kine 427 morton final
1/316
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
317 Terms
What is pain?
Subjective sensation: “unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage”
Photobiomodulation absorption wavelengths
UV-B, UV-A, Blue (400-470) —— skin
Red (600-650) —— subcutaneous
infrared (>1350) HEAT
Universal contraindications
pregnancy
pacemakers
areas of sensitivity (eyes)
sites of infection or accute inflammation
tumors or cancerous lesions
metal implants
pain or diminish sensation
open wounds
ABCs of Pain perceptions (3)
Affective - one’s emotional factors affect pain experience
Behavioral - how one expresses or controls pain
Cognitive - one’s beliefs (attitude) about pain
BIOWAVE EXPLANATION
BioWave is a non-invasive, high-frequency electrical stimulation device used in pain management and tissue healing. It delivers high-frequency pulsed current (HFPC) to target tissues, which modulates pain signals and promotes healing at the cellular level.
How It Works:
High-Frequency Stimulation: BioWave emits electrical pulses at frequencies (typically 10,000 Hz or higher) that penetrate deep into tissues without causing muscle contractions.
Pain Gate Mechanism: The electrical impulses interfere with pain signal transmission by activating non-painful nerve fibers (A-beta fibers), effectively "closing the gate" to pain signals in the spinal cord.
Enhanced Circulation & Healing: The stimulation increases local blood flow, reduces inflammation, and promotes the release of endorphins and other healing factors.
Cellular Effects: The electrical currents may enhance ATP production, reduce edema, and accelerate tissue repair by influencing ion channels and cellular metabolism.
Influence on Tissue Healing:
Reduces Inflammation: Modulates pro-inflammatory cytokines.
Accelerates Repair: Stimulates fibroblast activity and collagen synthesis.
Decreases Pain: Allows for improved mobility and faster recovery.
Pain vs. Nociception
nociception is the neurophysiological process that may be interpreted as pain
pain is the unpleasant sensation
Where does pain come from (4 major categories)
Nociceptive (somatic, visceral, cutaneous)
Neuropathic (peripheral, central)
Psychogenic
Carcinogenic
Cutaneous pain
sharp, bright, burning; can have fast or slow onset
Deep Somatic pain
stems from tendons, muscles, joints, periosteum, and blood vessels
Visceral pain
originates from internal organs; diffuse at first then may be localized
Psychogenic pain
individual feels pain but cause is emotional rather than physical
Pain Sources
Fast - localized through A-Delta axons in skin
Slow - aching throbbing burning carried by C Fibers
What is referred pain?
occurs away from pain site
Noxious means…
harmful, injurious
Nociceptor
nerve receptor that transmits pain impulsesP
Pain Threshold
level of noxious stimulus required to alert an individual of a potential threat to tissue
Pain Tolerance
amount of pain a person is willing or able to tolerate over the threshold
Accommodation phenomenon
adaptation by the sensory receptors to various stimuli over an extended period of time (less sensitive over time)
Hyperesthesia
abnormal acuteness of sensitivity to touch, pain, or other sensory stimuli
Paresthesia
abnormal sensation such as burning, pricking, tingling
Inhibition
depression or arrest of a function
Analgesic
a neurologic or pharmacologic state in which painful stimuli are no longer painful
Types of Nerves
Afferent (Ascending) transmitting from periphery to brain
first second and third order neurons
Efferent (Descending) transmitting from brain to periphery
First Order Neurons
Stimulated by sensory receptors, end in dorsal horn of spinal cord
A-Alpha: non pain
A-Beta: non pain
A-Delta: pain due to mechanical pressure (SHORT/FAST)
C Fibers: pain due to chemical or mechanical (SLOW)
Second Order Neurons
Lamina II, Substantia Gelatinosa (SG) determine the imput sent to T Cells from peripheral nerve
T Cells organize and transmit to CNS (brain)
ENDS IN THALAMUS
Third Order Neurons
Begin in Thalamus
ends in specific brain centers
perceive location, quality, intensity
integration of past experiences and emotions to determine reaction to stimulus
Neurotransmitters
Chemical substances that allow nerve impulses to move from one neuron to another
Substance P Neurotransmitter
responsible for transmission of pain producing impulses
Acetylcholine Neurotransmitter
transmits motor nerve impulses
Enkephalins Neurotransmitter
reduces pain perception by bonding to pain receptor sites
Norepinephrine Neurotransmitter
causes vasoconstriction
2 types of chemical neurotransmitters that mediate pain
Endorphins (morphine like, incr. pain threshold)
Serotonin (local vasodilation, incr. permeability of capillaries)
4 types of Sensory Receptors
Mechanoreceptors - touch, light or deep pressure
Thermoreceptors - hot/cold
Proprioceptors - change in length or tension
Nociceptors - painful stimuli
Nerve endings are
termination of a nerve fiber in a peripheral structure
endings may be sensory or motor
nociceptors and sensitivity
sensitive to repeated or prolonged stimulation
mechanosensitive - excited by stress & tissue damage
chemosensitive - excited by the release of chemical mediators
Neuroanatomy: synapse
“Lock and Key”
unique receptor shape for neurotransmitters allows for competitive inhibition (morphine)
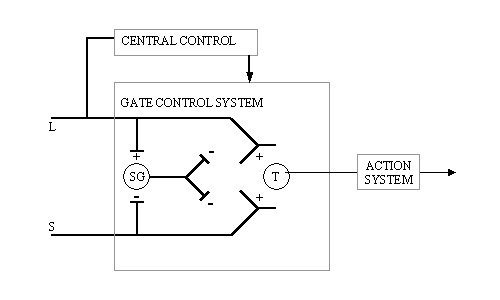
Gate Control Theory of Pain
Operates @ Spinal Level, proposing single gate mechanism located in the Second Order Neurons
Both large and small fibers stimulate T Cells which pass information to the action system, but they stimulate differently— Large fiber = + on SG, Small fiber = - on SG
Inhibitory mechanism located in the SG (inhibiting T Cell)
Central Control (brain) inhibits or facilitates the T cell directly. Central control integrates information from multiple sources.
Neuromatrix Theory of Pain
“multidimensional experience"
produced by characteristic neurosignature patterns of nerve impulses
patterns may be triggered by or independent of sensory inputs
Acute pain is evoked by brief noxious inputs transmitted to and processed by the CNS as described by the gate control theory
Neuromatrix: unique to each individual, initially determined by genetics, heavily modified throughout life/experiences
Questions to ask about pain
Pattern (onset & duration), Area, Intensity, Nature (description)
Pain assessment scales
Visual & Numeric analog scales, locate area of pain on picture scales
5 distinct and successive physiologic phases of experiencing pain
Transduction (converting energy)
Peripheral Transmission Phase
Modulation Phase (suppression/amplification)
Central Transmission Phase
Perception Phase
Variability of pain tolerance
varies from person to person and episode to episode
Learned pain
conditioned response which develops from pain memories of physiological and emotional elements of either nociceptive or neuropathic pain experience
Goals in managing pain
reduce & control
protect from further injury while encouraging progressive exercise
Drugs and Pain relief
Morphine blocks pain (fills NT binding site)
Bradykinin
directly stimulates nociceptors
Prostaglandins
sensitization of the nerve fibers so that other mediators can enhance nociception
Substance P
NT released centrally to produce the pain response and peripherally producing hyperalgesia and inflammatory responses
Histamine
released by mast cells to directly stimulate nociceptors
Pathology of pain
Referred pain - pain is felt some distance away from actual site
Phantom pain - following amputation pain in missing limb (neuroma, ectopic activation)
Problem Solving Approach (PSA) incorporates
Clinical exam findings, long term goals, available evidence
Treatment and Rehab program planning integrates
Clinical exam skills, knowledge of pathology, goal settings, patient motivation and education, knowledge of physiological effects of therapeutic techniques, id of the patient’s level of function
Internal Classification of Function (ICF)
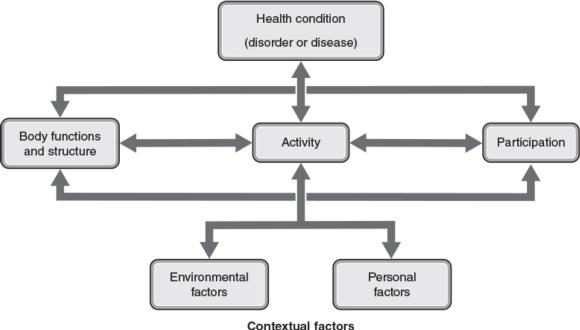
Disease oriented approach
interventions focused on resolving pathology
Patient oriented approach
interventions focused on factors that are meaningful to the patient
Minimum detectable change (MDC)
smallest clinically significant difference in the scores of 2 administrations of the instrument; useful in determining the efficacy of an intervention
Minimally clinically important change (MCID)
measure of responsiveness, smallest change that is important or beneficial to patient
the goal of evidence based practice is to
provide most efficient effective treatment, maximizing outcomes and making effective use of time
Factors to consider when choosing modality
can energy produced by modality directly or indirectly affect target tissues?
can modality produce the physiological response required to promote healing?
does this device improve patient outcomes better than a placebo treatment or no treatment at all?
PICO meaning?
Patient, intervention, comparison, outcome - provides a structure for developing clinical questions
PSA approach steps
Obtain medical history
Identify patient activity limitations
Prioritize the problems
Set treatment
Review evidence
Plan interventions
Re-examine patient and assess outcomes
Medical History
review existing records
identify contraindications to specific interventions
problem recognition
conduct formal patient examinations & re-examinations regularly
Long term goals
indentify and quantify the final outcomes of the program
focus on restoring participation rather than addressing the individual pathologies afflicting the person
Short Term goals
2 weeks or less
describe patient’s projected progress in a specific time and focus on the specific problems identified during the examination (and if they will achieve long term goals)
Treatment planning
application of knowledge of the physiological effects of the therapeutic modalities and exercise to resolve the problems required to achieve the patient’s goals
Considerations of the healing stage
Active inflammatory stage (decrease inflammation, reduce secondary hypoxic injury and control edema)
Proliferation phase (increase blood flow to and from injured tissue while trying to control edema)
Maturation phase (increase tissue extensibility and control post-exercise inflammation)
patient self treatment
instructions should be given to the patient in writing, and illustrations that depict the exercises to be performed are also helpful
Reexamination
if short term goals are met, create new ones
if not met, identify why
develop new treatment plan
re-administer outcome measures
influences on patient care
treatment setting, experience and expertise of staff, type of equipment available, time and financial constraints
why keep records?
communication and quality control
legal considerations
research
injury history
traffic patterns
Legal considerations in patient care
professional ethics and responsibility mandate the care provided be in the best interest of the patient, be safe and effective, and progress toward meeting the patient’s goals.
Scope of Practice
legal boundaries that define the manner in which clinicians may practice
Medical prescription
therapeutic modalities that require prescription medications necessitate that each patient have a prescription
informed consent
except in cases of emergency care, patients must grant their consent to be treated
seeking treatment implies consent
patient confidentiality
Health Insurance Portability and Accountability Act (HIPAA) affects past present and future medical records and seeks to ensure confidentiality by controlling protected health information (PHI)
Family Education Rights Privacy Act (FERPA) protects education records, including medical files, from unauthorized release
Negligence
providing care that falls below the minimally accepted standard
omission occurs when an individual fails to response to a given situation
commission occurs when an individual acts on a situation but does not perform at the level that a reasonable and prudent person would
negligent care of facilities
food and drug administration oversight
major regulator of over the counter and prescription medications
occupational safety and health administration regulations (OSHA)
prevent work related injuries and illnesses and through enforcement branch fines or prosecutes employers who do not comply with these standards
medical documentation
if it wasnt documented it wasnt done
each state’s statute of limitations determines the length of time that medical records should be kept after the patient is no longer receiving care
treatment rendered and patient progress
documentation of the day’s treatments should describe the date, time, individual or individuals providing the care, the pathology treated, the modalities and exercises used and parameters used
legal record
well-documented records assist in proving that staff exercised reasonable patient care if a liability were to come to trial
reimbursement documentation
therapeutic services billed for this purpose wil be reimbursed only if they meet the patient’s treatment goals
legal considerations
most lawsuits occur years after the event usually after the memory of specific details are gone
records supply proof
facilities
physical facility where care is given must be free of potential hazards and be conducive to patient care, including access by disabled patients or clinicians
hydrotherapy area, treatment area, plumbing and electrical are of special concern
product maintenance
requires regular inspection for defects/hazards, periodic cleaning, and professional calibration according to manufacturer recommendations
SAID principle
Specific Adaptation to Imposed Demands
body responds to a given demand with a specific and predictable adaptation
Atrophy vs. Hypertrophy
Atrophy
protein synthesis ↓
protein degradation ↑↑
Hypertrophy
protein synthesis ↑↑
protein degradation ↓
Principle of Specificity
exercise adaptations specific to mode and intensity of training
must stress most relevant physiological systems for given sport
training adaptations highly specific to type of activity, training volume, and intensity
Muscle Overload
muscles must be loaded beyond normal loading for improvement
strength training
high resistance 2-10 RM training
gains in strength
Primary signals of resistance training in muscle fiber
Muscle stretch increase = microtears → igf-1 , Akt, mTOR → protein synthesis
Signal timing for protein synthesis
hours post exercise incr. protein synthesis
muscular hypertrophy most important aspect
the load
mechanisms of muscle strength gain: fiber type alterations
type IIx → type IIa transition common
muscular endurance is the ability to
make repeated contractions against a submax load
endurance training involves
low resistance training 20+ RM
Primary signals for resistance training
increase in Ca2+, AMP/ATP, Free Radicals
post exercise endurance training
days post exercise = increase in PGC-1 and mitochondrial biogenesis
endurance training induced changes in fiber type
fast to slow shift in muscle fiber type
increased # of capillaries