Pathophysiology II - Exam 4 - AOM, Sinusitis, & Pharyngitis👃🏼
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
38 Terms
what is otitis media? what is acute otitis media (AOM) and otitis media with effusion?
inflammation of the middle ear
- AOM: inflammation of the middle ear with infection
- with effusion: inflammation of the middle ear with fluid and without infection
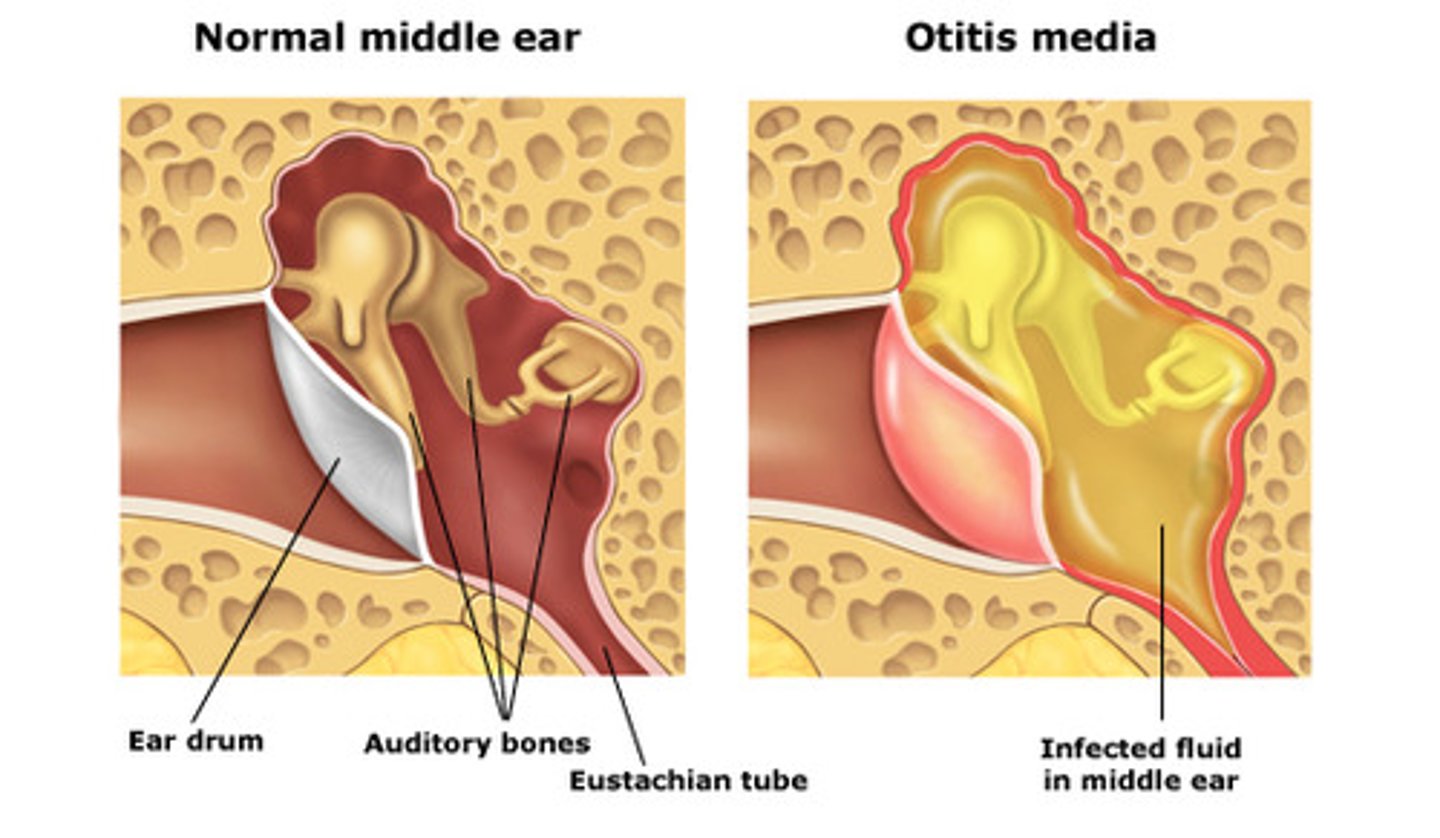
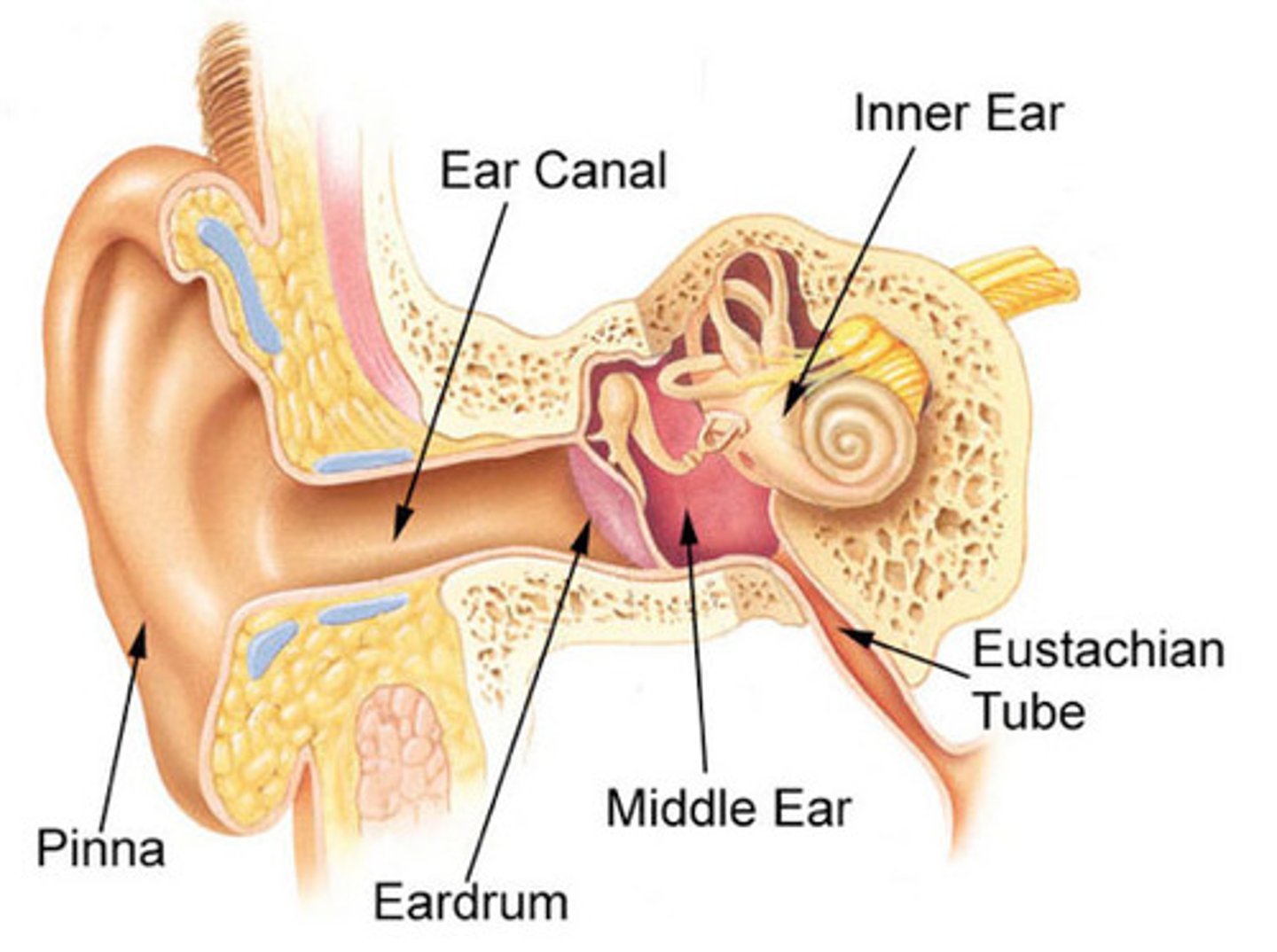
what is the eustachian tube? what does it do?
passage between the sinuses and the middle ear space
- drains fluid and balances pressures
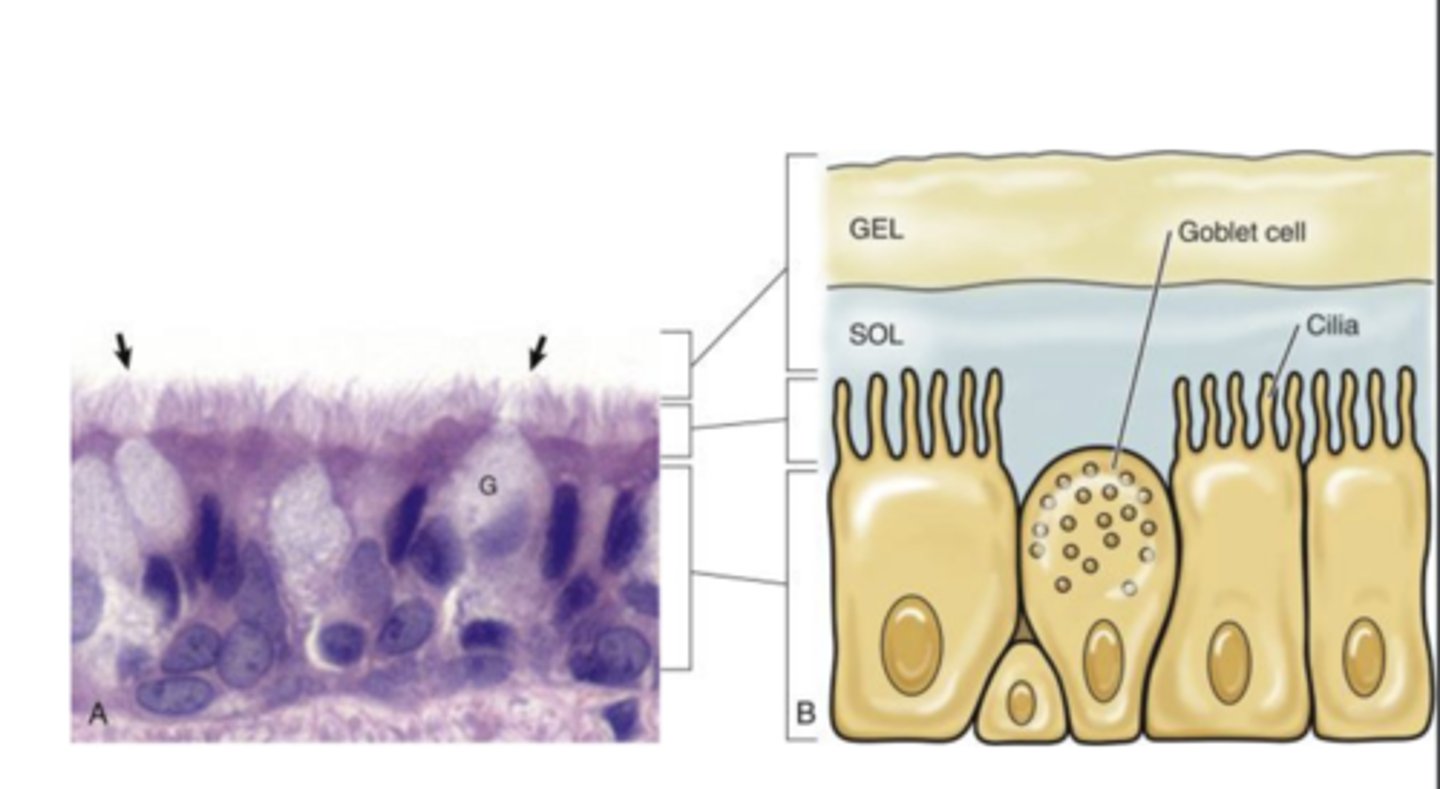
what is the mucociliary apparatus? what does it do?
hair-like structures on the outside of epithelial cells
- physically clears pathogens
what population experiences the highest prevalence of AOM?
pediatric population
- ages 3-24 months
- ~50% will have 1+ ear infections by 2 yo
incidence of AOM has decreased over time due to the introduction of...?
pneumococcal immunizations (early 2000s)
describe the main steps of the pathophysiology that leads to AOM
① viral upper respiratory tract infection
② mucociliary apparatus and eustachian tube dysfunction
③ fluid buildup behind the tympanic membrane
④ impaired clearance by mucociliary system
⑤ bacteria from the nasopharynx become trapped in fluid
⑥ AOM
T/F: viruses are the most common cause of AOM
FALSE
- only ~20% of cases are caused by viruses alone
- ~80% of infections are bacteria
what are the most common viral and bacterial causes of AOM?
- viral: coronavirus, respiratory syncytial virus (RSV), adenovirus
- bacteria: most often upper respiratory tract colonizers; Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis
describe Streptococcus pneumoniae as a cause of AOM
gram-positive cocci in chains
- colonizes mucosal surfaces of the respiratory tract
- preventable through vaccination
describe Haemophilus influenzae as a cause of AOM
gram-negative coccobacilli
- facultative anaerobe
- preventable through vaccination (during childhood)
describe Moraxella catarrhalis as a cause of AOM
gram-negative diplococcus
- colonizes the upper respiratory tract
what are the common risk factors of AOM?
- daycare attendance
- bottle-feeding
- smoking (and second-hand smoke)
- age 3-24 months old
- FH
- Hx of atopy
describe the clinical presentation of AOM
- fever
- otorrhea (ear drainage)
- otalgia (ear pain)
- reduced hearing
- bulging tympanic membrane (ear drum)
- tinnitus (ear ringing)
- vertigo
what are the non-specific indicators of AOM, especially as seen in young children?
- crying
- irritability
- ear tugging
- sleep difficulties
what are the diagnostic criteria for AOM?
middle ear effusion AND
moderate-severe bulging of the tympanic membrane OR new onset otorrhea that is NOT due to AOM
OR
middle ear effusion AND
mild bulging of the tympanic membrane AND onset of ear pain within 48 hours or intense erythema of the tympanic membrane
what are the common complications of AOM?
rare but serious complications:
- hearing loss
- tympanic membrane rupture (may require surgical repair)
- mastoiditis
- CNS infections (bacterial meningitis, intracranial or epidural abscesses)
what is sinusitis? what is acute bacterial rhinosinusitis (ABRS)?
inflammation of the paranasal sinuses
- ABRS: bacterial infection in the paranasal sinuses AND nasal mucosa
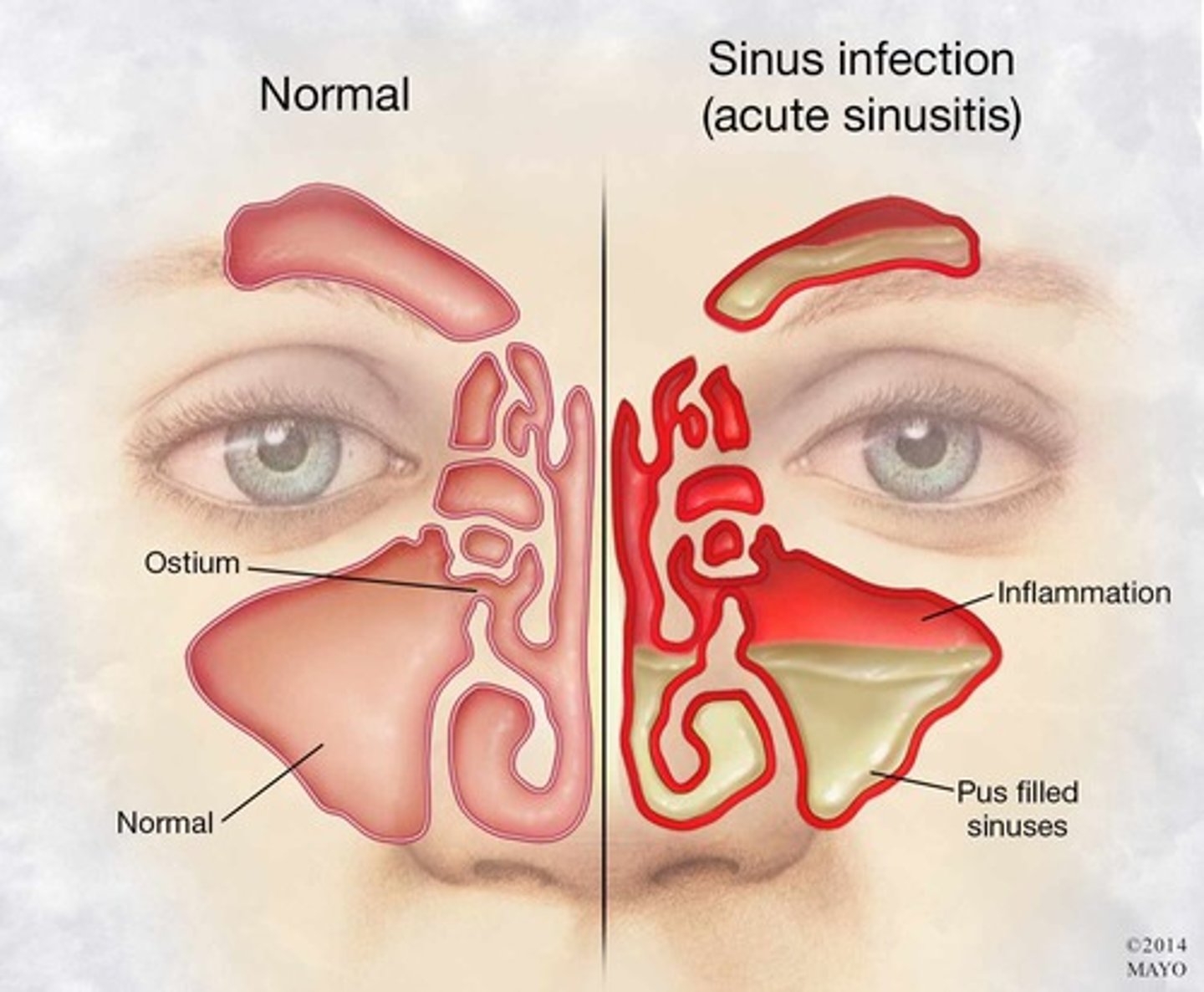
what is the criteria for acute, recurrent acute, and chronic ABRS?
- acute: ≤4 weeks of purulent nasal drainage with nasal obstruction, fascial pain, pressure, or fullness
- recurrent acute: ≥4 episodes per year of ABRS
- chronic: ≥12 weeks of 2+ Sx AND 1+ objective evidence of inflammation
what population has the highest prevalence of ABRS?
adults
- ~12% of the adult population is affected
- associated with high rates of overprescribing ABX!
describe the basic pathophysiology that leads to ABRS
① viral upper respiratory tract infection
② mucosal inflammation, edema, and thickened nasal secretions
③ obstruction of the pathways that drain the sinuses
④ trapping of mucosal secretions and impaired host defenses
⑤ bacterial proliferation
⑥ ABRS
what viruses are often associated with causing sinusitis?
can be viral alone, or predecessor of bacterial infection
- rhinovirus
- influenza
- coronavirus
- respiratory syncytial virus (RSV)
- adenovirus
what bacteria are often associated with causing sinusitis?
most often upper respiratory tract colonizers;
- nosocomial (HC-associated) pathogens are possible, but uncommon: P. aeruginosa, MRSA
- S. pneumoniae
- H. influenzae
- M. catarrhalis
what are the common risk factors for ABRS?
- smoking (and second-hand smoke)
- air travel/exposure to atmospheric pressure changes
- swimming (especially in chlorinated pools)
- asthma
- allergies
- immunocompromised
describe the clinical presentation of ABRS
- purulent nasal drainage
- facial pain, pressure, fullness
- nasal congestion
- HA
- fever
- dental pain
- ear pain
what clinical manifestations are indicative of bacterial sinusitis vs. viral sinusitis?
bacterial
- HIGH fever (≥102 F)
- persistent signs/Sx for ≥10 days
- "double-worsening" (Sx improve then worsen within 10 days)
viral
- afebrile or LOW fever
- Sx peak at 3-6 days
- Sx resolve within 10 days
what are some complications associated with ABRS?
rare but serious complications:
- CNS infections (bacterial meningitis, intracranial or epidural abscesses)
- orbital complications (cellulitis, abscesses, thrombophlebitis)
- osteomyelitis
what is pharyngitis? what is acute pharyngitis (AP)?
inflammation of the pharynx
- AP: acute infection of the oropharynx or nasopharynx
what populations have the highest prevalence of AP?
pediatric patients
- school-aged children AND their parents
- seasonal outbreaks in the winter and spring!
describe the basic pathophysiology that causes AP
① microbes invade the pharyngeal mucosa
② altered host immunity
③ excess secretions and edema
④ acute pharyngitis
T/F: viruses cause the majority of AP cases
TRUE
- account for 70-80% of cases while bacteria only account for 20-30%
what viruses cause AP?
- rhinovirus
- coronavirus
- adenovirus
- HSV
- influenza and parainfluenza viruses
- EBV
what type of bacteria is most commonly associated with AP?
Strep. pyogenes (Group A Strep)
- aka strep throat!
- gram-(+) cocci in pairs or chains that colonizes the surfaces of the respiratory tract
- produces a toxin that helps evade the hose immune system
what are the risk factors for AP?
- younger age (5-15 yo)
- sick contacts
- immunocompromised
- smoking
- overcrowding
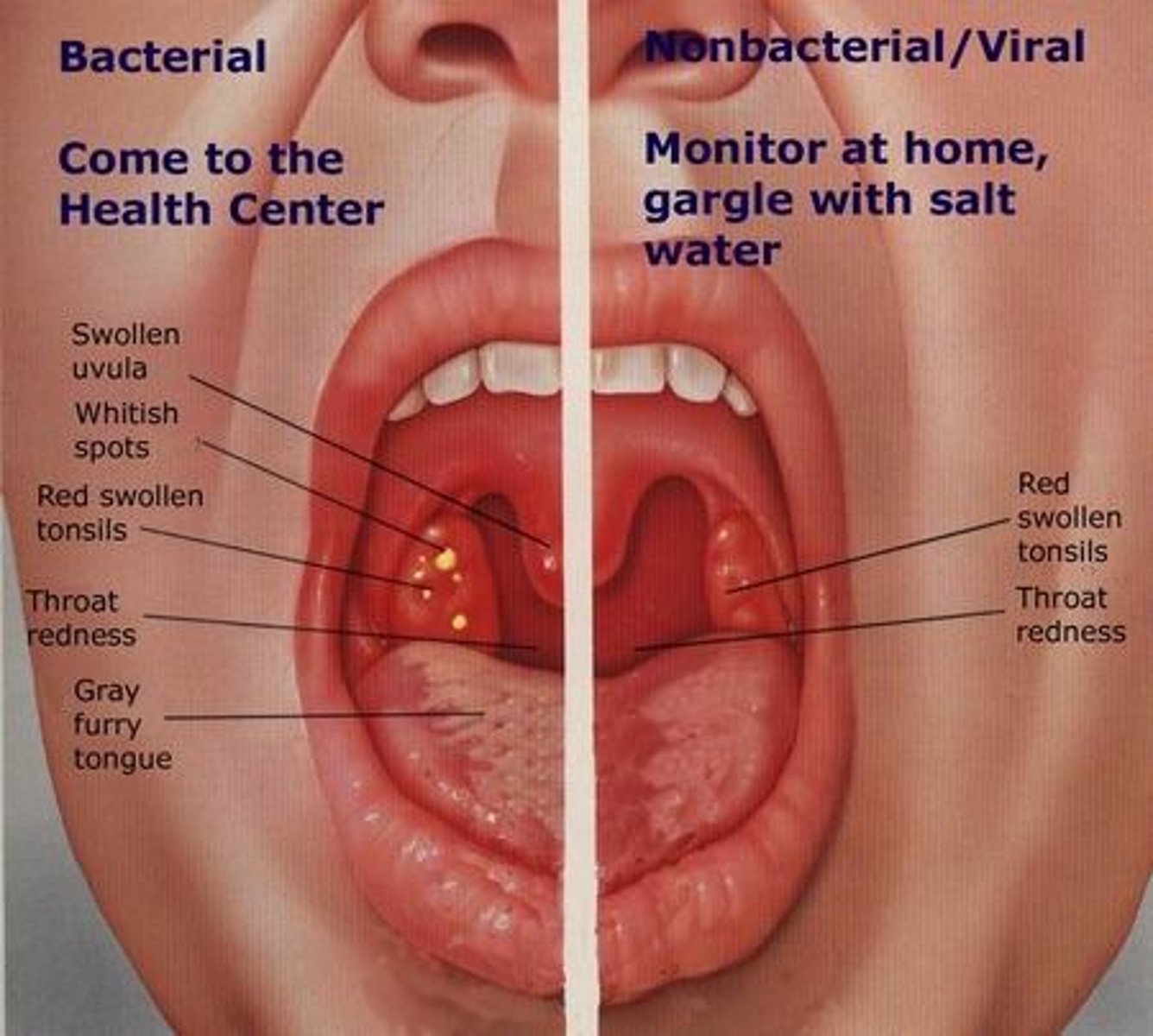
describe the clinical presentation of AP
- sore throat
- pain when swallowing
- fever
- HA
- swollen uvula, petechiae (purple spots) on soft palate, scarlatiniform rash (redness)
what is the FIRST test performed on a patient with suspected AP?
throat swab
- used for a rapid Ag detection test (RADT)
AP - what is the diagnosis if a throat swab returns positive?
GAS acute pharyngitis
AP - what are the next steps if a throat swab returns negative?
throat culture
- if (+), diagnose GAS acute pharyngitis
- if (-), diagnose viral acute pharyngitis
what are the complications of AP?
rare but serious complications:
- peritonsillar abscess/phlegmon
- mastoiditis
- cervial adenitis
- AOM
- thrombophlebitis of the internal jugular veins (Lemierre's Syndrome)!