Mycology Introduction, Systemic Fungal Infections, And Opportunistic Fungal Infections
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
39 Terms
General Fungal Characteristics
Eukaryotic
nucleus, nuclear membrane, mitochondria
Sterols in the cell wall
lipids, play role in membrane integrity
Chemoheterotrophs
require organic nutrition
aerobes, grow best at neutral pH
Saprophytic: living on dead or decaying organisms
acquire food by absorption
produce sexual and asexual spores (conidia)
most produce asexually
Most fungi exist as:
Molds: multicellular, filamentous form of fungi consisting of thread-like filaments to form fuzzy colonies
Yeasts: unicellular, produce circular, restricted, pasty, or mucoid colonies
Fungi can also be:
dimorphic: exhibit a yeast or mold phase dependent on temperature
if ingested, would be a yeast due to higher body temps
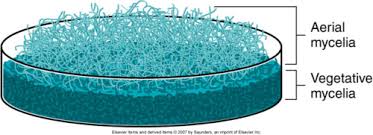
Filamentous Fungi (mold)
composed of microscopic filaments called hyphae that branch to form a network called the mycelium (colony)
extend over or through whatever substrate the fungus is using as a food source
Aeriel: hold reproductive structures (spores, seeds)
Vegetative: absorb nutrients
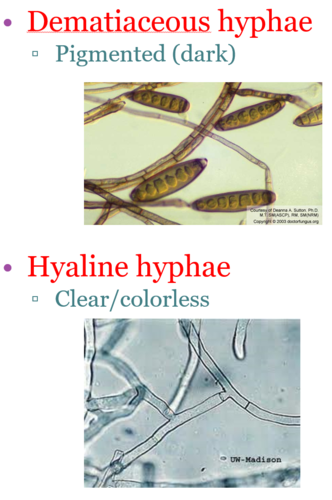
Hyphae
Shape: antler, racquet, spiral, rhizoid
Septate: perpendicular cross-walls
can be sparse or common
pigmentation
Hyaline (non pigmented hyphae)
Dematiaceous (dark pigmented due to presence of melanin in cell wall)
Fungal Spores (conidia)
Functions:
means of dispersal
means of survival (low metabolic state of activity)
Dormant state; will germinate when environment conditions are favorable again for growth
vary in size, shape, and color
unicellular or multicellular
Unicellular Yeast
Capable of reproducing asexually and sexually
Asexual: budding or binary fission (most bud)
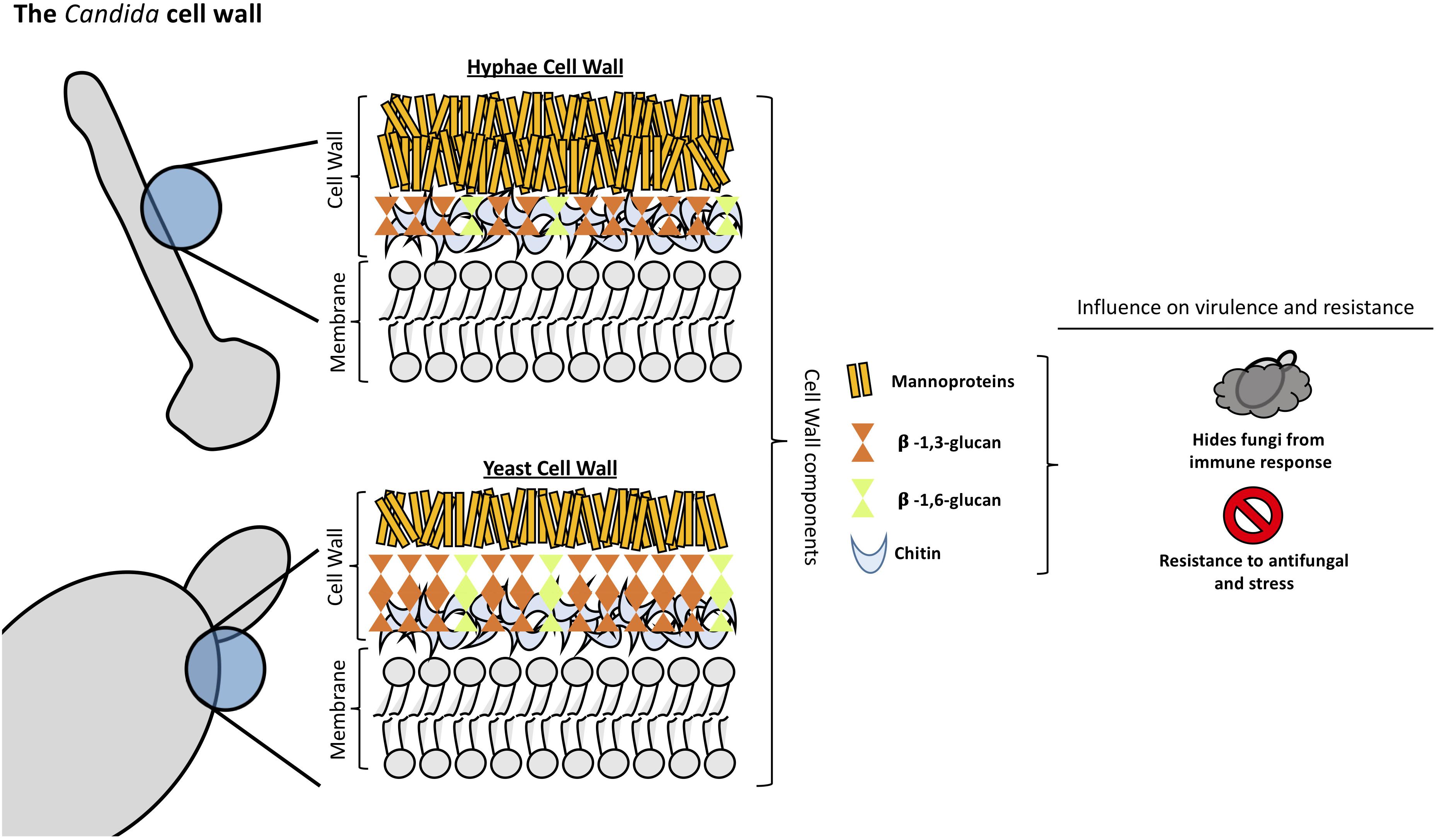
Candida Cell Wall
mannoproteins for cell stability
Chitin and Glucan (polysaccharides) for structural integrity
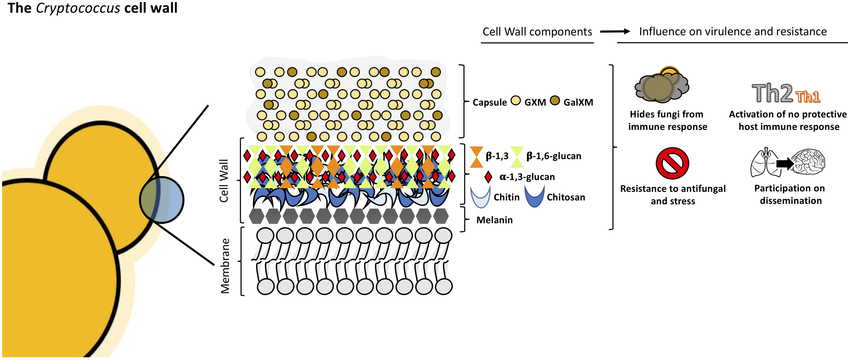
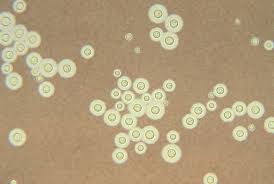
Cryptococcus Cell Wall (yeast)
Capsule (polysaccharide)
separates yeast species
masks antigens
virulence factor (protection against and interfere with host immune cells)
Chitin and Glucan (polysaccharides) for structural integrity
Melanin: virulence factor
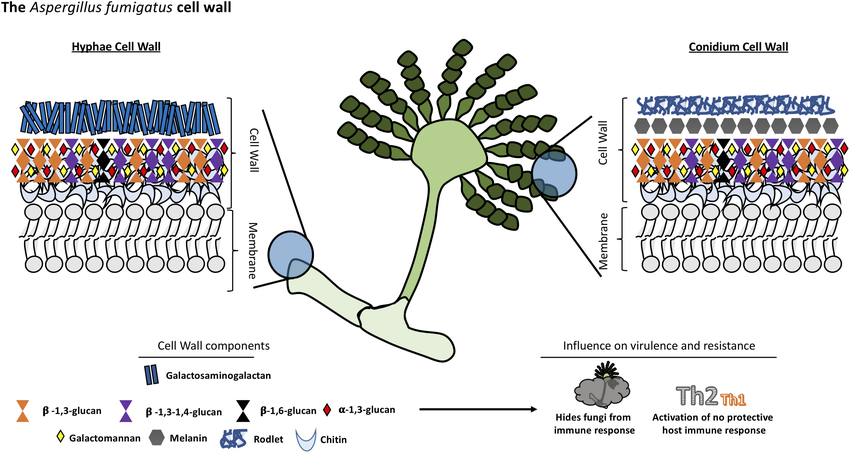
Aspergillus Cell Wall (mold)
Galactomannan (polysaccharide): released during tissue invasion
can be tested for in a clinical setting for diagnosis
Chitin and Glucan (polysaccharides) for structural integrity
Rodlet (protein) virulence factor
Fungal Diseases
Grouping is traditionally based on botanic taxonomy (classification)
Clinical microbiology groupings based on mycoses (fungal diseases)
Superficial: confined to the outermost dead layer of the skin or hair
Cutaneous: affects the keratinized layer of the skin, hair, or nails
Subcutaneous: deeper skin layers including muscle, bone and connective tissue without dissemination to distant sites
Systemic: affects the internal organs or deep tissues of the body
Opportunistic: found primarily in immunocompromised persons; infections of a great variety of tissues
pose a significant diagnostic challenge due to complexity due to complexity of the patient population at risk and increasing array of fungi that can infect immunocompromised individuals
Innate Resistance
despite constant exposure to the infectious forms of various fungi (between 1000 to 10 BILLION spores daily from vast number of species)
The key factor that provides barrier is out internal temp — fungi unable to adapt to higher temps
A healthy immunocompetent individual will have high innate resistance to fungal infections
Mode of Transmission
Dependent on type of mycoses (infections)
Superficial & Cutaneous: person-to-person contact, person-to-animal contact, as well as fomites (objects/materials that carry infectious agents)
Subcutaneous: through the skin, after a cut or other trauma to the skin
Deep mycoses: opportunistic growth in immunocompromised; inhalation of spores/conidia; or presence of intravenous device
most common mode
Lab Values to Support Fungal Infection
increased WBC count
increased lymphocytes and monocytes
mod-marked increase in total protein
normal-to-low glucose
lactate > 25mg/dl
Specimen Collection, Transport, Handling, And Growing
Based on information from clinical examination and radiographic studies and consideration of the most likely fungal pathogens that may cause a specific type of infection
Collected aseptically or after proper cleaning/decontamination of the site sampled
adequate amount of clinical material is collected in a sterile, leak proof container accompanied by a relevant clinical history, to be tested immediately or stored at 4oC
Specimens processed under a bio safety cabinet
Identification methods:
direct microscopy, culture, biochemicals and susceptibility testing
automated identification systems
immunologic methods
molecular methods
Culture Time and Conditions
Time: growth of yeast is usually detected within 48-72 hours, mold could take up to 4-6 weeks
Temp: fungal cultures grown at 25-30oC, while dimorphic fungi are grown at mold temps and yeast temps for conversion to yeast phase which could take 7-14 days
Culture Media
Enriched media to ensure growth of fastidious thermally dimorphic fungi (blood enrichment)
General purpose media to ensure growth of a varieties of molds and yeasts
contain no antimicrobial agents
contain an antibacterial
contain an antibacterial and antifungal (cycloheximide)
cycloheximide inhibits Cryptococcus neoformans, Mucorales, Candida spp., Aspergillus spp., Histoplasma spp.
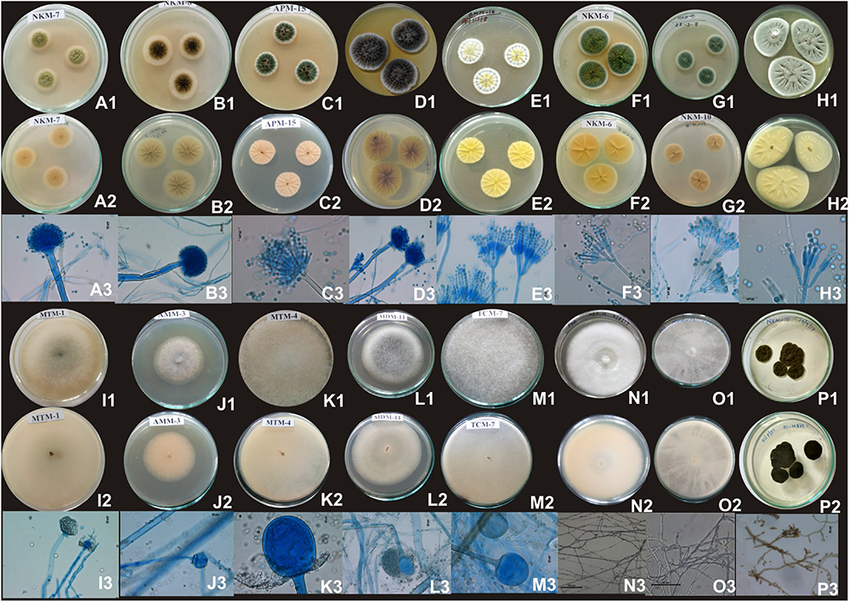
Colony Morphology
Texture: height of aerial hyphae
wooly/cottony (dense, high)
velvety (low aerial hyphae)
granular (flat, dense aerial hyphae)
Color: surface and reverse
Topography: designs of hills and valleys

Microscopy
Stains & Reagents
Lactophenol cotton blue:
kills any organism and lactic acid acts as a clearing agent and preserves fungal structures
stains the chitin in fungal cell walls
Potassium Hydroxide
10-20% solution of KOH dissolves keratin
contrast black / white staining gives outline of organism
Calcofluor White
fluorochrome stain that binds to cellulose and chitin in fungal cell walls
appears fluorescent green
Gram Stain
fungi stain gram positive (purple)
Identification of fungi by observance of asexual structures (sporangiospores or conidia)

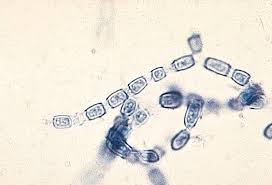
Microscopy Conidia
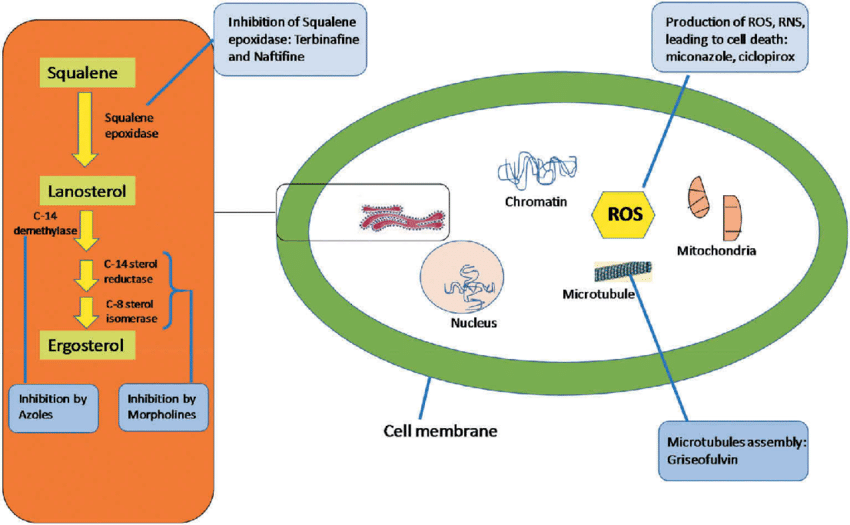
Antifungal Agents
Agents can have broad or narrow spectrum
Fungistatic (inhibits and slows growth) or Fungicidal (kill organism)
Systemically active and topical Agents
Polyenes
systemically active agent
Amphotericin B and Nystatin
Work by binding to ergosterol, the principal membrane sterol of fungi. Binding produces ion channels, which destroy the osmotic integrity of the fungal cell membrane and lead to leakage —> eventually death
also bind to cholesterol, main membrane sterol of mammal cells (makes polyenes toxic)
nephrotoxicity (kidney damage)
Broad spectrum of activity
dimorphic fungi
opportunistic fungi
Candida spp.
Cryptococcus neoformans
Fungicidal
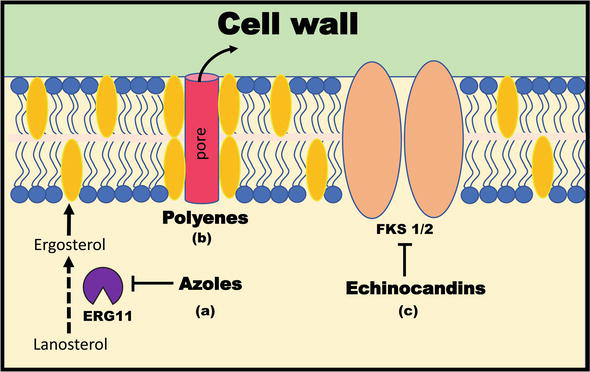
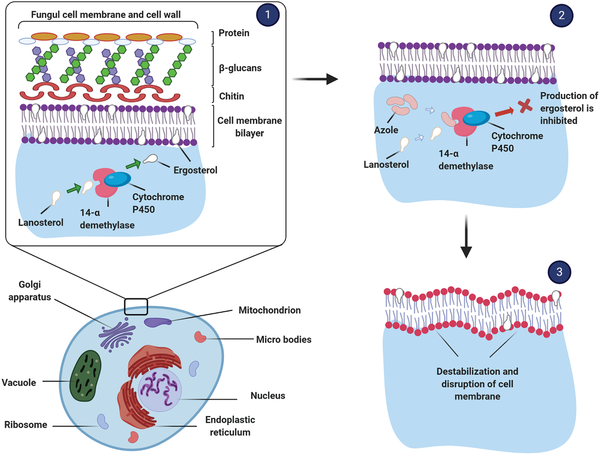
Azoles
Systemically active agent
Inhibit fungal Cytochrome P-450-dependent enzyme, lanosterol 14-alpha-demethylase
enzyme is involved in the conversion of lanosterol to ergosterol
inhibition disrupts cell membrane synthesis
fungistatic in yeast and fungicidal in mold
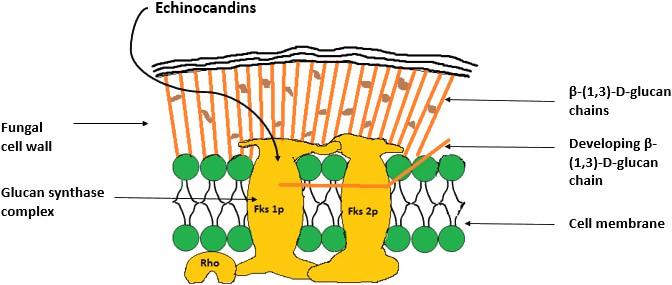
Echinocandins
systemically active agent
Inhibit synthesis of 1,3 beta-glucans, constituents of fungal cell wall
Fungicidal in Candida and fungistatic in Aspergillus
low toxicity - we don’t have cell walls
Ex. Caspofungin
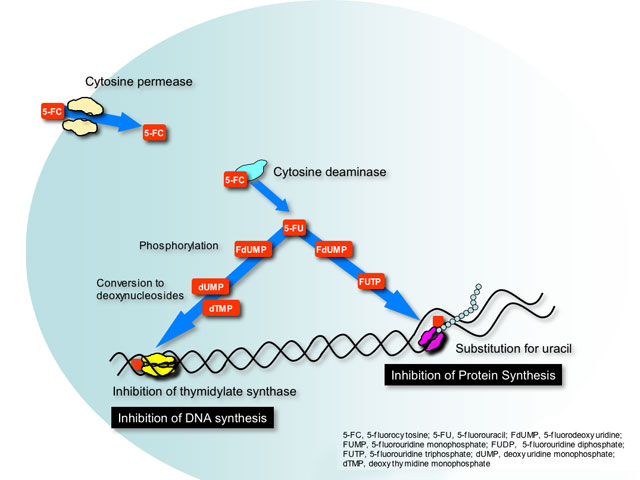
Flucytosine
systemically active
interferes with the synthesis of DNA, RNA and proteins of the fungal cell wall
Enters the cell wall via cytosine permease; converted by cytosine deaminase in fungal cells to fluorouracil — which competes with uracil and results in RNA miscoding
fluorouracil is metabolized to 5-fluorodeoxyuridylic acid which halts DNA synthesis
Fungistatic
limited spectrum of activity
typically used in combination with another antifungal agent due to resistance
Allylamines
Systemically active
Ex. Terbinafine
Inhibit the enzyme squalene epoxidase which results in a decrease in ergosterol and an increase in squalene, producing a toxic effect within the cell membrane
broad spectrum of activity (dermatophytes, yeasts, molds)
Fungicidal
Topical Active Agents
Available in most classes of antifungal agents
creams, lotions ointments, powders, and spays
treatment of superficial, cutaneous, and mucosal infections
Use of topical vs systemic therapy is dependant on status of host as well as type and extent of infection
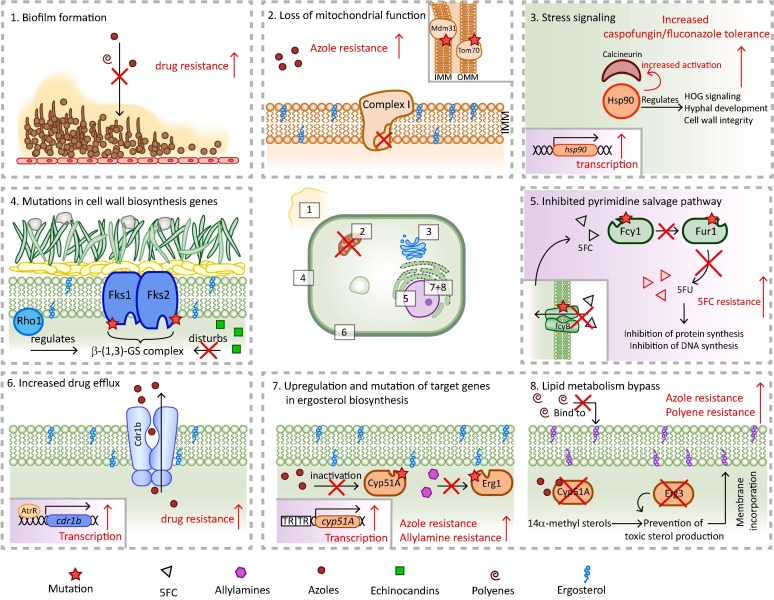
Antifungal Resistance
Resistance develops slowly and involves the emergence of intrinsically resistant species or a gradual, stepwise alteration of cellular structures or functions
Mechanisms
biofilm formations — reduced penetration of antifungals
Efflux pumps — reduces accumulation of drug
Target alterations/mutations
overexpression of target
Pathogenesis of Fungal Disease
few fungi are virulent enough to be considered primary systemic pathogens or capable of initiating infection in an immunocompetent person
Most are considered opportunistic pathogens, only causing infections when there are disruptions to protective barriers (skin) or when there is defects in the immune system
Primary Systemic Pathogens
agents of respiratory infection
have a saprobic phase (found on soil or decaying vegetation) thats forms airborne cells
And a parasitic phase (adapted to growth at 37oC and reporduces in host
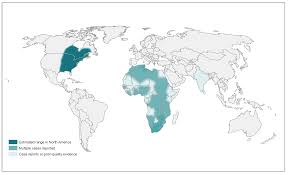
Blastomyces dermatitidis
geographic distribution: North America (OH and MS river valleys) Africa, and SW Asia
Ecologic niche: soil, woody plants and decaying matter
250 cases/yr
Dog infection rate is 10x that of humans
Route of infection: inhalation of conidia, inoculation od soil, dog bite
Clinical Syndromes: severity is dpendent on extent of exposure and immune status
Symptoms occur in fewer than half of infected individuals
incubation 1 to 15 weeks
Illness: pulmonary disease or extrapulmonary disseminated disease (heart)
pulmonary blastomycosis is asymptomatic or presents as mild-flu like illness
~50% are asymptomatic
classic form of blastomycosis: chromic cutaneous mycosis
Pathogenicity:
following inhalation, conidia (2-10um) convert to yeast (8-30um)
larger yeast resist immune attack
localized yeast invasion of host invokes an inflammatory response
yeast escape recognition by macrophages (shed antigen from cell surface and modify cell wall)
Diagnosis
microscop detection in tissue
broad-base budding yeast
serologic assays not useful
antigen test
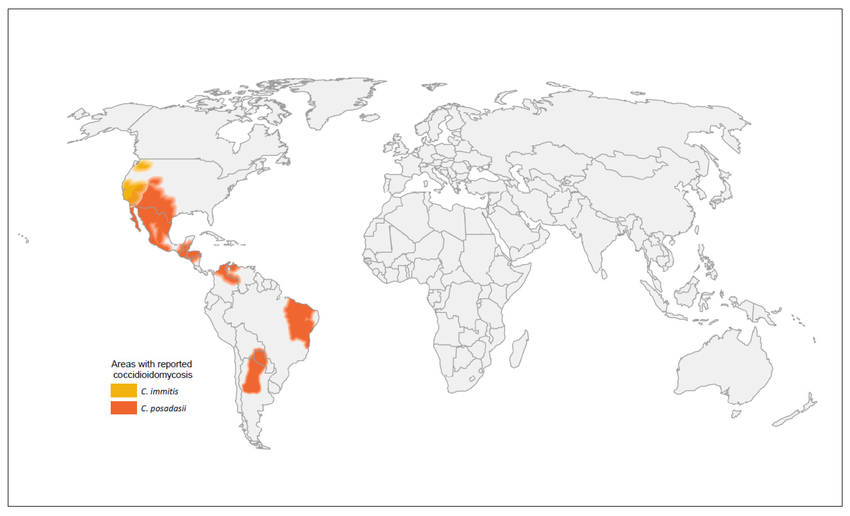
Coccidioides immitis / posadasii
Geographic distribution: Southwestern US, Mexico, Central & South Americas
C. immitis is localized to California
C. posadasii accounts for majority of infections outside of CA
Ecological niche: soil, dust, bat and bird droppings — nitrogenous (alkaline)
Cycles of heavy rain allows growth, drought and wind allows dispersal
Route of infection: inhalation of arthroconidia
only a few can produce primary coccidiomycosis
Clinical syndromes: can be either pulmonary or extrapulmonary
asymptomatic in 30-60% of patients
incubate for 1-3 weeks
last for a few weeks to months
Symptoms:
fever, cough, headache, muscle aches and joint pain
valley fever
cutaneous manifestations (rash)
chronic pneumonia
meningitis
bone and joint infection
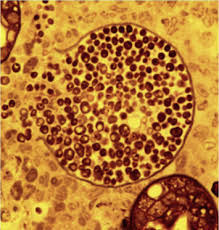
diagnosis:
microscopic detection of the fungus in tissue or other clinical material with confirmation by culture
spherules containing endospores in tissue
serologic testing (IgM and IgG)
antigen test

Histoplasma capsulatum
Distribution: North America (OH and MS river valleys, Mexico) Central & South America, Africa, Asia, Australia
Ecological niche: soil with high nitrogen, bat and bird droppings
~90% infected are male
Route of Infection: inhalation of microconidia
Clinical syndromes:
severity depends on extent of exposure and immune status
Symptoms: like pneumonia occur in ~10% of infected individuals
incubation: 4-18 days
in the event of heavy inoculum, pulmonary histoplasmosis occurs
1 in 2000 adults
reactivation common among immunocompromised
an estimated 60-90% of people living around Ohio and Miss. River valleys have been exposed
incidence higher in ages 65+
Diagnosis:
microscopic detection in tissue
small, oval narrow budding yeast
serologic testing in blood or urine
antigen test

Talaromyces marneffei
Distribution: southcentral, southeast and east Asia
Ecologic niche: soil and has been isolated from bamboo rats
Route of infection:
inhalation of conidia
traumatic implantation
eating bamboo rat
Clinical syndromes:
disseminated skin infections (skin, soft tissue)
occurs primarily in immunocompromised people in Thailand and SE China (early indicator of HIV)
resembles histoplasmosis, cryptococcosis and tuberculosis
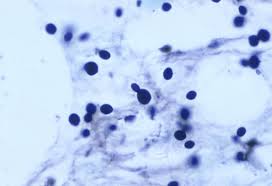
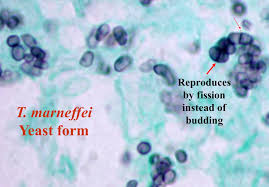
Diagnosis:
microscopic detection in tissue
morphology: elliptical fission yeast that are intracellular
no serological testing but under development
molecular assay
Systemic Fungi treatment options
clinical form, severity, and immune status, antifungal toxicity must be taken into consideration
treatment duration may range from 3 months to year(s) AIDS patients require lifelong treatment
Oppritunistic Mycoses
Pose significant diagnostic challenge:
complexity of the patient population (immunocompromised) and increasing array of fungi that can infect these individuals
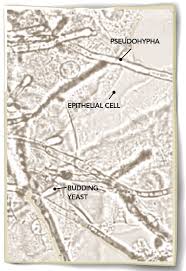
Candidiasis (yeast)
more than 100 species, only ~20 have have been implicated in clinical infections
C. albicans accounts for 90-100% of mucosal isolates and 50-70% of bloodstream infections
C. glabrata
C. parapsilosis
C. tropicalis
Emerging pathogen: C. auris
causes invasive infection
Japan, 2009
Often resistant to multiple antifungals
challenging to identify
health-care associated transmission
Epidemiology:
known colonizers of humans an warm-blooded animals
Primary site: GI tract from rectum to mouth
commensals in the vagina and urethra, on the skin, under nails
most represent endogenous infections
exogenous infections- can transmit person to person
Clinical syndromes: cause infection of virtually every organ system
range from superficial mucosal and cutaneous to widespread hematogenous dissemination involving target options
liver, kidney, heart, brain and spleen
Candidiasis
diagnosis: collection of tissue or fluid followed by direct microscopy
Treatment, prevention, and control:
generally treated with single antifungal agent
remove source of infection and enhance immune system
remove catheters, drain absesses

Cryptococcus neoformans
distributed worldwide
ecological niche: soil contaminated with bird droppings
Route of infection: inhaling aerosol cells
clinical syndromes:
can cause latent or systematic disease (basec on virulence and immune status)
can cause disease in healthy individual, more frequent and severe in immunocompromised
incubation of 6-8 weeks
presents as either pneumonia or a central nervous system infection secondary to hematogenous and lymphatic spread
meningitis in 40-80% of cases
clinical syndrome: disseminated disease includes skin lesions and ocular infections
diagnosis:
microscopy detection of yeast and examination of CSF might reveal characteristic encapsulated budding yeast
direct detection of capsular polysaccharide antigen
treatment:
cryptococcal meningitis and other disseminated forms are fatal if left untreated
severe infection: amphotericin B + flucytosine for 2 weeks followed by 8 weeks of fluconazole
mild to moderate: fluconazole
AIDS patients require lifelong treatment
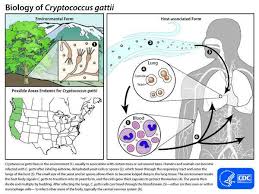
Cryptococcus gattii
located in pacific northwest and moved down to southeast US
important to be distinguished from C. neoformans infections bc C. gatti requires lengthier treatments and more aggressive
typically infections patients without HIV
most infections stay pulmonary
ecological niche: woody materials
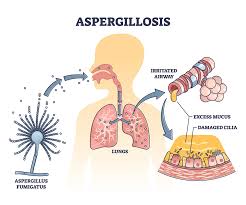
Aspergillosis
distributed worldwide
ubiquitous in air, soil, decaying matter
A. fumigatus
A. flavus
common in hospital environments
at-risk populations: “patients with”
prolonged neutropenia
immunodeficient or immunocompromised
corticosteroids
Aspergillosis
route of infection: inhalation of conidia
incubation of 3 days —> 3 weeks
allergic bronchopulmonary aspergillosis (ABPA): manifestations based on hypersensitivity to antigens, causes wheezing and coughing
sinusitis
invasive aspergillosis: 70% mortality! seen in neutropenic and immunodeficient patients and cystic fibrosis patients
clinical syndromes:
produce aflatoxin when it A. flavus contaminates food
peanuts, dried fruits, corn, rice
symptoms: nausea, vomiting, abdominal pain, convulsions
chronic exposure associated with liver cancer
safe levels regulated by FDA
Diagnosis:
aspergillus galactomannan antigen in serum
isolation from blood is rare
specimen source: bronchoalveolar valve
Treatment:
prevention in high risk patients
reconstitute host defenses
surgical removal
antifungal therapy — amphotericin B
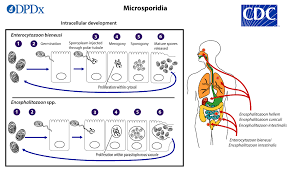
Microsporidia
spore forming
15 species are pathogens to humans
distrubuted worldwide and have a wide host range
7-50% of aids patients infected
transmitted by inhalation of spores
unknown incubation period
Clinical syndromes:
double infections with Cryptosporidium are common
symptoms: profuse, watery diarrhea
dissemination to involve loss of vision, neurologic disturbances, hepatitis, UTI, pulmonary infections
clinical manifestations are very diverse, varying to causal species
Diagnosis:
detection of organisms in biopsy and examination of cerebrospinal fluid and urine
molecular methods
treatment and prevention:
restoration of immune system
improved sanitation
Mucormycosis
distributed worldwide
common bread mold, also found in soil and decaying vegetation
common pathogens:
Rhizopus
Mucor
Lichtheimia
clinical syndromes:
1.7 million annual US infections
infections with mortality ranging from 70-100%
infections acquired by inhalation, ingestions, or contamination of wound from sporangiospores
clinical syndromes
gastrointestinal mucormycosis
more common in young children
disseminated mucormycosis
fungus spreads into bloodstream to affect various parts of body
affects the brain and heart
diagnosis:
tissue for direct microscopy and culture
specimens from nasal scrapings, sinus aspirates, biopsy material
serology not useful
negative culture results common even when hyphae are seen in tissue
Treatment:
amphotericin B often supplemented with surgical debridement
duration of treatment is individualized
Hyalohyphomycosis
100 known organisms
infections caused by non pigmented mold
distributed worldwide
commonly encountered in lab environment as saprobes
many infections acquired during construction/demolition and hospital acquired
mostly seen in immunocompromised
Fusarium
causes mycotic keratitis
disseminated infection in immunocompromised
diagnosis
fungi can be recovered from patients having no evidence of infection
culture for identification
Treatment:
resistance to antifungals
immune reconstitution
surgical removal
Phaeohyphomycosis
100 known organisms
caused by pigmented mold
distributed worldwide
everywhere in nature
clinical syndromes:
disseminated infections or localized infections of the lung, paranasal sinuses and CNS
mostly seen in immunocompromised
diagnoses:
culture for identification
fungi can be recovered from patients having no evidence of infection
treatment:
amphotericin B
surgical removal
Pneumocystis
P. jiroveci causes illness almost exclusively in immunocompromised patients especially with HIV
prefer humans and animals
transmit by inhalation or person-person
clinical syndromes:
pneumonia
extrapulmonary manifestations
lymph nodes, spleen, bone marrow, liver, eyes, ears
diagnoses:
microscopic examination of clinical material
molecular assay
Treatment:
SXT for 3 weeks and prophylaxis
interferes w acid synthesis