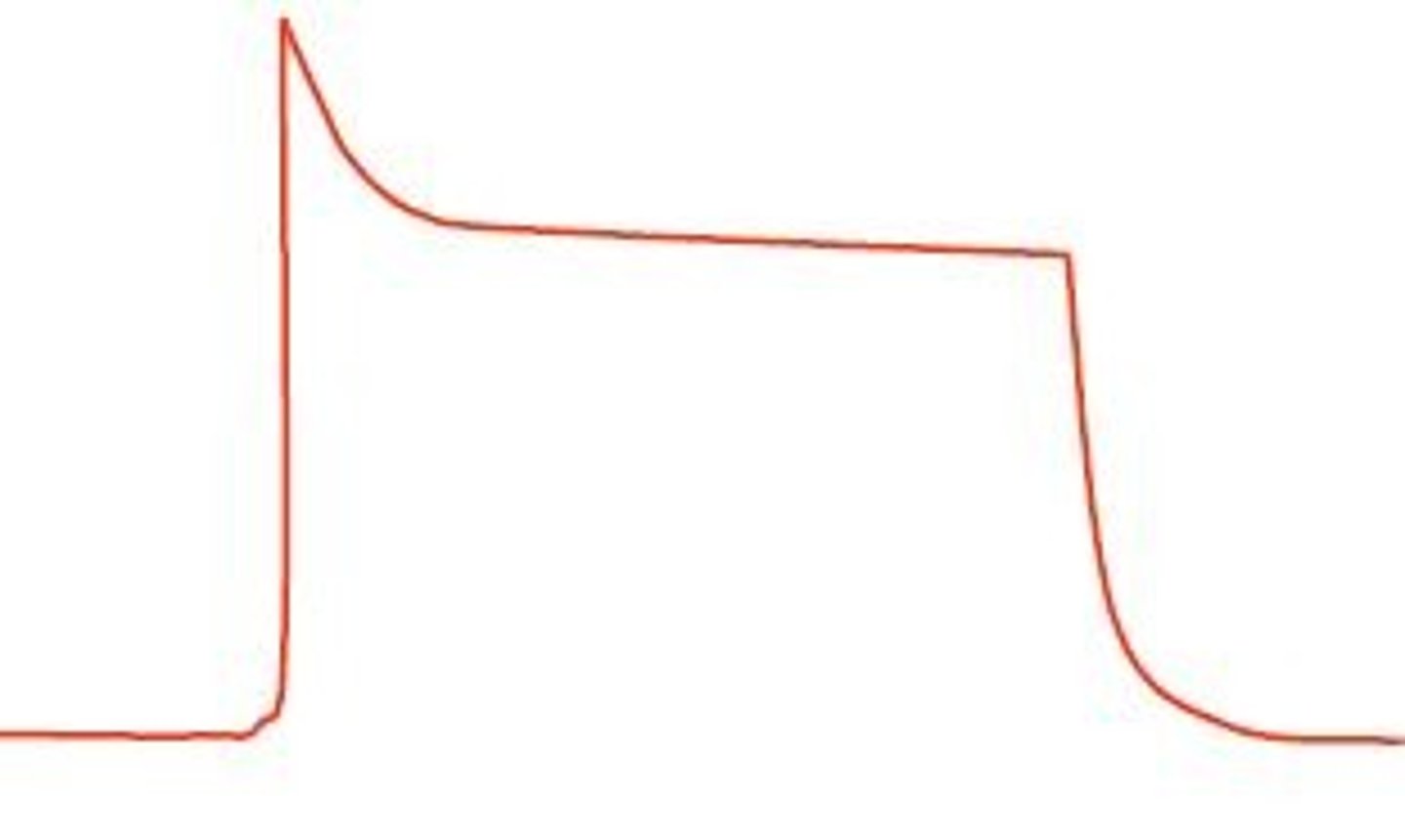
the 5 phases of an AP in conducting and contracting cells
Phase 0- Upstroke
Phase 1- Initial (or early) repolarization
Phase 2- Plateau
Phase 3- (final) repolarization
Phase 4- Resting Membrane Potential
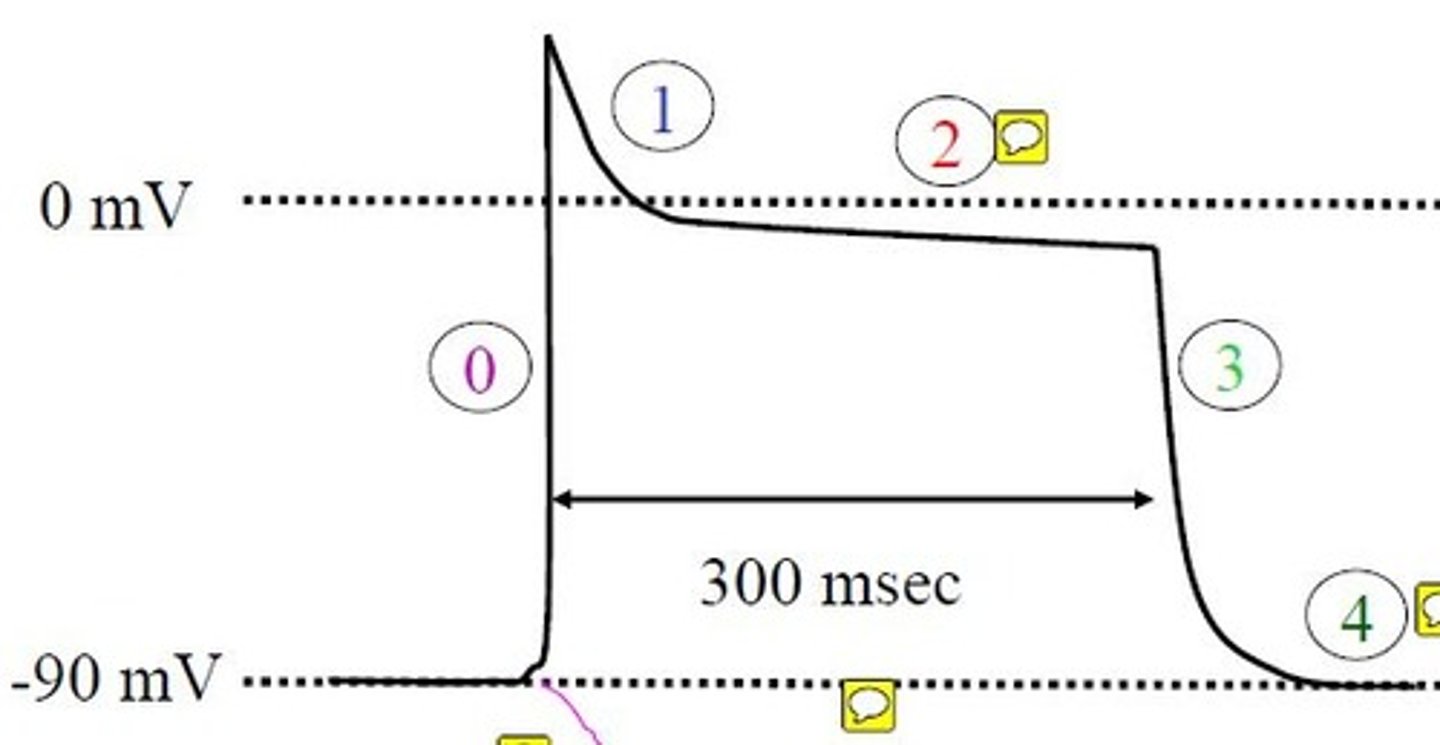
Phase 0: Upstroke (Conducing and Contracting Heart Cells AP)
cells repolarizes as a result of the spread of an AP from a neighboring cell.
-this depolarization opens FAST voltage-gated Na+ channels.
-this leads to further depolarization which opens up more voltage-gated Na+ channels
Phase 1: Initial (or early) repolarization (Conducting and Contracting Heart Cells AP)
-cell hyperpolarizes slightly
-this is due to the opening of voltage-gated type I K+ channels and inactivation of voltage-gated Na+ channels
Why does Phase 1- Early repolarization occur in conducting and contracting cells
due to the opening of voltage-gated K+ channels and inactivation of voltage-gated Na+ channels
What type of K+ channel opens up in early repolarization (Conducting and Contracting Heart Cells AP)
type I
Phase 2: Plateau (Conducting and Contracting Heart Cells AP)
-the cell remains at 0 mV (due to the opening of type II K+ channel and voltage gated Ca2+ channels)
-Since both channels are open, the membrane potential is somewhere in between the Nernst potential for K+ and Ca2+ (near 0mV)
why does the cell remain around 0 mV during phase 2: plateau (Conducting and Contracting Heart Cells AP)
due to the opening of type II K+ channel and voltage gated Ca2+ channels--the membrane potential in the middle for the Nernst for both
what type of K+ channel is open in Phase 2: plateau (Conducting and Contracting Heart Cells AP)
type II
type I inactivates in the beginning of phase 2
Phase 3: repolarization (Conducting and Contracting Heart Cells AP)
towards the end of phase 2 and during this phase (3), the voltage-gated Ca2+ channels inactivate and the voltage-gated K+ channels dominate so the membrane potential hyperpolarizes towards the Nernst potential for K+ (-94 mV)
in phase 3 (Conducting and Contracting Heart Cells AP) , why does repolarization occur
the voltage-gated Ca2+ channels inactivate and the voltage-gated K+ channels dominate so the membrane potential hyperpolarizes towards the Nernst potential for K+ (-94 mV)
Phase 4:resting membrane potential (Conducting and Contracting Heart Cells AP)
-the membrane potential when there is no AP
-it is negative and is due to K+ channels which are open at any membrane potential (leak channels)
all 4 types of voltage-gated channels in the conducting/contracting AP (2K+, 1Na+,1Ca2+) are what type of channels in terms of voltage
depolarization activated channels
order of opening of channels in the conducting/contracting AP
voltage-gated Na+ channel--> type I voltage-gated K+ channel--> voltage-gated Ca2+ channel--> type II voltage-gated K+ channel
in phase 0 (conducting/contracting AP) which channels are open, inactive, closed and what dominates
open: Na+ (dominates), K+-type I, Ca2+, K+-type II
in phase 1 (conducting/contracting AP) which channels are open, inactive, closed and what dominates
open: K+-type I (dominates), Ca2+, K+-type II
inactive: Na+
in phase 2 beginning which channels are open, inactive, closed and what dominates
open: K+-type II, Ca2+ (both dominate)
inactive: Na+, K+-type I
in phase 2 (conducting/contracting AP) towards the end which channels are open, inactive, closed and what dominates
open: K+-type II (dominates)
inactive: Ca2+
in phase 3 (conducting/contracting AP) which channels are open, inactive, closed and what dominates
open: K+-type II (dominates)
inactive: Ca2+, Na+, K+-type I
in phase 4 (conducting/contracting AP) towards the end which channels are open, inactive, closed and what dominates
all 4 are closed. only channel open are K+ leak channels
of the 4 channels in the AP in conducting/contracting heart cells which does not inactivate
K+-type 2 goes from closed to open to closed
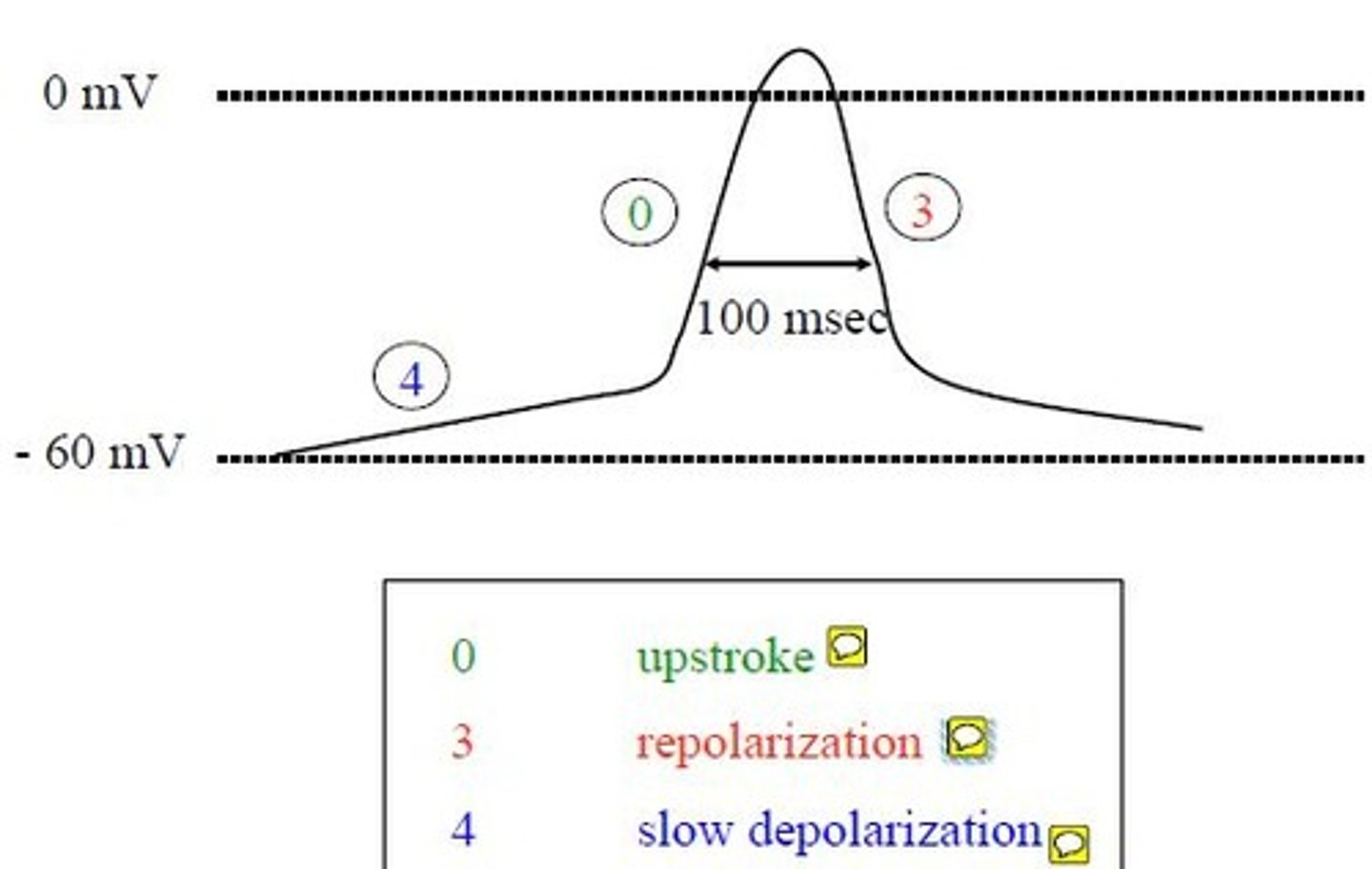
Pacemaker Action Potential is made up of what phases
4) Slow depolarization
0) Upstroke
3) Repolarization