(2) Acute vs. Chronic Inflammation, Apoptosis vs. Necrosis
1/88
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
89 Terms
secreted proteins that function as mediators of immune and inflammatory reactions
cytokines
What secretes cytokines? (4)
macrophages, NK cells, T cells, endothelial cells
2 examples of cytokines
TNF, ILs
family of low molecular weight cytokines that stimulate leukocyte movement and regulate migration of leukocytes from blood to tissues
chemokines
severe immune reaction in which the body releases too many cytokines into the blood too quickly
occurs as a result of an infection, autoimmune condition, or other disease; includes fever, inflammation, fatigue, and nausea, and it may be severe or life-threatening and lead to multiple organ failure
cytokine storm
Which leukocytes are responsible for the initial response in acute inflammation?
neutrophils
Is it more common for acute inflammation to be resolved or progress to chronic inflammation?
resolved
True or false: If acute inflammation doesn't result in resolution and regeneration, then it undergoes repair, which forms a scar.
true
What is the most common outcome of acute inflammation?
resolution
What is the most common outcome of chronic inflammation?
scarring
What are 3 effects of acute inflammation? (Hint: pertains to blood vessels, leukocytes present, and other chemicals present)
vascular changes, neutrophil recruitment, mediators
What are 3 effects of chronic inflammation? (Hint: pertains to blood vessels, leukocytes present, and histologic consequences)
angiogenesis, fibrosis, mononuclear cell infiltrate (along with B & T cells)
What are two possible outcomes of chronic inflammation?
scarring, regeneration
Which outcome of chronic inflammation is more common: scarring or regeneration?
scarring
(results in dense fibrosis & loss of function)
What are two examples of tissues that can undergo regeneration back to normal after chronic inflammation?
liver, GI epithelium
How long does acute inflammation last?
few minutes to few days
How long does chronic inflammation last?
few days to years
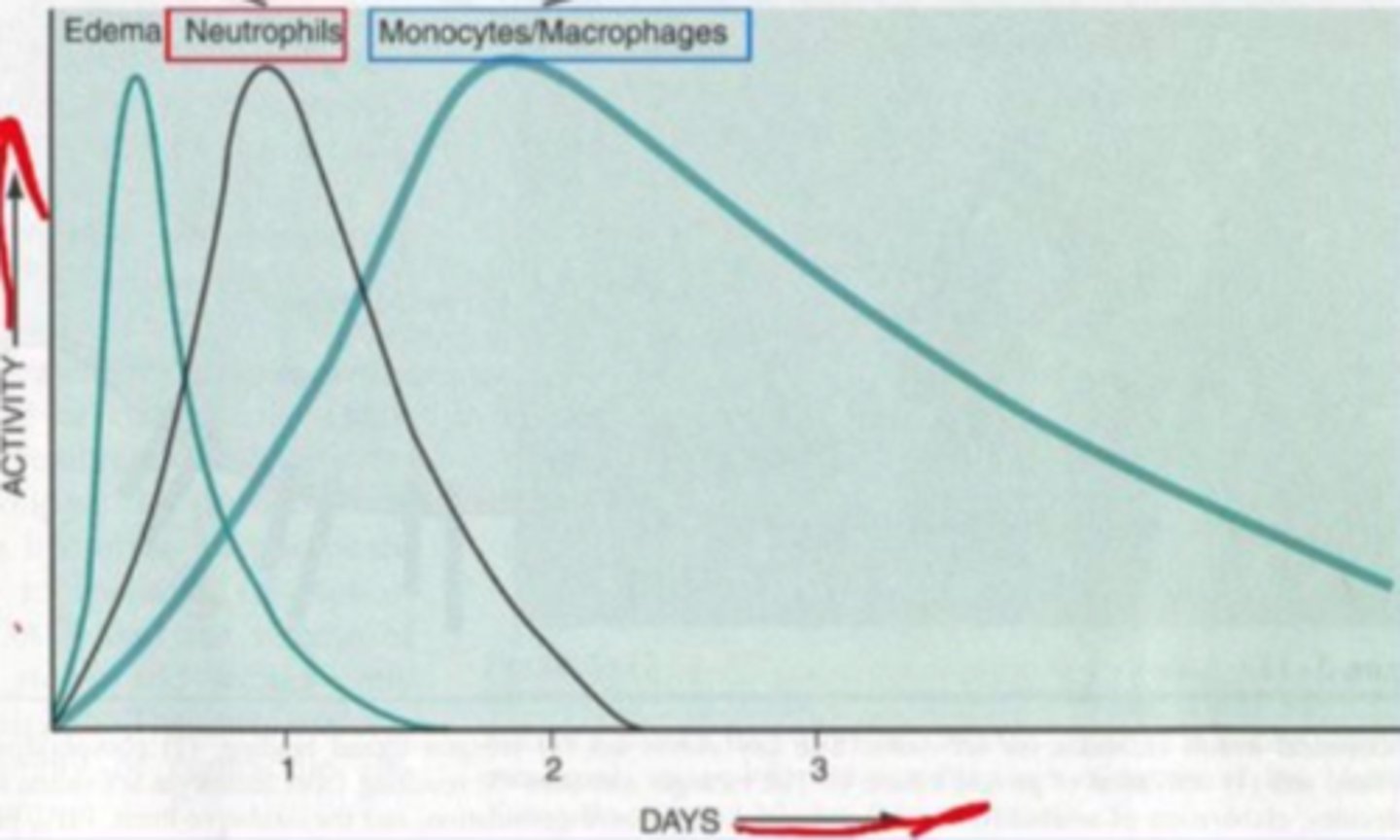
What is the first thing that happens in the inflammatory response?
edema
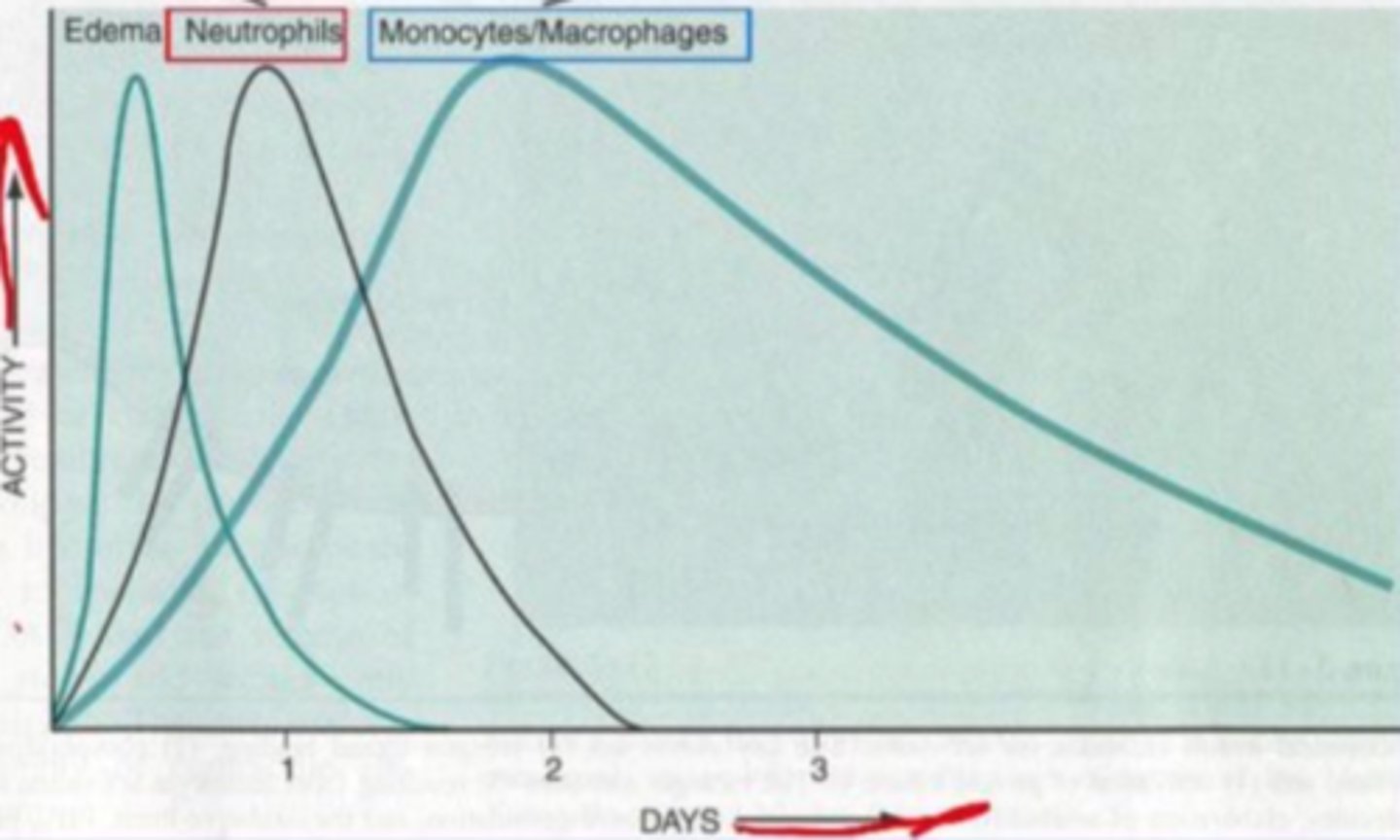
When do neutrophils peak in the inflammatory response?
24 hours
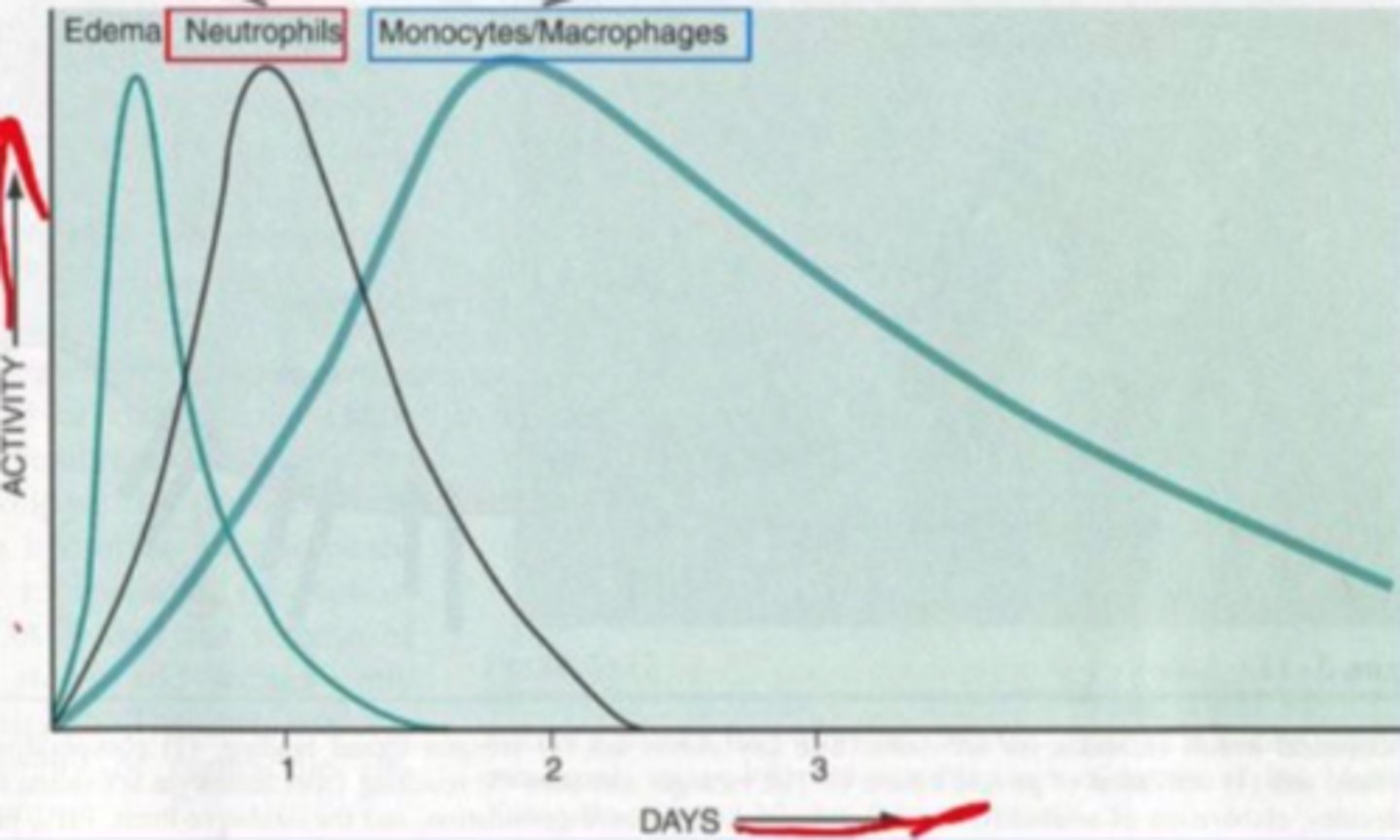
When do monocytes/macrophages peak in the inflammatory response?
2 days
(but they can stay elevated for a while after that)
What are the 2 main vascular changes that occur in acute inflammation?
vasodilation, increased capillary permeability
What are the 3 main cellular events that occur in acute inflammation?
leukocyte extravasation, accumulation, activation
What happens in the initial inflammatory response: vasodilation or vasoconstriction?
vasodilation
(to bring plasma proteins and leukocytes to the area)
Why does edema occur first thing in inflammation?
increased capillary permeability results in extravasation of fluid and plasma proteins
fluid that accumulates in a wound; may contain serum, cellular debris, bacteria, and white blood cells
exudate
refers to acute inflammation that involves increased fluid accumulation; basically is a skin blister with fluid edema directly beneath the epidermis
serous inflammation
refers to acute inflammation that involves fibrin leaking out of vessels, which occurs in body cavity linings and tissues
fibrinous inflammation
refers to acute inflammation that involves abscesses forming and the accumulation of pus
suppurative inflammation
What makes up pus? (3)
neutrophils, edema, necrotic cell debris
refers to an inflammatory response that is so destructive it destroys tissue in that area, causing that necrotic issue to shed
ulceration
Upon injury, before vasodilation occurs to start the inflammatory response, there is actually a transient vasoconstriction response that happens first. Why?
don't want excess blood leaking out
(which would lead to a hemorrhage)
Upon injury, does blood flow to the area get faster or slower?
slower
(due to increased vascular permeability - more fluid flowing out of capillaries, so more blood is leaving than flowing through the vessels)
refers to leukocytes starting to gather near the affected area upon injury that will eventually result in extravasation
leukocyte margination
Does capillary hydrostatic pressure increase or decrease during inflammation?
increase
(due to vasodilation, resulting in more blood flow to capillaries)
Does capillary osmotic pressure increase or decrease during inflammation?
decrease
(due to more plasma proteins leaking out into interstitial fluid as a result of increased permeability)
Typically, acute inflammation is resolved. When this resolution occurs, where does the excess fluid (edema) drain into?
lymphatic vessels
Typically, acute inflammation is resolved. When this resolution occurs, what happens to neutrophils and debris?
phagocytosed by macrophages
Typically, acute inflammation is resolved. When this resolution occurs, what do macrophages release? What is the result?
growth factors, new blood vessels and increased fibroblasts
(both aid in the repair process)
What are three histologic characteristics of chronic inflammation?
monocyte infiltration, tissue destruction, fibrosis/repair
When infiltration occurs in chronic inflammation, this mostly includes what two types of leukocytes?
macrophages, lymphocytes
True or false: Both acute and chronic inflammation can result in scar formation.
true
Does angiogenesis occur in acute or chronic inflammation or both?
chronic
What triggers angiogenesis, or neovascularization?
VEGF, FGF-2
Why is angiogenesis (neovascularization) important?
delivers cells and nutrients to site of repair
Why can angiogenesis (neovascularization) be detrimental?
**as seen in retinopathies, AMD, and cancer
new vessels have incomplete basement membranes, so they are very leaky
In blood vessels, do we have monocytes or macrophages?
monocytes
At what point do monocytes become macrophages?
when they migrate into tissues
Monocytes differentiate into macrophages when they enter tissues from the blood. However, these macrophages are not yet activated because they have to be activated by what? (3)
microbes, dead cells in the area, cytokines released by nearby T cells
Activated macrophages can go on to play roles in what 2 processes?
inflammation, fibrosis
If activated macrophages go on to be involved in tissue injury and inflammation, then what 4 things can be released to also contribute to this process?
ROS, proteases, cytokines, coagulation factors
If activated macrophages go on to be involved in fibrosis, then what 3 things can be released to also contribute to this process?
growth factors, fibrogenic cytokines, angiogenesis factors
What is the relationship between macrophages and T lymphocytes in regards to stimulation?
they constantly activate each other
cytokine released by activated macrophages that activates T cells
IL-12
cytokine released by activated T cells that activates macrophages
IFN-y
What is the first phase of wound healing?
inflammation
(so we do need inflammation to occur in order for wounds to heal properly!)
3 examples of acute inflammatory disorders
acute transplant rejection, asthma, glomerulonephritis
5 examples of chronic inflammatory disorders
arthritis, asthma, atherosclerosis, chronic transplant rejection, pulmonary fibrosis
If we have more neutrophils, are we in chronic or acute inflammation?
acute
If we have more macrophages, are we in chronic or acute inflammation?
chronic
What are 4 ways that cells can adapt to injury?
atrophy, hypertrophy, hyperplasia, metaplasia
refers to decrease in cell size
atrophy
refers to increase in cell size
hypertrophy
refers to increase in amount of cells
hyperplasia
refers to conversion of cells of one type to cells of another type
metaplasia
Does loss of ATP result in reversible or irreversible cell injury?
reversible
What is the main consequence of loss of ATP in reversible cell injury?
cell swelling
Does increased glycolysis result in reversible or irreversible cell injury?
reversible
What is the main consequence of increased glycolysis in reversible cell injury?
decreased pH (due to buildup of lactic acid)
Does decreased protein production result in reversible or irreversible cell injury?
reversible
Does plasma membrane damage result in reversible or irreversible cell injury?
irreversible
Do damaged mitochondria result in reversible or irreversible cell injury?
irreversible
Do damaged lysosomes result in reversible or irreversible cell injury?
irreversible
What happens to chromatin in necrosis?
clumping
What happens to organelles in necrosis?
swelling
When membranes are damaged in necrosis, why is this so detrimental?
lysosomal enzymes may escape and damage nearby structures
What happens to chromatin in apoptosis?
condensation and fragmentation
What happens to the cytoplasm in apoptosis?
budding
(these apoptotic bodies are then phagocytosed by nearby cells)
What is the difference between apoptosis and necrosis?
apoptosis is cell suicide, necrosis is cell homicide
How does cell size change in necrosis vs. apoptosis?
enlarged in necrosis, reduced in apoptosis
How does the nucleus change in necrosis vs. apoptosis?
shrinks and then lyses in necrosis, fragments in apoptosis
How does the plasma membrane change in necrosis vs. apoptosis?
disrupted in necrosis, intact but with altered structure in apoptosis
How do the cellular contents change in necrosis vs. apoptosis?
digested by enzymes in necrosis, intact in apoptosis
Which apoptosis pathway is known as the mitochondrial pathway?
intrinsic
Which apoptosis pathway is known as the death receptor pathway?
extrinsic
6 steps of the intrinsic pathway (only) of apoptosis:
1. Cell injury triggers [these molecules]
2. Those trigger [these molecules]
3. Those cause the mitochondria to release [this protein]
4. That protein activates [these enzymes]
5. That protein also releases [these other proteins]
6. Those other proteins activate [these enzymes]
Bcl-2 family sensors, Bcl-2 family effectors, cytochrome c, initiator caspases, pro-apoptotic proteins, executioner caspases
4 steps of the extrinsic pathway (only) of apoptosis:
1. [this ligand] binds with [this receptor]
2. [these proteins] are activated
3. Those proteins activate [these enzymes]
4. Those enzymes activate [these other enzymes]
Fas, TNF receptor, adaptor proteins, initiator caspases, executioner caspases
What do the intrinsic and extrinsic pathways in apoptosis have in common? (i.e. What is the fundamental event that ensures that apoptosis will occur?)
both activate executioner caspases to activate endonuclease and proteinases and break down cytoskeleton
Which of the following is most likely to convert reversible cell injury to irreversible cell injury?
A. plasma membrane damage
B. protein degradation
C. cell swelling
A
The primary purpose of the vascular changes in an invaded or injured area is to...
A. produce swelling, redness, heat, and pain.
B. bring to the affected area phagocytes and plasma proteins that defend against the offending agent.
C. produce pus
D. exert an anti-inflammatory effect to protect against damage by potentially over-reactive defense mechanisms
E. trigger specific immune responses
B