Lecture 14: The Reproductive System II
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
46 Terms
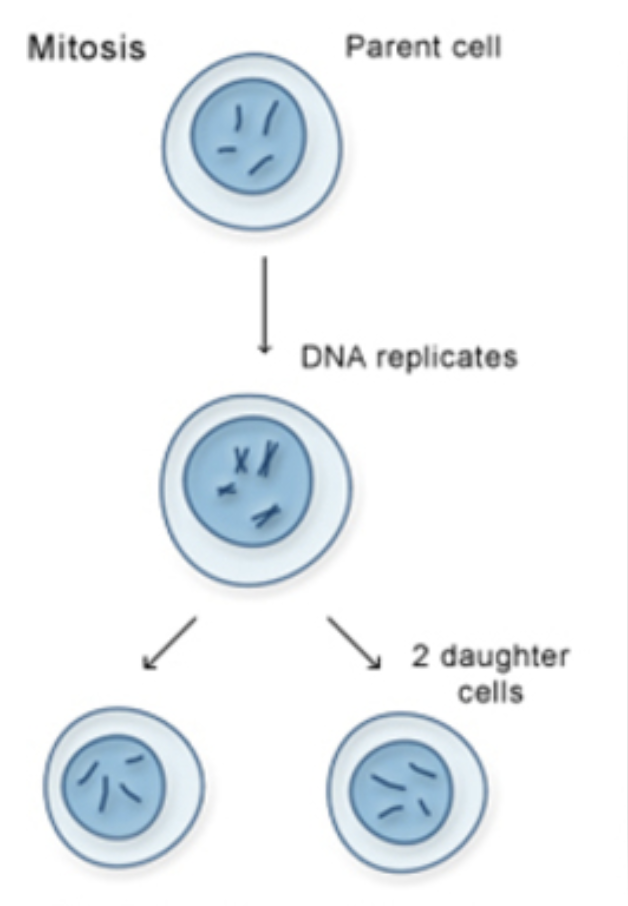
What is mitosis? What is meiosis?
Both are ways for cells to divide, but:
Mitosis = For growth, repair, and regular body cell renewal
Meiosis = For making gametes (sperm & egg cells only) for reproduction
Outline how mitosis works. Starts with one cell (46) ends with 2 daughter cells (46)
Parent cell: Starts with 2n = 46 chromosomes (diploid)
DNA replicates: So now there’s double the info
The number of chromosomes stays the same (46)
BUT each chromosome now has two sister chromatids (basically a "copied" arm)
So we went from 46 single chromosomes → 46 duplicated chromosomes
Cell splits into 2 identical daughter cells - They're exactly the same as the parent cell and each other
Each one still has 2n = 46 chromosomes
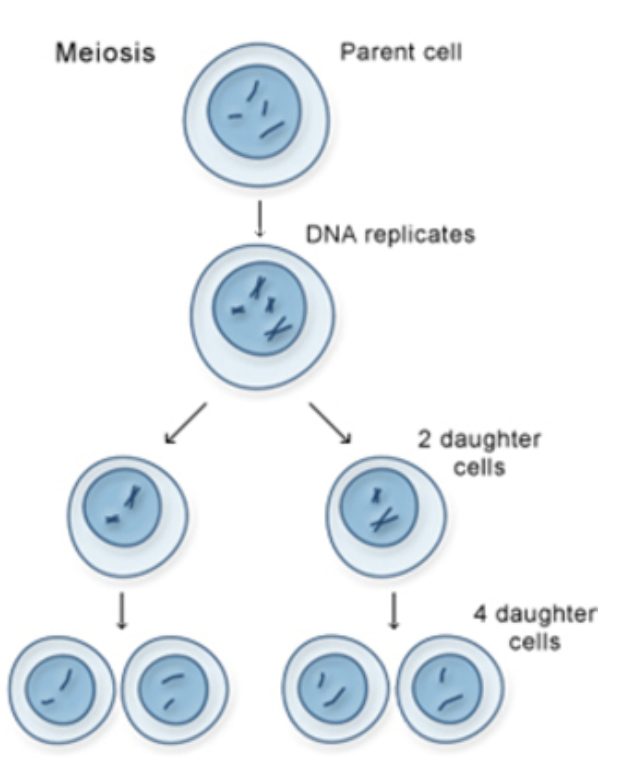
Outline how meiosis works. Starts with one cell (46) ends with 4 cells (23)
Parent cell: Starts as 2n = 46 chromosomes (diploid)
DNA replicates
The number of chromosomes stays the same (46)
BUT each chromosome now has two sister chromatids (basically a "copied" arm)
So we went from 46 single chromosomes → 46 duplicated chromosomes
🔄 Meiosis I: First division
Makes 2 cells with different combinations of DNA
Because during Meiosis I, chromosomes cross over and swap genes
🔁 Meiosis II: Second division
Each of those 2 cells splits again → total of 4 cells
Each cell is n = 23 chromosomes (haploid) - And each one is genetically unique
definition of n, 1n, and 2n?
what is spermatogenesis?
Spermatogenesis is the process of making sperm cells in the testes.
Where does spermatogenesis start?
The Testes
Inside each testicle are seminiferous tubules (tiny, coiled tubes).
what is the difference between the outer vs inner (closer to lumen) portions of the seminiferours tubules
The cells on the outside of the tube are baby/immature sperm cells.
The inside/lumen is where fully-formed sperm go once they're made.
What cells helps the sperm to develop?
Sertoli Cells
Nurse Cells
Located in the seminiferous tubules.
They help sperm develop, give nutrients, and protect them.
Think of them like babysitters or personal trainers for sperm
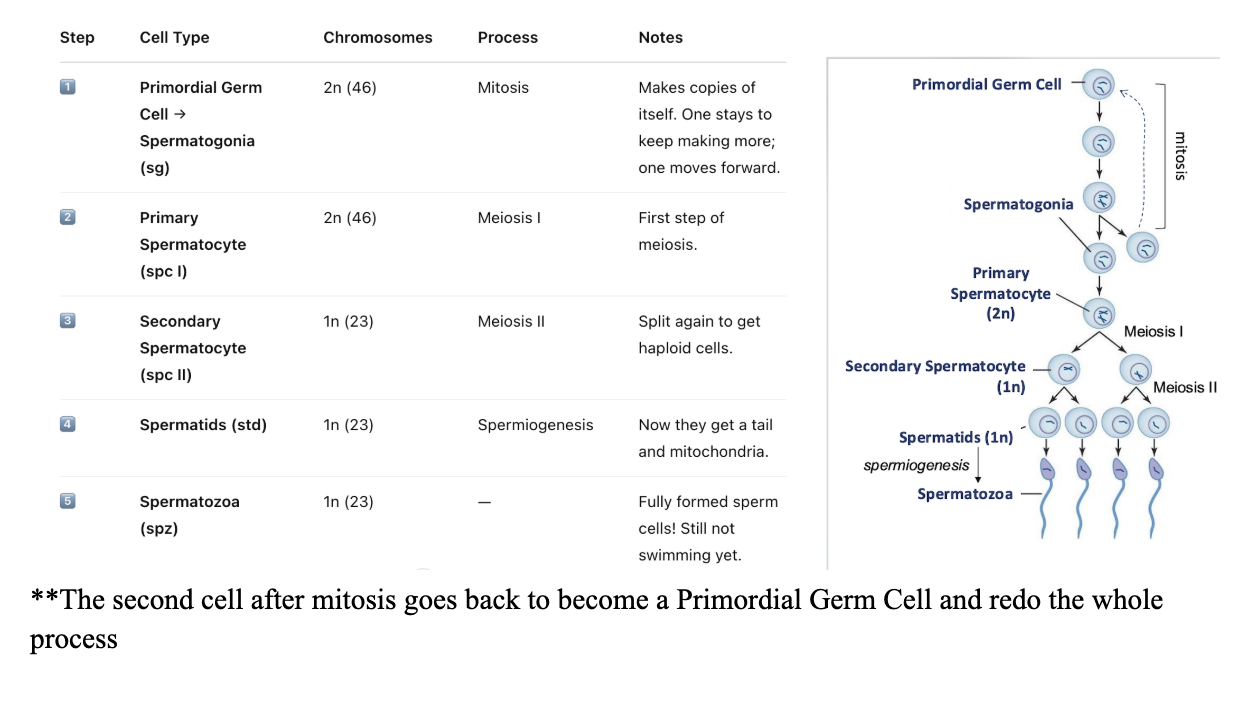
how does sperm go from Primordial germ to to spermatozoa using meiosis in the testes
How cells become sperm:
Through MITOSIS + MEIOSIS
Primordial Germ Cell to Spermatozoa
RECALL: Pathway of sperm
**prostatatic fluids give the ability to swim
What is semen?
Semen = sperm + secretions from glands
Cloudy white fluid consisting of sperm + secretions from accessory glands.
Provides nutrients, acts as a transport medium to protect sperm.
2-5mL per ejaculation containing 100s of millions of sperm!
What are the 3 important acessory glands that contribute to sperm/semen
SEMINAL VESICLE (aka the mother)
What it Adds
Alkaline fluid + sugars
Why it’s Important
Feeds sperm
Makes vaginal environment less acidic
Thins cervical mucus
Triggers reverse peristalsis (pulls sperm up female tract!)
PROSTATE GLAND (aka the father)
What it Adds
Citric acid + enzymes (via ejaculatory ducts + prostatic ducts)
Why it’s Important
Keeps semen liquid
Protects DNA
Turns on sperm’s swimming ability
BULBOURETHRAL GLAND
What it Adds
Pre-ejaculatory fluid
Why it’s Important
Cleans out urine (acidic!) from urethra before sperm passes through
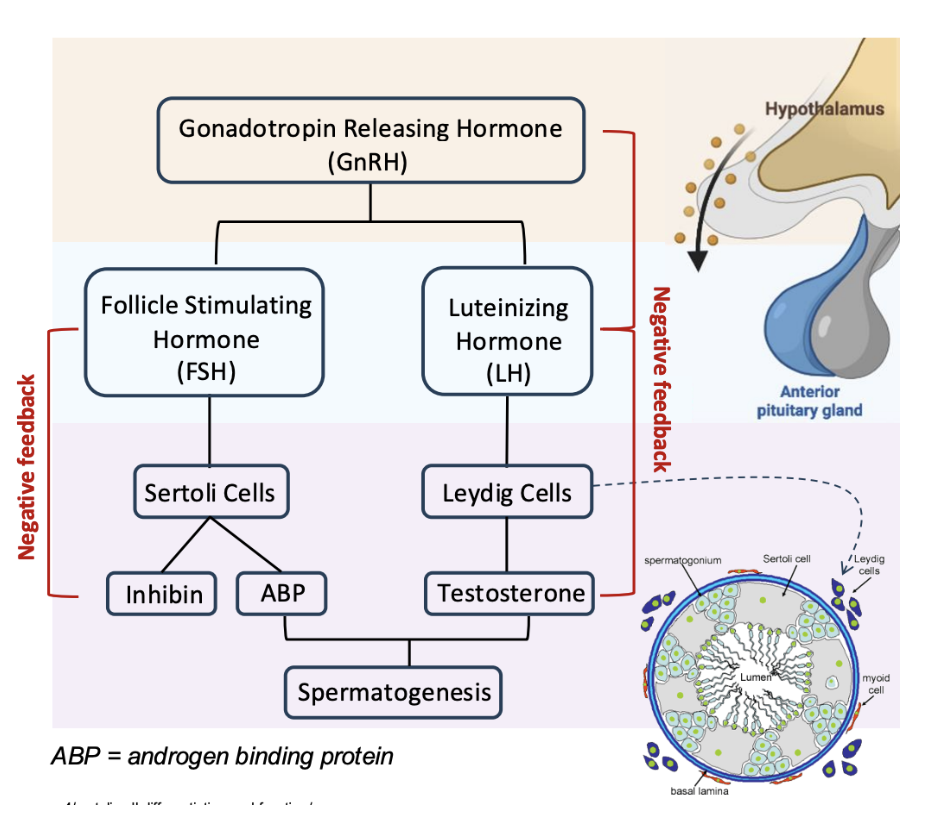
Where does Hormone control begin in Males? What does it release
Step 1: Start at the Brain – Hypothalamus
The hypothalamus is like the boss that sends out the first signal:
GnRH = Gonadotropin-Releasing Hormone
GnRH tells the anterior pituitary to get to work.
After GnRH is released, what is released as a result?
Step 2: Anterior Pituitary Releases Two Hormones
FSH = Follicle Stimulating Hormone
LH = Luteinizing Hormone
Both go to the testes, but they do different jobs.
What does LH do in the testes
**Step 3: What LH Does
LH goes to Leydig cells in the testes (outside the seminiferous tubules).
Leydig cells release testosterone
Testosterone does a lot:
Starts, maintains, and drives spermatogenesis (making sperm)
Grows facial/body hair, deepens voice, builds muscle
Keeps up libido (sex drive) and accessory glands like the prostate
Too much testosterone?
Negative Feedback to shut down GnRH and LH → less testosterone made
Think: GnRH ➡ LH ➡ Leydig (Testes) ➡ Testosterone
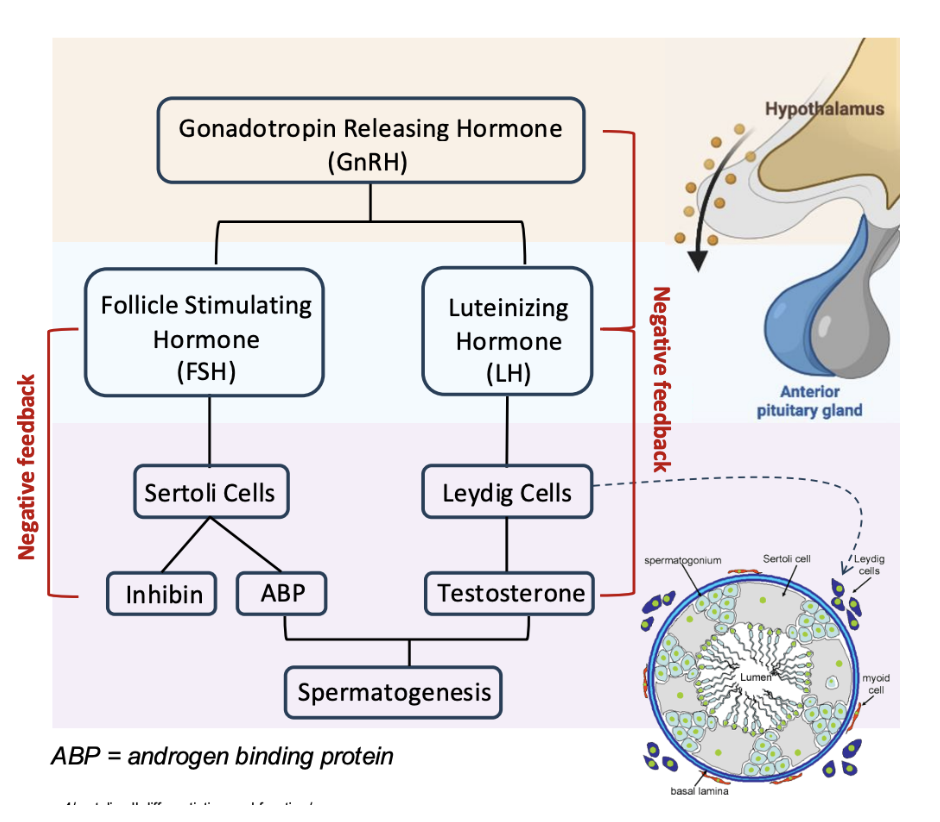
What doe FSH do in the testes?
**Step 4: What FSH Does
FSH goes to Sertoli cells in the testes (inside seminiferous tubules — the "nurse cells")
Sertoli cells release ABP = Androgen Binding Protein
ABP holds on to testosterone (released by the Leydig cell) and keeps it in place, so it can help sperm grow!
It binds to testosterone and helps keep testosterone levels high inside the seminiferous tubules
Because sperm cannot develop properly without high levels of testosterone in the tubules.
Too much sperm?
Sertoli cells release inhibin → shuts down FSH → less ABP → slows down sperm production
Think: GnRH ➡ FSH ➡ Sertoli (Testes) ➡ ABP
ABP ➕ Testosterone ➡ Spermatogenesis
What is 1 common disorder of the prostate? symptoms?
Benign Prostatic Hypertrophy (BPH)
Common with age — affects 70% of men over 70
Even more likely if it runs in your family
The prostate gets bigger and squishes the urethra — the pee tube inside it
Symptoms:
Weak pee stream
Gotta pee urgently or often
Trouble fully emptying bladder
Sometimes pain or leaking
This is not cancer, just annoying and affects quality of life.
What is another disorder of the prostate
Prostate Cancer
1 in 8 men will be diagnosed — also pretty common.
Symptoms:
Frequent urination
Blood in urine (bad sign — go see a doc!)
Pain when peeing
can’t empty bladder fully
Treatment:
Radiation or chemo
Surgical removal of prostate
****But here’s the catch:
If the prostate is removed, the man can become infertile because…
The prostate's secretions are what:Help sperm swim AND Protect sperm DNA on the journey
No prostate = sperm can’t swim = sperm can’t reach the egg ❌
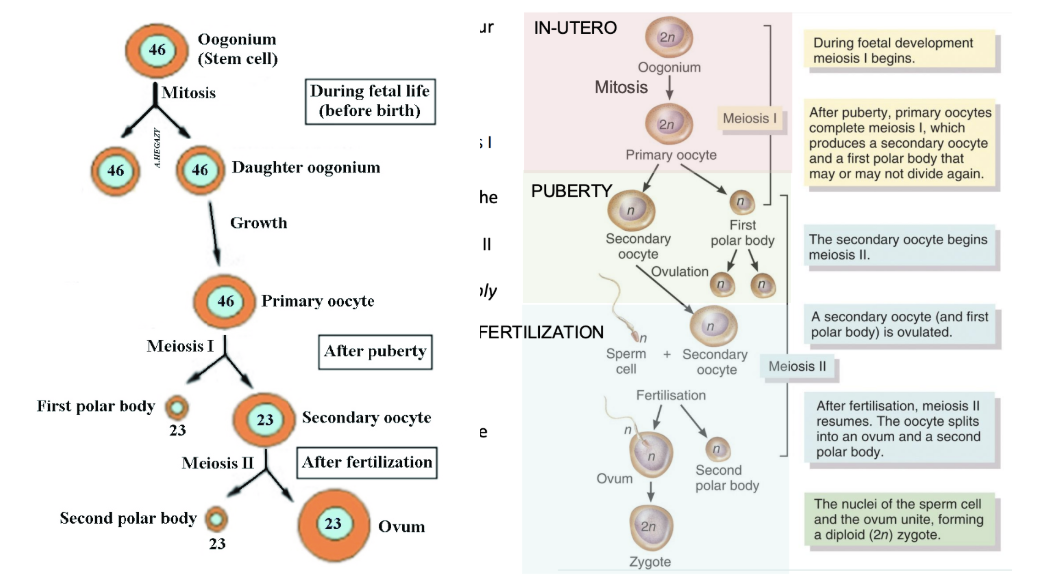
What is oogenesis?
Oogenesis = the process of making a mature egg (ovum) in people born female.
When does oogenesis start
IN UTERO: Before You Were Born
What proccesses occur in oogenesis IN UTERO: Before You Were Born
IN UTERO: Before You Were Born
You started with oogonium (a baby egg cell, 2n = 46 chromosomes).
It made primary oocytes by mitosis.
These primary oocytes begin meiosis I... but paused halfway and got frozen in it!
You were born with all the eggs (primary oocytes) you'll ever have — ~500,000, each paused in mitosis before meiosis I.
So from birth to puberty, all your eggs are just chilling, frozen in time.
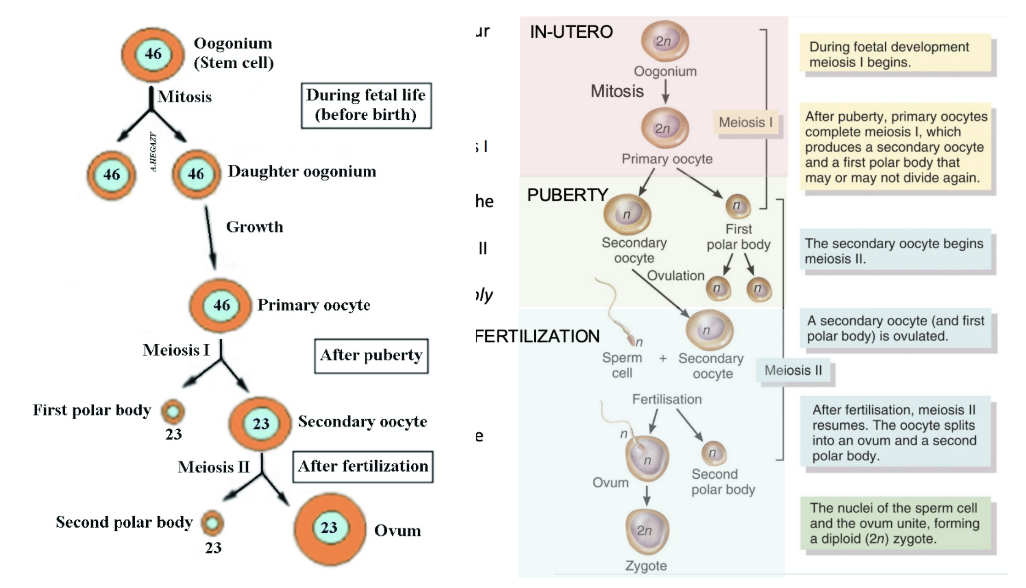
What proccesses occur in oogenesis during PUBERTY: The Eggs Wake Up
PUBERTY: The Eggs Wake Up
When you hit puberty, your hormones (like FSH and LH) wake up some of those frozen primary oocytes.
Each month, a few unfreeze and complete meiosis I.
This gives:
A secondary oocyte (what gets ovulated)
And a first polar body (a tiny useless cell that gets tossed away)
The secondary oocyte now paused in meiosis I before it starts meiosis II
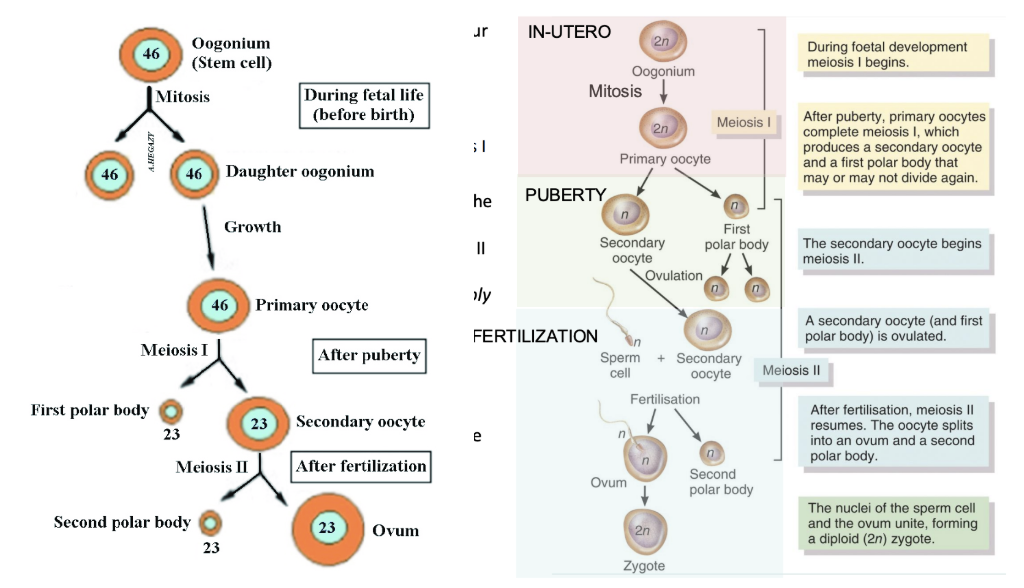
What proccesses occur in oogenesis during OVULATION
OVULATION
The secondary oocyte is released from the ovary into the fallopian tube.
This is called ovulation.
Important: It is still NOT a mature ovum! It only finishes meiosis II if it's fertilized by sperm.
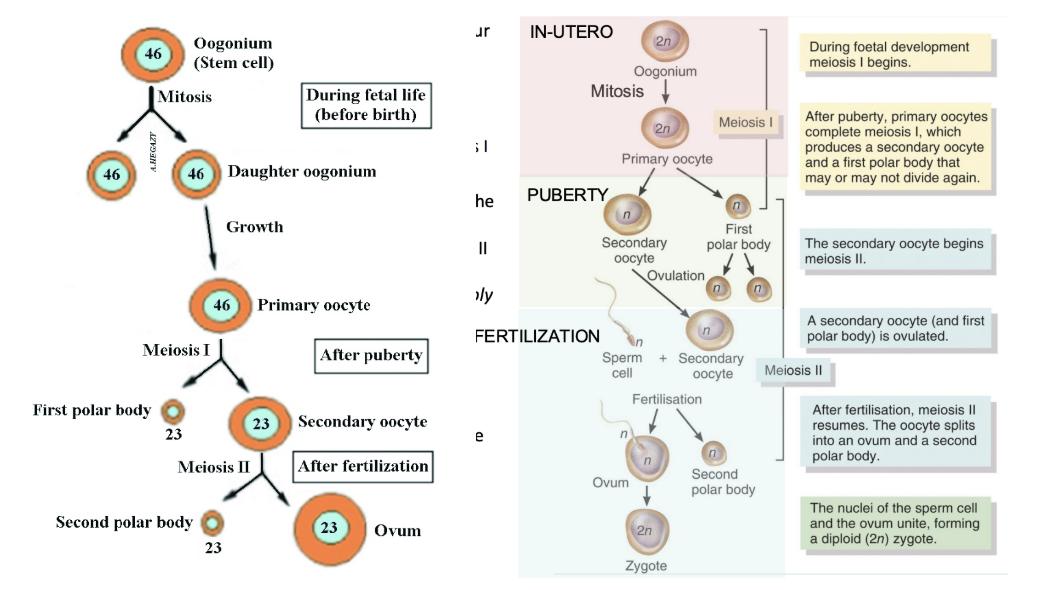
What proccesses occur in oogenesis during OVULATION
FERTILIZATION
If a sperm cell enters the secondary oocyte:
Meiosis II finishes!
The oocyte becomes a mature ovum
A second polar body is tossed out
The ovum (1n = 23) and sperm (1n = 23) combine to make a zygote (2n = 46)
This is the moment new life begins.
What are all the polar bodies??
You don’t want to split your cell contents equally.
You keep all the nutrients, organelles, cytoplasm in one big cell (the egg)
The leftover DNA gets shoved into tiny polar bodies that die.
This ensures the ovum is strong and ready to grow a baby if fertilized.
What is a follicle?
Follicles are “nests” that support the developing egg.
What does each follicle contain?
Each follicle in the ovary contains only ONE egg (primary oocyte - that has STOPPED after mitosis0
What are the 7 stages of follicular development
Follicle Stages:
Primordial follicle
➤ You’re born with ALL the eggs you’ll ever have, but they’re immature.
➤ These immature eggs are inside primordial follicles, which contain primary oocytes.
➤ They stay frozen before meiosis I and don’t finish developing… yet.
**PUBERTY OCCURS
Primary follicle
➤ Hormones wake up some of those sleeping primordial follicles.
➤ They now turn into primary follicles (still holding the same egg — still a primary oocyte).
➤ A few of these start developing each month, but only ONE becomes dominant most of the time.
Secondary follicle
➤ That dominant follicle becomes a mature follicle (also called a Graafian follicle) and contains a secondary oocyte — the egg is now halfway matured!
➤ MEIOSIS 1 complete
Mature (Graafian) follicle
➤ Ready to ovulate — releases secondary oocyte
Ovulation
➤ Follicle bursts, egg is released
➤ It releases the secondary oocyte — this is ovulation.
➤ The egg is now in the fallopian tube, waiting for sperm.
➤ Meiosis II is still not finished yet — it pauses again!
Corpus luteum
➤ The empty follicle (left behind after egg pops out) becomes a Corpus luteum - A hormone-secreting structure (a temporary gland)
➤ It secretes:
Estrogen
Progesterone
Inhibin
➤To prepare the uterus for pregnancy
Corpus albicans
➤ If no pregnancy happens, luteum breaks down into scar tissue
➤ The egg dies
➤ The corpus luteum shrinks and becomes a corpus albicans (basically scar tissue)
➤ Hormone levels drop
➤ You get your period (uterine lining sheds)
what would happen if there WAS fertilization
**What If There Is Fertilization?
➤ The sperm meets the secondary oocyte in the fallopian tubes.
➤ That triggers MEIOSIS II to finish
➤ The egg becomes a true ovum, and the nuclei from sperm + egg fuse.
➤ You now have a zygote (fertilized egg) — 46 chromosomes (23 from each parent).
Where does Hormone control begin in females? What does it release
Step 1: Start at the Brain – Hypothalamus
The hypothalamus is like the boss that sends out the first signal:
GnRH = Gonadotropin-Releasing Hormone
GnRH tells the anterior pituitary to get to work.
After GnRH is released, what is released as a result?
Step 2: Anterior Pituitary Releases Two Hormones
FSH = Follicle Stimulating Hormone
LH = Luteinizing Hormone
Both go to the OVARIES, but they do different jobs.
What does FSH do in the ovaries
**Step 3: What FSH Does
FSH goes to the ovaries, specifically to growing follicles (the tiny egg sacs).
FSH stimulates the growth of follicles
Those growing follicles release estrogen and a little inhibin.
Too many follicles growing?
Inhibin shuts down FSH production (negative feedback).
GnRH ➡ FSH ➡ Ovarian Follicles ➡ Estrogen & Inhibin
what does LH do in the ovaries
**Step 4: What LH Does
LH goes to the ovaries and it does two major things
When estrogen levels are high (positive feedback), LH surges → triggers ovulation (the egg pops out of the mature follicle)
After ovulation, LH helps that leftover follicle become the corpus luteum
GnRH ➡ LH ➡ Ovulation ➡ Corpus Luteum
Specialized feature of the ovaries**: What does the corpus luteum do in the ovaries?
**Step 5: What the Corpus Luteum Does
After ovulation, the corpus luteum (the leftover egg sac) becomes a little hormone factory. It releases:
Progesterone: Protects the uterine lining (endometrium) so it's ready for a baby
Estrogen: Still helping thicken the lining
Inhibin: Stops more FSH from being made—no new follicles, please!
Relaxin: Keeps uterus chill (no contractions yet); softens joints/cervix later if pregnant
Too much estrogen + progesterone?
Negative feedback shuts down GnRH, LH, FSH
what are the 3 stages of the menstrual cycle?
THE MENSTRUAL CYCLE (28 Days-ish)
Split into 3 major stages:
FOLLICULAR PHASE (Days 1–13)
OVULATION (Days 14)
LUTEAL PHASE (Days 15 - 28)
what happens during the FOLLICULAR PHASE
FSH rises → stimulates follicles to grow
One follicle becomes dominant (contains secondary oocyte)
Follicle releases estrogen
Estrogen thickens the endometrial lining
At first: Low estrogen levels = blocks LH, allows FSH to rise
By the end: High estrogen levels = LH surge! (**inhibin from follicles shuts down FSH production)
what happens during the OVULATION phase
LH surge (due to high estrogen levels) causes follicle to rupture
Egg is released!
Egg travels to the fallopian tube
what happens during the LUTEAL PHASE
Follicle becomes the corpus luteum (with help of the LH)
Corpus luteum makes: Progesterone, Estrogen, Inhibin, Relaxin
Progesterone holds the uterine lining in place
If no fertilization:
Corpus luteum shrinks
Hormones drop
Uterine lining sheds → period starts
OVERALL: what is the roles of Progesterone, Estrogen, FSH, LH
OVERALL: Recap the hormone levels during a full cycle
Clinical Correlate: What is endometriosis?
Endometrial-like tissue grows outside the uterus
What Happens:
Tissue still responds to cycle hormones
Bleeds during period → but nowhere to exit
Causes scar tissue, pain, and infertility
Symptoms:
Painful periods
Pain during sex, pooping, or peeing
Infertility
Treatment:
Birth control pills (reduce estrogen)
Surgery (remove tissue)
What are 4 forms of contraception?
Intrauterine Device (IUD)
A small T-shaped device placed inside the uterus.
Comes in 2 main types: hormonal (secretes progestin) or copper (non-hormonal).
How it works:
Thickens cervical mucus, making it hard for sperm to swim through the cervix.
Alters the environment in the uterus/fallopian tubes, making it hard for sperm or a fertilized egg to survive.
Progestin (a synthetic form of progesterone) creates a negative feedback loop — it tells the brain to stop releasing GnRH, which means less FSH and LH, so no ovulation happens.
Oral Contraceptive (Birth Control Pills)
Contains estrogen and progesterone, or just progesterone.
Mimics pregnancy hormone levels → prevents ovulation.
High hormone levels tell the brain: "We're already pregnant, no need to ovulate!"
Red pills in the pack are placebos (no hormones) → causes a drop in hormone levels → triggers a "fake period".
How it prevents pregnancy:
❌ No ovulation
❌ Thicker mucus
❌ Unfriendly environment for sperm
Vasectomy
Procedure for individuals assigned male at birth.
Vas deferens is cut and tied → no sperm can get into semen.
Reversible sometimes, but not guaranteed.
Tubal Ligation
Procedure for individuals assigned female at birth.Fallopian tubes are blocked, cut, or tied so the egg can't meet sperm.
Permanent (irreversible).
So even if ovulation happens, fertilization cannot.
What is menopause?
Natural end of menstruation and fertility in people assigned female at birth.
what happens during menopause?
What happens:
Ovaries shrink (atrophy) and stop responding to FSH and LH.
Estrogen and progesterone levels drop.
No more ovulation
No more periods
FSH and LH rise in the blood (because ovaries are ignoring them now).
Descent of the Gonads - 👦 Assigned Male at Birth
Testes start inside the abdomen during early development.
A structure called the gubernaculum pulls the testes down through the body wall into the scrotum by 9 months of gestation.
If testes don’t descend → infertility (they get too hot inside the abdomen for sperm production).
Spermatic cord (bundle of “wires” - vas deferens, blood vessels, lymph vessels etc.) forms from this descent.
Descent of the Gonads - 👧 Assigned Female at Birth
👧 Assigned Female at Birth
Ovaries also descend but only into the pelvis.
The ovaries stay inside the body (they don’t exit like testes).
The gubernaculum becomes:
The ligament of the ovary (connects ovary to uterus)
The round ligament of the uterus (anchors uterus forward)