Spinal Cord Injury
1/108
Earn XP
Description and Tags
Yowch My Back :(
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
109 Terms
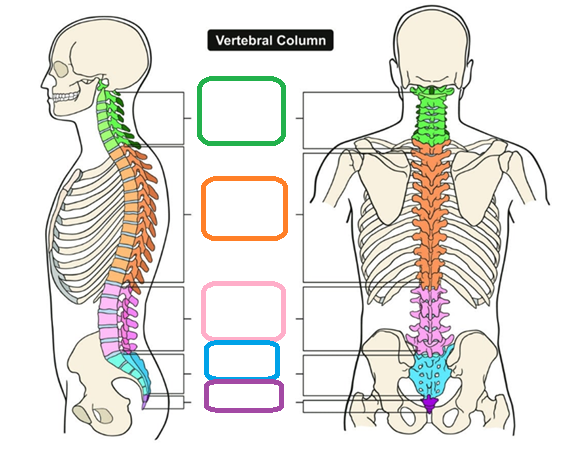
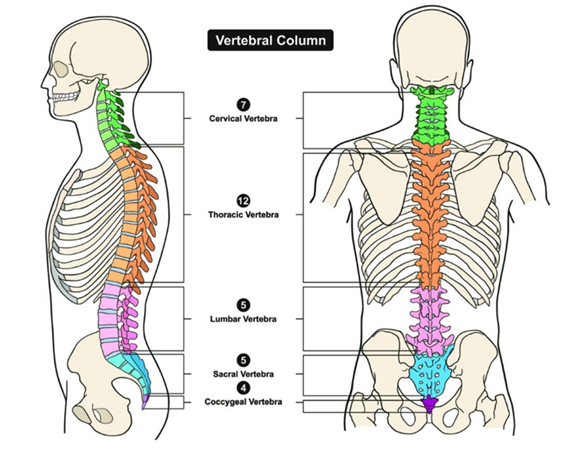
Spinal Cord
Extends from _________ to ____
_____ pairs of spinal nerves
Diameter?
Ending components?
Extends from foramen magnum to L2
31 pairs of spinal nerves
Diameter?
Cervical enlargement → Supplies upper limbs
Lumbar Enlargement → Supplies lower limbs
Ending components?
Conus medullaris → Ending, tapered. Between L1 and L2
Cauda Equina → Origin of spinal nerves from conus medullaris
What portion of the spinal cord supplies the upper limbs?
Cervical enlargement
What portion of the spinal cord supplies the lower limbs?
Lumbar enlargement
Conus Medullaris
Inferior ending of spinal cord
Ends between L1 and L2
Cauda Equina
Origin of inferior spinal cords
Extends from conus medullaris
Membrane layers of the meninges
Dura meter → Strong, outer layer
Arachnoid mater → Thin, non-vascular
Pia mater → Inner layer, tightly bound to spinal cord
Dura mater
Layer of meninges
Strong and tough
Outer layer, continuous
Arachnoid mater
Layer of meninges - Middle
Thin, non-vascular
Pia mater
Layer of meninges
Inner layer
Tightly bound to spinal cord
Epidural space
OUTSIDE of dura mater
Anesthetics injected here
Fat-filled for padding
Subdural space
Between dura and arachnoid
Filled with serous fluid
Subarachnoid space
Between Pia and arachnoid
Filled with CSF
Spinal anesthesia is injected here
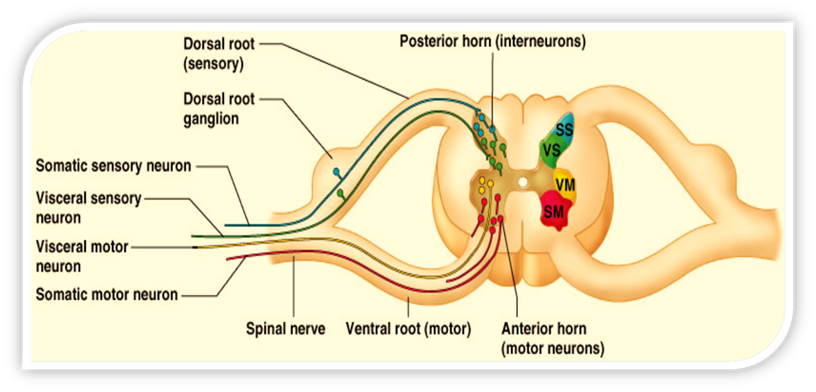
Grey matter
neuron cell bodies, dendrites, and axons
Divided into horns
Posterior
Anterior
Lateral
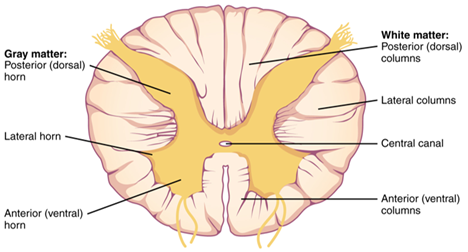
White matter
Myelinated axons
3 columns
Ventral
Dorsal
Lateral
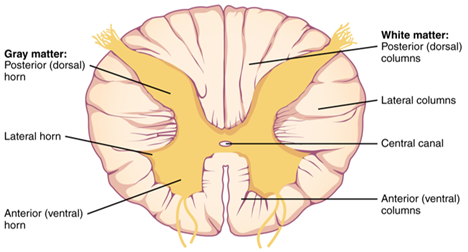
Posterior horn of spinal cord
Sensory roots and ganglia
“Dorsal half”
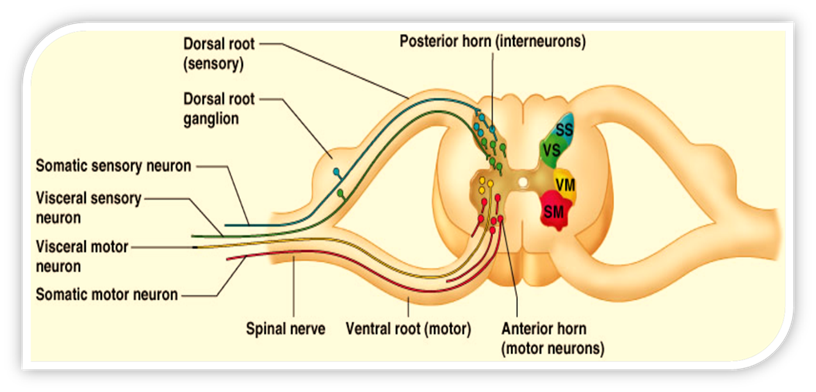
Anterior horn of spinal cord
Motor roots
“Ventral half”
True or false:
Spinal cord injuries and their associated changes are always permanent
FALSE
Can be temporary or permanent
Only type of 100% permanent spinal cord injury → SEVERED
Leading cause of traumatic spinal cord injuries
Motor vehicle crashes
Primary spinal cord injury
Initial physical trauma
Unlikely for the severity of it to be changed by surgery or any other interventions
Examples:
Spinal cord compression
Penetrating trauma
Secondary Spinal Cord Injury
Ongoing and progressive damage - Occurs after and as a result of initial injury
Can be prevented/altered with nursing care!!!
Occurs minutes to hours after initial injury
Edema → Cord compression → Ischemic damage → Neuron destruction
Glial scar
Glial scar
Secondary spinal cord injury
From inflammatory response
Physical barrier to nerve communication → Irreversible nerve damage
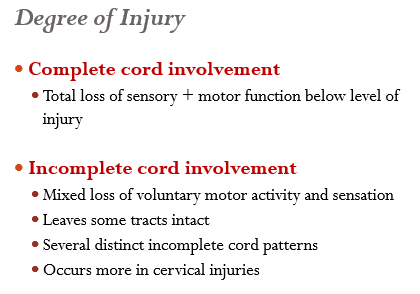
Spinal cord injuries are classified by…
Mechanism of injury
Level of injury
Degree of injury
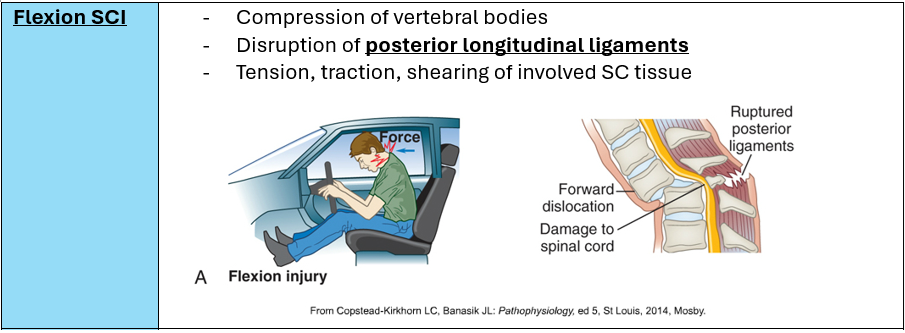
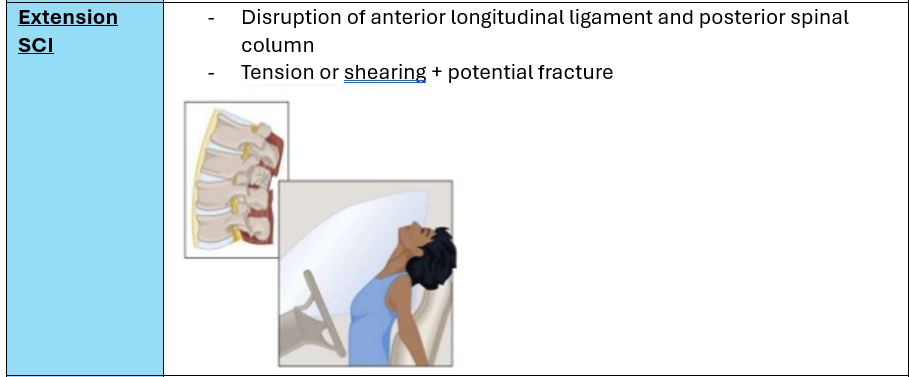
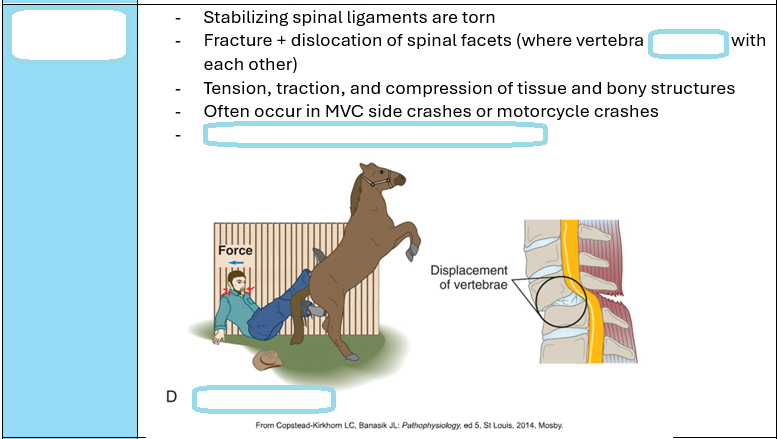
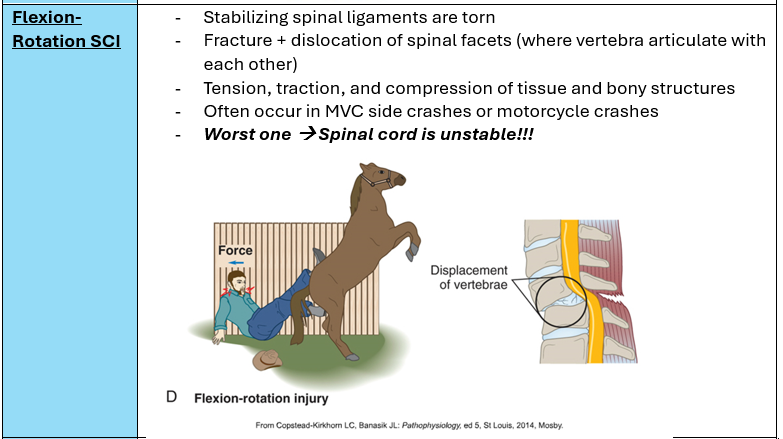
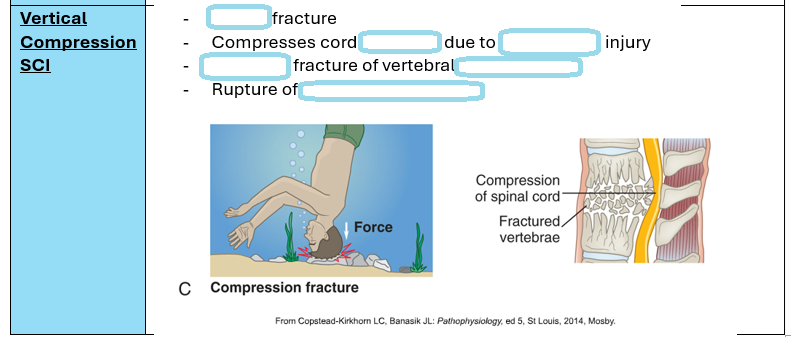
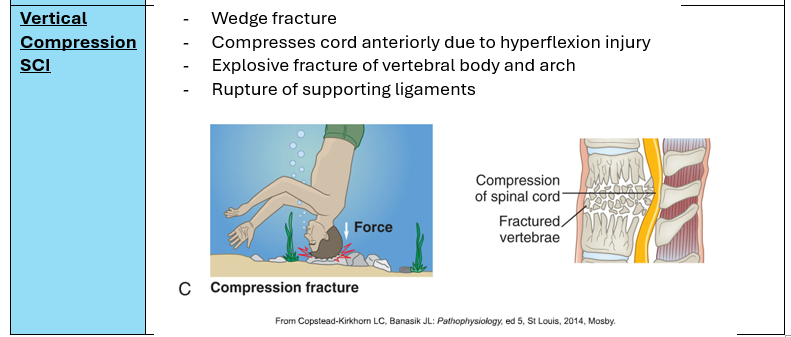
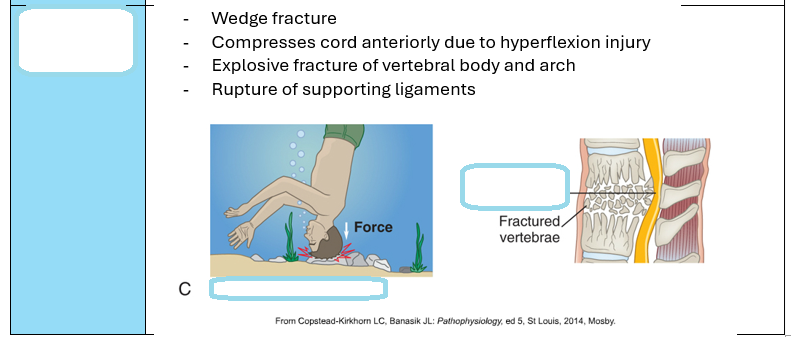
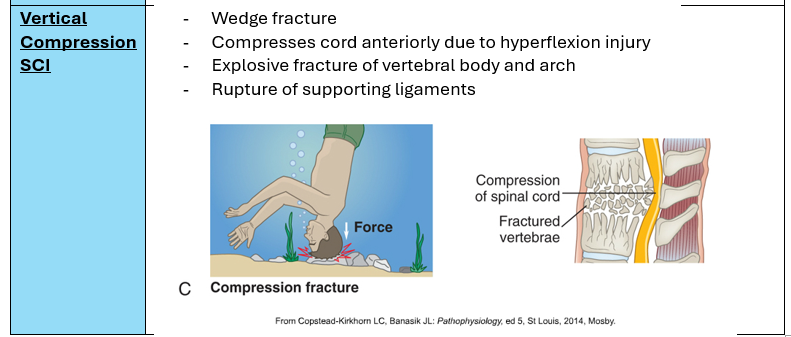
Major mechanisms of spinal cord injury
Flexion
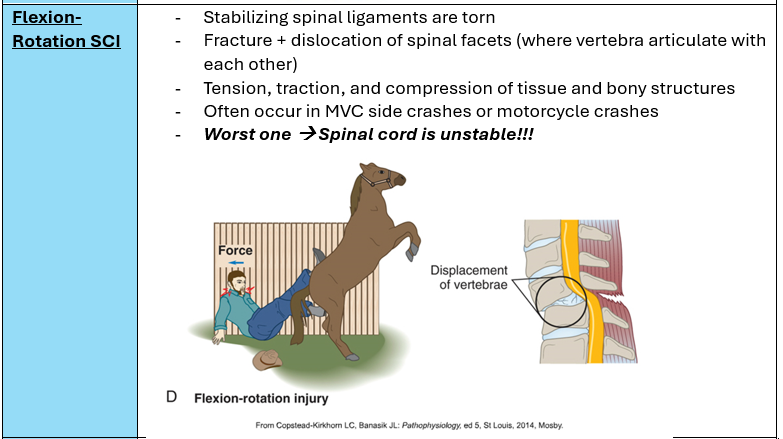
Flexion-Rotation
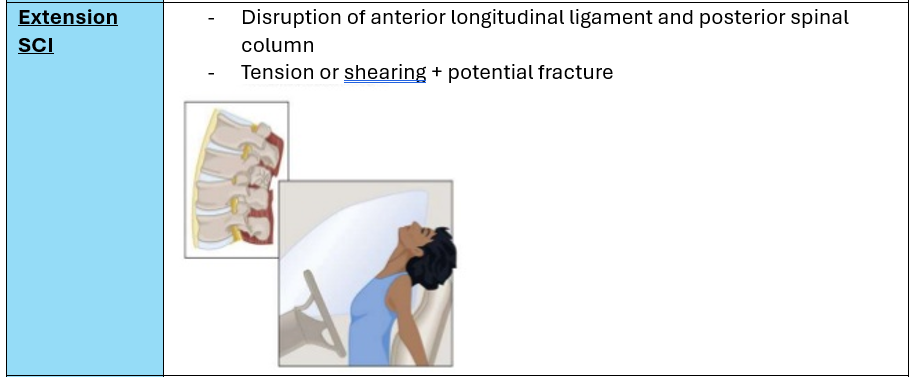
Hyperextension
Rotation
Vertical compression
What mechanism of spinal cord injury is the most unstable?
Flexion-rotation
Can lead to severe neuro deficits
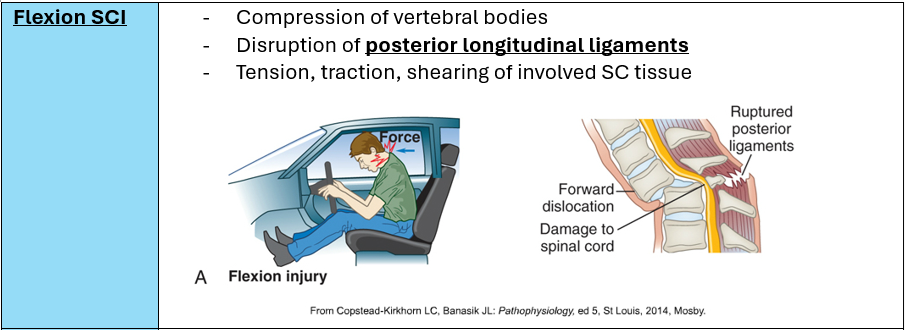
Flexion Spinal Cord Injury
Compression of vertebral bodies
Levels of spinal cord injury
Skeletal → Where the most damage to vertebra and ligaments is
Neurological → Damage to the cord itself
Determine the lowest segment of cord with normal function
Skeletal vs Neurological level of injury
Skeletal
Where the vertebra, ligaments, and supporting structures have the most damage
Neurological
The lowest segment on the spinal cord that has normal functioning
Everything below that level is impacted by the injury
How to determine the neurological level of injury
Test sensory and motor function on both sides
True or false
The skeletal and neurological level of injury are not always the same
True
A spinal cord injury between C1 and T1 results in…
Tetraplegia
Involvement of all 4 extremities
Arms may be completely or partially paralyzed/involved, but lower injury is generally better
A spinal cord injury below T2 results in…
Paraplegia
Lower extremities affected\
Potential for total independence 🙂
A spinal cord injury between ___ and ___ results in tetraplegia
C1 and T1A
A spinal cord injury below ___ results in paraplegia
T2
Are most spinal cord injuries generally complete or incomplete?
Incomplete!
What type of bony injury results in a singular break of spinous or transverse processes, and alignment of spinal cord generally remains intact?
Simple fracture
May cause later spinal column instability!!!
What bony injury occurs when one vertebrae overrides another?
Dislocation
May have unilateral or bilateral facet dislocation
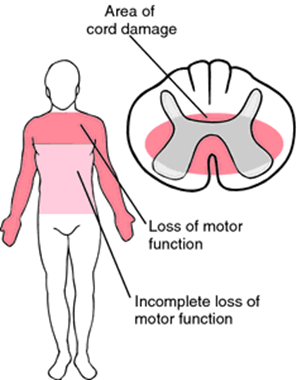
Incomplete vs Complete cord involvement
Incomplete → More common, mixed loss of function/activity
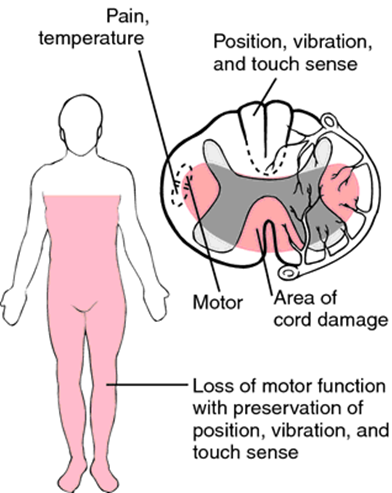
Anterior cord syndrome
Injury details?
Impaired functions?
Intact functions?
Flexion injury w/ anterior cord compression
Damage to anterior spinal artery → Compromises blood flow to cord
Impaired functions:
Motor paralysis
Loss of pain and temperature sensation below level of injury
Intact functions:
Touch, position, vibration, and motion sensations
Central cord syndrome
Damage to _____ cord
Most commonly occurs in the _____ region
More common in what population?
Upper extremities?
Lower extremities?
Damage to central cord
Most commonly occurs in the cervical region
Neck hyperextension
More common in older adults w/ degenerative disease
Motor weakness + altered sensation in upper extremities
Lower extremities usually not affected
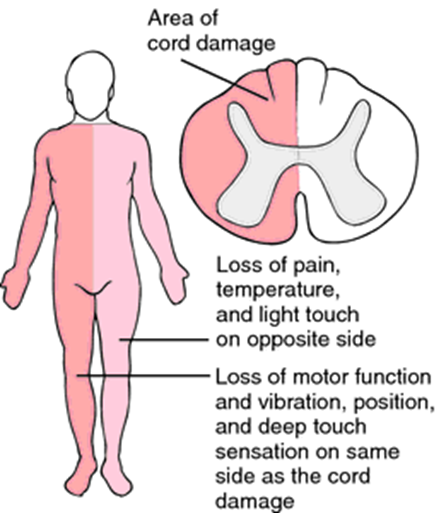
Brown-Sequard Syndrome
Rare
Damage to half the cord
Usually caused by penetrating injury
Same side of body as injury
Loss of motor function, light touch, pressure, position, vibration sense
Opposite side of body as injury
Loss of pain, temperature sensation
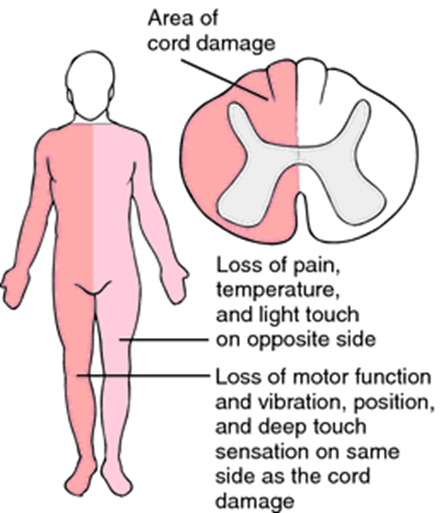
What rare incomplete spinal cord injury is often caused by penetrating injuries?
Brown sequard syndrome
What is useful for determining where the spinal cord injury occurred and is used when testing sensory function?
Dermatomes → Dividing and assigning body areas to vertebral levels
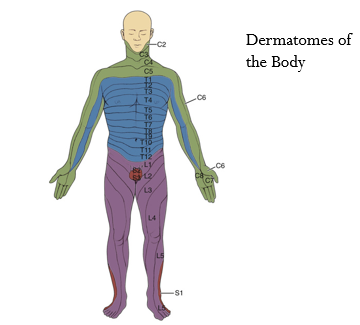
Classification of SCI severity
Testing motor and sensory function
Sensory
Light touch/pinprick along dermatomes
Strength grading of muscles on both sides + motor function
Categories
A = Most severe
E = Least severe
Emergency management of a spinal cord injury
ABCs!!
Ensure patent airway + respirations
Cervical injury → No head-tilt or chin lift
Keep SaO2 > 90% → Administer O2
Stabilize the cervical spine → Prevent further damage
Other things → Assess for other injuries, obtain imaging
Immobilization of spine
Maintain ______ position
Keep patient ______
Materials:
Turning → _______
Use ______________ if needed
Spinal immobilization should not interfere with __________
Maintain neutral position
Materials:
Rigid cervical collar
Backboard with straps
Keep patient supine
Turning → Log-roll
Use reverse trendelenburg if needed
Spinal immobilization should not interfere with resuscitation
If a patient has a suspected spinal cord injury, what should we also suspect?
Head injuryyy
What characteristics make a SCI patient a possible early surgery candidate?
Cord compression
Open/Compound fracture
Penetrating wounds
Bony fragments in cord
Progressive neurologic deficit
Purpose of skeletal traction
NOT long term!
Keep cervical spine in alignment until a permanent solution is developed
Spinal reduction/decompression
True or false:
Gardner-Wells tongs require pin site care due to a risk for potential infection
FALSE
Typically short term
No pins!
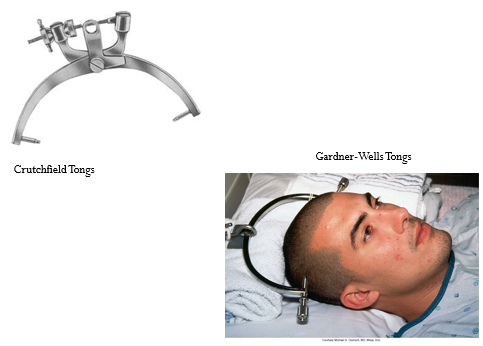
Skeletal traction
Short term - No pins!
Usage of weights (10 pounds, then 40-70 lbs)
Spinal decompression/reduction
Crutchfield or Gardner-Wells tongs
Halo Vest
Used for immobilization with spinal fractures
Allows movement and ambulation while bones fuse
Pin Site Care
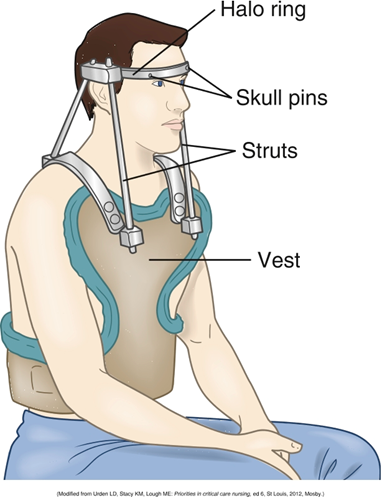
Contraindications of halo vest
Ligament instability
Morbid obesity
Older age
Cachexia
Non-compliance
Pin site care for Halo Vest
Risk for infection!!!
Chlorohexidine swabs twice a day
Antibiotic ointment
What immobilization method is used for stable thoracic or lumbar spine injuries?
“Body Jacket”
Thoracolumbar sacral orthosis TLSO
Limits spinal flexion, extension, and rotation
Requires meticulous skin care!!!
What immobilization method is used for unstable thoracic or lumbar spine injuries?
Surgery → Decompression and fusion +
TLSO (body jacket)
Lumbosacral orthosis LSO
Spinal cord injuries above ___ and ____ result in the requirement for mechanical ventilation
C3 and C4
How do spinal cord injuries above C3 and C4 impact respiratory ability?
Unable to breathe independently/spontaneously
Mechanical ventilation ☹
How do spinal cord injuries below C4 impact respiratory function?
Diaphragmatic breathing (if phrenic nerve is functional)
Loss of intercostal and abdominal muscles → Hypoventilation
Intubation might be needed
Other interventions
Monitor for labored breathing, poor cough, or exhaustion
Administer O2
Chest physiotherapy to clear secretions
Respiratory assessment of spinal cord injury patients
Breath sounds
ABGs
Uncomplicated = PaO2 >60, PaCO2<45
Skin color (pallor, cyanosis)
Breathing patterns
Sputum
Ability to count to 20 without taking a breath
What are cardiovascular effects that may occur as a result of spinal cord injury?
Unopposed vagal response
Vagal stimulation may lead to
Bradycardia
Risk for cardiac arrest
Loss of SNS in Peripheral vessles
Chronic hypotension
Orthostatic hypotension
Risk for VTE
Possible impacts on the cardiovascular system in spinal cord injuries?
a. Bradycardia
b. Chronic hypertension
c. Stroke
d. Cardiac arrest
A, C, and D
Unopposed vagal response → Bradycardia and cardiac arrest
Loss of SNS in peripheral vessels → Chronic hypotension, orthostatic hypotension, and VTE risk
Why might a patient with a spinal cord injury be at risk for bradycardia and cardiac arrest?
Unopposed vagal response
Avoid vagal stimulation
Why might spinal cord injury patients be at risk for chronic hypotension or venous thromboembolism?
Loss of Sympathetic nervous system control in peripheral vessels
If a patient has symptomatic bradycardia, what is the expected treatment?
Atropine and/or pacemaker
In spinal cord injury patients, systolic BP should be kept _____ and MAP should be ______
In spinal cord injury patients, systolic BP should be kept above 90 and MAP should be between 85-90
A spinal cord injury at __ and above results in orthostatic hypotension in patients.
A spinal cord injury at T6 and above results in orthostatic hypotension in patients.
A spinal cord injury at T6 and above results in _________ in patients.
A spinal cord injury at T6 and above results in orthostatic hypotension in patients.
If a SCI patient has symptomatic orthostatic hypotension, what are important nursing interventions?
Abdominal binder
Graduated compression stockings
Midodrine → Venous return
What medication is suggested for orthostatic hypotension?
Midodrine
VTE prophylaxis
Low-molecular-weight heparin or low-dose heparin
SCDs and/or graduated compression stockings
Assess thighs and calves every shift
ROM exercises + stretching
Urinary retention and SCI
Immediately following injury
Neurogenic Bladder → Loss of autonomic + reflex control of bladder and sphincter
Acute → Indwelling catheter
Long-term → Intermittent catheterization
True or false:
For long-term management of neurogenic bladder, indwelling catheters are used.
FALSE
Acute phase → Indwelling catheter
Long-term → Intermittent catheterization
Chronic catheter increases infxn risk
SCI and GI system:
T5 → _____________
T12 → _____________
T5 → GI hypomotility
Paralytic ileus
Gastric distension
T12 → Neurogenic bowel
Loss of sphincter control/reflexes
SCI and GI system
__ → GI hypomotility
__ → Neurogenic bowel
T5 → GI hypomotility
Paralytic ileus
Gastric distension
T12 → Neurogenic bowel
Loss of sphincter control/reflexes
When a T5 injury impacts GI function…
What are complications?
Nursing management?
Results in GI hypomotility
Can cause paralytic ileus and gastric distension
Interventions:
NG tube, intermittent suction
PPI or H2 receptor blockers (omeprazole, famotidine)
T12 injury and GI function
Neurogenic bowel → Loss of voluntary control
Can also occur during spinal shock
Bowel is areflexic
Decreased sphincter tone
Interventions:
When reflexes return → BOWEL PROGRAM
Aids in sphincter toning, and reflex emptying
When is bowel program initiated?
Neurogenic bowel
Following spinal shock
SCI at T12 or below
When reflexes return!
Decreased thermoregulation is more common in patients with…
High cervical injury
Decreased thermoregulation
More common w/ high cervical injuries
Decreased ability to sweat or shiver below the level of injury
Don’t over cool or overheat the patient!

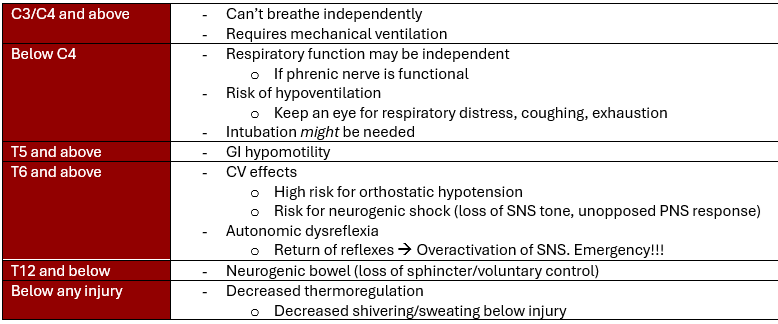
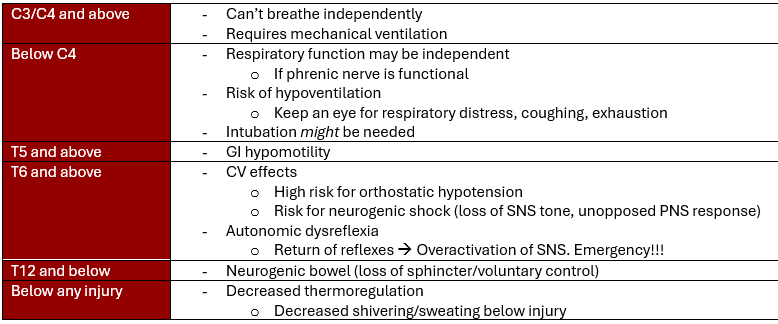
Neurogenic Shock
T6 or higher SCI
Loss of SNS tone → Unopposed PNS response
Distributive shock!!!!
Peripheral vasodilation
Reduced venous return, pooling of blood in veins, loss of pressure
Hypotension
Decreased cardiac output
Bradycardia
From loss of sympathetic tone/muscle contractility
Fluid infusions may not help
Vasopressors may be indicated
Norepi, phenylephrine, dopamine
Spinal shock
½ of all SCI pts
Immediate loss of function below level of injruy
Loss of Deep tendon/sphincter reflexes
Loss of sensation
Flaccid paralysis (including bowel/bladder)
Lasts 1-6 weeks post injury (normally, can be faster)
After spinal shock
Lasts days to weeks, usually 1-6 weeks post injury
Spinal neurons gradually regain excitability → Ending of spinal shock
May mask post-injury neurologic function
We won’t know their true ability/severity until spinal shock ends
Don’t know if it will be permanent!
Autonomic dysreflexia
T6 or above
Occurs following spinal shock
Returning reflexes → Get out of wack!
SNS excitement/overactivation, PNS can’t respond
MEDICAL EMERGENCY!
How is autonomic dysreflexia often caused?
Identification and elimination of inciting stimulus can lead to resolution
Usually caused by distended bladder, rectum, tight clothing/shoes
How does autonomic dysreflexia occur?
strong sensory input below injury
SNS below level of injury responds with arteriolar vasoconstriction and increased BP
PNS unable to fully counteract, but may lead to bradycardia
Manifestations of Autonomic Dysreflexia
Hypertension
20-40 above systolic baseline, but may reach up to 300
Nasal congestion
Bradycardia
PNS is trying to respond to HTN
If these are reported, check BP!!!
Throbbing headache
Spots/Blurred visual field
Anxiety and nausea
Piloerection (goose bumps) BELOW level of injury
Diaphoresis and Skin flushing ABOVE level of injury
Treatment of Autonomic Dysreflexia
FIRST: Elevate head of bed 45 degrees or high-fowlers
Search for cause
Immediate catheterization → Bladder distension
Check indwelling
Remove skin stimuli → Tight clothes/shoes
Rectal exam after applying anesthetics → Stool impaction
Notify provider
Antihypertensive meds
NTG, nitroprusside, hydralazine
What treatment may decrease or eliminate ventilator requirements in patients with high SCI?
Implanted phrenic nerve stimulator
Electronic diaphragmatic pacemakers
What treatment may decrease or eliminate ventilator requirements in patients with low level SCI?
Respiratory muscle training
Abdominal binders
Overall → Improving performance of respiratory muscles