Ventilatory Control Self Study/Irregular Breathing SS
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
20 Terms
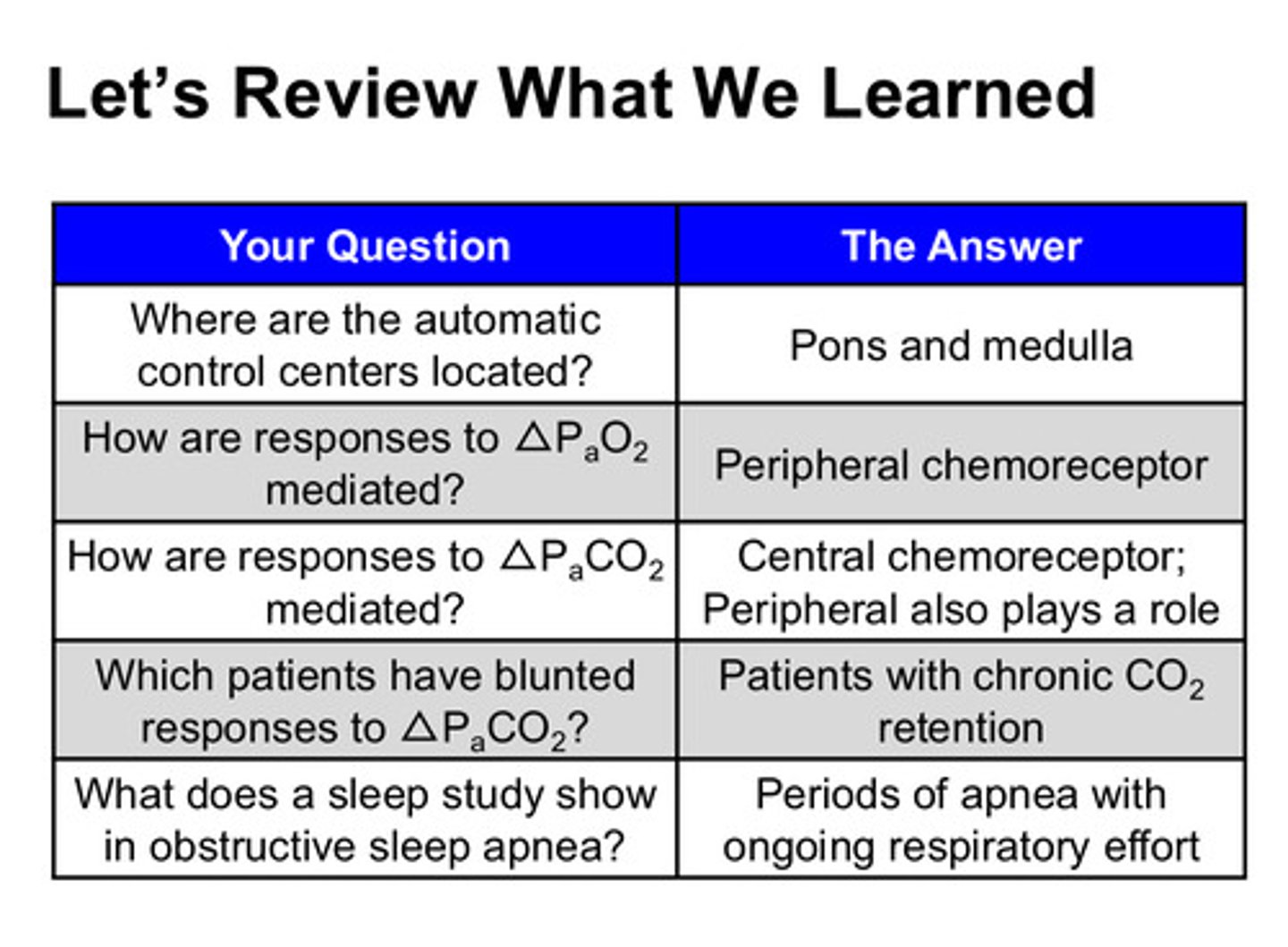
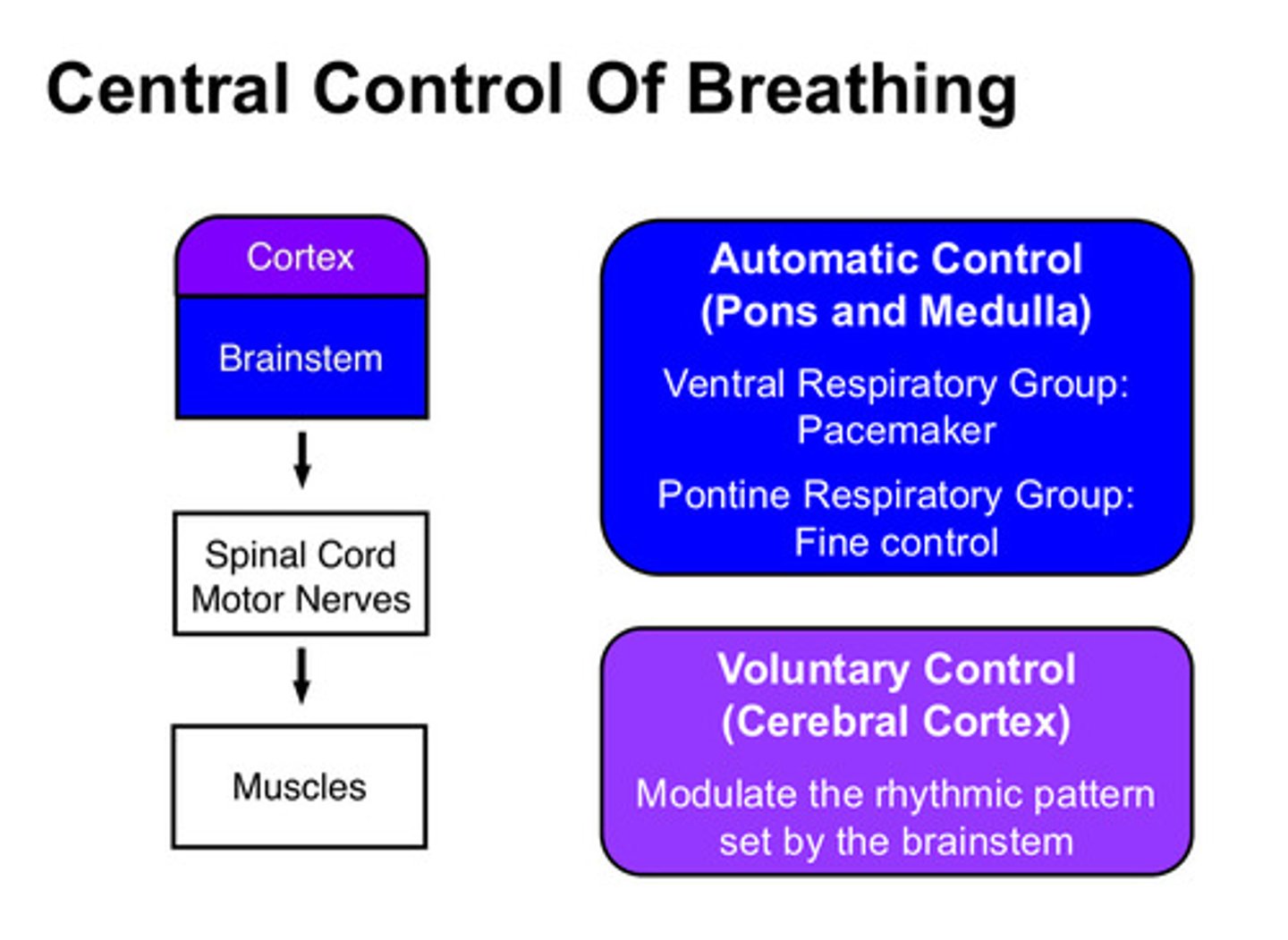
the central control of breathing resides in 2 main sites: what are they
1) brainstem (pons and medulla)
2) cerebral cortex
which control site controls involuntary (autonomic) breathing?
the brainstem (pons and medulla): the "pacemaker" is in the ventral respiratory group and fine control is in the pontine respiratory group
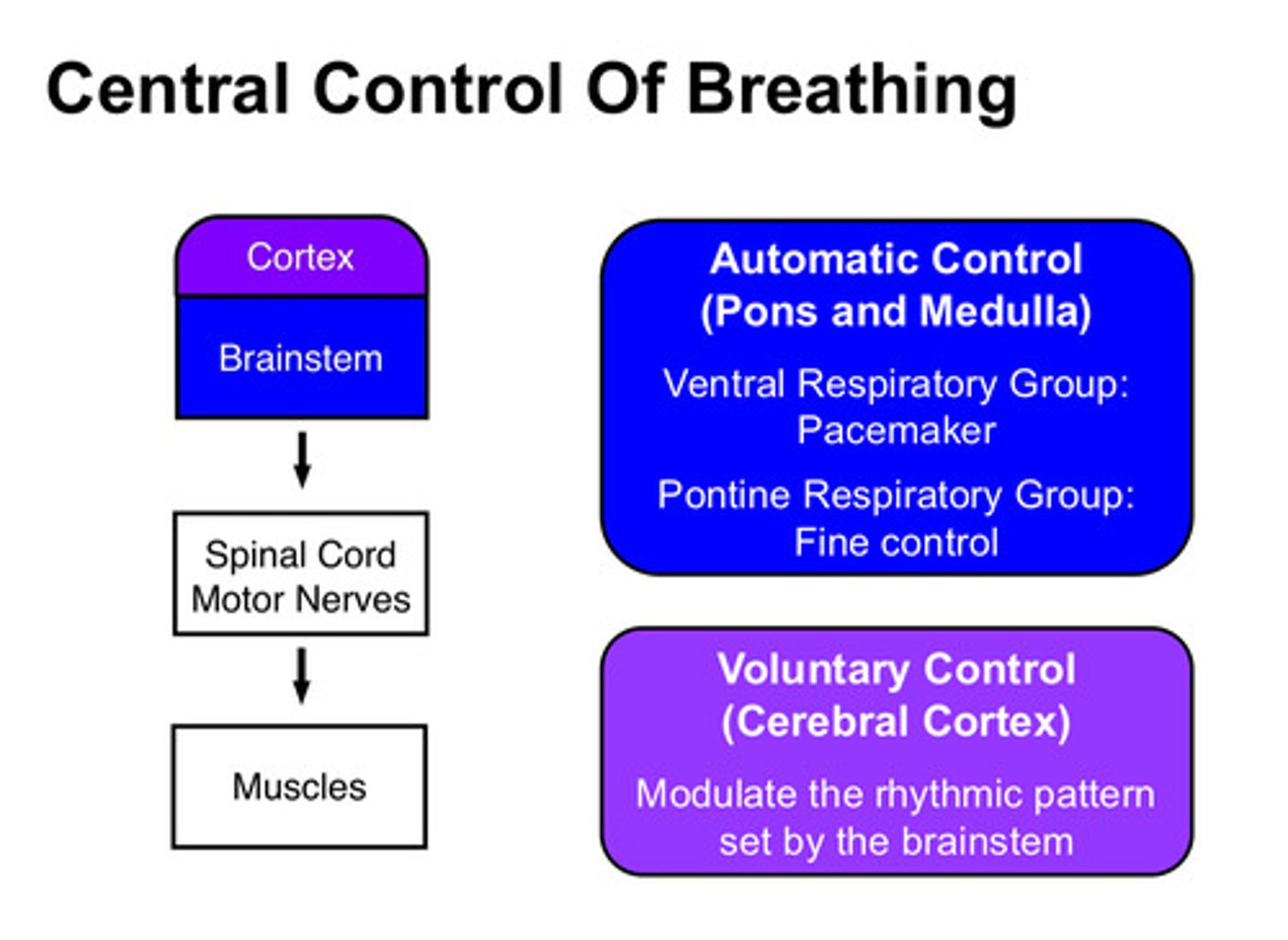
which control site controls voluntary breathing?
cerebral cortex
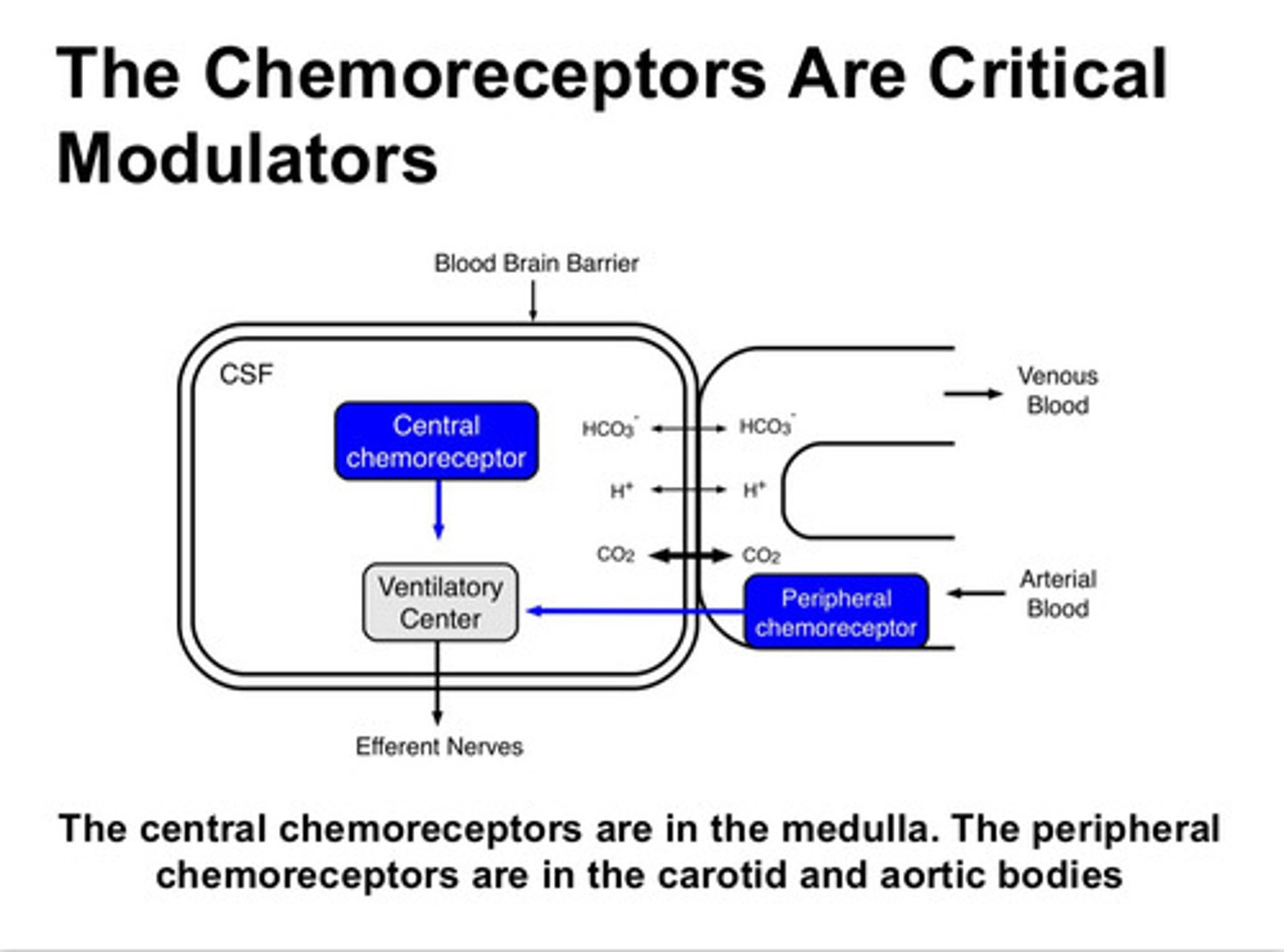
these control sites receive feedback through chemoreceptors: central and peripheral. where are the central chemoreceptors found and what do they perceive
found in the medulla; perceive PaCO2 and pH
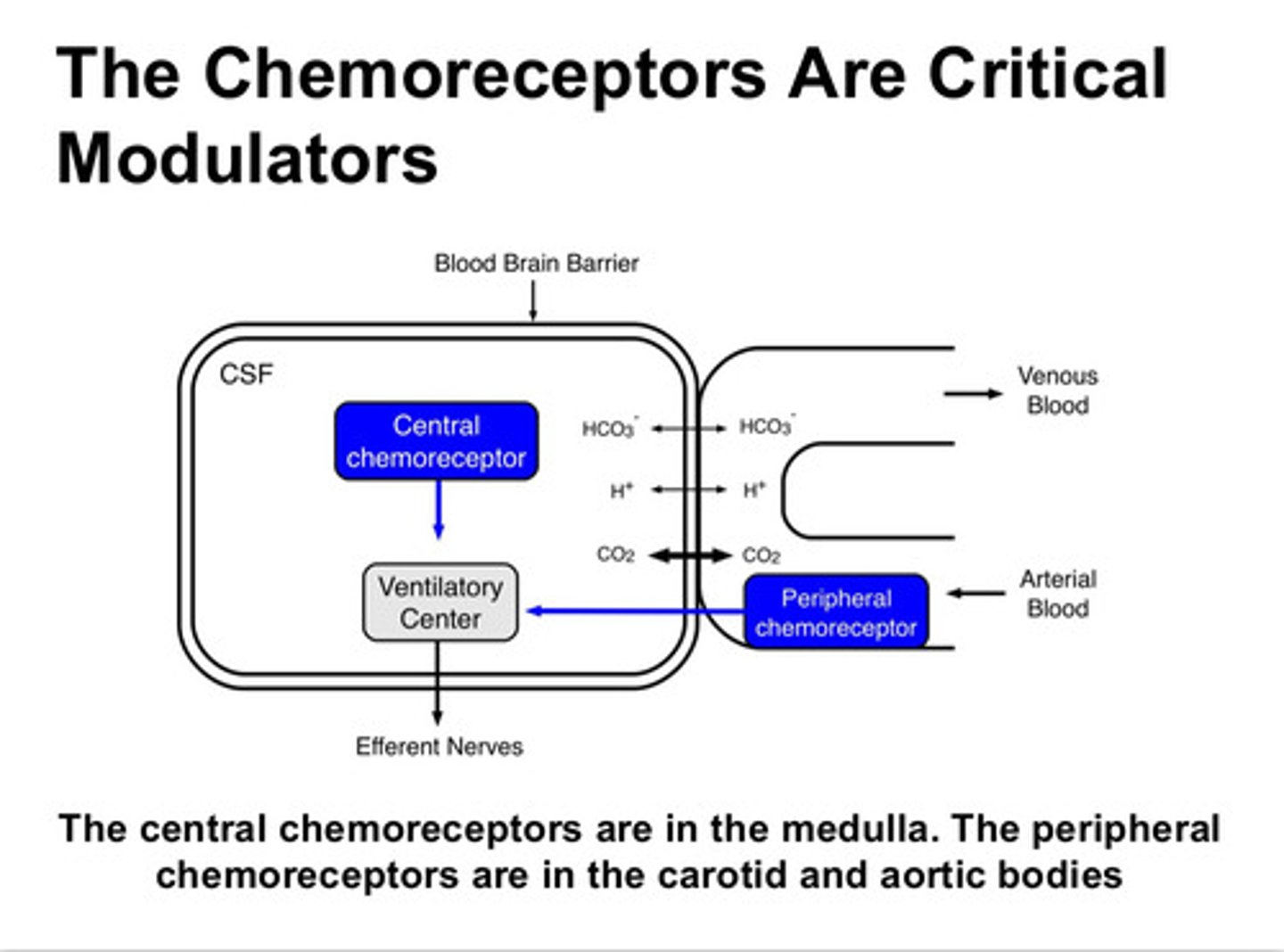
where are the peripheral chemoreceptors found and what do they perceive
found in the carotid and aortic bodies; perceive PaCO2, pH, and PaO2 (only the peripheral chemoreceptors respond to changes in PO2)
summary of chemoreceptors and the feedback they receive
output as in breathing/ventilation
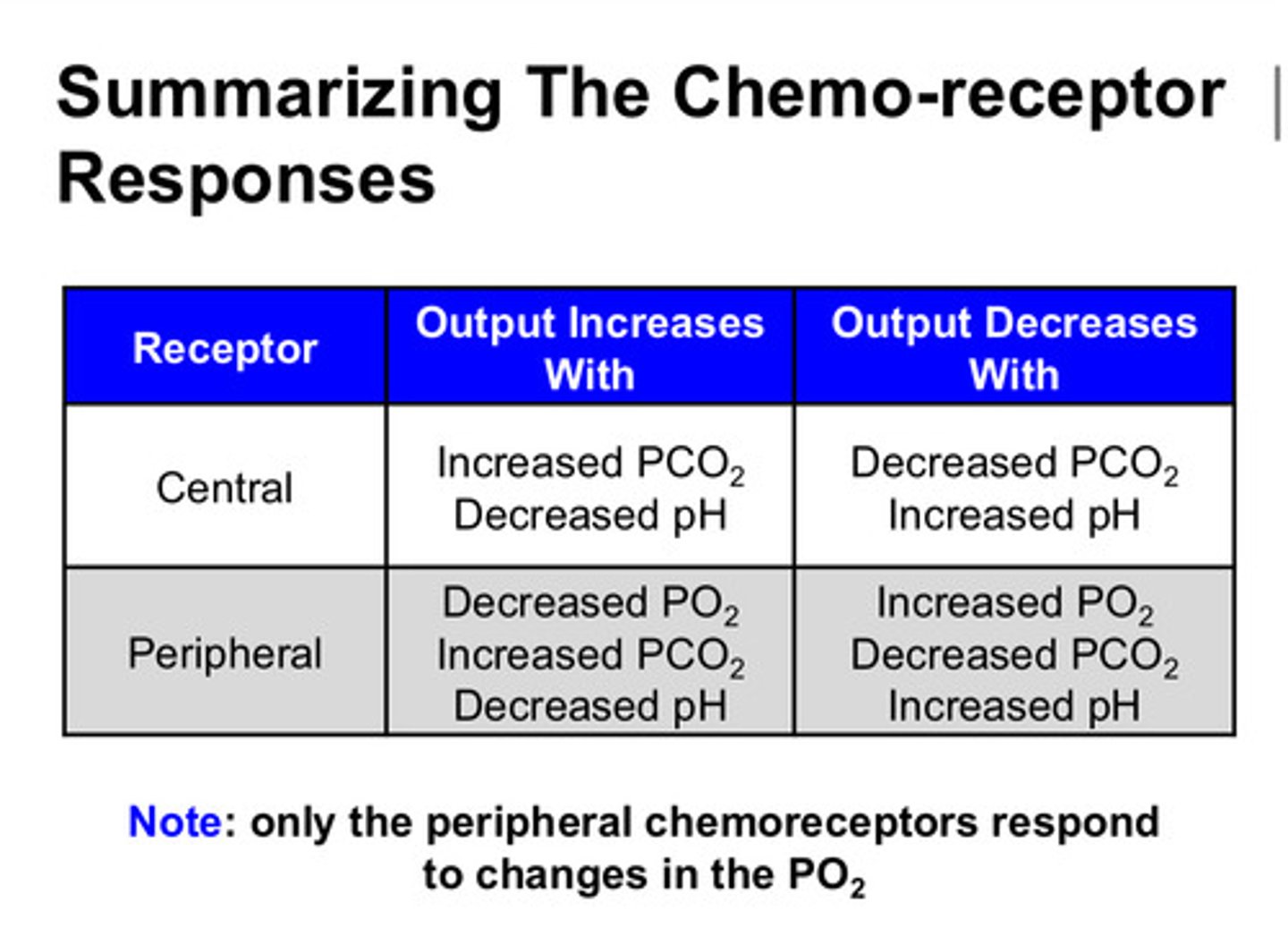
recall, which pressure is the primary driver of ventilation?
PaCO2!!! (in hypoxic states, however, PaO2 can have a strong influence)
what are the 2 kinds of ventilatory control disorders
1) primary ventilatory disorders: problem in the brain itself
2) secondary ventilatory disorders: problems that lead to a change in how the control centers work
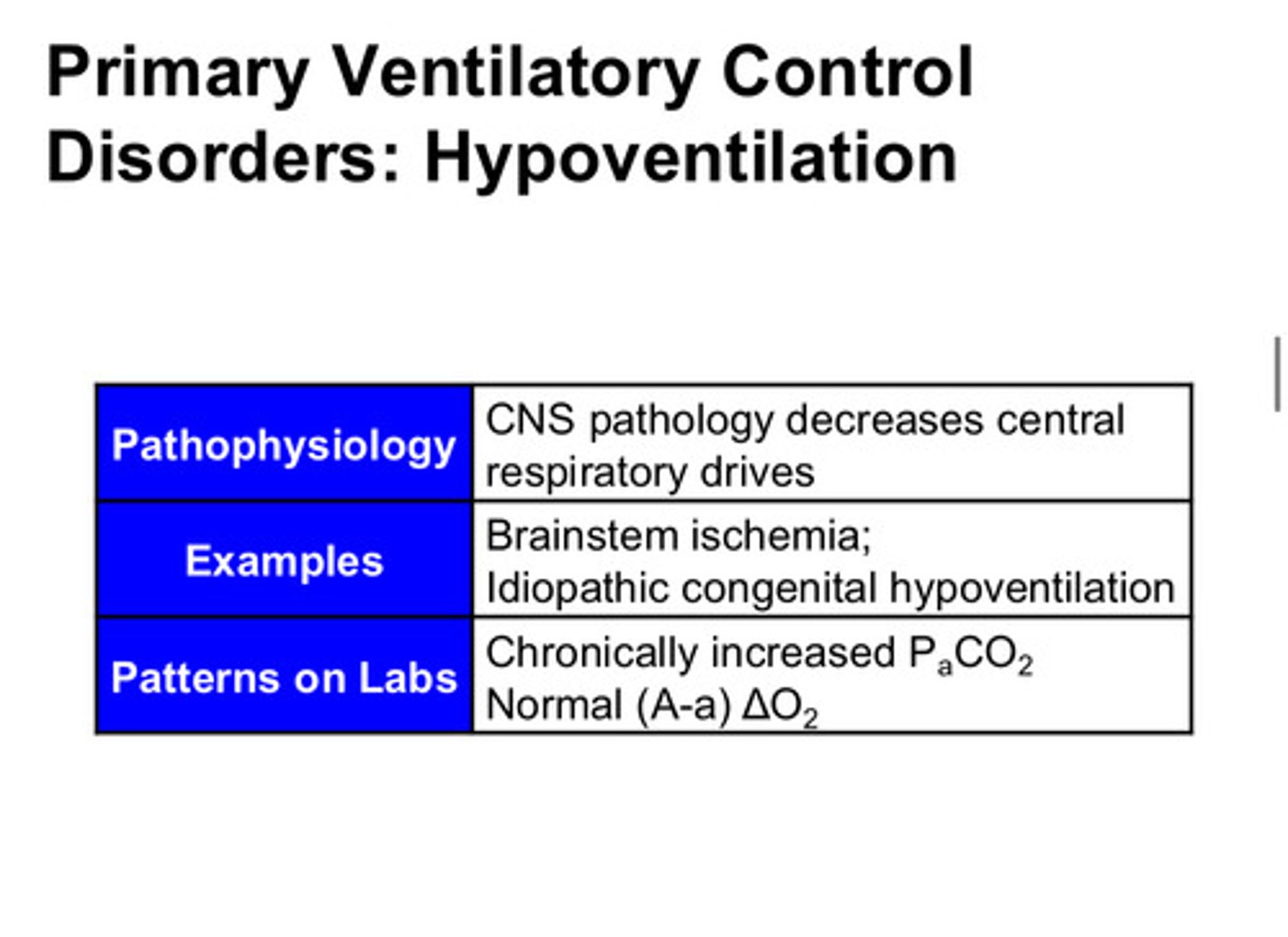
describe hypoventilation as a primary ventilatory disorder
hypoventilation can result from decreased brainstem function such as a brainstem stroke. this can lead to chronic increased PaCO2 with a normal PaO2 (the peripheral chemoreceptors are working better than the central receptors which were damaged in the stroke, so the peripheral chemoreceptors regulate the PaO2 with less input from the central chemoreceptors)
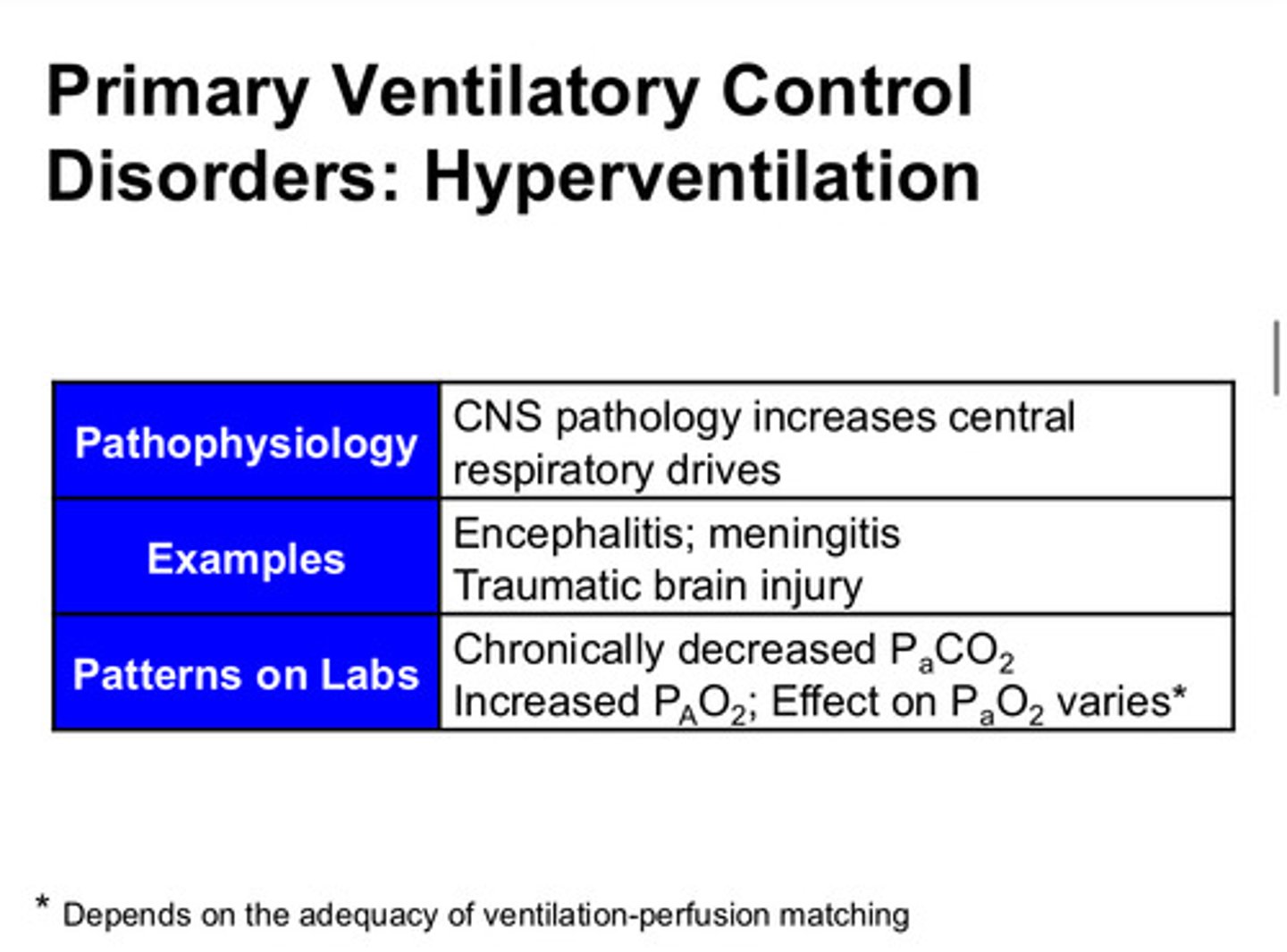
describe hyperventilation as a primary ventilatory disorder
hyperventilation can result from a response to a brain injury or brain infection. this hyperventilation results in chronic decreased PaCO2 with a varied response on the PaO2
what is a secondary ventilatory disorder that might result in chronic hyperventilation?
people who live at a chronic elevation (low PiO2) have chronic hyperventilation because their peripheral chemoreceptors have greater influence to increase the ventilation in an effort to raise the PaO2
what are secondary ventilatory disorders that might result in chronic hypoventilation
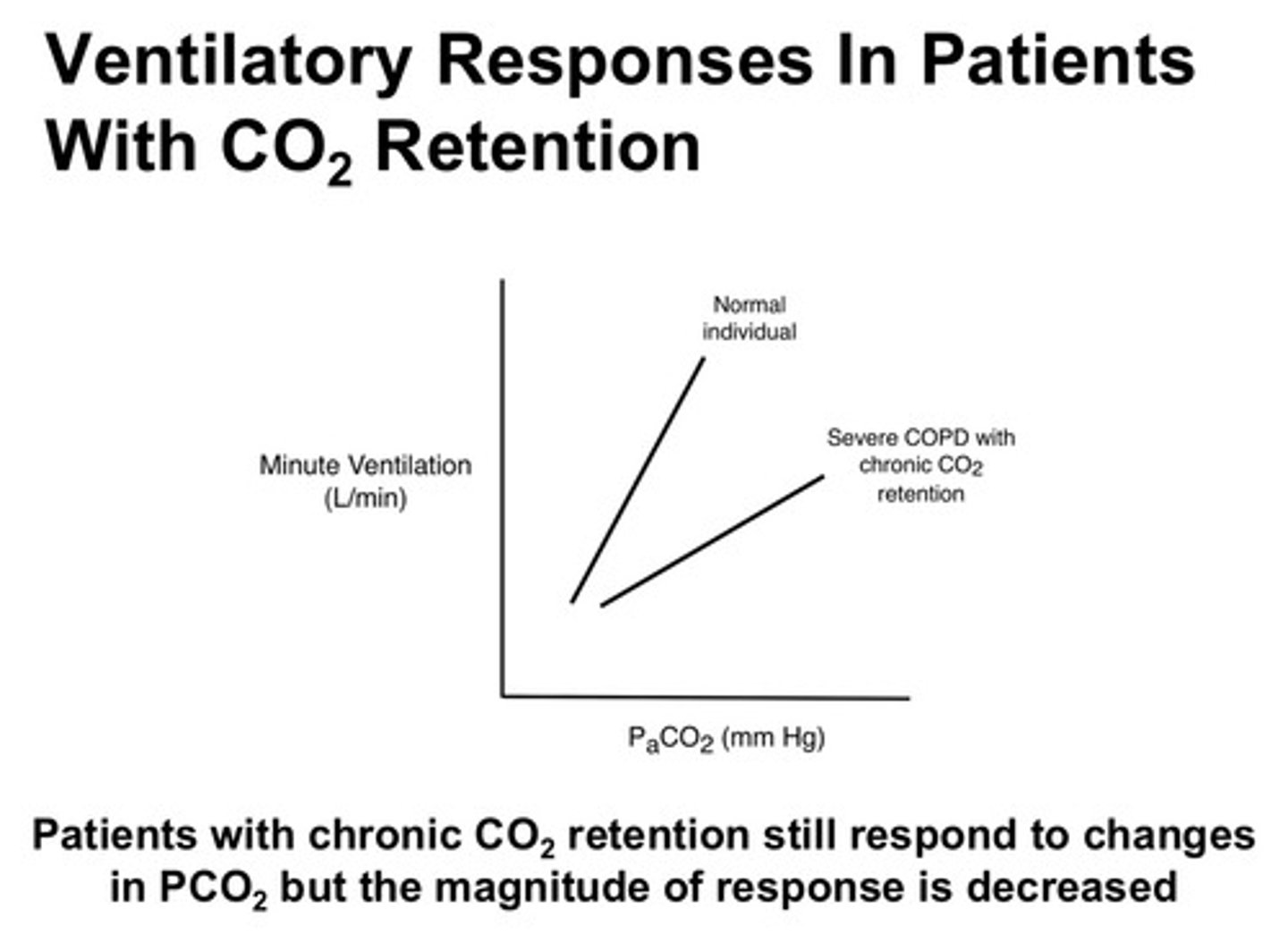
1) people who live with COPD (increased "dead space" from disease) have chronic hypoventilation as all their chemoreceptors have less response to the PaCO2 and the PaO2
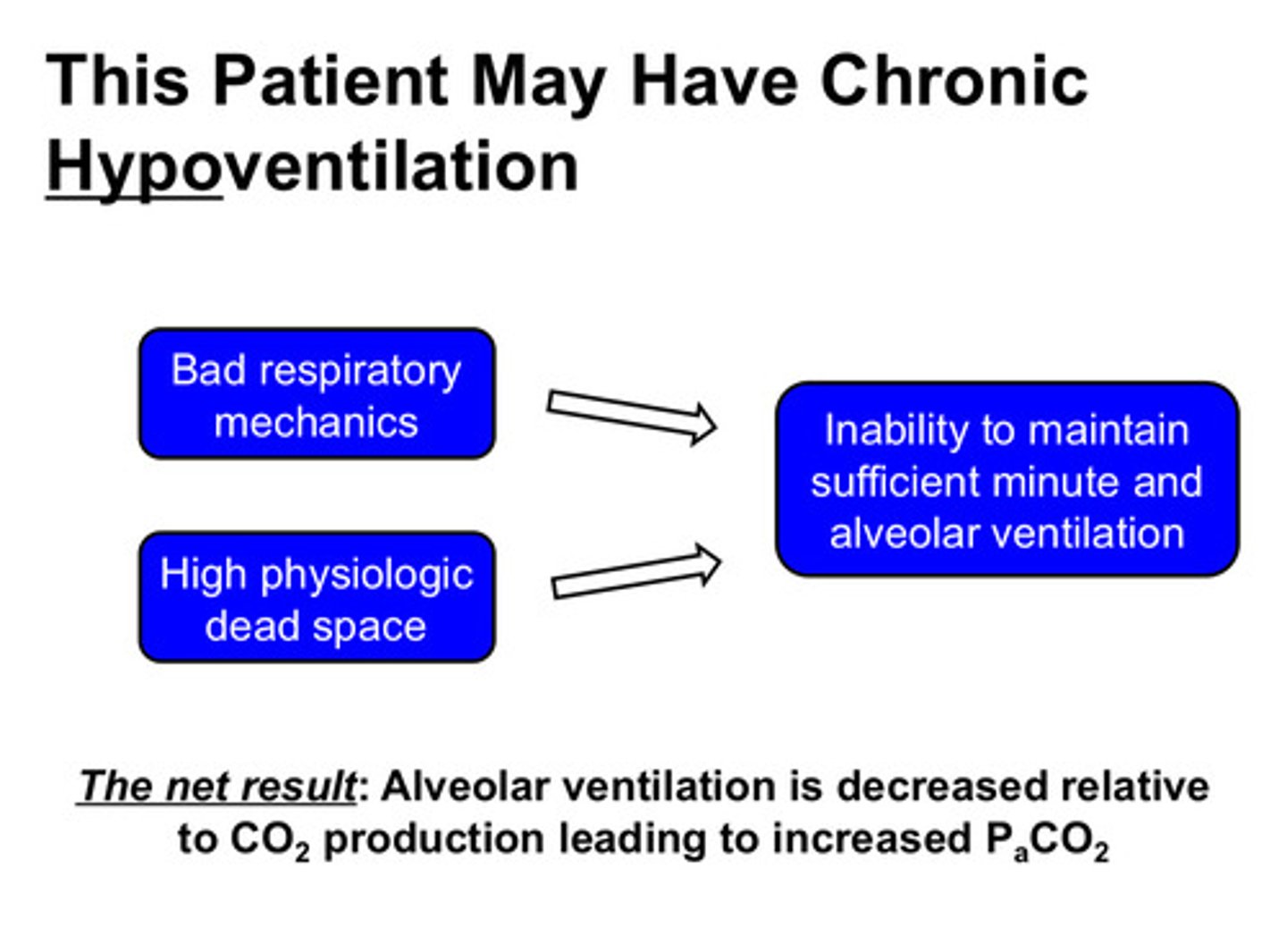
2) people with chronic dyspnea: bad respiratory mechanics + high physiologic dead space can lead to the inability to maintain sufficient minute and alveolar ventilation; alveolar ventilation is decreased relative to CO2 production, leading to increased PaCO2
note: patients with chronic CO2 retention still respond to changes in PCO2, but the magnitude of the response is decreased
what are the 2 main disorders of ventilation during sleep?
1) central sleep apnea
2) obstructive sleep apnea
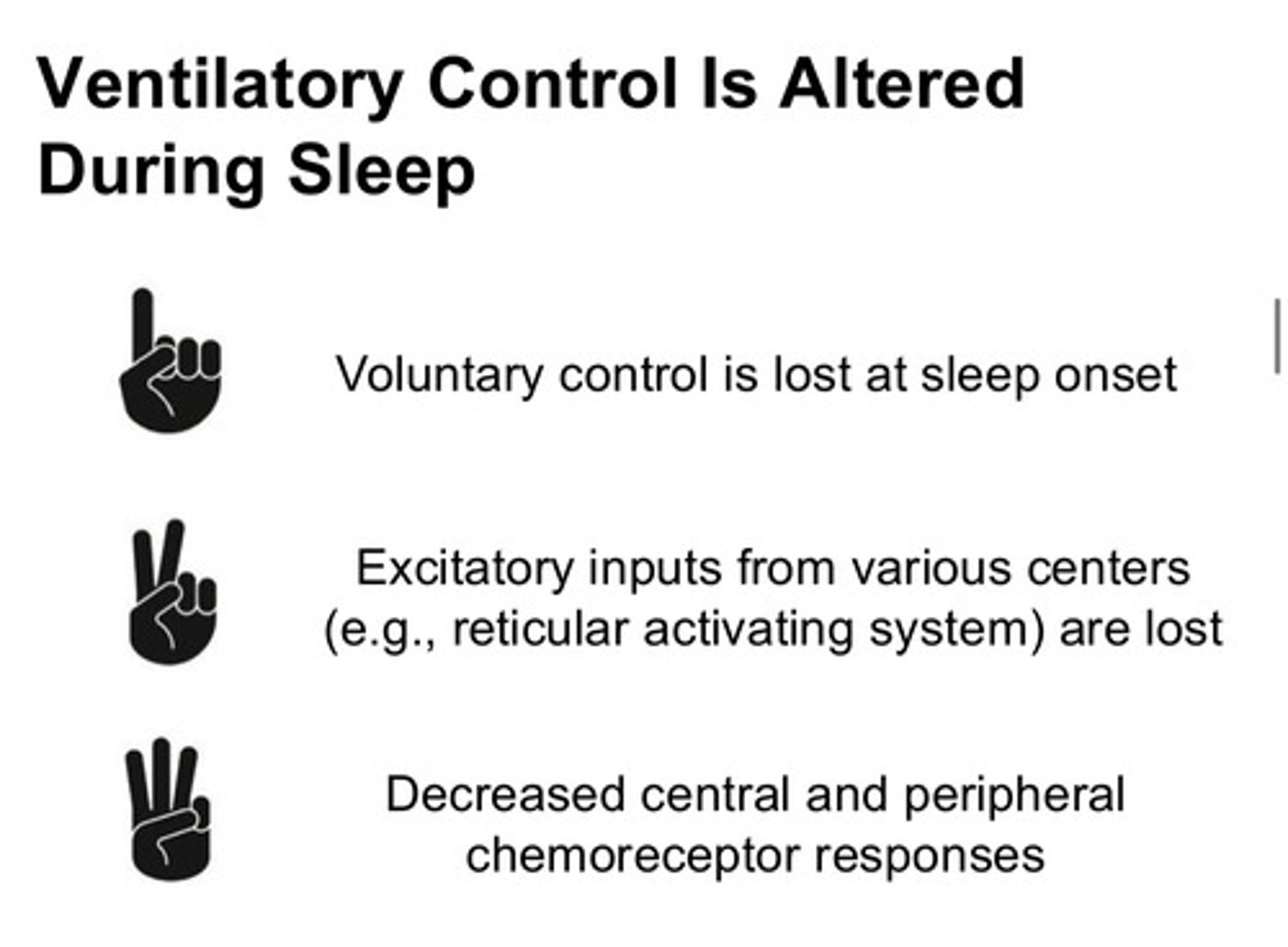
what normally happens to ventilatory control during sleep?
1) voluntary control is lost (because the person is asleep)
2) there is less stimulation from other excitatory brain centers
3) the central and peripheral chemoreceptors have decreased response
what does apnea mean
episodes of no airflow
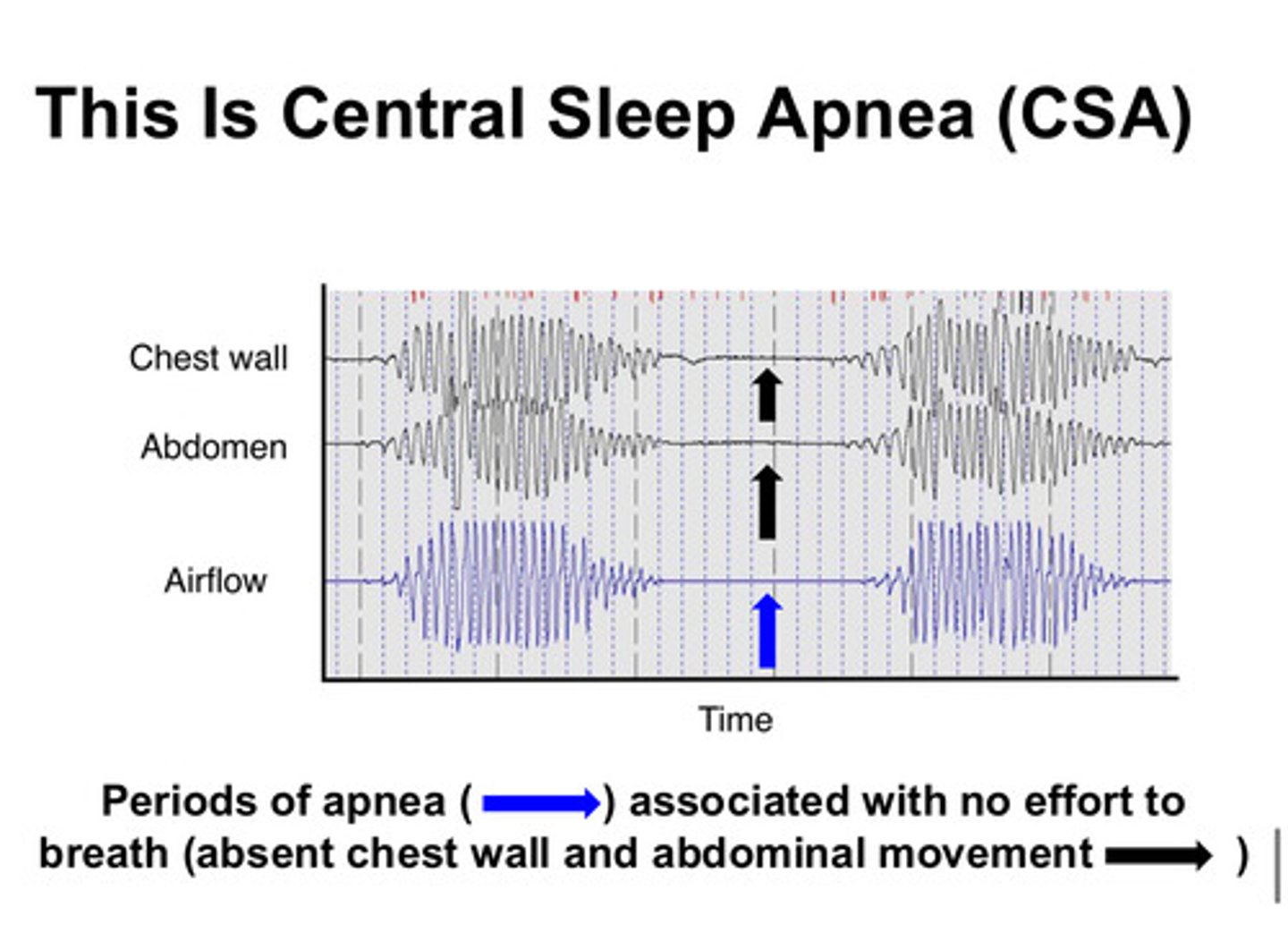
what is central sleep apnea and what is happening?
in CSA, there is a problem with the ventilatory control itself. the chemoreceptors either do not detect changes in PaCO2 appropriately or do not communicate to the control center appropriately. people have NO chest wall/abdominal movement or breathing efforts during periods of apnea
what is obstructive sleep apnea and what is happening?
in OSA, there is a problem (obstruction) in the pathway of the air into/out of the lungs. these patients will have episodes of no airflow in or out of the lungs, but they continue to have chest wall/abdominal movements as they attempt to breathe
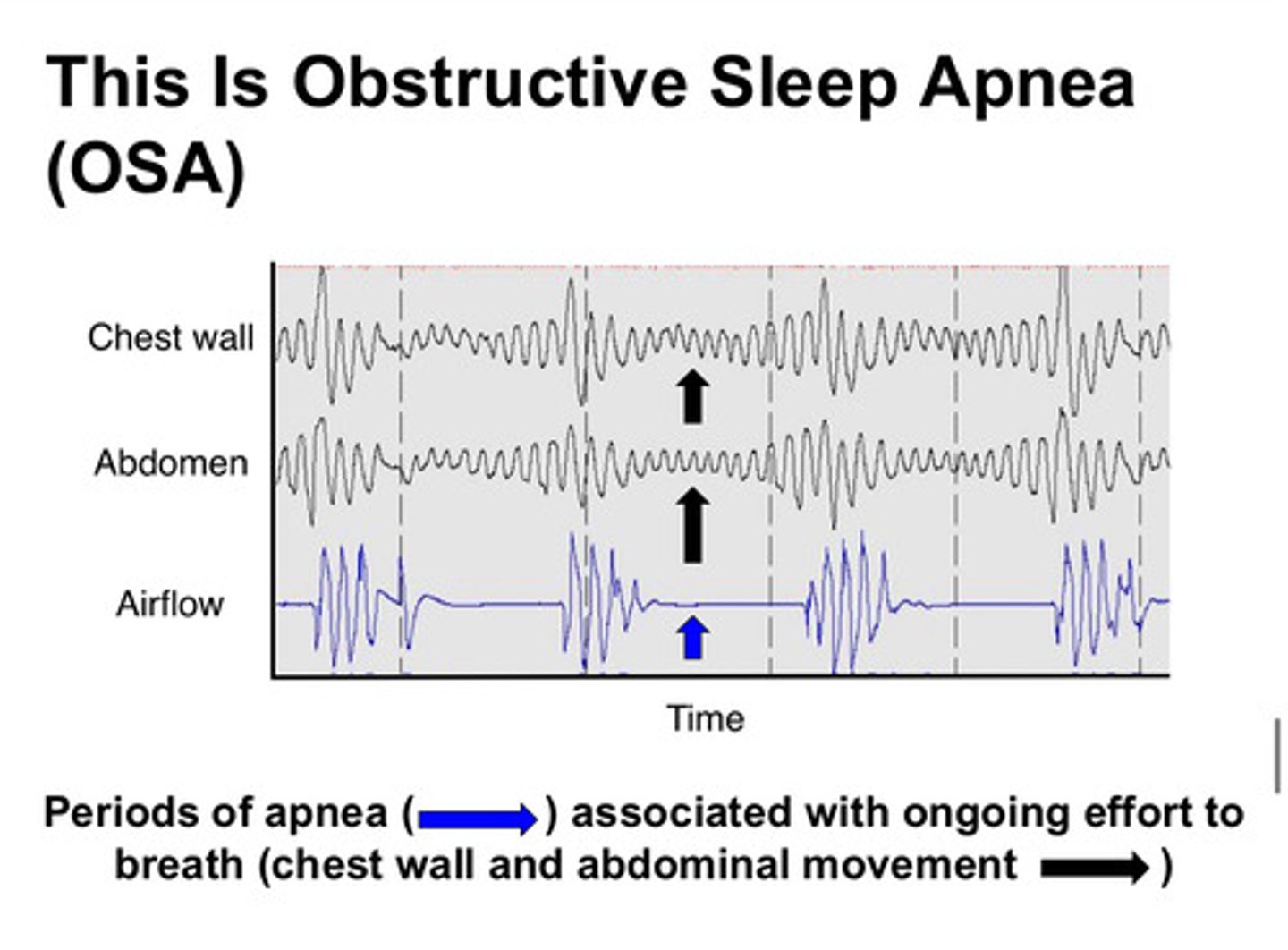
what are the differences between OSA and CSA?
OSA is an issue with air pathways, CSA is an issue with chemoreceptors; OSA has chest wall/abdominal movements, CSA have NO chest wall/abdominal movements
the difference between the 2 types of disorders of ventilation during sleep is very important because the treatments used to treat each are quite different from one another
key points