Exercise Rx for Individuals w/ CVD
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
22 Terms
cardiac rehabilitation (CR)
-used to deliver exercise and other lifestyle interventions to individuals with cardiovascular disease (CVD)
*if have known CVD OR if at high risk for heart attack and get intervention
oTypically delivered in outpatient settings (also inpatient)
oReduces rate of mortality and morbidity and health care costs
oMedicare and private insurance reimbursements for MI/acute coronary syndrome, CABG, PTCA, stable angina, valve repair/replacement, CHF, and heart transplant.
Ischemia vs Infarction
-Ischemia: at risk for a heart attack, blocked coronary arteries but no permanent damage yet
-Infarction: heart attack, damage to the heart, maladaption to future work
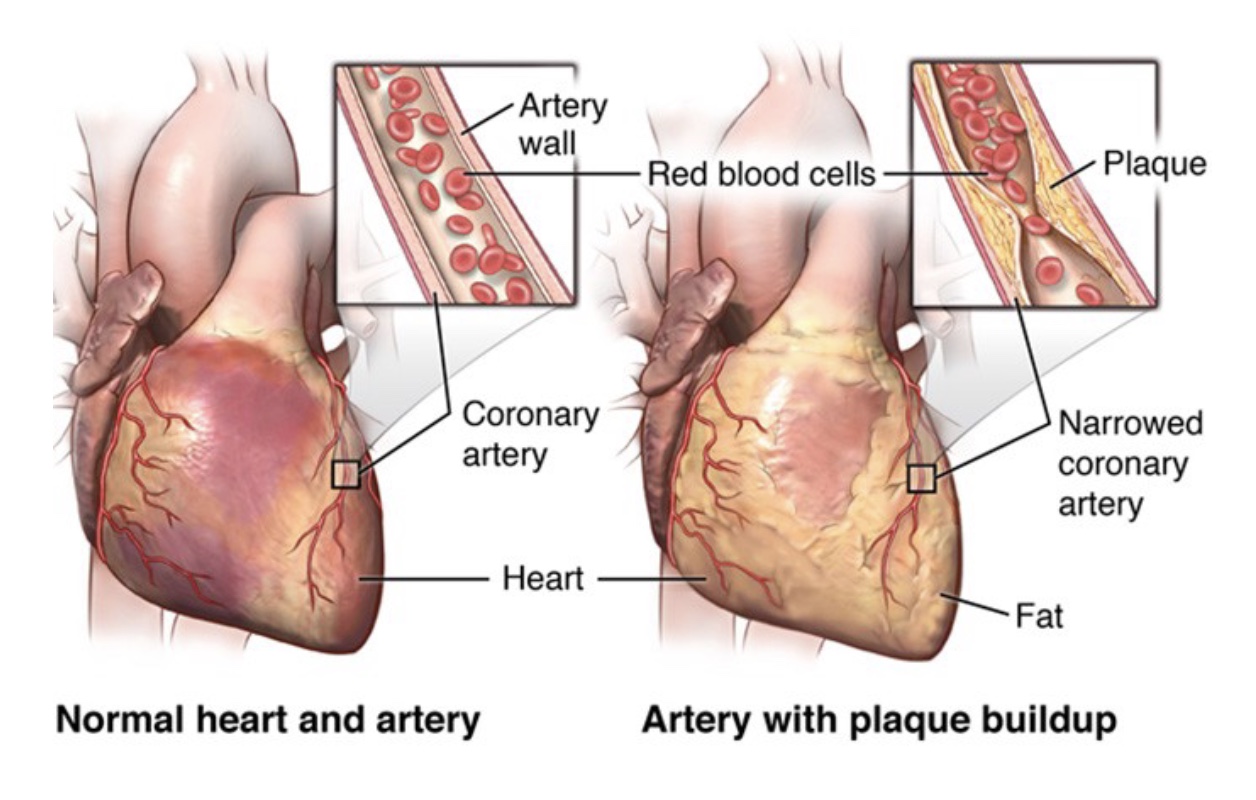
Coronary Artery Disease
-CA off the aorta, supply heart with O2/blood
-plaque builds up in the CA and disrupts blood flow, so heart has to work harder
-heart attack if tissue death
-likely if smoke, have obesity, etc.
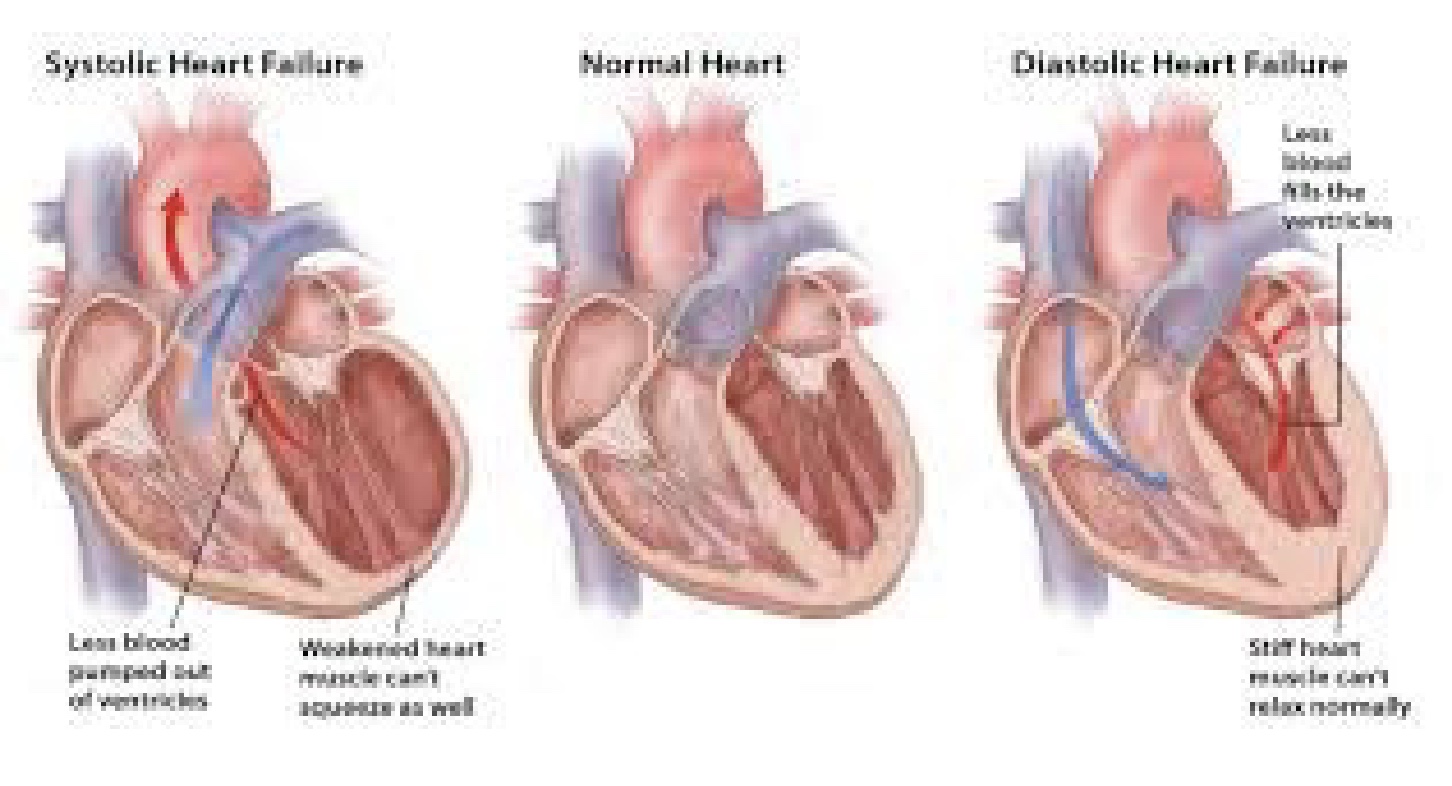
Heart Failure
-no longer squeezing adequately so inability to maintain Q and can’t meet metabolic demands of body
-50% mortality rate next 5 years
*previous injury so at high risk; more likely in older aged people who show signs
Systolic Heart Failure
-big chambers, so can’t generate enough force to get blood out
-more seen in older aged
-treat w/ high contractility using meds, pacemakers, etc. (easier to treat)
Diastolic Heart Failure
-ventricle really thick, so small chamber and squeez well but not fill well; significant afterload
-hard to treat bc can’t make chamber bigger
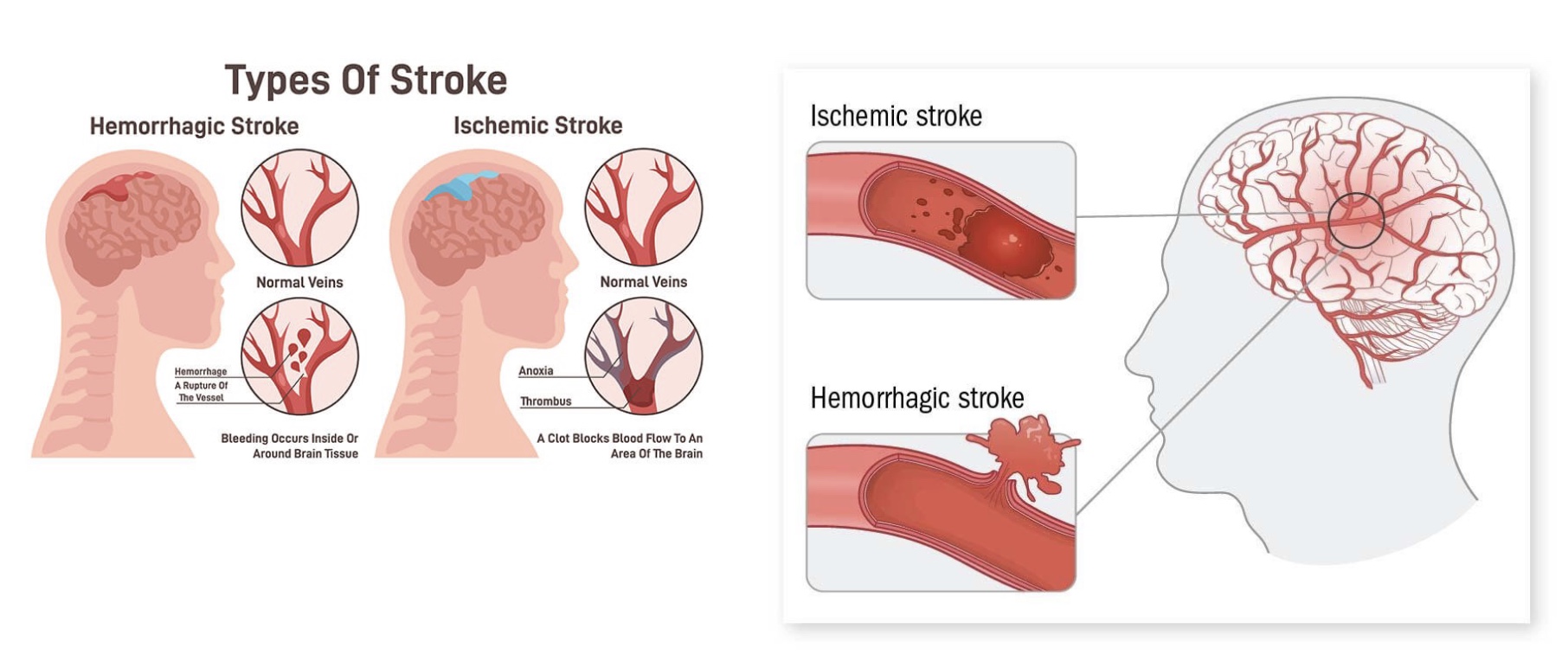
Stroke
-disrupt blood flow to brain; causes disfunction so need rehab
-Hemorrhagic Stroke: vessel ruptures, brain bleed, swelling
-Ischemic Stroke: clot formation; treat with powerful clot medicine
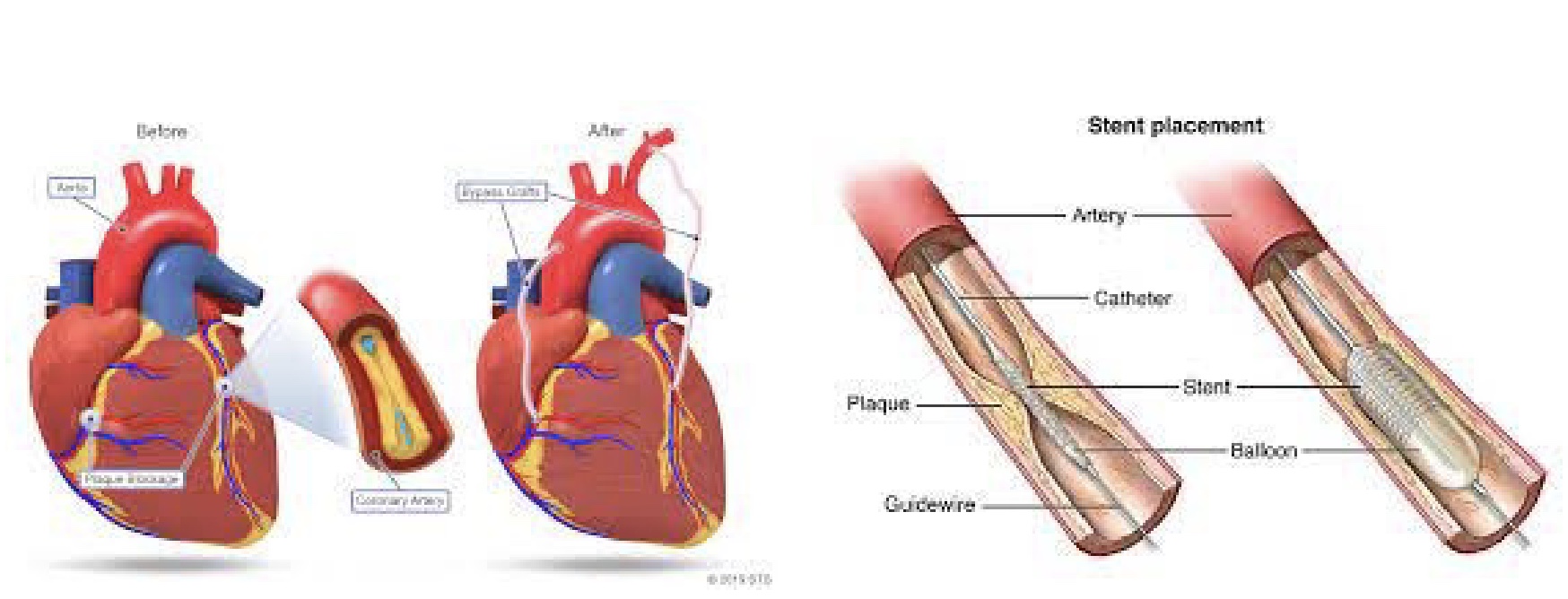
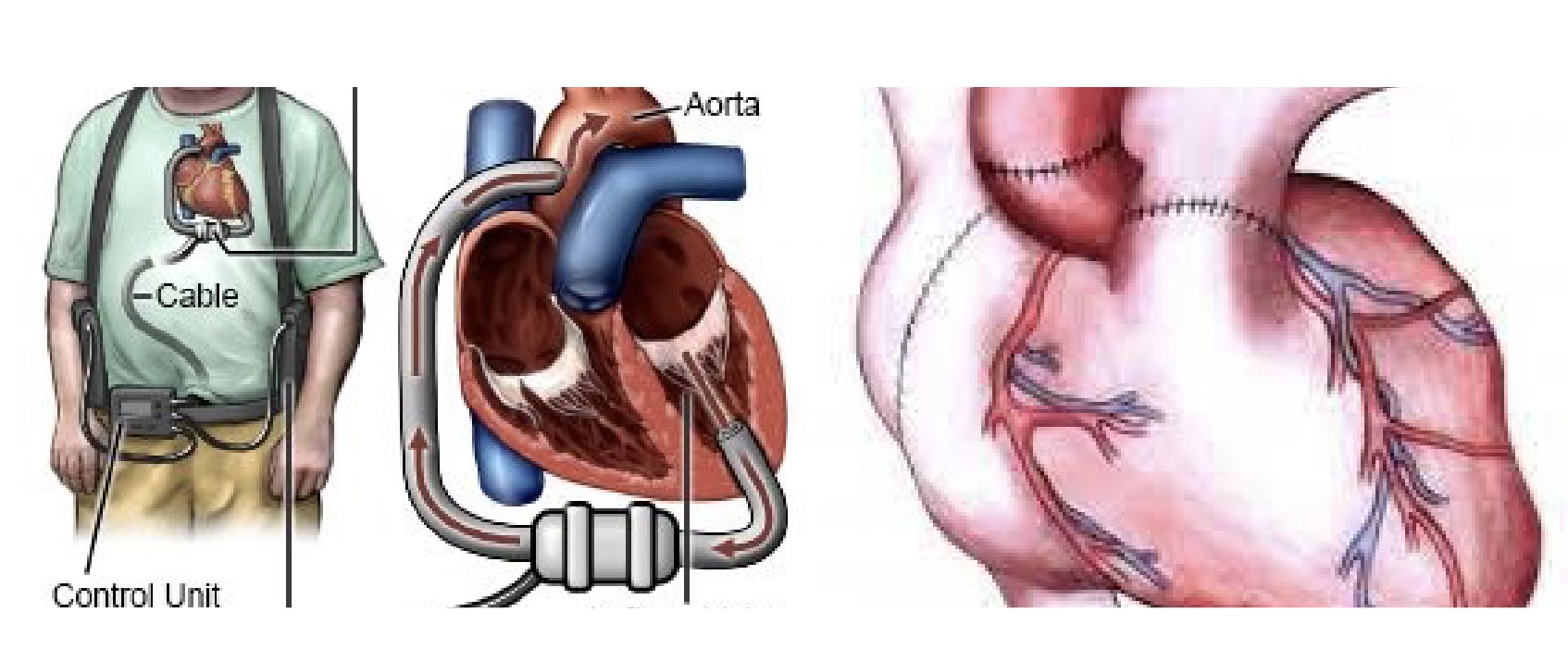
Revascularization: Bypass graft vs Ballon Stent
Bypass graft
-open up sternum and sew on bypass vessel from aorta to coronary artery; more invasive
-longer to recover from, but less restenosis rate
Balloon Stent
-catheter and stent and balloon, “angioplasty”
-restores blood flow
-invasive but quick, but not not good if multi-vessel
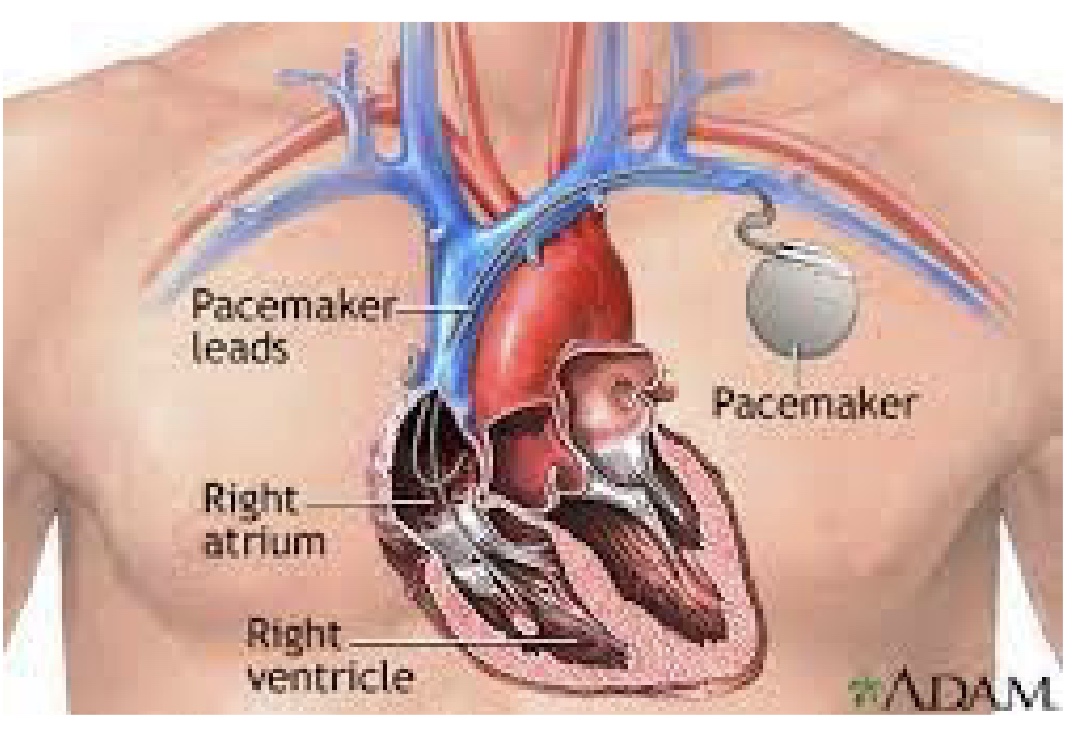
Pacemaker/ICD
-if have a primary arrhythmia
-generates cardiac rhythm for the heart
-exercise Rx depends on pacemaker
1) what is the HR response?
2) don’t want to damage the pacemakers
Ventricular Assist Device vs Heart Transplant
Ventricular Assist Device
-bridge to transplant; higher Q; bypasses heart as pump
-now smaller and battery run, but make sure battery doesn’t run out!
-can adjust the pump rate
-Exercise Rx complicated bc based on the pump
Heart Transplant
-no longer have NS intervention (no response SNS and PSNS)
-HR response really different
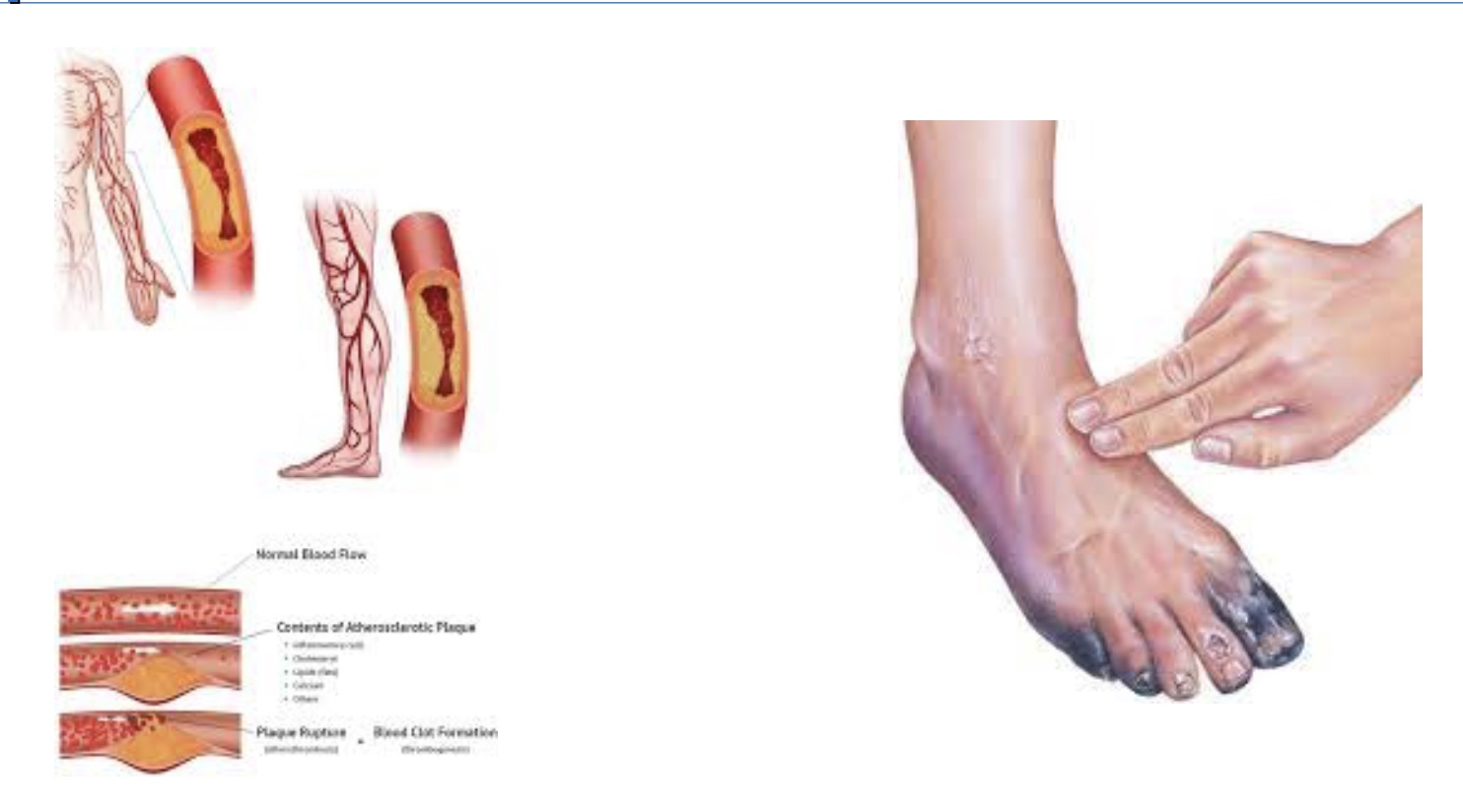
Peripheral Arterial Disease
-lack good blood flow to arms, legs, and vital organs
-skin lost and amputations
-exercise Rx like CV or Type II diabetes
guidelines for inpatient CR program
oCurrent clinical status assessment (*limitations, stable)
oMobilization (*1st thing test; orthostatic work like increase HR and BP when stand)
oIdentification and provision of information regarding modifiable risk factors and self-care
oDischarge planning with a home PA and ADL (*expectations when go home)
oReferral to outpatient CR
*attentive audience
Inpatient Cardiac Rehab clinical assessments and supervised daily ambulation
-Clinical assessments: diagnosis, current medical status, comorbidities, CVD risk factors, personalized goals, and readiness for PA (risk stratification) and learning
-Supervised daily ambulation (indications/contraindications should be considered)
oInclude assessment and documentation of vital signs (*monitor all times)
oIntermittent sitting or standing within 12–24 hours of MI may prevent exercise performance decrements.
oNo defined optimal dose – progress from self-care activities, ROM, and postural changes to limited supervised walking
*can they get dressed by self? go to the bathroom on their own?
Inpatient Cardiac Rehab education
-EDUCATION: modifiable risk factors, lifestyle changes, and self-care should occur once the individual’s physical ability and psychological willingness to learn is assessed
oAssess knowledge of disease and treatment
oDetermine preferred learning style
oCommunicate in lay terms
oExpand knowledge with use of technology, visual aids, and family involvement
*redefine them as a heart patient now
Inpatient Cardiac Rehab: upon hospital discharge + caustion
-Upon Hospital discharge =
ocomprehensive plan of care and educational materials (*including exercise Rx)
oPsychosocial and socioeconomic issues, such as access to care, risk of depression, social isolation, and health care disparities
oSafe, progressive plan of exercise
-CAUTION:
oUntil evaluated with an exercise test or entry into a clinically supervised outpatient CR program, the upper limit of HR or RPE noted during exercise should not exceed those levels observed during the inpatient program.
oIndividuals should be counseled to identify abnormal signs and symptoms suggesting exercise intolerance and the need for medical evaluation.
*chest pain? shortness of breath? dizzy? heart racing may be normal
oAll eligible individuals should be strongly encouraged to participate in a clinically supervised outpatient CR program.
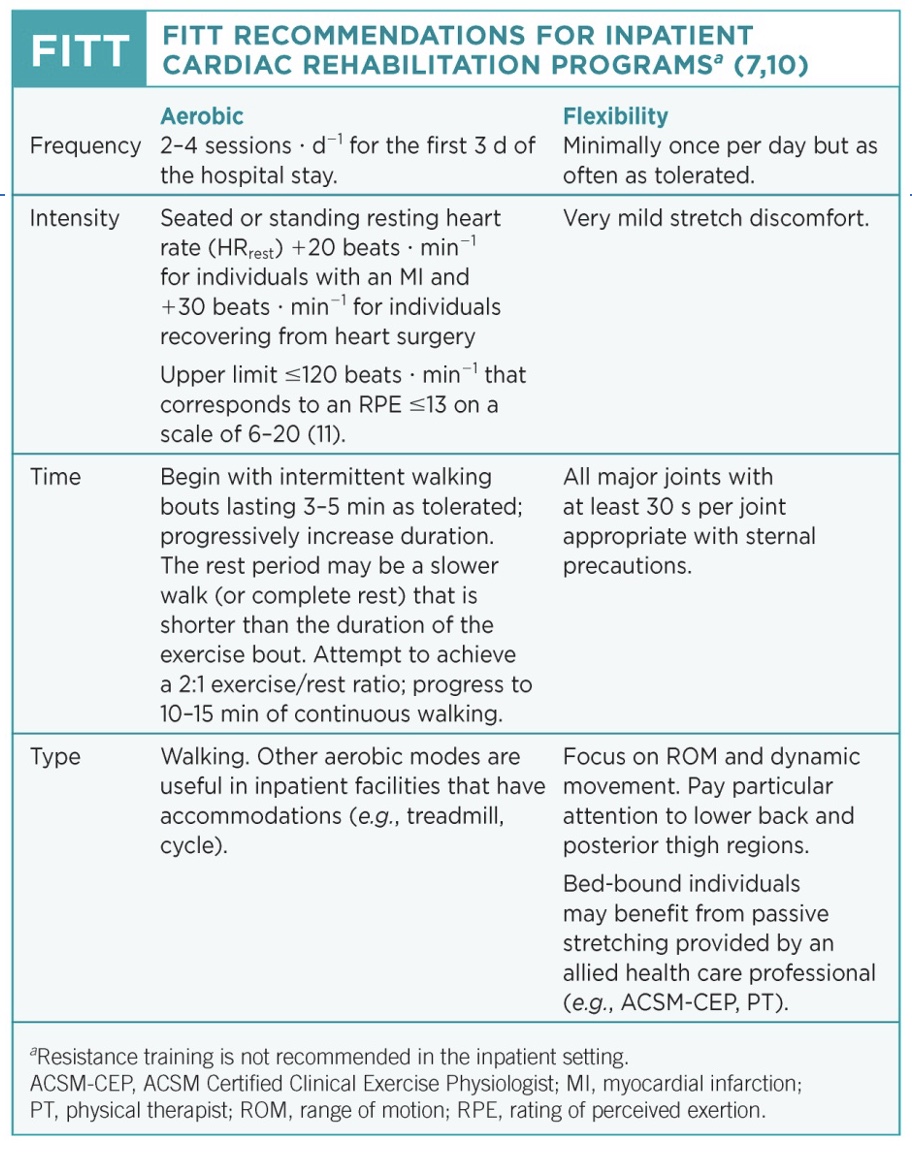
Inpatient Cardiac Rehab FITT
-aerobic: +20beats/min means responding well, don’t work really hard; 3-5minutes as tolerates; walking
-flexibility
Outpatient Cardiac Rehab: at time of referral
-At the time of physician referral or program entry, the following assessments should be performed:
oMedical and surgical history including the most recent cardiovascular event, comorbidities, and other pertinent medical history
oPhysical examination with an emphasis on the cardiopulmonary and musculoskeletal systems
*taking meds? HR and BP before and during exercise
oReview of recent CV tests and procedures including.. 12-lead electrocardiogram (ECG), coronary angiogram, echocardiogram, stress test, cardiac surgeries or percutaneous interventions, and pacemaker/implantable defibrillator implantation
*do submax test 4-5 days post, and max 2-3 weeks post
oCurrent medication routine/dose/frequency
oCVD risk factors
*want constant improvements
Outpatient cardiac rehab routine pre-execise assessment
-Routine preexercise assessment of risk for exercise should be performed before, during, and after each rehabilitation session, as deemed appropriate by the qualified staff and include the following:
oHR, BP, and weight
*weight big concern if dramatic weight gain bc could be retained fluid/edema
oSymptoms or evidence of change in clinical status not necessarily related to activity (e.g., dyspnea at rest, light-headedness or dizziness, palpitations or irregular pulse, chest discomfort)
oSymptoms and evidence of exercise intolerance
oChange in medications and adherence to the prescribed medication regimen
oECG and HR surveillance for accurate rhythm detection
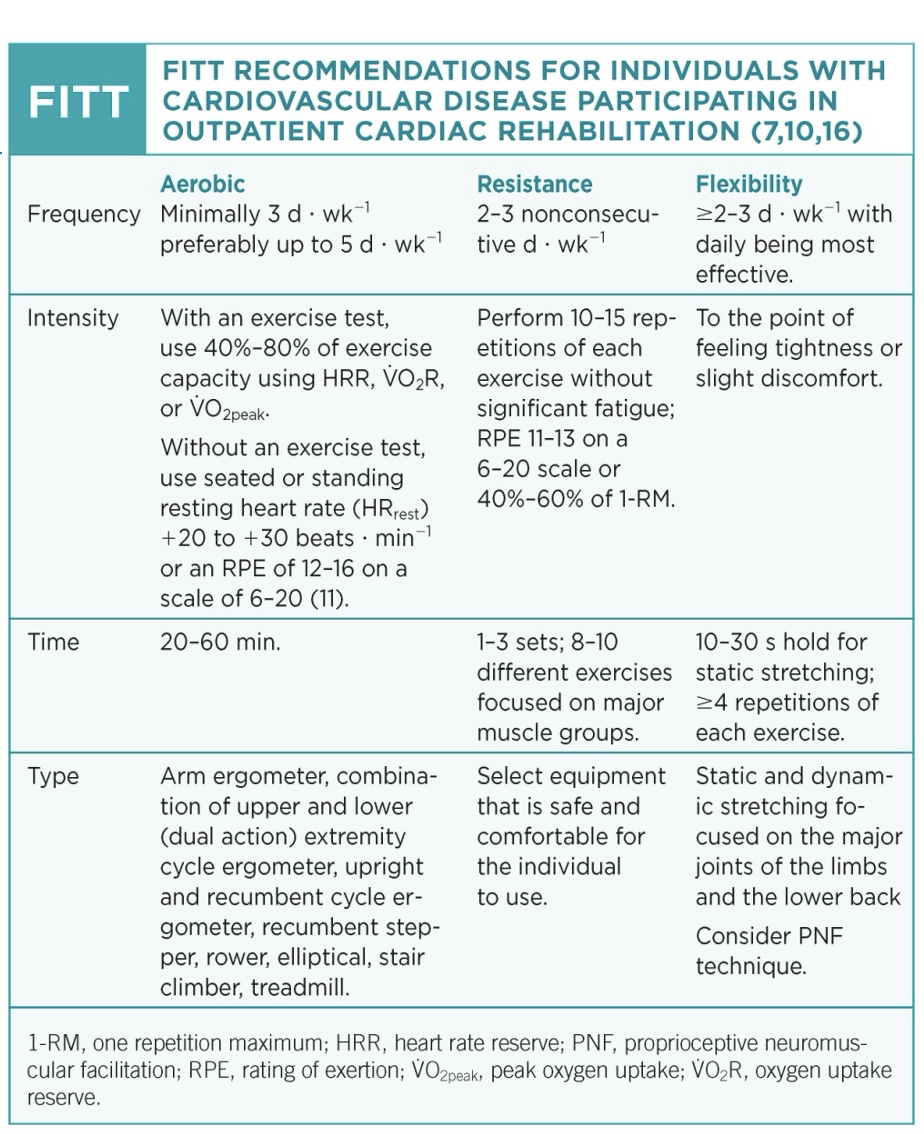
Outpatient cardiac rehab FITT
-aerobic: 3-5 days/week; 40-80% of capacity; 20-60 min
*now can have a formal Rx; daily activities of aerobic work
-resistance: added, when depends on surgery (ex: if cut open no RT for 6-8 weeks)
-flexibility: bc tight UB
Outpatient cardiac rehab Exercise Training Considerations
-For individuals with very limited exercise capacities, daily bouts <10 minutes may be considered as a starting point, with a goal of increasing over time.
*ejection fraction as low as 20-30% (normally 50-60%); hope EF rebounds but might not
-If an ischemic threshold has been determined, the exercise intensity should be prescribed at an HR of 10 beats · min−1 below the HR at which the event was identified
-If peak HR is unknown, the RPE method should be used to guide exercise intensity using the following relationships: (*education important!)
o<12 (<3 on CR10 Scale) is light or <40% of HRR
o12–13 (4–6 on CR10 Scale) is somewhat hard or 40%–59% of HRR
o14–16 (7–8 on CR10 Scale) is hard or 60%–80% of HRR
-Individuals on a b-blocker may have an attenuated HR response to exercise and an increased or decreased maximal exercise capacity.
oFor individuals who have had a b-blocker dose change, monitor signs and symptoms and establish a new target for exercise intensity.
-It is recommended that an exercise test be performed any time that symptoms or clinical changes warrant.
-Individuals on diuretic therapy are at an elevated risk for volume depletion, hypokalemia, or orthostatic hypotension particularly after bouts of exercise.
*so urinate a lot of fluid, heart works less but low BP and electrolyte risk (thus give K+ pills)
-The aerobic exercise portion of the session should include rhythmic, large muscle group activities with an emphasis on increased caloric expenditure for maintenance of a healthy body weight and its many other associated health benefits.
Ischemic threshold
-point heart works were risk goes extremely up
-determined with a controlled max test
-exercise Rx should be below the ischemic threshold (~10 bpm)
*can give beta blocker if needed
true or false: exercise RX can be set based on HR even if the patient is on a beta-blocker
true!
-can still set up Rx based on HR, but need to know their peak HR w/ a max test
-if don’t know their HR max, then different story
Outpatient Cardiac Rehab: Continuous EKG monitoring
-continue until known stable CVD and low risk for complications
Takeaways outpatient cardiac rehab
-Although a symptom-limited GXT prior to CR is ideal in the development of an exercise program, it is not common.
-Ex Rx procedures: based on recommendations of guidelines and what was accomplished during the inpatient phase.
-6-MWT or other forms of submaximal exercise tests: can be a measurement of exercise tolerance and capacity
*if tolerate well can progress; if can’t need more conservative Rx
-RPE: practical method for prescribing both aerobic and resistance exercises
-The individual should be educated on and closely monitored for signs and symptoms of intolerance (excessive fatigue, dizziness or light-headedness, chronotropic incompetence, and signs and symptoms of ischemia).
*educate on how to take care of themselves and their risk!