Movement Disorders
1/63
Earn XP
Description and Tags
Same as before - any thing italicized is from uptodate/2025s. Also Ninja Nerd because my man, my man, my man
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
64 Terms
Essential tremors, Huntington’s, Tourette’s, Restless legs, Tardive dyskinesia
Which movement disorders are hyperkinetic
Parkinsons
Which movement disorders are hypokinetic?
Essential tremors
What is the most common cause of action/postural tremor - meaning that it occurs when you fight against gravity?
brainstem, cerebellum
Essential tremors are due to issues in the _____________ or _______________.
Autosomal dominant (effects 1% of the population and increases with age)
Essential tremors are associated with what inheritance pattern?
isolated tremor consisting of BUE action tremor without other motor abnormalities, at least 3 years, with/without other locations (head, voice, rarely legs), absence of ataxia, dystonia, parkinsonism
What are the diagnostic criteria for essential tremors?
propanolol, primidone, xanax
90 y/o female presents to the clinic for “shaking hands,” she notes that this has going on for years, but that it has gotten to the point that she can no longer cook or crochet. She notes that it slightly improves when she has a glass of wine. On a physical exam you note a tremor that only occurs during voluntary hand movements OR when arms are fixed against gravity. Let’s say this is mild, situational exacerbations → how do you want to treat it?
Primidone or a combination with propanolol
90 y/o female presents to the clinic for “shaking hands,” she notes that this has going on for years, but that it has gotten to the point that she can no longer cook or crochet. She notes that it slightly improves when she has a glass of wine. On a physical exam you note a tremor that only occurs during voluntary hand movements OR when arms are fixed against gravity. Let’s say that the tremors are persistent and meds are ineffective→ how do you want to treat it?
Alprazolam, topiramate, gabapentin
90 y/o female presents to the clinic for “shaking hands,” she notes that this has going on for years, but that it has gotten to the point that she can no longer cook or crochet. She notes that it slightly improves when she has a glass of wine. On a physical exam you note a tremor that only occurs during voluntary hand movements OR when arms are fixed against gravity. Let’s say that the tremors are continuous → how do you want to treat it?
botox, deep brain stimulation, focus transcranial u/s thalamotomy, stereotactic radiosurgery (C/I with dementia, depression, anxiety)
90 y/o female presents to the clinic for “shaking hands,” she notes that this has going on for years, but that it has gotten to the point that she can no longer cook or crochet. She notes that it slightly improves when she has a glass of wine. On a physical exam you note a tremor that only occurs during voluntary hand movements OR when arms are fixed against gravity. Let’s say that nothing is working, and she now has head/vocal tremors → how do you want to treat it?
Gradually worsens with age, can lead to disability, refer to neuro to r/o out other causes
What is the prognosis for essential tremor?
Huntington Disease
What movement disorder is an autosomal dominant disease that has an onset of 30-50 years and is fatal in 15-20?
Mutation on the HTT gene that leads to a CAG repeat on chromosome 4 (4p16.3)
What goes wrong in Huntington’s Disease?
decreased GABA inhibition leading to increased stimulation of the motor cortex, severe striatal atrophy with ventricle enlargement
What is the result of the CAG repeats in Huntington’s disease
Genetic testing
44 y/o male presents to the clinic for involuntary movements (chorea). He notes that he has loss 10 weeks without trying. His wife reports that in the last couple weeks he has become more and more irritable and moody, when before he was the most patient husband. On a physical exam you note that reflexes are BRISK and that he is unable to maintain tongue protrusion. Labs and CSF are normal. PET shows reduced striatal metabolic rate. What can you use to confirm your diagnosis?
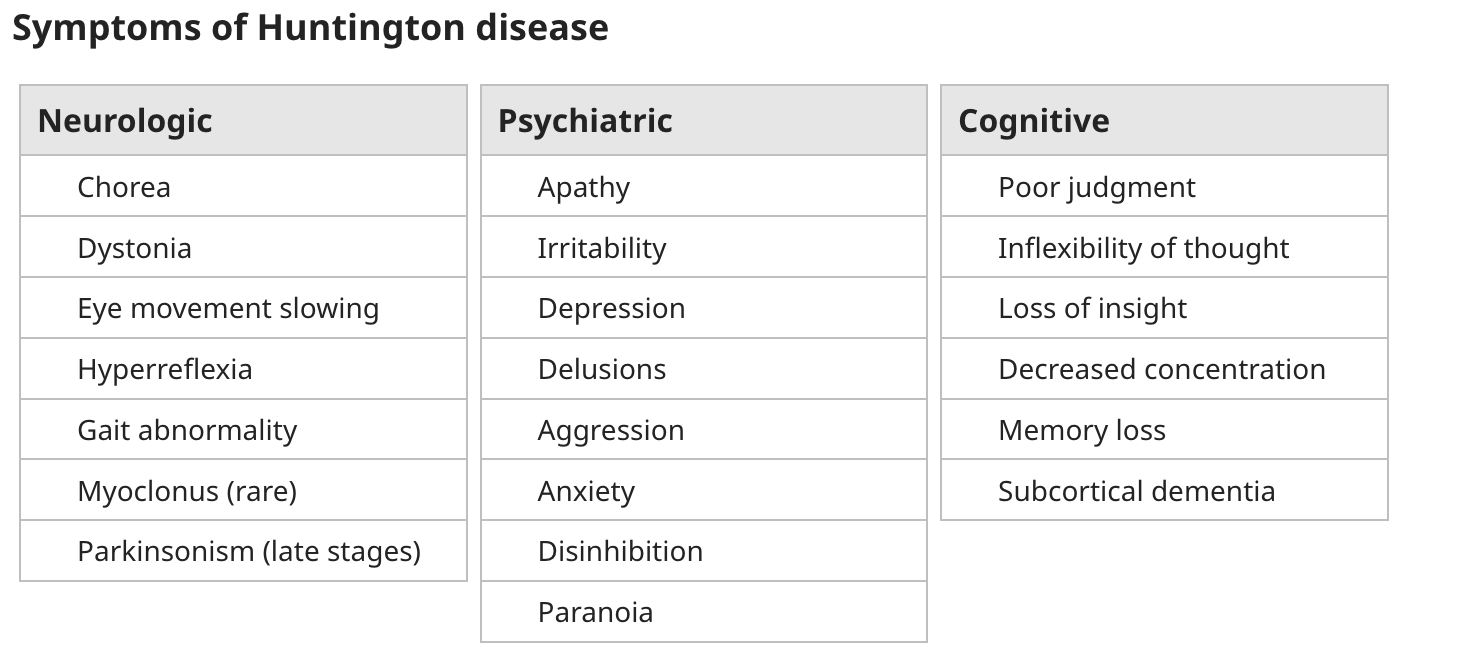
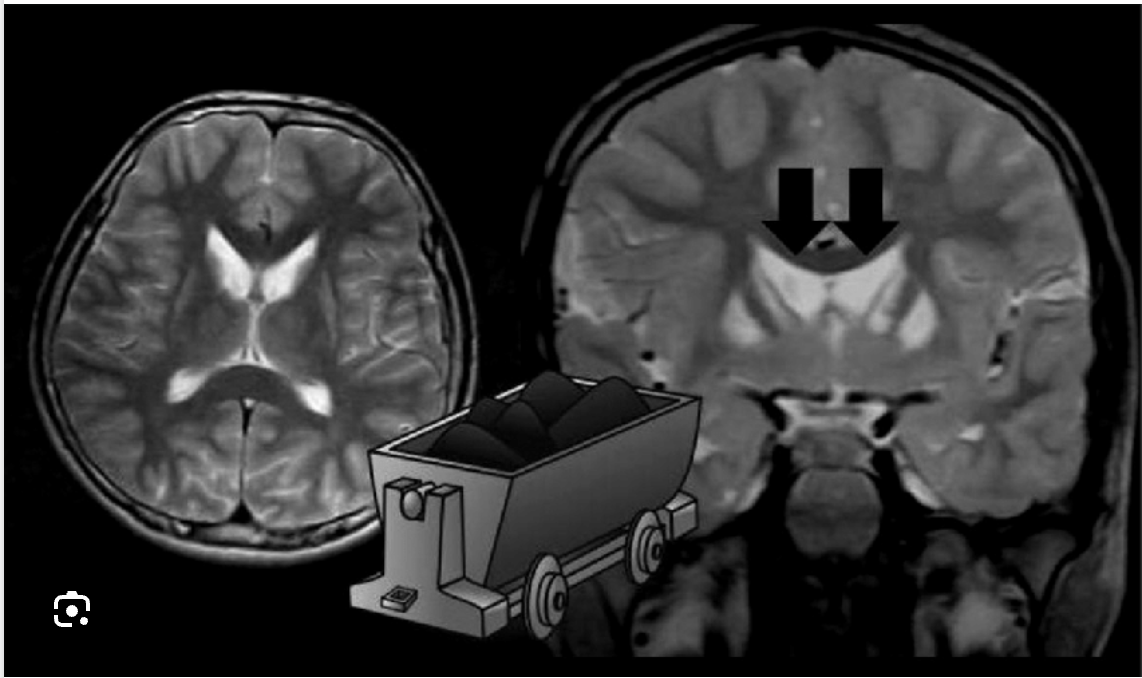
Cerebral atrophy, atrophy of caudate nucleus (boxcar ventricle)
What might you see on MRI/CT for Huntingtons?
PT/OT (aerobics, resistance training), counseling (deep brain stimulation), Tetrabenazine/deutetrabenazine (movement reducer, improves dyskinesia), Antipsychotics (dyskinesia, behavioral disturbances), Quetiapine (psychosis, disruptive behavioral symptoms), Amantadine (chorea), Clonazepam (behavioral)
Gameplan for Huntingtons → just symptomatic (no cure)
Stroke, lupus, HIV, medication reaction, paraneoplastic infections, Sydenham chorea (hx of strep infection, resolves), Huntington like disorders (issues on chromo 16/20)
DDx for Huntington’s
Parkinson’s Disease
A progressive degeneration of the dopaminergic neurons in the substantia nigra that leads to altered motor movements
Genetic mutations, environmental exposure (manganese dust, carbon disulfide, CO poisoning), Reversible (due to neuroleptic drugs, reserpine, metoclopromide), Space occupying lesion (presents as hemiparkinsonism), Idiopathic (parkinson’s disease)
What are the types of Parkinsonisms?
Resting tremor, bradykinesia (slow movements, Akinesia), rigidity, postural instability
Cardinal symptoms of Parkinson’s - TRAP
Age (45-65, usually 60), family hx, male, herbicide/pesticide exposure, Hx of head trauma
Risk factors for Parkinson’s Disease
Bradykinesa
Which cardinal symptom of Parkinson’s Disease is characterized by a difficulty initiating voluntary movements that usually starts distally and hesitate/halt with progression
Resting tremor (usually looks like pill-rolling)
Which cardinal symptom of Parkinson’s Disease is observed in a fully resting limb and is suppressed when movement is initiated (likely due to a lack of dopamine and cerebellar influence)
Rigidity (cogwheel vs. leadpipe)
Which cardinal symptom of Parkinson’s Disease is characterized by an increased resistance to passive movement of the major joints?
Masked facies (expressionless, immobile, widened palpebral fissure, infrequent blinking, seborrhea, soft voice), cognitive dysfunction and dementia (78% of patients), Myerson’s sign (unable to stop blinking when tapped between the eye brows), Gait (shuffling, short stepped, freezing, festination), hunched posture
What are the clinical symptoms of Parkinson’s
ratchety, clicky pattern of resistance and relaxation as the examiner moves the limb through its full range of motion - usually the arms
Describe cog-wheel rigidity
a tonic resistance that is smooth throughout the entire range of passive movement - usually the legs
Describe lead-pipe rigidity
Starts in 1 limb, then moves down the same side
What is the 1st stage of Parkinsons?
Neuropath examination on autopsy
What is the gold standard diagnosis for parkinson’s
Bradykinesia (or akinisia - can’t get started), postural instability (can’t oppose resistance)
The loss of dopaminergic neurons of the direct (D1) and indirect (D2) leads to
direct path stimulates (biceps contract), indirect path inhibits (triceps relax) → arm bends
Describe the direct and indirect pathways of the motor system
rigidity, tremors
With the destruction of dopaminergic neurons, ACh becomes the dominant force in the motor system → what does this explain
Lewy bodies
What are the abnormal aggregates of alpha-synuclein proteins that can be found within the neurons of the substantia nigra/cortex (Linked to LRRK-2) which will lead to neuronal degeneration by either apoptosis or necrosis
A minimum of bradykinesia + tremor/rigidity, Levodopa challenge test (can also be done with apormorphine)
Gameplan to diagnose Parkinson → refer to neuro
Effects the dominant hand, if it interferes with ADLs, social/leisure function, significant bradykinesia or gait disturbance, Patient values
When should we start the treatment of parkinson’s?
Rasagiline, selegiline, safinamide (selective MOAB inhibitors)
Which drugs for parkinson’s inhibit the breakdown of dopamine (slows progression) and can be used alone or with Levodopa - use in younger patients?
Amantidine
Which drugs for parkinson’s increase dopamnine release/block reuptake and can be used in patients with mild symptoms, improving all clinical features - even dyskinesias from levodopa therapy
Pramipexeole, ropinirole, rotigotine, apomorphine, bromocriptine (dopamine agonist)
Which drugs for parkinson’s are similar to Levodopa but we use early in the progression, C/I in peeps with mental illness, recent MI, and excessive sleepiness
Levodopa (L-dopa - more tolerable in older patient)
Which drugs for parkinson’s is converted to dopamine and improves ALL clincal features especially bradykinesia and rigidity but can lead to N/V, hypotension, arrythmias, dyskinesia (C/I in psychosis, glaucoma, and MAOI use)
Cabidopa (sinemet is the combined form)
Which drugs for parkinson’s limits extra-cerebral breakdown of levodopa → limits the side effects
benxtropine, mesylate, procyclidine, trihexyhenidyl (anticholingerics)
Which drugs for parkinson’s are helpful tremor and rigidity and C/I for narrow angle glaucoma and BPH?
COMT Inhibitors (catechol-O-methyl-transferase)
Which drugs for parkinson’s prolong and potentiate L-dopa effects (DO NOT USE ALONE)
progresses slowly (unless the patients are older when symptoms begin or there’s no tremor), reduces longevity by 10-20 years
Prognosis for Parkinson’s → improves with OT, PT, Speech, CBT
Wilsons, Huntington’s, Jacob-Creutzfeldt, lewy body dementia, essential tremor
DDX for parkinson’s
Tourette Syndrome (Gilles De La Tourette Syndrome)
Which movement disorder is the most common cause of tics (HALLMARK), more common in males, onsets before 21 (2-15 is average) and can be inherited from both parents (bilineal transmission) ?
disturbance in the striatal-thalamic-cortical (mesolimbic) spinal system (loss of inhibition)
What is going wrong in tourette’s
Coprolalia
What type of tic is characterized by the involuntary and repetitive use of foul language
Echolalia
What type of tic is characterized by the automatic repetition of words or phrases spoken by others?
Palilalia
What type of tic is characterized by the involuntary repetition of one’s own words or phrases (usually a specific word)
sniffing, blinking (most common initial symptom), frowning, shoulder movements, echopraxia (mimicking other’s movements)
Examples of motor tics in tourette’s → note tics may be self-harming and associated with OCD
Multiple motor + at least one vocal (doesn’t have to be concurrent), onset before 18, tics may wax and wane, present for a year, not due to anything else
DSM-5 criteria for tourettes - clinical diagnosis!
CBT, clonidine/guanfacine (alpha adrenergics - if concurrent ADHD), Vocal/focal motor tics that are painful/social disabling (botox), For bothersome tics (tetrabenzine - antipsychotics are an option but have tons of ADRs), Deep brain stimulation
Treatment plan for Tourettes → symptomatic
Restless leg syndrome (Willis-Ekborn Disease)
A movement disorder associated with parkinson’s, iron deficiency, pregnancy, and peripheral neuropathy that affects 1-5% of people and worsens with age
Electrical stimulation, lifestyle changes, Gabapentin enacarbil (1st line - approved), gabapentin/pregabalin (1st line but off-label)
65 y/o female presents to the clinic for difficulty sleeping. She states that when she tries to sleep she has an irresistible urge to move limbs and that her hips, knees, and ankles will move on their own. Hx is negative, physical exam is negative. Ferritin levels are normal. What is your treatment plan?
dopamine agonist (may augment symptoms), opioids (if symptoms are severe or refractory), iron sulfate (if ferritin is low), benzos (younger patients, mild cases)
Second line for restless leg syndrome
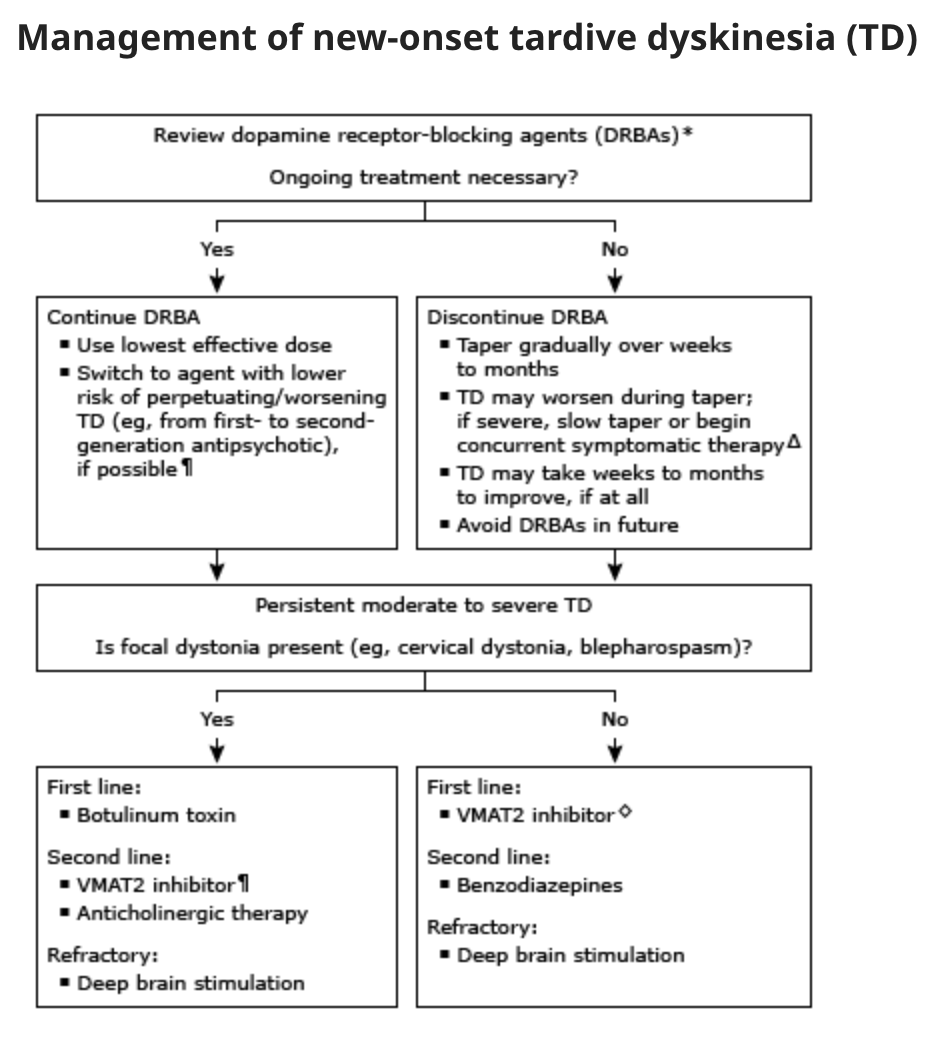
Tardive dyskinesia
Involuntary athetoid/choreiform movements lasting a few weeks, associated with neuroleptic medication use (Haldol my beloved)
Age, female, African American, 1G antipsychotic, high dose/long term antipsychotic (20%), prior ECT, EtOH or substance abuse, dementia, diabetes
Risk factors for tardive dyskinesia
Chorpromazine, fluphenazine, halperidol, perphenazine, prochlorperazine, metoclopramide (over 12 weeks, female, diabetes, 65+), antidepressants (rare)
Which drugs have a high rate of causing Tardive dyskinesia
Worm like tongue movements, facial tics, increased blinking, jaw movements
Early Tardive Dyskinesia Symptoms
lip smacking, chewing motions, puffing of cheeks, disrupted speech
Late tardive dyskinesia symptoms
Clinical diagnosis (vibes), labs and imaging to r/o everything else
How do you diagnosis tardive dyskinesia → refer to neuro
VMT-2s (valbenazine, deutetrabenzine, tretrabenazine), clonzapam, ginko biloba, amantadine
Treatment plan for tardive dyskinesia
huntington, tourettes, Rett Syndrome, Chronic motor tic disorder
DDX tardive dyskinesia