Kidneys: Basic Renal Processes- Tubular Reabsorption
1/24
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
25 Terms
Tubular Reabsorption
Selective movement of filtered substances from the tubular lumen into the peritubular capillaries (H2O, Na+, Cl-)
Tubular Epithelium
Throughout its entire length, the tubule is one cell layer thick
It has a luminal and basolateral membrane
Adjacent tubular cells form tight junctions (barriers so nothing can get through, therefore pores are needed)
Capillary Endothelium
Throughout its entire length, the capillary is one very thin cell layer thick
No tight junctions between endothelial cells (little barrier for H2O and solutes)
Fenestrated capillaries are even more permeable
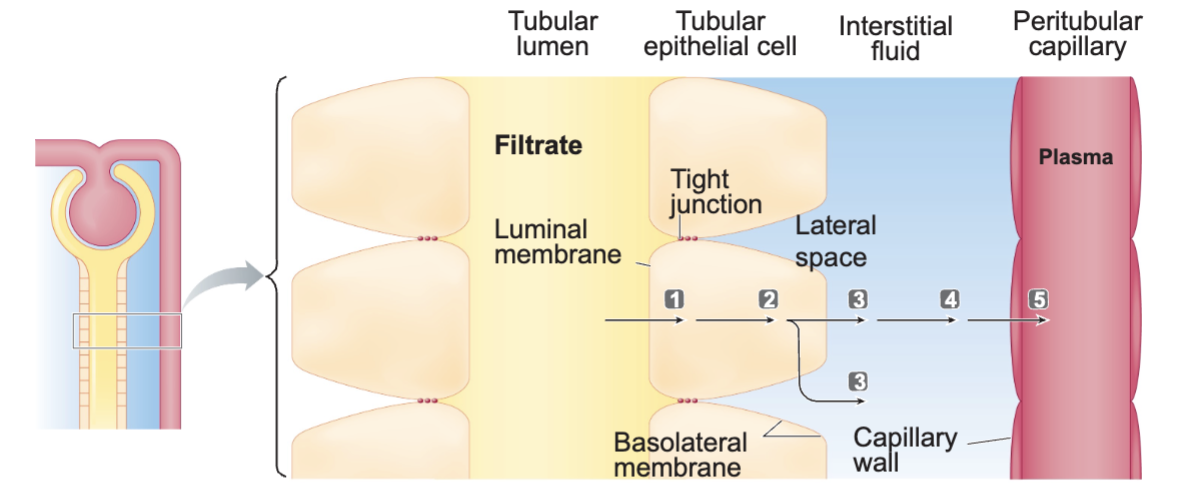
What five barriers does transepithelial transport cross?
The luminal membrane of tubular cell- allows reabsorption to be selective
The cytosol of tubular cell
The basolateral membrane of tubular cell- allows reabsorption to be selective
The interstitial fluid
The capillary wall
Permeability of tubular cell membrane varies along the length of the tubular system and in some areas is subject to hormonal control
What are the two types of tubular reabsorption?
Passive: movement down an osmotic or electrochemical gradient (H2O)
Active: requires ATP (Na+, glucose, amino acids, other electrolytes)
How much of Na+ is reabsorbed and where?
99.5% of Na+ is reabsorbed
67% in proximal tubule
25% in loop of Henle
8% in distal and collecting tubules (subject to hormonal control)
What is the role of Na+ reabsorption in different regions?
Proximal Tubule: Plays role in reabsorption of glucose, amino acids, H2O, Cl-, and urea
Loop of Henle: Plays role in kidneys ability to produce urine of varying concentrations and volumes
Distal Tubule: Subject to hormonal control, important in the regulation of ECF volume
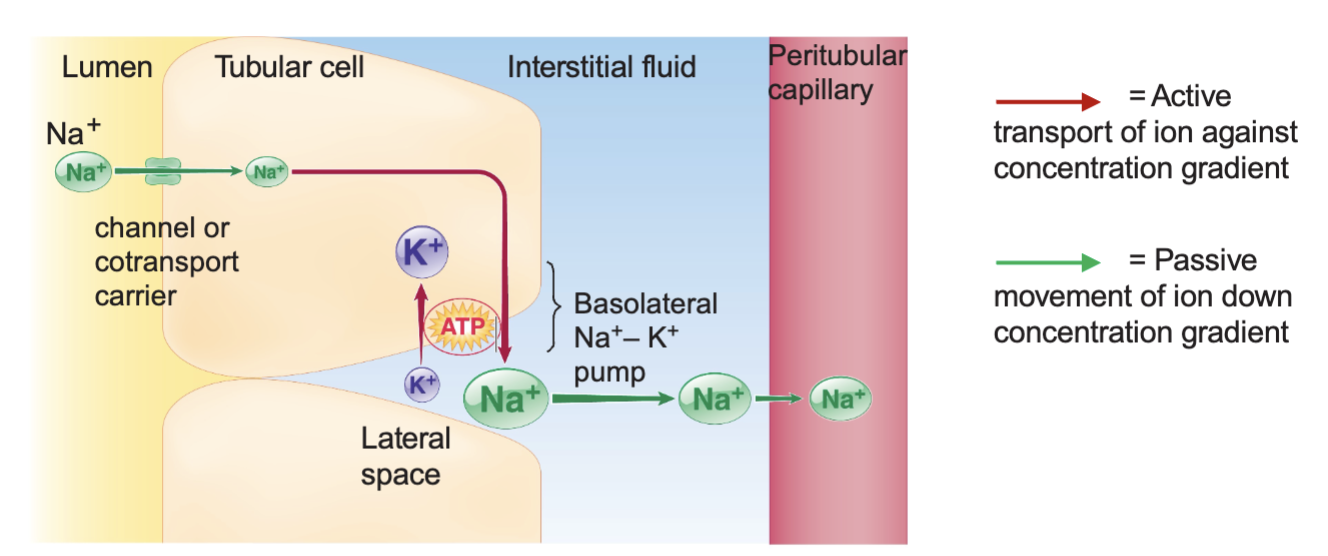
Na+ Reabsorption
The active step in Na+ reabsorption (tubular cells → interstitial fluid) involves the energy dependent Na/K ATPase pump loated in the tubular cells basolateral membrane
Intracellular concentration of Na+ is low, Na+ diffuses into the tubular cell down tis concentration gradient
Interstitial concentration of Na+ is high, Na+ diffuses into the peritubular capillary down its concentration gradient
Control Over Na+ Reabsorption
In the proximal tubule and loop of Henle, a constant percent of filtered Na+ is reabsorbed regardless of the amount of Na+ in the body
In distal and collecting tubules, the reabsorption of a small percent of Na+ is subject to hormonal control, the extent of this reabsorption is inversely related to the magnitude of the Na+ load in the body
The hormones are aldosterone and atrial natriuretic peptide
Aldosterone
Hormone that stimulates Na+ reabsorption in the distal and collecting tubules
Atrial Natriuretic Peptide
Hormone that inhibits Na+ reabsorption in the distal and collecting tubules
Active Na+ reabsorption drives…
Passive reabsorption of H2O, Cl-, and urea
H 2 O (osmotic gradient),
facilitated by aquaporins (AQP).Proximal tubules express AQP1 (always open). Distal and collecting tubules express AQP2 (regulated by vasopressin)
Cl- (electrochemical gradient)
Urea (only partial, concentration
gradient that increases towards
the end of the proximal tubules
as more H2O has left the filtrate)
How does aldosterone stimulate Na+ reabsorption in the distal and collecting tubules?
Insertion of additional leak channels in the luminal membrane
Inserting additional Na/K ATPase in the basolatereal membrane
What controls aldosterone release?
The renin-agiotensin-aldosterone system (RAAS)
What triggers RAAS?
Low NaCl concentration
Low ECF volume
Low systemic arterial blood pressure
What are the steps in RAAS?
Triggers are sensed in the kidneys which release the hormone renin
Renin will act on angiotensinogen from the liver (that is always in the blood) and convert it to angiotensin I
Angiotensin I is converted into angiotensin II by angiotensin-converting enzyme from the lungs (always produced)
Angiotensin II does four things
Causes the release of vasopressin from the hypothalamus which sends a signal to the kidneys to reabsorb H2O
Works on thirst center of the brain to make you thirsty
Causes general arterial vasoconstriction
Acts on adrenal cortex to release hormone aldosterone
What does aldosterone do when it is released?
Travels to the kidneys and drive the insertion of additional Na+ leak channels in the luminal membrane and Na/K ATPase in the basolateral membrane
This causes the reabsorption of the final 8% of Na+, allowing the body to retain it and more H2O
This restores the low blood pressure and low volume, which deactivates RAAS
Angiotensinogen
Hormone and enzyme
Synthesized in the liver
Always present in the plasma
Renin
Released from the kidneys (granular cells) into plasma
Converts angiotensinogen into angiotensin I
Angiotensin-Converting Enzyme (ACE)
Enzyme present in the lungs
Converts angiotensin I into angiotensin II
Angiotensin II
Has many effects
Stimulates adrenal cortex to release aldosterone
Aldosterone
Increases Na+ reabsorption in the distal and collecting tubules by promoting the insertion of Na+ channels and Na/K ATPase carriers
What triggers natriuretic peptides to inhibit Na+ reabsorption?
High NaCl concentration
High ECF volume
High arterial blood pressure
What do natriuretic peptides inhibit?
Na+ reabsorption
RAAS
Smooth muscle of arterioles (increased GFR)
Sympathetic nervous system to reduce cardiac output and peripheral resistance
Natriuretic peptides are the opposite of RAAS, they reduce blood pressure
Reabsorption of glucose and amino acids
Reabsorbed in the proximal tubule by Na+ dependent specific symport carriers across the tubular membrane into the cell (secondary active transport)
Glucose then diffuses across the basolateral tubular membrane via glucose transporters (facilitated diffusion)
Glucose reabsorption is efficient and complete but the number of sodium-glucose symporters are finite, there is a tubular maximum
Excess glucose is lost in urine- uncontrolled diabetes