Thorax & Lungs
1/81
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
82 Terms
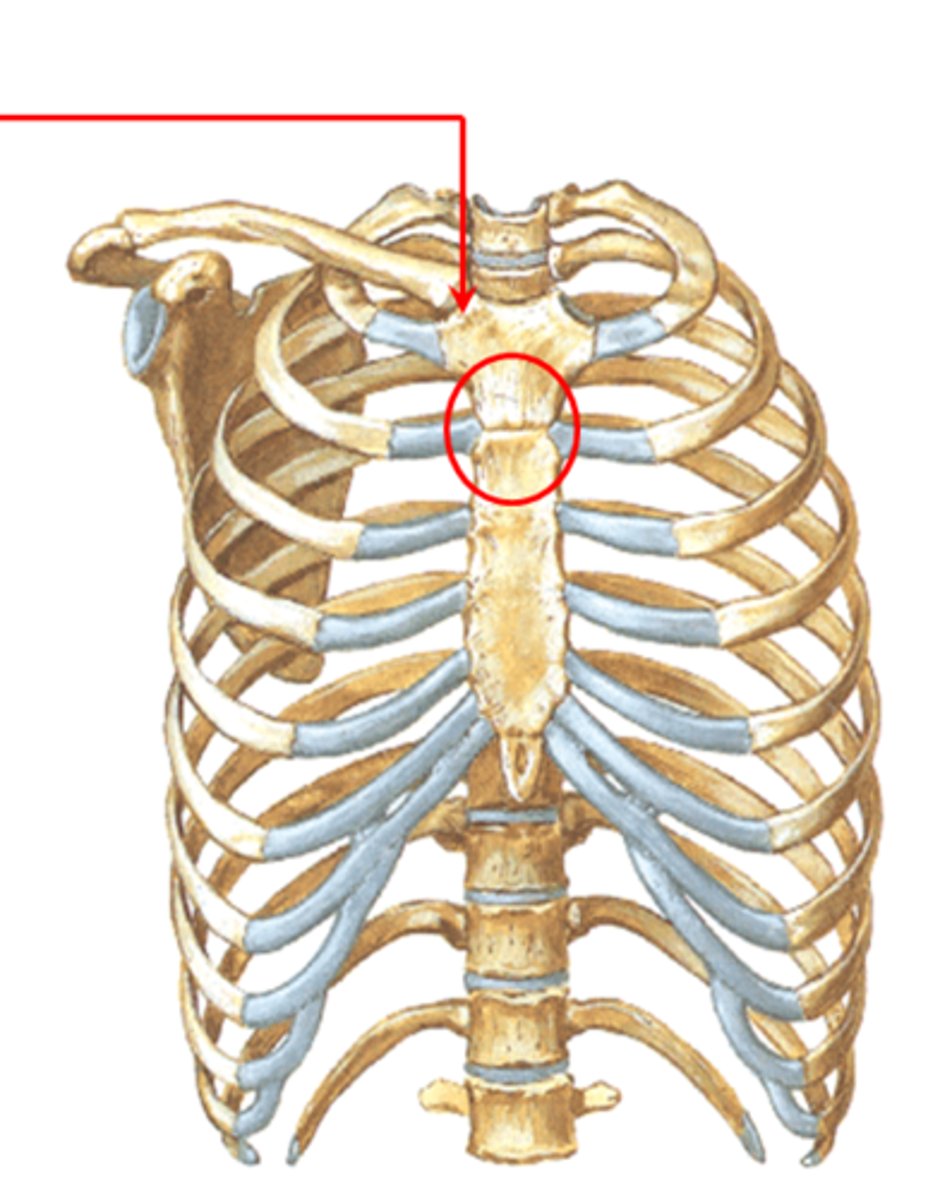
Angle of Louis (sternal angle)
*marks trachea bifurcation into 2 main stem bronchi
*corresponds with upper border of atria
*continuous with 2nd rib
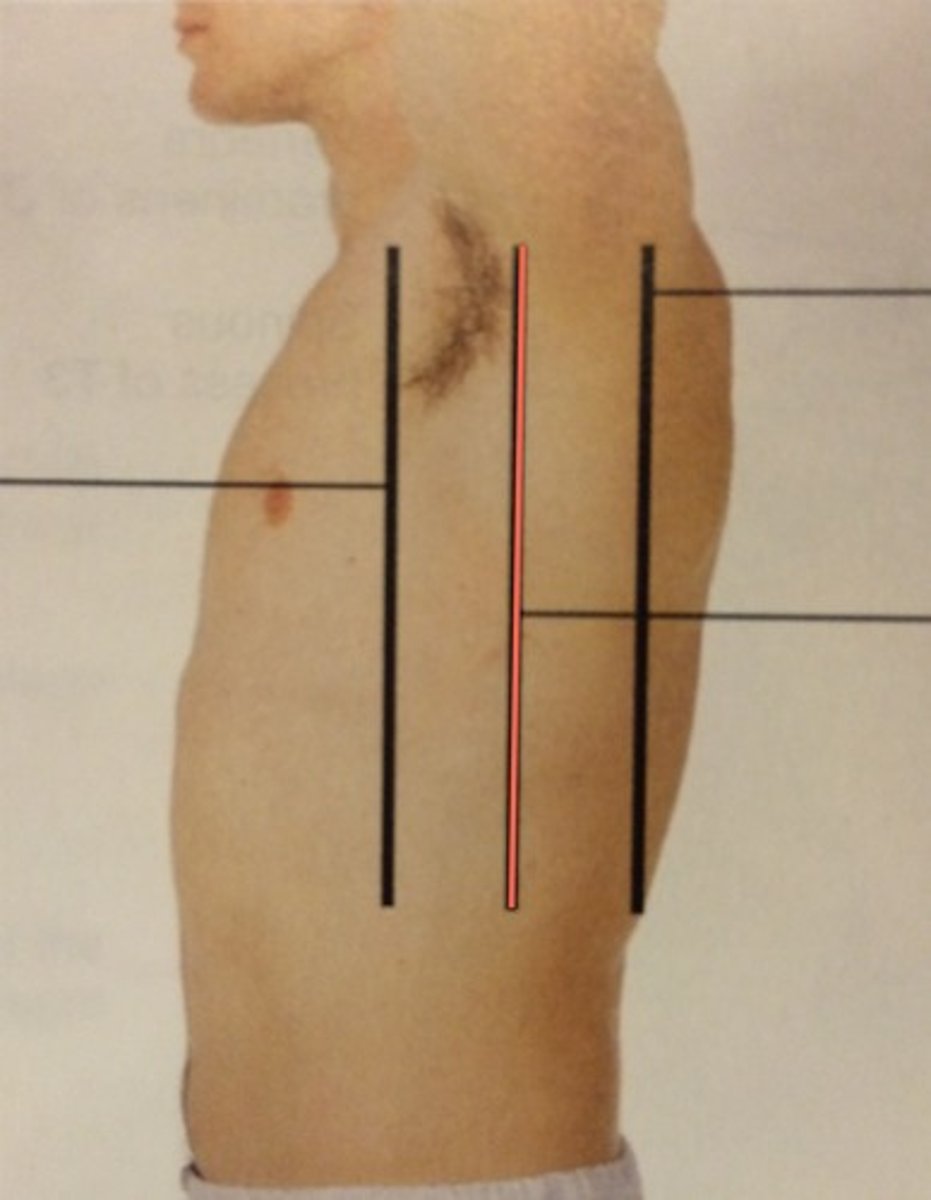
midaxillary line
left lung
2 lobes separated by oblique fissure
*upper lobe extends from apex to 5th rib/midaxillary line
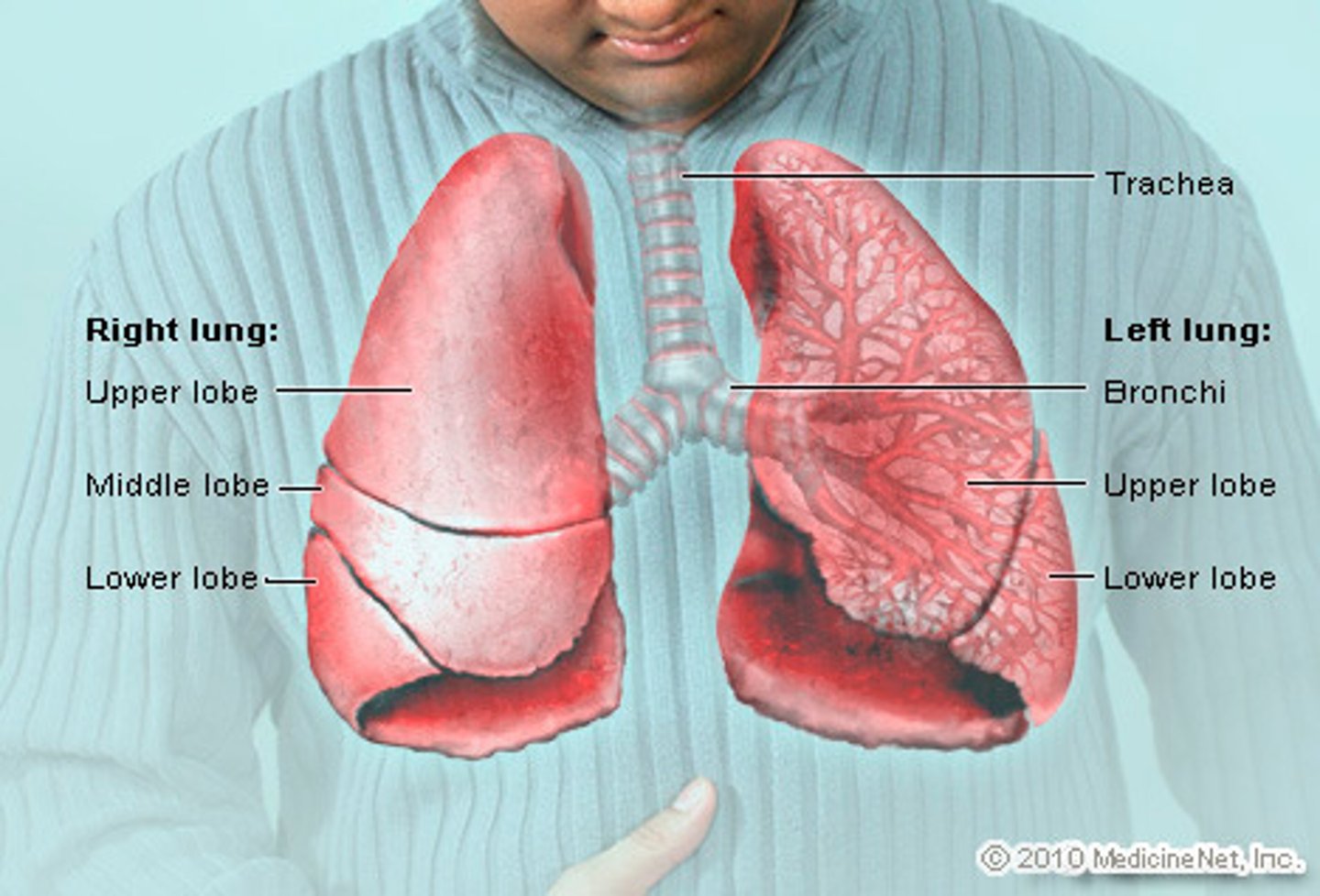
right lung
3 lobes separated by horizontal and oblique fissures
*upper lobe extends from apex to horizontal fissure at 5th rib
*middle lobe extends from horizontal fissure down and forward to 6th rib
Laterally, the lung tissue extends from _____ to _____ fissure at _____ rib.
apex
horizontal
5th
pleura
thin, slippery double-layered membrane surrounding each lung; forms an envelope between the lungs and chest wall
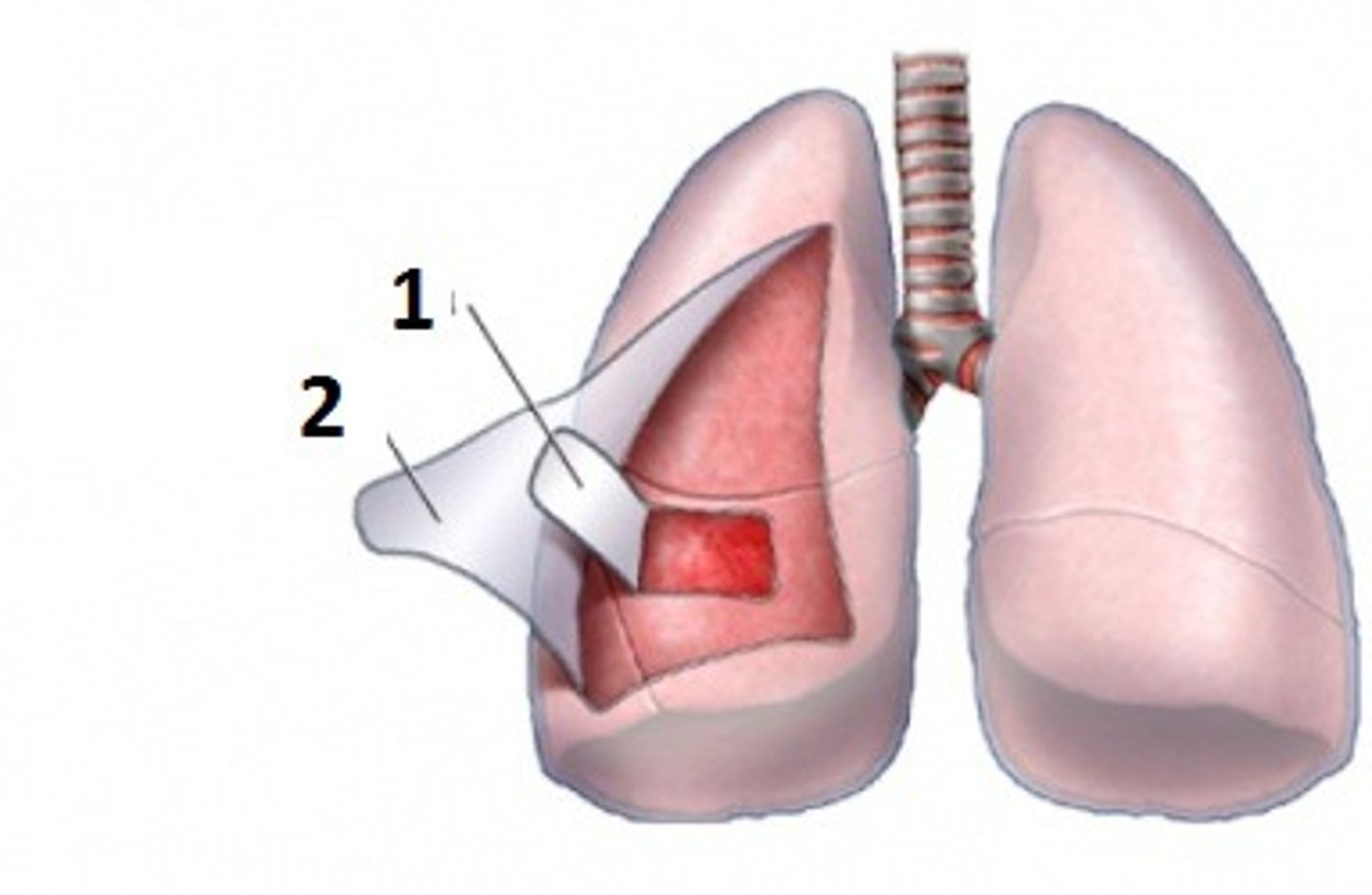
visceral pleura
inner layer of pleura that envelopes the lung tissue
parietal pleura
outer layer of pleura lying closer to the ribs and chest wall
Swallowed foreign objects usually go into the _____ main bronchus.
right
*because it is shorter, wider, and more vertical than left main bronchus
4 major functions of respiration
1. supply oxygen for energy production
2. eliminate CO2 as a waste product
3. maintain homeostasis (acid-base balance)
4. thermoregulation (less essential)
hypercapnia
excessive CO2 in the blood
*normal stimulus to breath
hypoxemia
deficient oxygen in the blood
*also stimulates respiration, but not as effectively as hypercapnia
A cough is defined as "chronic" if it has been present for _____ months.
2+
continuous coughing is often a sign of...
an acute issue, such as a respiratory infection
intermittent coughing is often a sign of...
exposure to an irritant
night coughing is often a sign of...
postnasal drip or sinusitis
describing cough quality
hacking / dry / barking / congested
*dry cough common in early HF
*congested cough common in cold, bronchitis, pneumonia, etc.
dyspnea
difficulty breathing; also called "shortness of breath"
orthopnea
ability to breathe only in an upright position
hemoptysis
coughing up blood
subjective data: health history
current cough? if so, productive or non-productive?
dyspnea?
orthopnea? (# of pillows)
chest pain with breathing?
hemoptysis?
history of respiratory infections?
history of smoking? (pack years)
environmental exposures?
self-care measures?
1. inspect chest wall posteriorly
for shape, configuration, skin abnormalities, skin color changes
*anterior-posterior diameter should be 1/2 of transverse chest (EXCEPT neonates)
*spinous processes should be symmetric, midline
*scapulae should be symmetric b/l
*skin color should be consistent with patient's ethnic background
*costal angle should be < 90 degrees
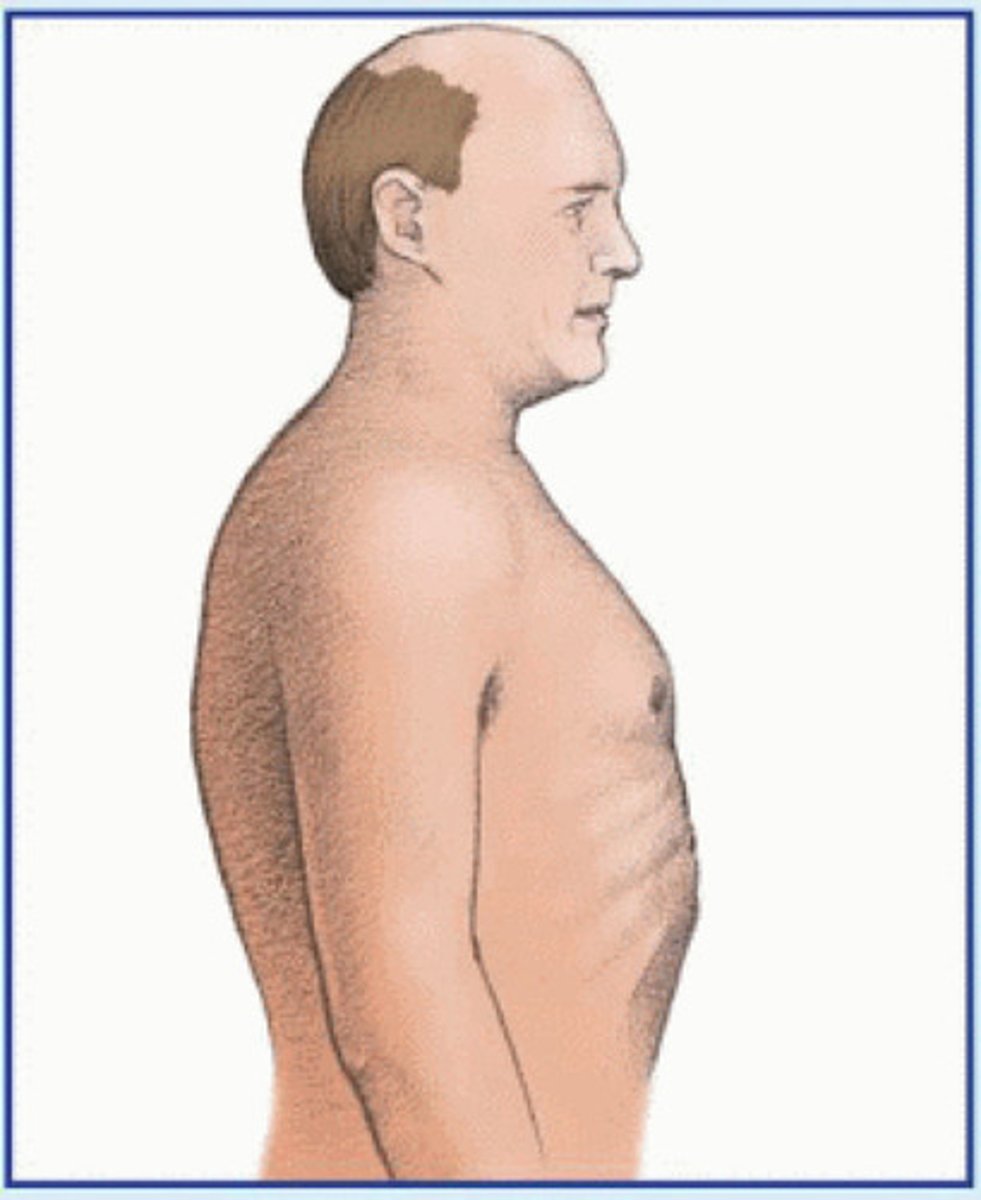
barrel chest
a condition characterized by increased anterior-posterior chest diameter caused by increased functional residual capacity due to air trapping from small airway collapse
*frequently seen in patients with COPD, such as chronic bronchitis and emphysema
pectus excavatum
sunken sternum and adjacent cartilages

pectus carinatum
forward protrusion of the sternum

scoliosis
abnormal lateral curvature of the spine
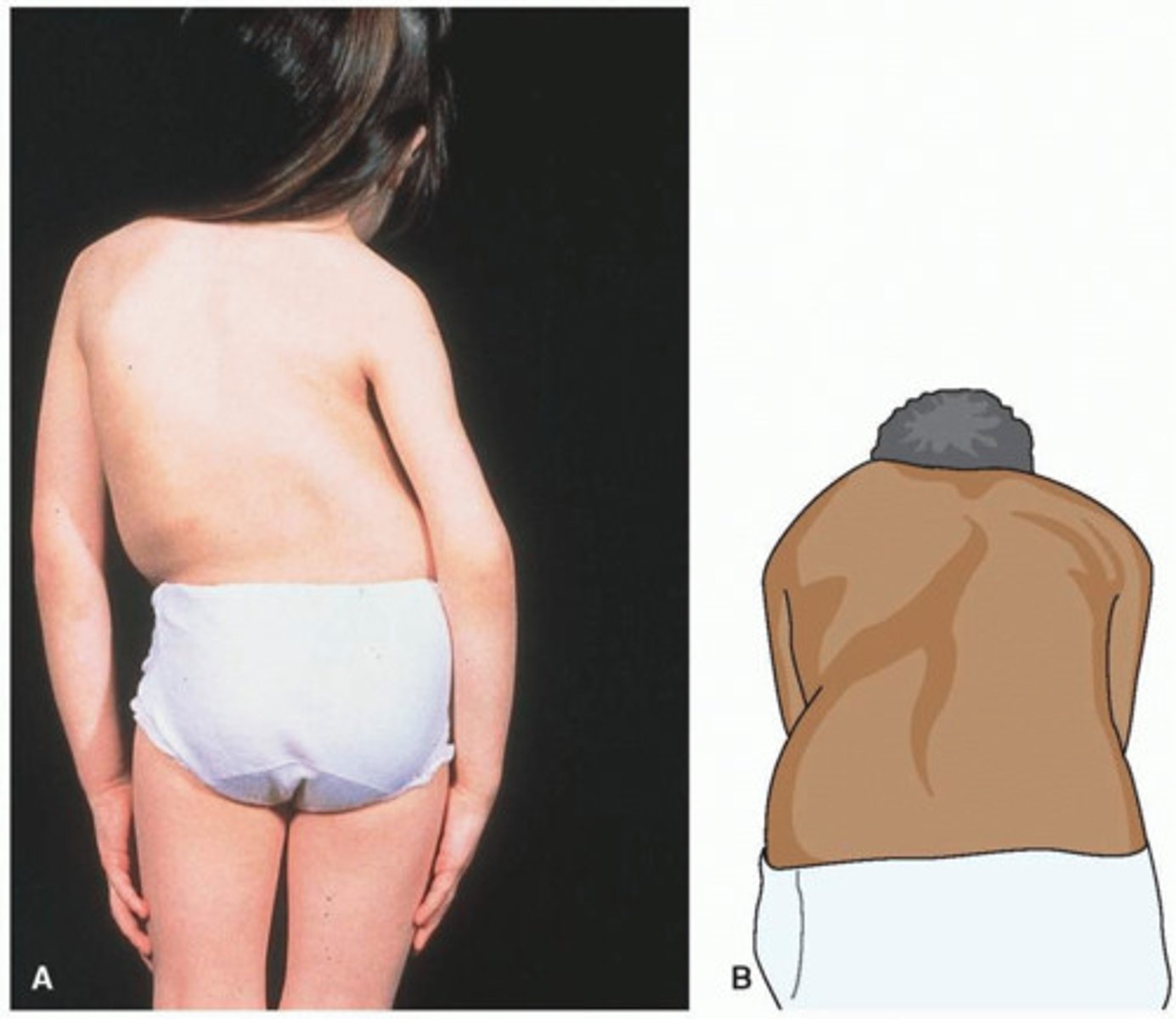
kyphosis
excessive outward curvature of the spine causing hunching of the back

2. inspect facial expression
to determine WOB
*position should be relaxed
tripod position
an upright position in which the patient leans forward onto two arms stretched forward and thrusts the head and chin forward; typically seen in patients having difficulty breathing

3. inspect respirations
for rate, rhythm, quality
*should be effortless, regular, even
tachypnea
abnormally rapid breathing (> 20 bpm). Lower tidal volume
causes: fever, pain, heavy exercise
bradypnea
abnormally slow breathing (< 12 bpm)
causes: some drugs, increased intracranial pressure
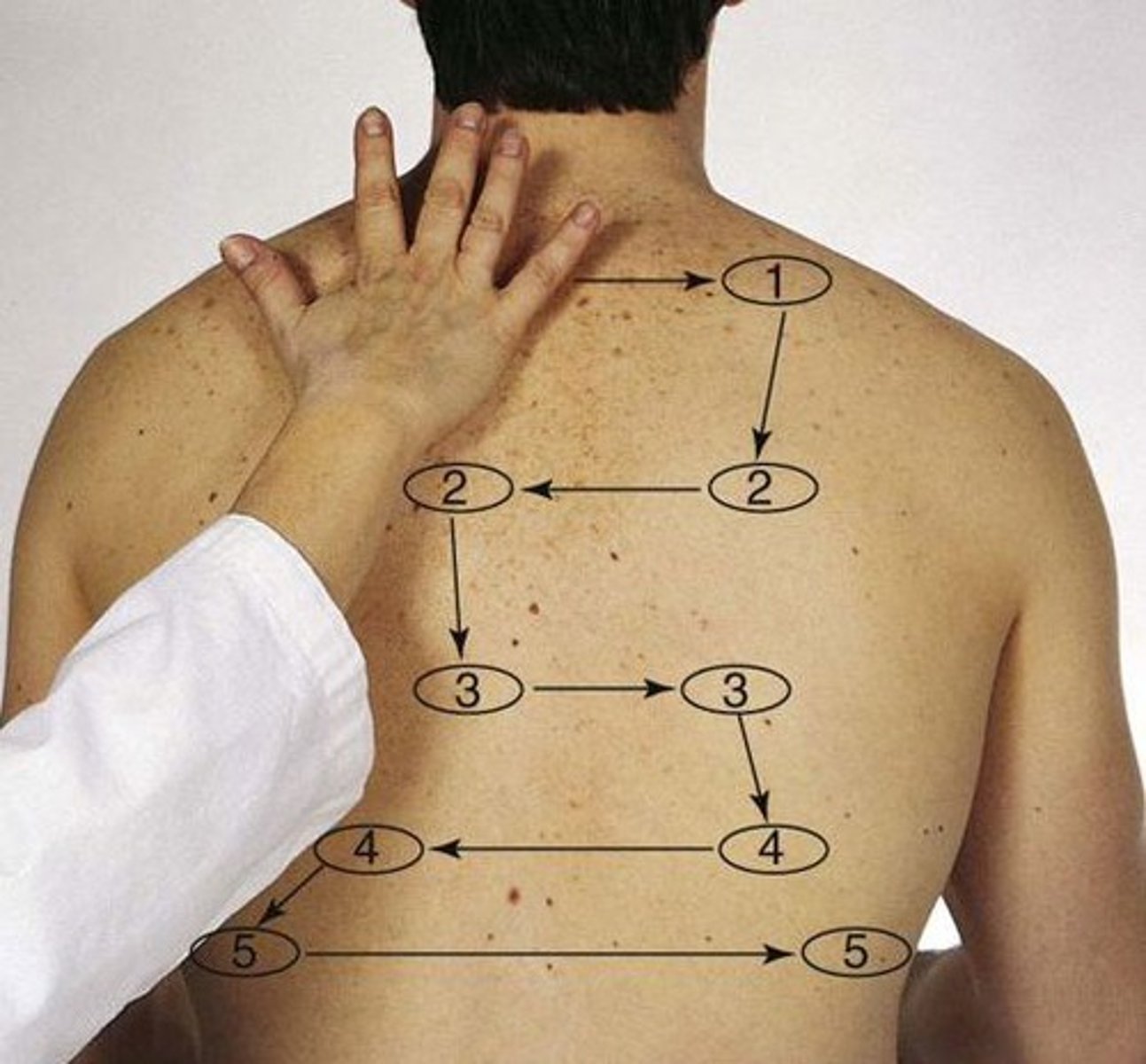
Cheyne-Stokes respirations
a distinct pattern of breathing characterized by quickening and deepening respirations followed by a period of apnea
causes: CHF, renal failure, increased intracranial pressure, dying patient
Biot's respirations/ ataxic
varying depth and rate of breathing, followed by periods of apnea; very irregular breathing pattern
causes: head trauma, brain abscess, heat stroke
chronic obstructive respirations
normal inspiration + prolonged expiration + air trapping
4. palpate posterior chest for symmetric expansion
1. place hands on posterior chest wall at T9 or T10 with thumbs along costal margins and pointing inward
2. ask patient to take a deep breath
3. watch thumbs move apart symmetrically and note smooth expansion

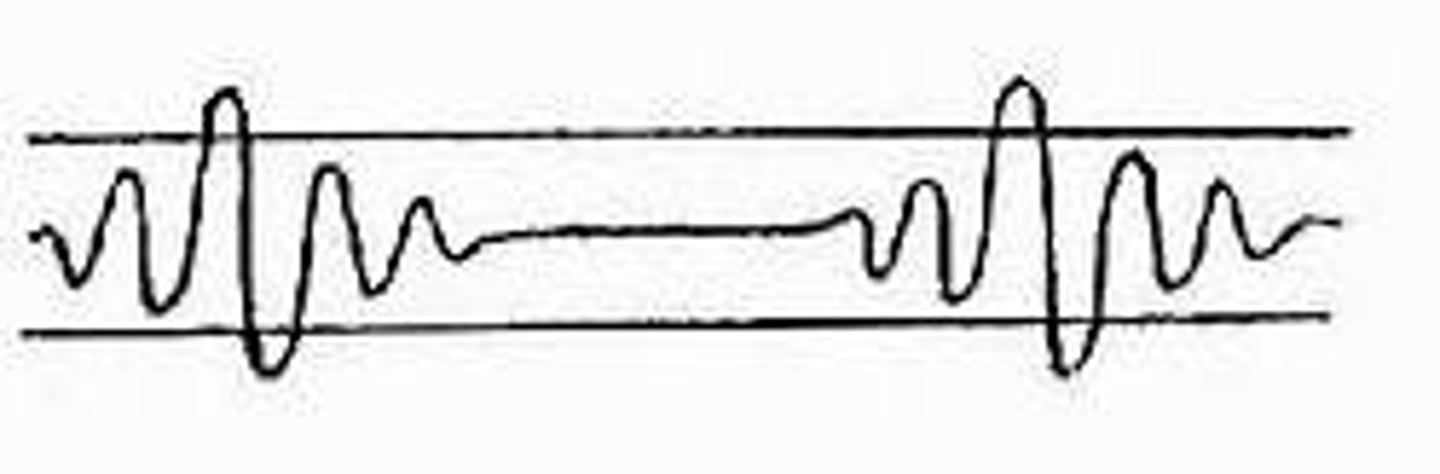
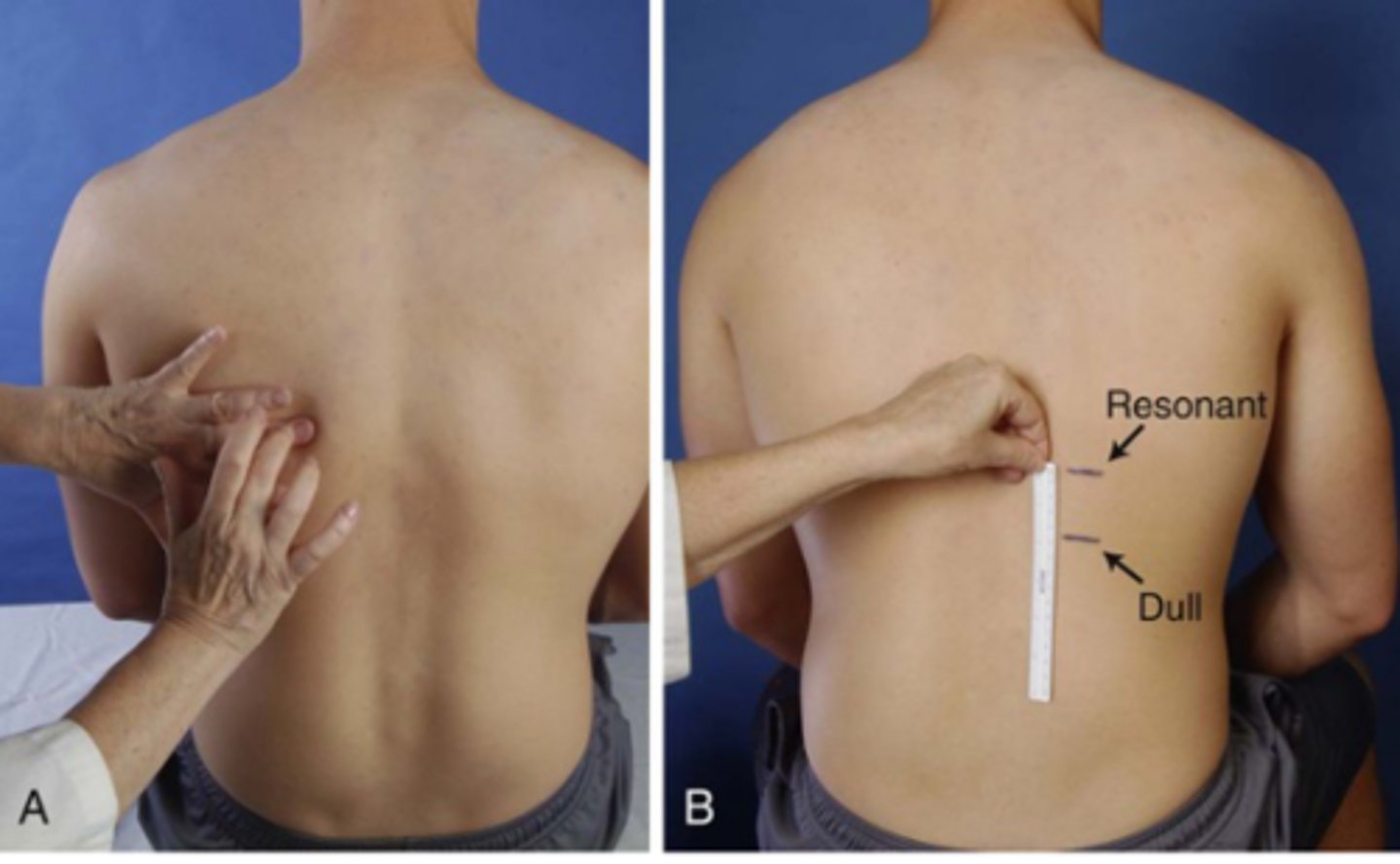
5. palpate posterior chest for tactile (local) fremitus
using palmar base of finger or ulnar edge, touch chest while patient says "99", moving in a zig-zag pattern from the apices and palpate from side to side or compare sides
*vibrations should be equal b/l
*increased tactile fremitus = consolidation of lung tissue (e.g. pneumonia)
*decreased tactile fremitus = obstruction in bronchi, PE, emphysema
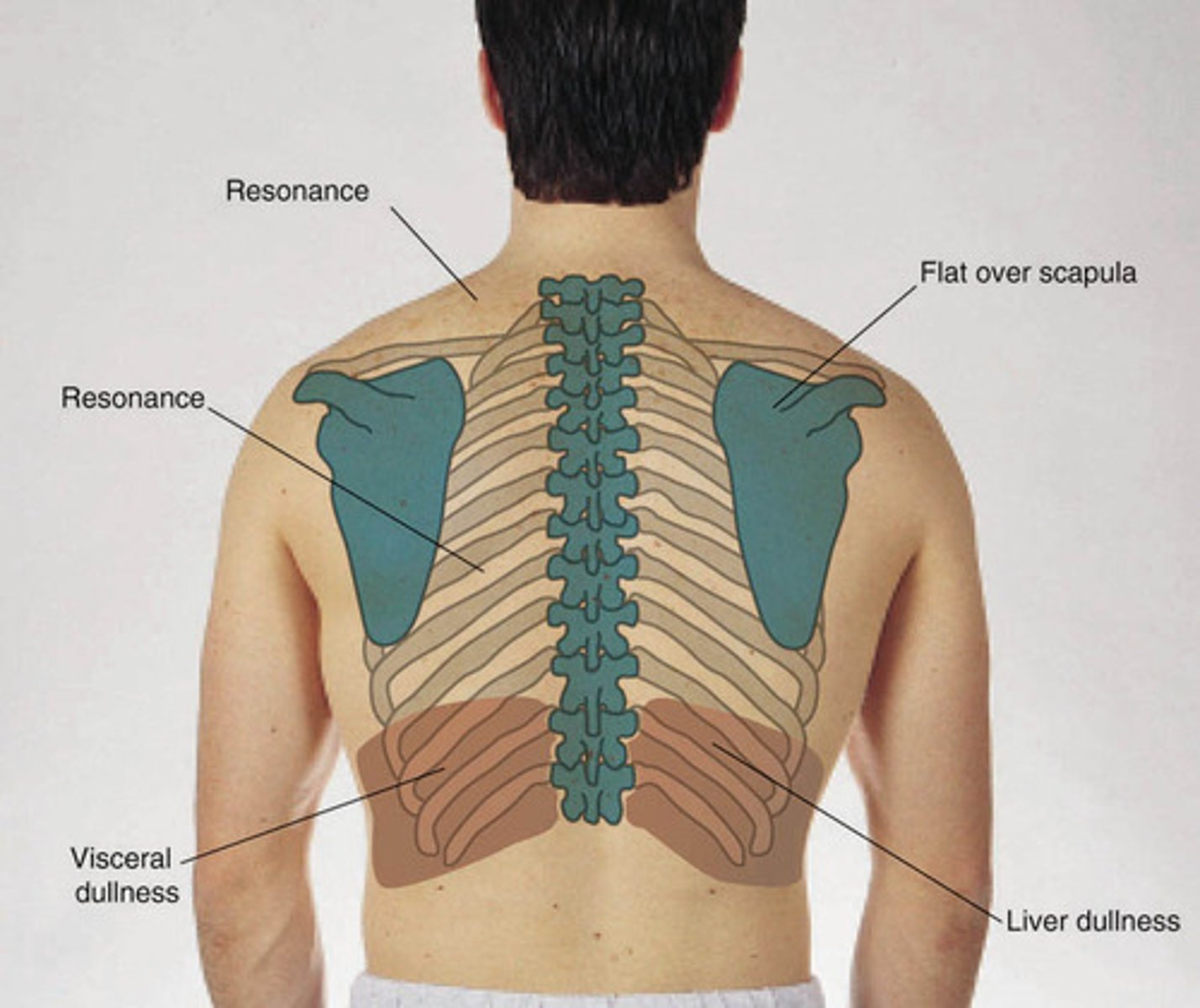
6. percuss posterior chest for symmetry
sounds over lung tissue should be resonant b/l
hyperresonance = overinflation (e.g. emphysema)
7. percuss posterior chest for diaphragmatic excursion
1. ask patient to exhale and percuss down to dullness
2. ask patient to inhale and percuss down to dullness again
3. measure the distance between the 2 lines
*difference should be equal b/l (3 - 5 cm)
*not used in clinical practice very much anymore
8. auscultate posterior lung fields for breath sounds
patient sits with hands in their lap, leaning slightly forward while breathing thought their mouth, a bit deeper than usual (may need to pause to prevent patient from becoming lightheaded)
hold diaphragm of stethoscope firmly on chest wall, listening to 1 full breath in each spot
decreased lung sounds = bronchial tree obstruction (secretions or forcing body), emphysema, any obstruction between lung and stethoscope (e.g. fluid in pleural space)
increased lung sounds = pneumonia
adventitious breath sounds
abnormal breath sound heard over the lungs
crackles (rales, crepitations)
crackling sound heard usually during inspiration that indicates an accumulation of fluid
fine crackles
high-pitched, short (like rubbing hair with fingers outside ear)
causes: air coliding w/ secretions or small airways popping open
coarse crackles
low-pitched, gurgly (like velcro opening)
causes: air bubbles moving through secretions in the large bronchi
sonorous wheezes
low-pitched snoring (like a musical snoring), musical sound made upon expiration air moves through narrowed or partially obstructed airway passages
causes: bronchitis
sibilant wheezes
high-pitched, squeaking
causes: asthma, HF
stridor
crowing sound during inspiration
causes: croup, airway obstruction
MEDICAL EMERGENCY!
pleural rub (friction rub)
scratchy sound produced by pleural surfaces rubbing against each other
causes:
9. auscultate posterior lung fields for transmitted voice sounds
ask patient to speak while auscultating lung fields
*voice should be heard as a soft, muffled, indistinct sound
if abnormal (increased lung density enhances transmission of voice sounds), assess:
1. bronchophony
2. egophony
3. whispered pectoriloquy
bronchophony
louder, clearer "99" reflecting transmission through airless tissue
indicates abnormality like pneumonia
normal: sounds are muffled and indistinct
egophony
"E" to "A" changes which occur in lobar consolidation from pneumonia
whispered pectoriloquy
louder, clearer whispered words reflecting transmission through airless tissue
normal: usually heard faintly or indistinctly, if at all
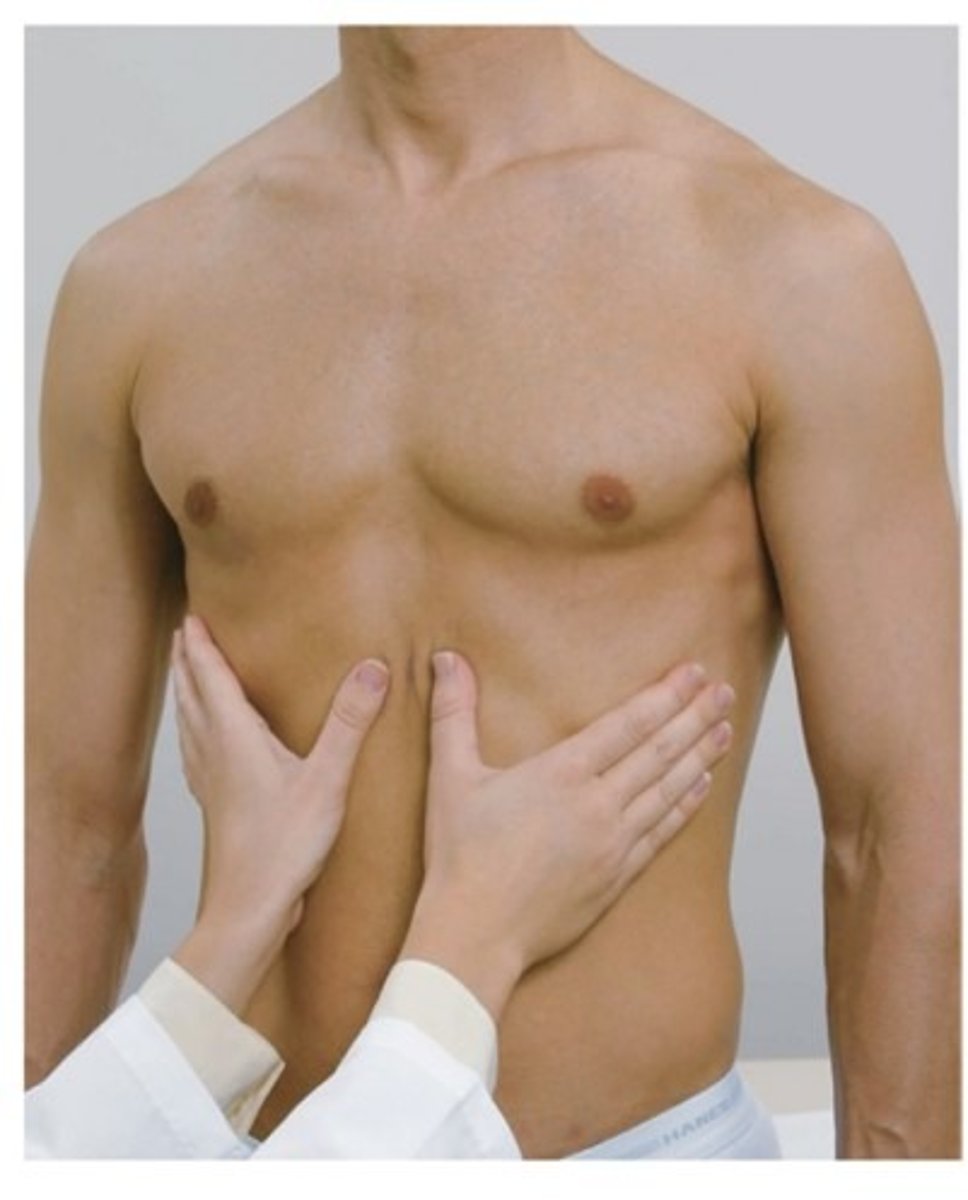
10. palpate anterior chest for symmetric expansion
1. place hands on anterior chest wall with thumbs along costal margins and pointing inward towards the xyphoid process
2. ask patient to take a deep breath
3. watch thumbs move apart symmetrically and note smooth expansion
12. percuss anterior chest
not usually done because there isn't much to percuss without observing changes in sounds over heart, liver, stomach, etc.
atelectasis
collapsed, shrunken section of alveoli or entire lung
signs:
- trachea may be shifted toward involved side
- percussion dull over airless area
- breath sounds usually absent when bronchial plug?
- tactile fremitus usually absent
- no adventitious sounds (unless bronchi patent, then might hear a few crackles)
lobar pneumonia
infection of one or more lobes of the lung causing alveoli to fill with fluid, bacteria, blood, pus (consolidation)
◦ Health history: fever, cough w/ chest pain, blood-tinged sputum, chills, SOB, fatigue
signs:
- increased RR (24 bpm) and HR (> 100 bpm)
- guarding and lag upon expansion on affected side
- chest expansion decreased on affected side
- tactile fremitus increased if bronchus patent/decreased if bronchus obstructed
- percussion dull over pneumonia
- bronchial, late inspiratory crackles over involved area
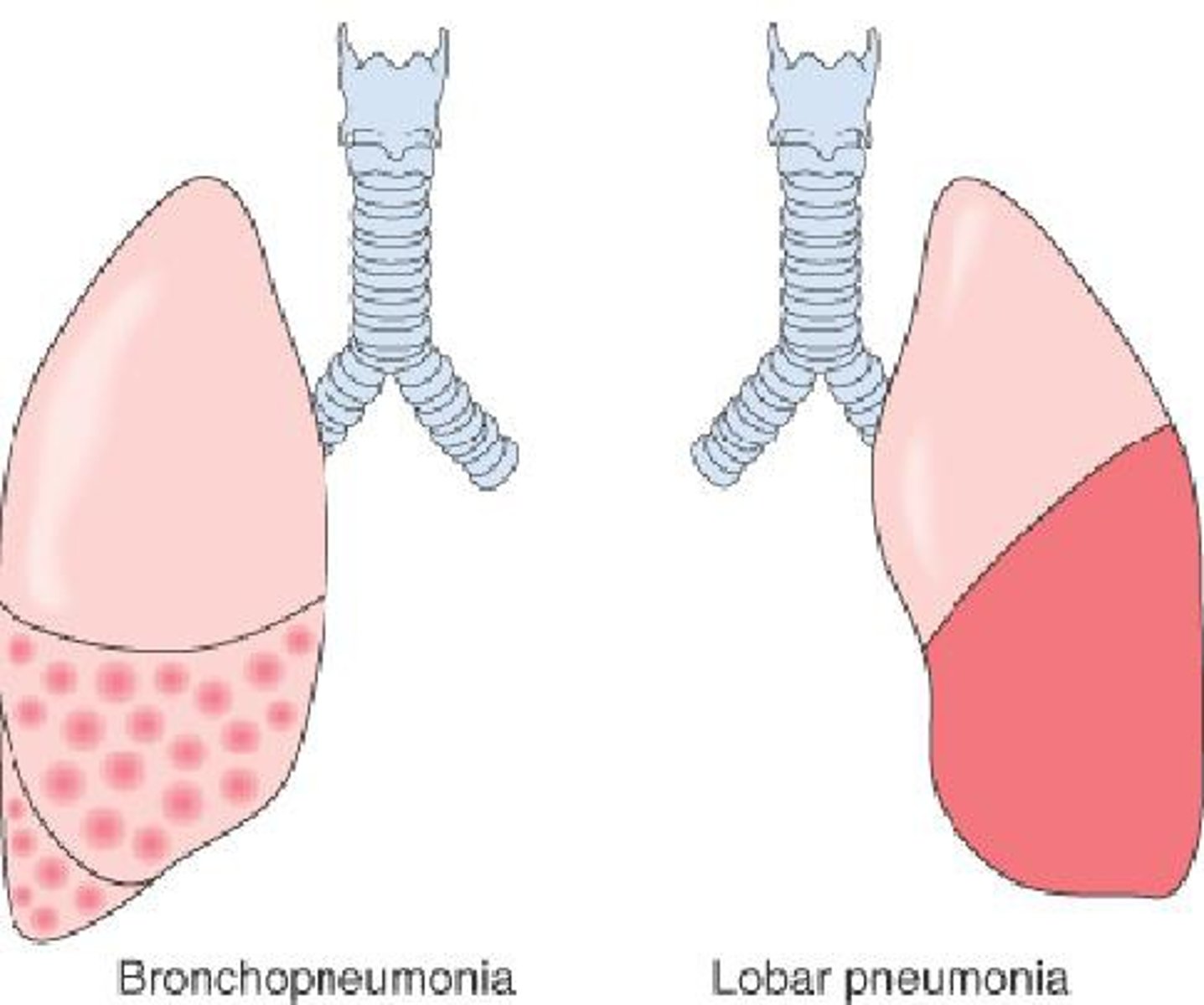
bronchitis
inflammation of the bronchi causing mucous build up
Signs
Trachea - midline
Tactile Fremitus - normal
Percussion – resonant
Breath sounds – vesicular except perhaps over large bronchi or trachea
Adventitious sounds – none OR coarse crackles in early inspiration and/or sonorous wheezes (rhonchi)
emphysema
Slowly progressive disorder (often due to smoking) in which the distal air
spaces enlarge and lungs become hyperinflatedOften also develops chronic bronchitis
Signs
tachypnea
tactile fremitus: decreased
percussion: hyper-resonant
breath sounds: decreased to absent
adventitious sounds: none or scattered coarse crackles in early inspiration
and perhaps expiration and/or sonorous wheezes (rhonchi) associated with chronic bronchitis
asthma
Widespread, usually reversible narrowing of the tracheobronchial tree
(bronchospasm and underlying inflammation), diminishing airflow
signs:
- SOB
- chest tightness
- tachypnea
- accessory muscles used to aid expiration
- some cyanosis
- retraction of intercostal spaces
- tactile fremitus: decreased during attacks
- percussion: resonant to hyper-resonant
- breath sounds: often obscured by sibilant wheezes
- adventitious sounds: wheezing during attacks
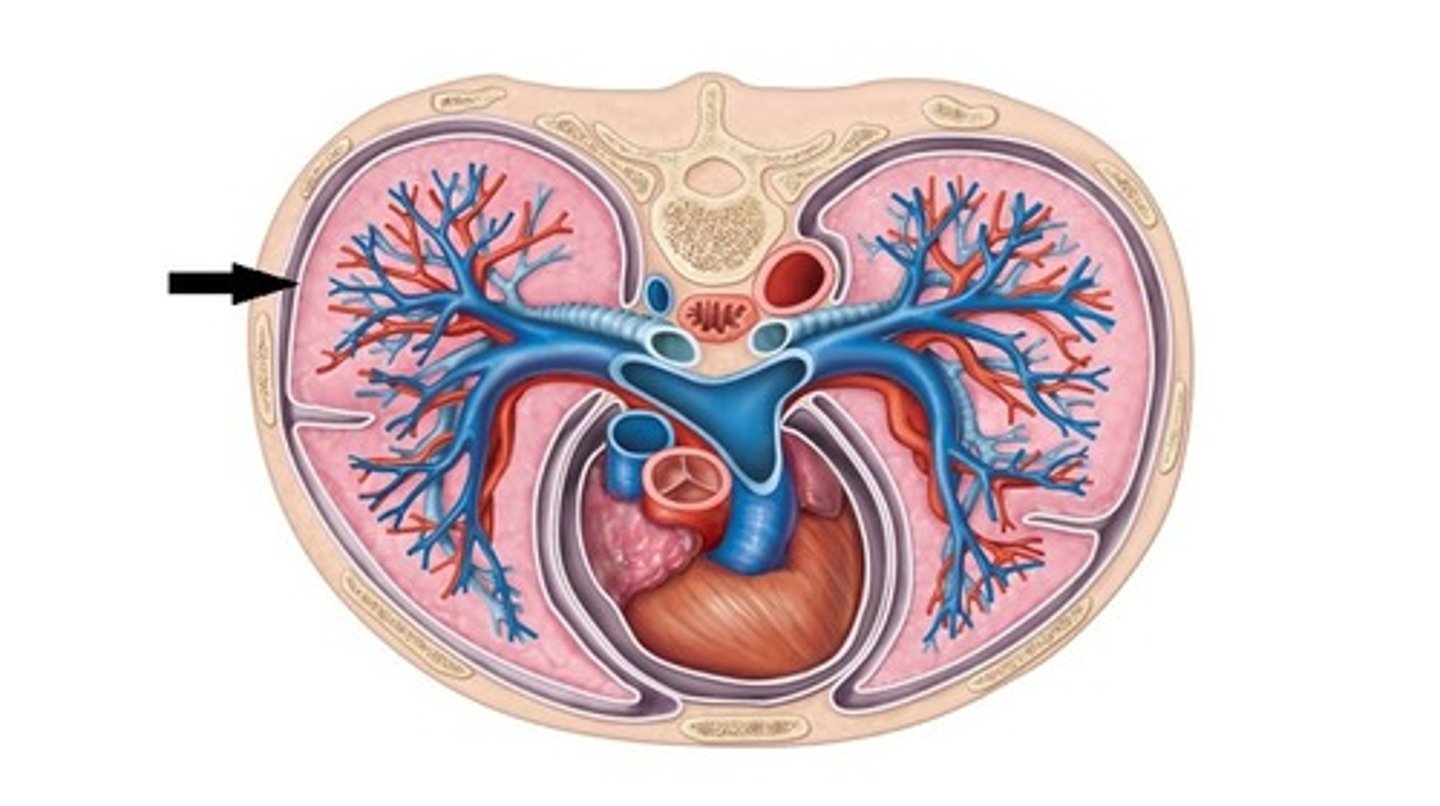
pleural effusion
Fluid accumulation in the pleural space, separating air-filled lung from
the chest wall, blocking the transmission of sound
*effusions may contain watery capillary fluid, protein, purulent matter, blood, lymphatic fluid
causes: HF (most common), infection, cancer
signs:
- tachypnea
- SOB
- tachycardia
- some cyanosis
- asymmetric expansion of lungs
- trachea shifted toward opposite side in large effusion
- tactile fremitus: decreased to absent
- percussion: dull to flat over fluid
- breath sounds: decreased to absent, but bronchial sounds may be heard near top of large effusion
- adventitious sounds: possible rub
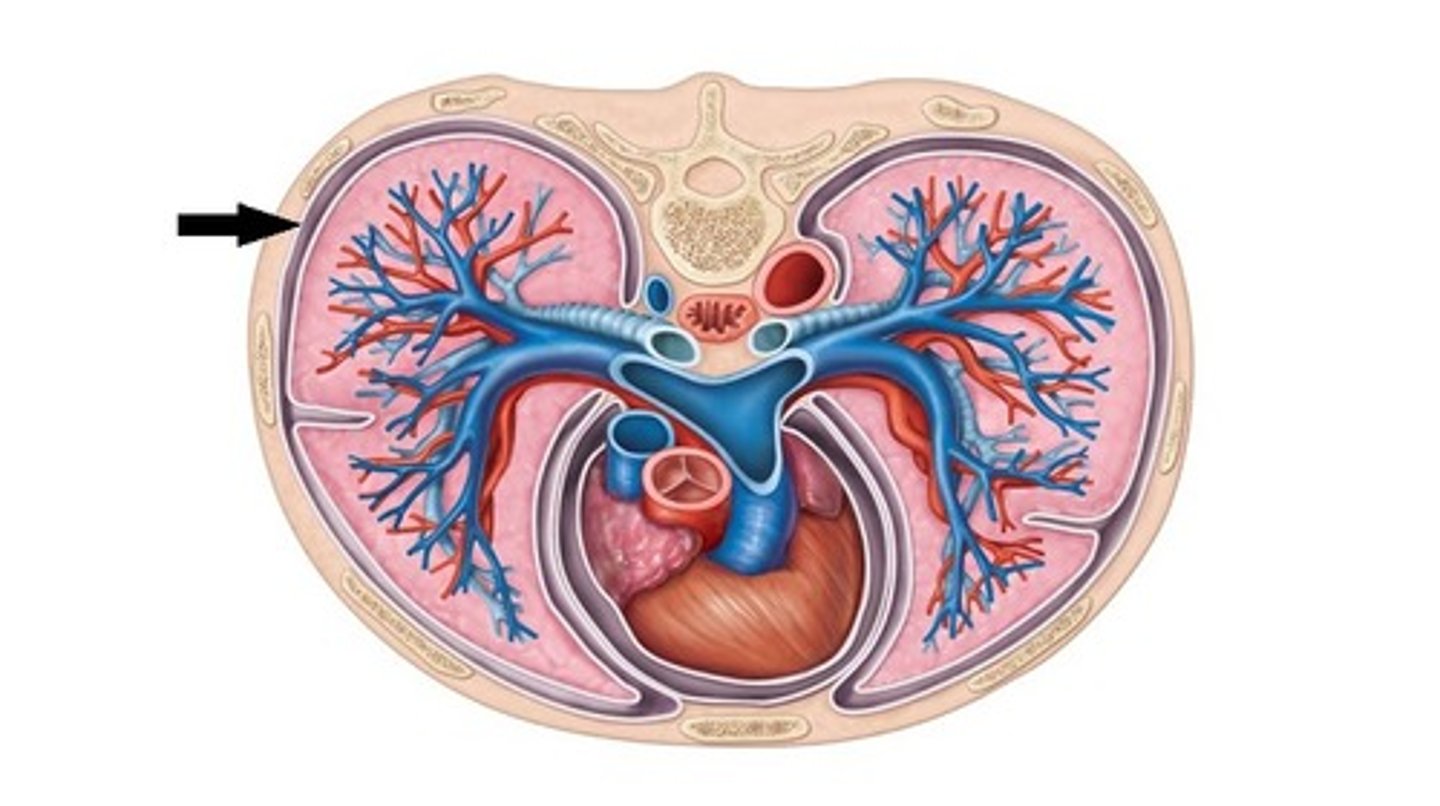
pneumothorax
Air leak into the pleural space, usually unilaterally, causing the lung to recoil
from the chest wallPleural air blocks the transmission of sound
*usually unilateral
*can be spontaneous, traumatic, tension
Signs
unequal chest expansion
trachea shifted toward opposite side if much air
tactile fremitus: decreased to absent over pleural air
percussion: hyper-resonant to tympanic over pleural air
breath sounds: decreased to absent over pleural air
adventitious sounds: possible pleural rub
congestive heart failure (CHF)
aka pulmonary edema
Increased pressure in pulmonary veins due to fluid overload, causing
congestion and interstitial edema around the alveoliBronchial mucosa
may also be edematous
signs:
- tachypnea
- SOB upon exertion
- orthopnea
- paroxysmal nocturnal dyspnea
- nocturia
- ankle edema
- pallor in light-skinned patients
- tactile fremitus: normal decreased
- adventitious sounds: late inspiratory crackles in the dependent portions of lunges, possible wheezes
lung parenchyma
portion of the lung involved in gas transfer: the alveoli, alveolar ducts and respiratory bronchioles
Hyperventilation
more tidal volume and more breathing
**ex. Kussmaul breathing
Type I diabetes bc their increase in glucose --> trying to blow off acid
Ex. of hyperventilation
Kussmaul breathing
Type I diabetes bc their increase in glucose --> trying to blow off acid
What kind of breathing is common in a dying patient?
Cheyne-stokes
Consolidation
when the air that usually fills the small airway in your lungs is replaced with pus, blood, water, or a solid
Flat percussion sound
very soft, high pitched, shorter duration
heard over very dense tissue
Ex. bone or muscle
Dull percussion sound
soft, muffled, moderate to high pitched, short duration
Resonance percussion sound
moderate to loud, low pitched, moderate duration
heard over healthy lung tissue
Hyperresonance
loud booming, very low pitched, long duration
hyper-inflated lungs as with COPD
Tympanic
loud, drum like, musical sound
heard over air/fluid filled cavities
ex. stomach, bowel, bladder, lung w/ large pneumothorax
Vesicular lung sounds
soft/low pitched breezy sound
normal over peripheral lung fields
length of inspiration > expiration
Bronchovesicular lung sounds
medium pitched, moderately loud
normal over mainstem bronchi
length of inspiration = expiration
Bronchial (tracheal) lung sounds
loud, coarse, blowing sound
normal over trachea
length of inspiration < or = expiration
Are breath sounds louder or quieter over areas of consolidation in the lung?
Louder bc sounds travels more easily through liquid or solid compared to air
Are breath sounds louder or quieter over areas where pus, abnormal fluid, or air is inside the pleural space?
quieter bc there is a physical barrier preventing the sound from making it to the stethescope
What do you asses if abnormal bronchovesicular or bronchial breath sounds are heard?
asses the transmitted voice sounds - bronchophony, egophony, whispered pectoriloquy
Where is the right middle lobe best auscultated?
Anterior chest
Summary of healthy lung findings
Trachea - midline
Tactile Fremitus – normal/symmetrical
Percussion –resonant
Breath sounds – vesicular except over large bronchi or trachea
Adventitious sounds -none
tracheobronchial tree and alveoli are clear; pleurae are thin and close together; mobility of chest wall is unimpaired
causes of atelectasis
mucous plug, foreign body, or surrounding pressure
pulmonary embolism
Blockage in the arteries bringing blood to the lung tissue
(usually a clot), which leads to lung tissue damageCould be air or fat embolism too
Signs
Trachea - midline
Tactile Fremitus – normal
Percussion – resonant
Breath sounds – vesicular
Adventitious sounds – usually none, may
have few crackles (rales)Symptoms
Low O2 levels
Dyspnea
Possible cyanosis
Sharp chest pain with inspiration
PMH
Known deep vein thrombosis that breaks off and travels to lungs
Sedentary