Optic Nerve and Visual Pathway
1/68
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
69 Terms
Optic Disc (Optic Nerve Head)
• Manual technique count ~1.2 million RGCs
• Automated models 700,000 to 1.4 million RGC
• Other studies range from 1 million to 2.22 million
• Approximately loss of 5000 axons per year of life
• Small-diameter macular fibers to larger extramacular fibers
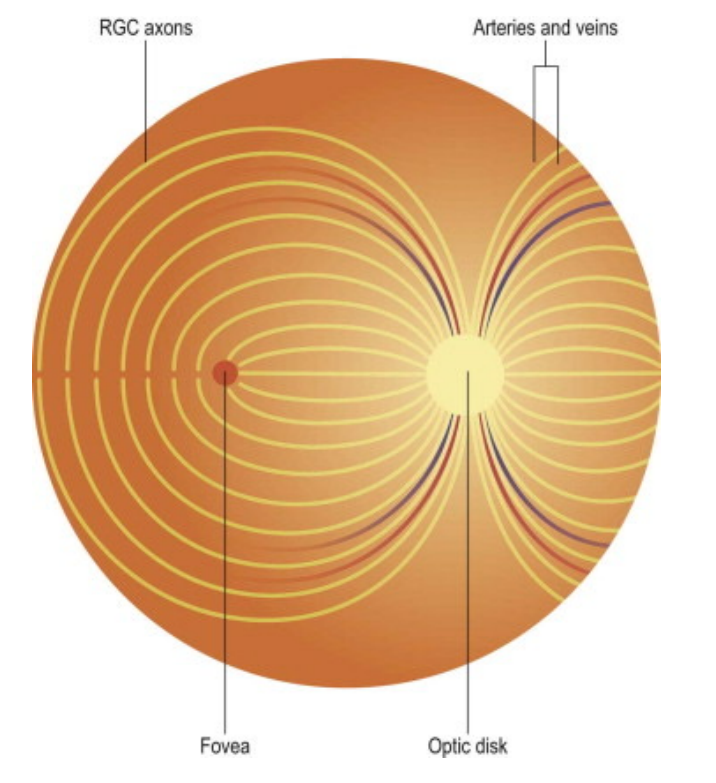
Retinal ganglion cell axons move towards the vitreous, then turn 90 degrees forming the retinal fiber layer, and head towards the optic disc
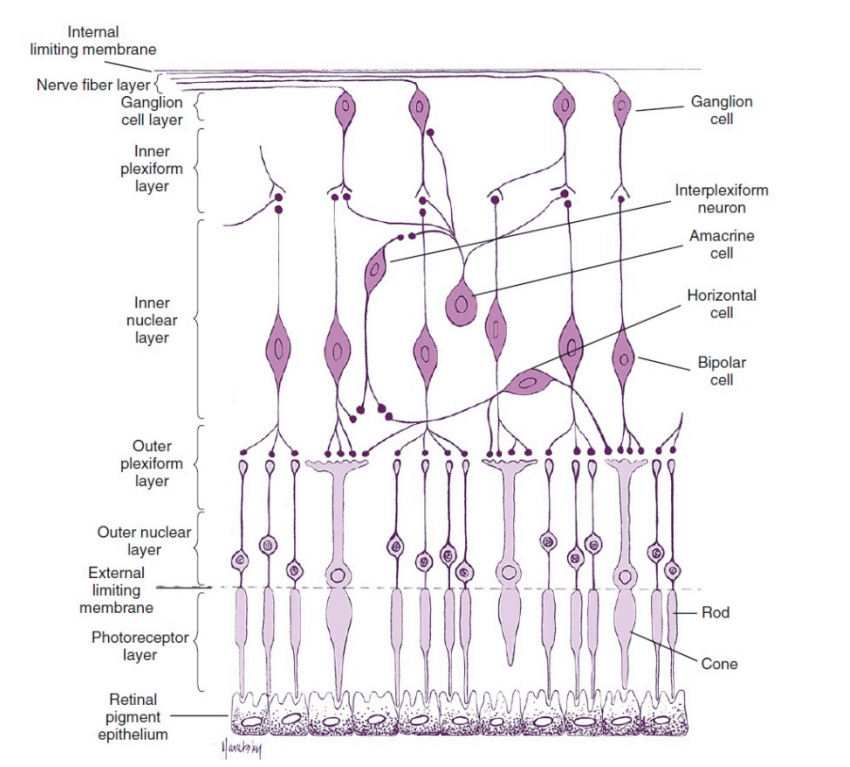
Arcuate bundles
Some axons do not course directly towards the disc. This pattern of fibers creates the arcuate bundles (superior, inferior, nasal radial, papillomacular).
This prevents axons from crossing the highly sensitive fovea to avoid scattering light and degrading visual acuity
The superior and inferior arcuate are separated by the horizontal raphe. This anatomical feature is vital in identifying optic nerve pathology
Optic Disc Location and Dimensions
Located nasal to the macula and slightly superior to the fovea
~15 degrees from the fovea
It is a physiological blind spot
Slightly vertically elongated
The size of the optic disc ranges
Different studies range (H x V) • 1.5 H x1.7 V mm
Lacks all retinal elements except nerve fiber layer and internal limiting membrane
Müller cells processes are replaced with those of astrocytes
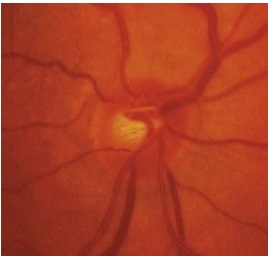
Optic Disc Color
No RPE gives it a lighter-colored look compared to the rest of the retina
Pink, salmon color of the optic disc is a combination of the scleral lamina cribrosa and capillary network
The lamina is more visible in some individuals
Flat with distinct margins
Cup-to-disc ratio
The nerve fibers around the edge make up the neuroretinal rim.
The space in the center, not containing nerve fibers, is called the cup.
The cup-to-disc ratio ranges from 0 to 1.0
Split into horizontal and vertical C/D.
Slightly larger horizontally
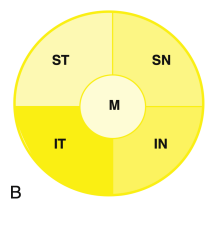
ISNT rule
Enlarging C/D ratio can be indicative of pathology (especially vertically)
Normal C/D ratio is slightly different between different ethnicities
Optic Nerve
RNFL turn another 90 degrees at optic Disc and exit as the “optic nerve”
90% will terminate in the LGN, 10% control pupils or circadian rhythm.
5-6 cm long
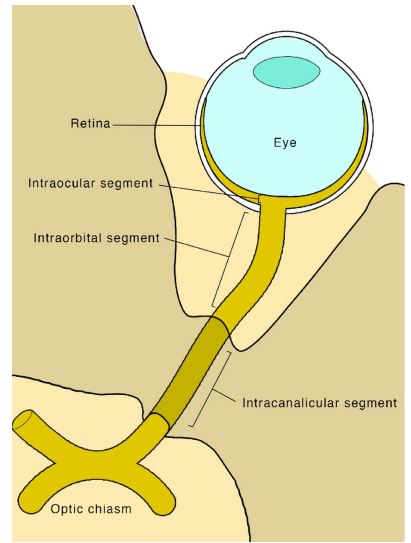
4 segments based on location
• Intraocular – 0.7 to 1 mm (shortest)
• Intraorbital – 30 mm (longest)
• Intracanalicular – 6 to 10 mm
• Intracranial – 10 to 16 mm (8-19 in some sources)
Intraocular (Intrascleral) Optic Nerve
Prelaminar and laminar regions
Axons from more peripheral retinal ganglion cells (RGCs) are peripheral within the optic nerve head
Glial tissue provides structural support for the nerve fibers
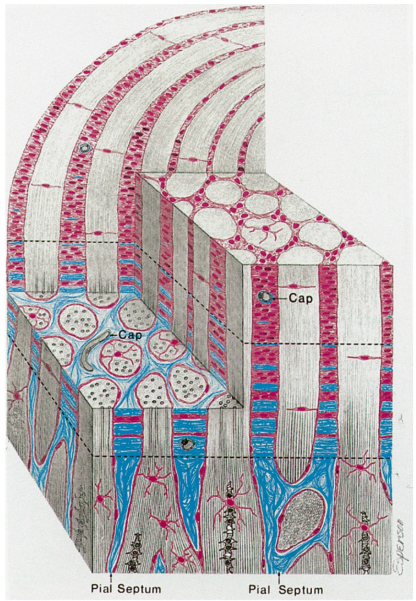
Astrocytes sheaths bundle the nerve fibers into fascicles, each containing 1000 fibers. Separated by pia-derived septa.
The marginal (border) tissue of Elschnig is a ring of collagenous tissue of scleral derivation that lies outer to the glial sheath
Tight junctions in the border tissue prevent any leakage from adjacent choriocapillary vessels.
The intermediary tissue of Kuhnt is a ring of glial tissue separating the optic nerve fibers from the retinal layers
The border tissue of Jacoby is the continuation of the intermediary tissue, and it separates the choroid from the optic nerve.
Lamina Cribrosa
Posterior Scleral Foramen
Interwoven collagen fibers form canals where optic nerve fibers pass
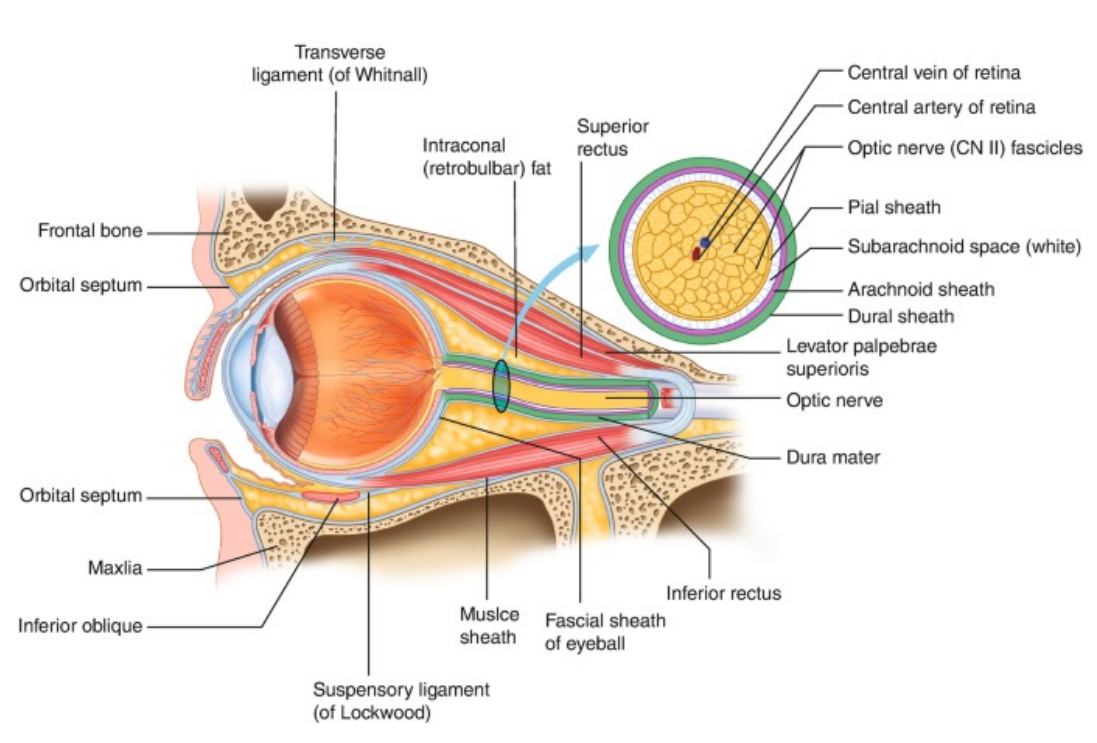
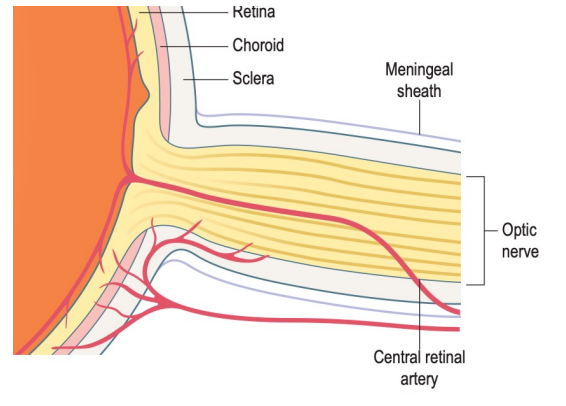
Intraorbital (post laminar) Optic Nerve
Exceeds the distance from the globe to the apex of the orbit
Shaped like a slight sine-wave shaped curve allowing for complete eye movements without stretching the nerve.
The superior and medial rectus muscles are adherent to the sheath of the optic nerve
Source of pain on eye movements in conditions like optic neuritis
Surrounded by three meningeal sheaths – all three fuse and become continuous with the sclera
Dura – outside; dense connective tissue full of elastic fibers
Arachnoid – middle; thin collagenous layer
Subarachnoid space is continuous with intracranial subarachnoid space and contains cerebrospinal fluid (CSF) – source of papilledema
Pia – innermost layer made of loose vascular connective tissue. Allows for blood vessels and connective tissue septa into the nerve. Only one to continue along the intracranial optic nerve
Unmyelinated retinal fibers pass through scleral perforations of the lamina cribrosa
Fibers from nasal macula continue to be located centrally
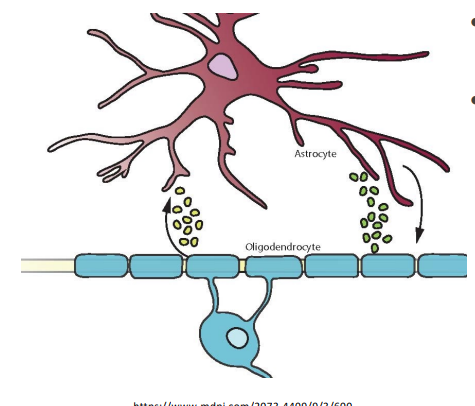
They become myelinated by oligodendrocytes as they pass through the pores
Myelin insulates axons and increase their efficiency and speed of conduction
The additional sheath of connective tissue from the pia mater and each fascicle nearly doubles the diameter of the optic nerve.
~1.5 mm at the level of the retina to 3 mm after it exits the globe
Astrocytes provide structure, store glycogen, and a regular extracellular concentration of ions
Travels within the muscle cone formed by the superior, lateral, inferior, and medial rectus muscles
Tumors within this cone can become a source of compressive optic neuropathy
Enlargement of the muscles secondary to systemic conditions like Grave’s disease, can also compress the nerve.
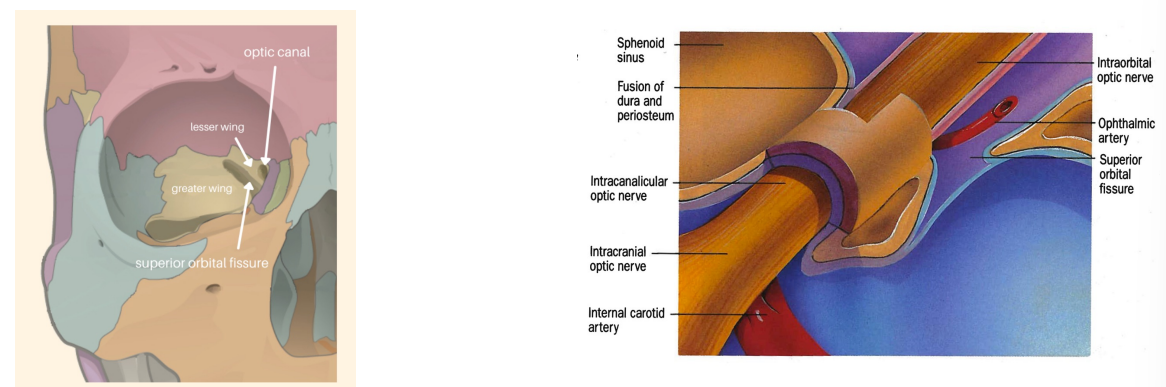
Intracanalicular
Optic Canal is a 5-12 mm passage located superonasal to the superior orbital fissure.
Passage for axons of the sympathetic pathway as well as the ophthalmic artery (inferolateral to the optic nerve, covered in dura)
Intracranial
Highly variable length 8-19 mm with average of 12 mm
Superior to optic nerve:
Anterior perforated substance
Root of olfactory tract
Anterior cerebral artery
Medial to optic nerve – sphenoid sinus
Inferior to optic nerve – internal carotid artery (inferior at first)
Lateral to optic nerve – internal carotid artery (inferior then lateral)
Ophthalmic artery enters the Dural sheath of the optic nerve as it passes through the optic canal
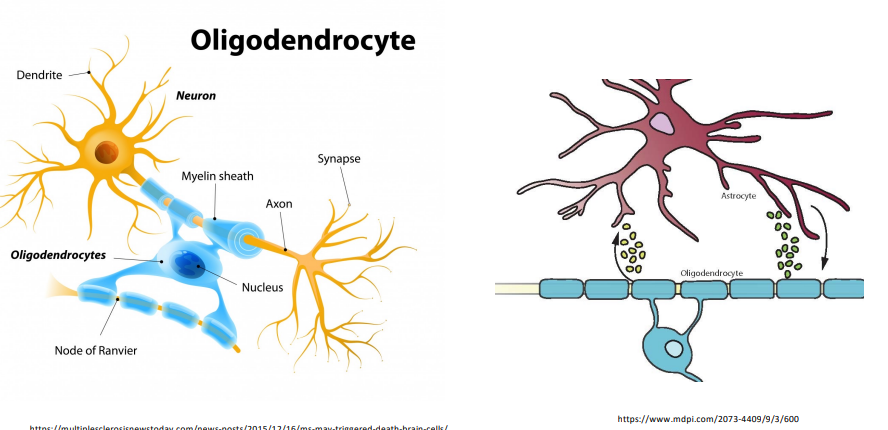
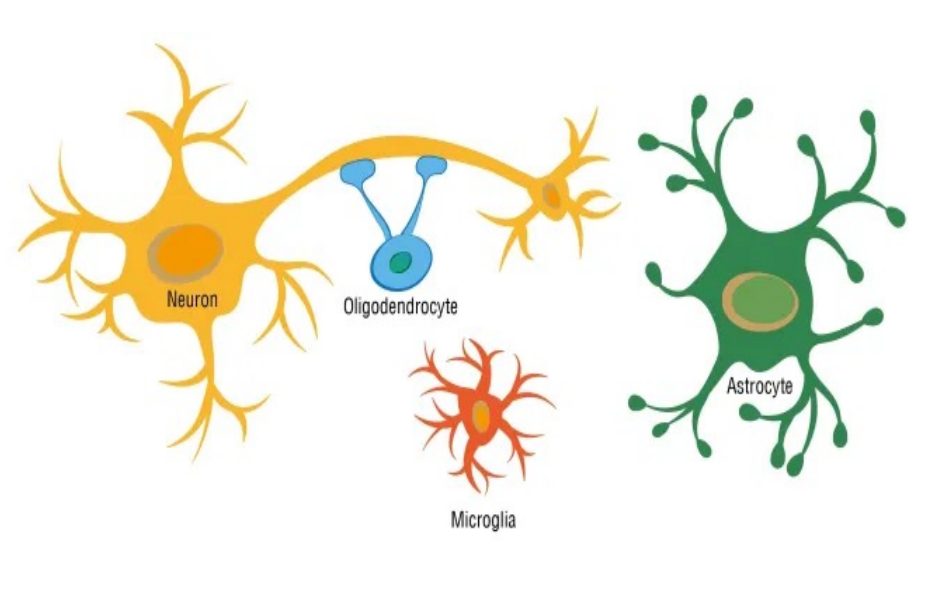
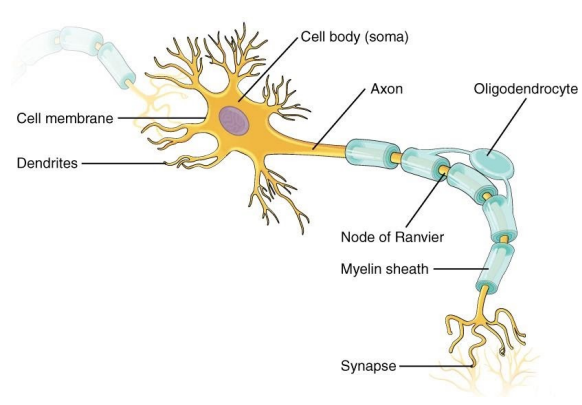
Cytology- Oligodendrocytes
myelin sheath. allow for transduction of signals
Cytology- Meninges
protective layers that surround the nerve
(inner) pia, subarachnoid, dura (outer)
Cytology- Astrocytes
Named for their stellate appearance
Glial tissue in the central nervous system
Regulates ionic and energy homeostasis in white matter like optic nerve
Highly efficient at transporting potassium
Accumulate glycogen serving as an energy source in the absence of glucose (ischemia)
Concentrated at the nodes of Ranvier and in contact with nearby capillaries
Transports substances between circulation and axons
Signal blood vessels to dilate and constrict to regulate metabolism of nerve
Pathology: Most common intrinsic tumors is astrocytoma (optic nerve glioma)
Usually found in childhood
Cytology- Microglia
Macrophage
Likely from peripheral bone marrow origin and not neuroectoderm like astrocytes and oligodendrocytes
Phagocytizes extracellular material
Associated with axon bundles
Involved in stimulation of immune system

Blood Supply – Optic Nerve Head
The central retinal artery enters the optic nerve approximately 12 mm behind the globe
Its branches supplies the inner retina
As it branches at the optic disc, it also provides partial perfusion of the superficial optic disc via small capillaries
Anastomoses of the posterior ciliary artery branches form the circle of Zinn-Haller which contributes significant perfusion to the optic nerve head.
Optic nerve vessels are non-fenestrated endothelial cells with tight junctions surrounded by pericytes and share the same blood-nerve barrier as the blood-brain barrier.
Optic nerve head vessels can also autoregulate to maintain blood flow despite intraocular pressure changes
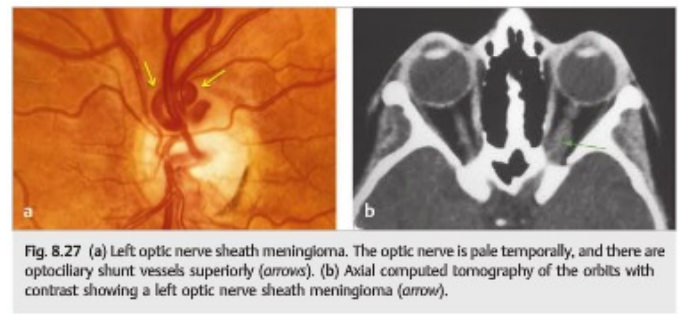
Blood Supply – Intraorbital Optic Nerve and Optic Canal
Intraorbital perfused primarily through the pial circulation
Branches off of the ophthalmic artery either directly or indirectly via recurrent branches of the short posterior ciliary arteries.
Intracanalicular perfused by three branches of the ophthalmic artery (medial collateral, lateral collateral, and ventral branch) which perfuse the pial surface and then penetrate the nerve
Removing optic nerve sheath meningiomas is very delicate because any removal of the pial supply will lead to a possible infraction and blindness
Axonal Action Potential
RGC axons transmit information via action potentials
All-or-nothing spikes of electrical activity
This is in contrast with the graded potentials of the retina
The actual amount of voltage-change, i.e., depolarization, is the same while the number of impulses per second and the distribution of impulses within the axons is the way visual information is carried down the optic nerve
Resting potential
Potential across the membrane is driven by the concentration of potassium
Concentration are achieved via the Na+ -K+ -ATPase.
Small amounts of leakage occur constantly
High concentration of Potassium [K+] inside of axon compared to extracellular
Higher concentration of Sodium [NA+] outside of axon compared to intracellular
Overall, negative resting potential
Depolarization
Potential across the membrane is driven by the concentration of sodium
Adjacent sections of the membrane of the axons gets depolarized
Opens voltage-sensitive sodium channels
Rush of sodium enters the axons causing it to be more positive (depolarized)
Each segment in the axons goes through the same process and the action potential travels throughout the axon
Repolarization
Voltage-sensitive sodium channels close and a transient opening of voltage-sensitive potassium channels open
The potential is then returned to be weighed by the potassium equilibrium and the resting potential is restored
Hyperpolarization
![<p><strong>RGC axons</strong> transmit information via <strong>action potentials</strong></p><p><strong>All-or-nothing</strong> spikes of electrical activity</p><ul><li><p>This is in contrast with the graded potentials of the retina</p></li></ul><p>The actual amount of voltage-change, i.e., depolarization, is the same while the number of impulses per second and the distribution of impulses within the axons is the way visual information is carried down the optic nerve</p><p><strong>Resting potential</strong></p><ul><li><p>Potential across the membrane is driven by the concentration of <strong>potassium</strong></p></li><li><p>Concentration are achieved via the Na+ -K+ -ATPase.</p></li><li><p>Small amounts of <strong>leakage </strong>occur constantly</p></li><li><p><strong>High </strong>concentration of <strong>Potassium </strong>[K+] <strong>inside </strong>of axon compared to extracellular</p></li><li><p><strong>Higher </strong>concentration of <strong>Sodium </strong>[NA+] <strong>outside </strong>of axon compared to intracellular</p></li><li><p>Overall, <strong>negative resting potential</strong></p></li></ul><p><strong>Depolarization</strong></p><ul><li><p>Potential across the membrane is driven by the concentration of <strong>sodium</strong></p></li><li><p><strong>Adjacent sections</strong> of the membrane of the axons gets <strong>depolarized</strong></p></li><li><p><strong>Opens</strong> voltage-sensitive <strong>sodium</strong> <strong>channels</strong></p></li><li><p>Rush of <strong>sodium enters the axons</strong> causing it to be <strong>more positive </strong>(depolarized)</p></li><li><p>Each segment in the axons goes through the same process and the action potential travels throughout the axon</p></li></ul><p><strong>Repolarization</strong></p><ul><li><p>Voltage-sensitive <strong>sodium channels close </strong>and a transient opening of voltage-sensitive <strong>potassium channels open</strong></p></li><li><p>The potential is then returned to be weighed by the<strong> potassium equilibrium</strong> and the <strong>resting potential </strong>is <strong>restored</strong></p></li></ul><p><strong>Hyperpolarization</strong></p>](https://knowt-user-attachments.s3.amazonaws.com/50394140-ac23-4610-849c-5e85820a91f6.png)
Role of Oligodendrocytes and Myelin
Decreases capacitance
Less sodium needed to enter the axon in order to depolarize the membrane
Increases resistance
Less leakage of charge across the membrane, thus saving energy that is spent by the Na+ -K+ - ATPase.
Ion channels in adult myelinated axons are not distributed uniformly
They are grouped into patches within the small areas where the axons are unmyelinated called nodes of Ranvier
Saltatory conduction
much faster
jumping from one node to the other
Such clustering is induced by oligodendrocytes
Axonal Transport
Orthograde – away from cell body and towards the brain.
Retrograde – towards the cell body and away from the brain.
Different rates of transfer
Fast and slow orthograde transport
Retrograde transport occurs at about half the velocity of fast orthograde
Axonal Repair
Adult Retinal ganglion cells (RGC) loss is irreversible, if true cell death occurred
Elsewhere in the CNS, embryonic neurons can regenerate and lose that ability with development.
Rate and timing of RGC death after optic nerve injury depends on the species, age, RGC cell body size, location of optic nerve transection in relation to the vascular supply
The distance from the site of the injury to the RGC is controversial
Some suggest that the shorter the distance, the more rapid degeneration. Others suggest that the two are not correlated
Axonal injury, binding of tumor necrosis factor to its receptors, and glutamate excitotoxicity all may result in apoptosis
Why does the apoptosis occur?
Lack of neurotrophic factors from the target tissue
Typically, these factors promote axon regeneration
Phagocytosis and immune activation
If macrophages and microglia are activated, they are poorly able to phagocytose degraded myelin, then the inhibitory signals found in myelin may prevent axonal regeneration
Gliosis
Astrocytes hypertrophy
Actively inhibits axons from regenerating
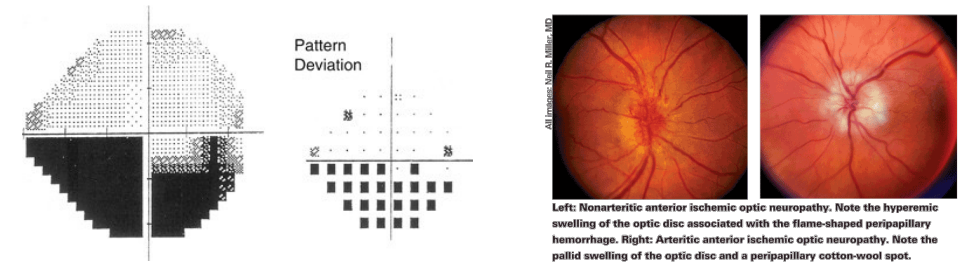
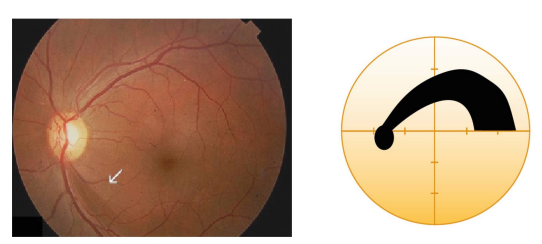
Clinical Cases- Ischemic Optic Neuropathy
Occlusion of the posterior ciliary arteries - not enough oxygen getting in
Non-arteritic anterior ischemic optic neuropathy (NAION) - associated with vascular disease and sleep apnea
Arteritic anterior ischemic optic neuropathy (AAION) - ocular emergency/ from GCA
Altitudinal defects; not distinct or flat edges → nerve swelling
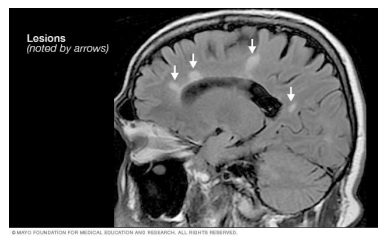
Clinical Cases- Optic Neuritis
Young to middle aged adults
More common in females
Often a presentation of multiple sclerosis
Inflammation results in demyelination of the optic nerve. Multiple rounds of such damage causes axonal loss and optic atrophy
Clinical Cases- Glaucoma
Group of distinct optic neuropathies distinguished by a distinct characteristic pattern of progressive excavation of the nerve head without significant pallor
Affects RGC and their axons
Increased cup-to-disc ratio

Clinical Cases- Compressive Optic Neuropathy
Tumors - Typically presenting unilaterally
Grave’s disease
Aneurysms
Clinical Cases- Papilledema
Papilledema is defined as optic disk edema secondary to elevated intracranial pressure.
Bilateral!
Should not be used to denote to disc edema. (if monocular, just optic edema)
It is unclear whether the visual loss associated with chronic papilledema results from disturbances of axonal transport, or from ischemia due to congestion of the optic nerve head.

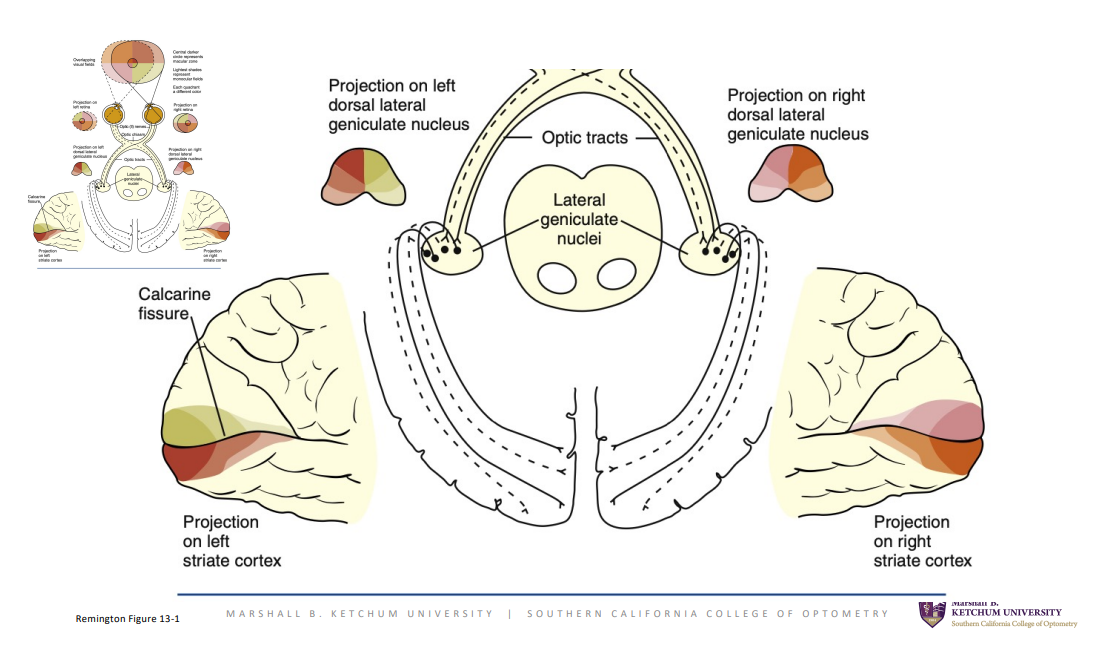
Overview
Optic Disc (Optic Nerve Head)
Optic Nerve (CN II)
Optic Chiasm
Optic Tract (one large axon from disc → tract)
Lateral Geniculate Nucleus (LGN) - 1st synapse
Optic Radiations
Striate Complex (visual cortex)
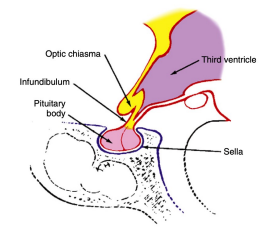
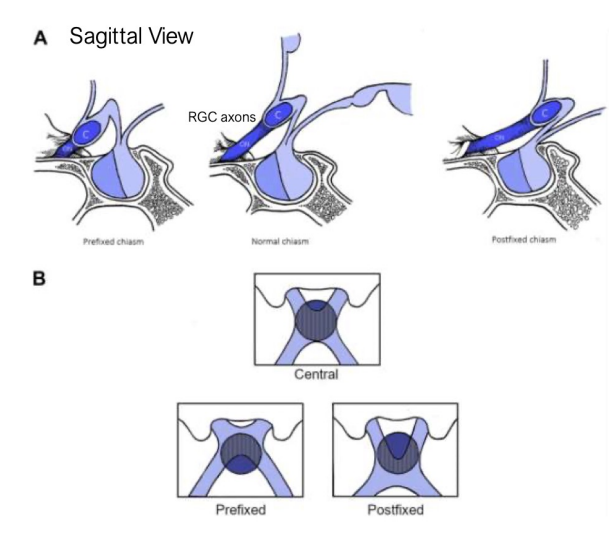
Optic Chiasm
Roughly rectangular
15 mm width, 8 mm anterior to posterior, 4 mm high
Located within the circle of Willis
Above the chiasm is the floor of the third ventricle, 1 cm below the chiasm is the pituitary gland
The chiasm is located above the sella turcica (the fossa in which the pituitary sits) ~10 mm above
Locations directly above (75%)
Prefixed – if the optic nerves are short and gland lies below the posterior part of the chiasm (10%)
Postfixed – if the optic nerves are long and the gland is situated toward the anterior of the chiasm (15%)
Temporal fibers remain ipsilateral
Nasal fibers cross at the chiasm and course towards the contralateral brain
Site of decussation
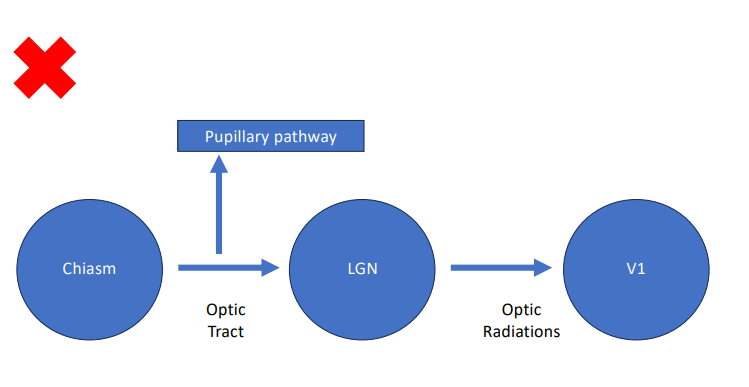
Optic Tract
Cylindric, slightly flattened
3.5 mm high x 5.1 mm long
Hippocampus is below the optic tract
Runs from the posterolateral corner of the chiasm to the LGN
Fibers of the pupillomotor reflex leave the tract before reaching the LGN and pass by way of the superior brachium to the pretectal nucleus in the midbrain
Some project to the hypothalamus involved in the circadian rhythm
Some terminate in the superior colliculus - orientation/ eye saccades
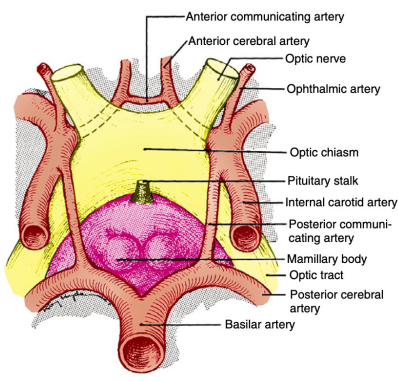
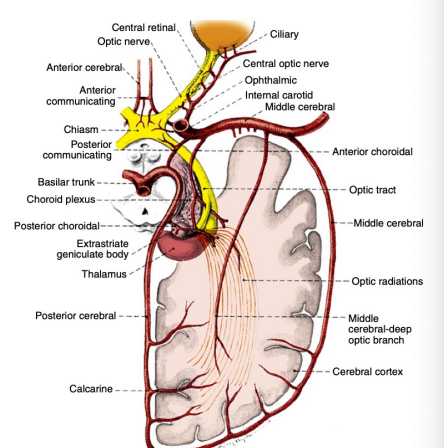
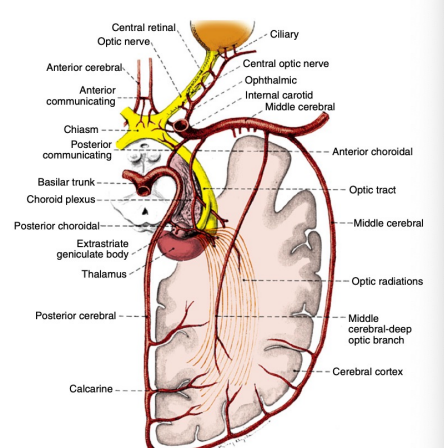
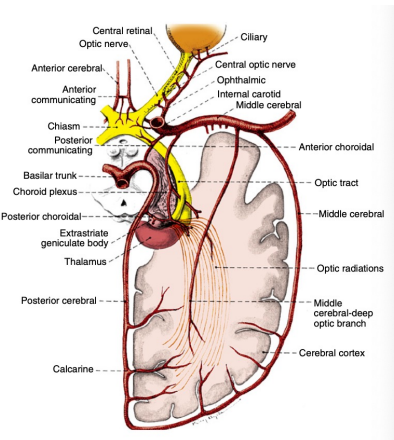
Blood Supply – Intracranial optic nerve, chiasm and optic tract
The intracranial optic nerve – branches from the ophthalmic, anterior cerebral, anterior communicating and internal carotid
Chiasm – circle of Willis forming two capillary beds:
Superior: anterior cerebral and anterior communicating arteries
Inferior: internal carotid, posterior cerebral, posterior communicating arteries
Optic tract is perfused by branches of the posterior communicating and anterior choroidal arteries (branches of the internal carotid)
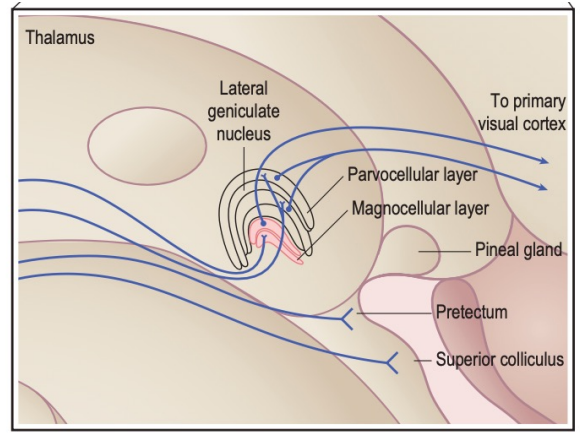
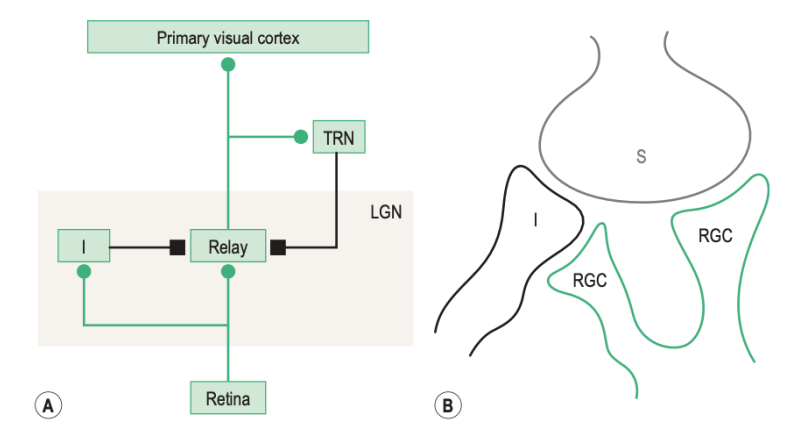
Lateral Geniculate Nucleus
It is the location where retinal axons terminate
Information from all the sensory systems except the olfactory pass through the thalamus before being transferred to the cerebral cortex
Visual information is processed in the LGN then related to higher cortical centers
Located on the dorsolateral aspect of the thalamus
Inferior horn of the lateral ventricle is posterolateral to the LGN
Not simply a relay station, but a center of complex processing
Receives input from cortical and subcortical centers as well as reciprocal innervation from the visual cortex.
Regulates flow of visual information
Axons leaving the LGN are called optic radiations
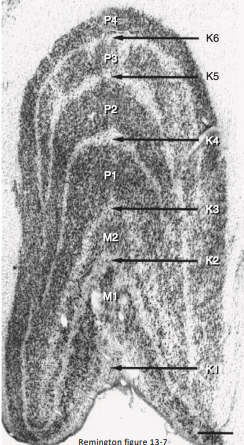
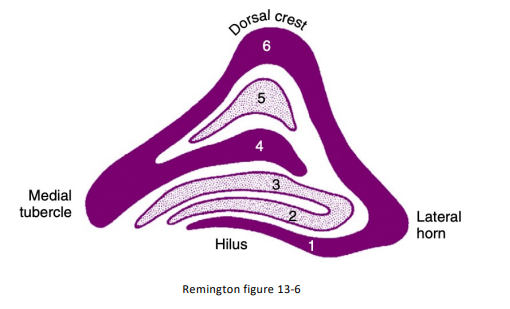
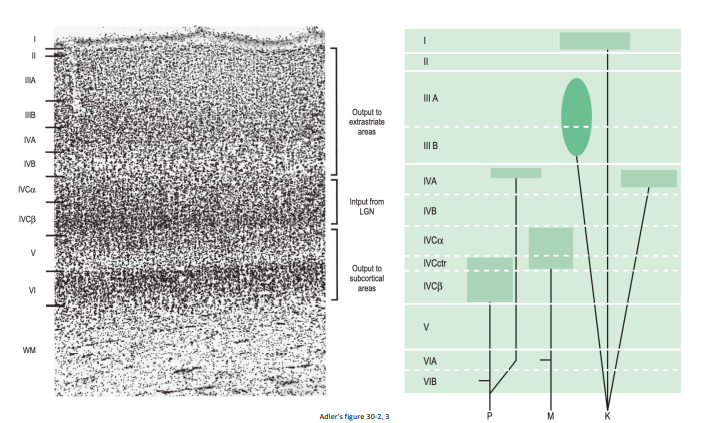
Lateral Geniculate Nucleus - 6 major layers
Each layer is composed of the same single cell type
Three types according to size:
Magnocellular (M cells) – large (2 layers located inferiorly)
Parvocellular (P cells) – medium (4 layers located superiorly)
Koniocellular (K cells) – small (below each of the six layers)
Lateral Geniculate Nucleus - Visual Field Processing
Most of the processing is dedicated to the central 2-17 degrees of the visual field
Mapped in specific layers
Superior visual field (inferior fibers) → lateral zone
Inferior visual field (superior fibers) → medial zone
Lateral Geniculate Nucleus - grouped in two cells classes
Relay cells – cells that send an axon to the visual cortex
Use glutamate
M, P, and K are all relay cells
Interneurons – cells with axons that remain within the LGN
Use gamma-amino butyric acid (GABA)
Ratio of 4:1 (relay to interneurons)
Lateral Geniculate Nucleus - inputs
Retina
Primary visual cortex
Some extrastriate areas
Pretectum
Superior colliculus
Parabigeminal nucleus (PBG) - satellite region of superior colliculus
Visual sector of the thalamic reticular nucleus (TRN) - send back info to LGN
*know red (input for visual stimuli), bolded (heaviest input), neurotransmitters used
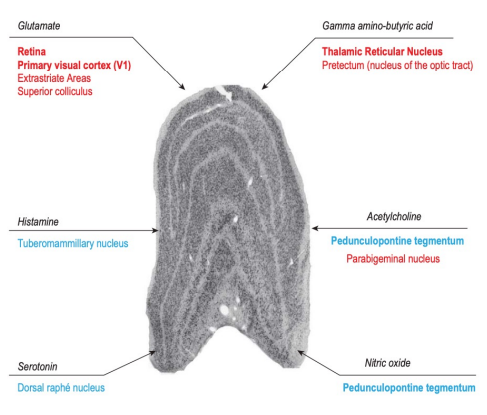
Lateral Geniculate Nucleus - outputs
Bulk primary visual cortex
Visual sector of the thalamic reticular nucleus (TRN)
Some terminate in extrastriate visual areas, the most well documented of these is the middle temporal area (MT).
Appears to originate from K LGN cells
~1 percent of all of the LGN cells
Responsible for residual vision referred to as “blindsight” in those who have lost their primary visual cortex.
Feedback pathway
Triad of retinal terminal synapses, relay cell dendrite, and a dendrite of an inhibitory interneuron
Retinal axons are the “drivers of the input” for 3 reasons:
They terminate closer than other excitatory inputs to the axon hillock of relay cells.
They have much larger terminals.
They signal through fast ionotropic glutamate channels located at these synaptic sites on LGN relay cell dendrites.
V1 cells get feedback from higher visual cortical areas, and these are very fast compared to slower messages arriving from the LGN to the cortex, thus intersecting continually, and adjusting messages from the retina continuously. (signal going out of LGN is slower)
Lateral Geniculate Nucleus - M, P, K cells
M Cells - hilus (bottom 2 layers)
Highest temporal frequency (temporal resolution)
Detect motion
Transient response: only at the entrance and withdrawal of a stimulus in their receptive fields
P Cells - crest (top 4 layers)
Higher sensitivity to spatial frequency (spatial resolution)
Responsible for red – green color detection
Sustained response: continue to respond to a visual stimulus as long as it remains present
K cells
Fall in between M and P cells in spatial and temporal resolution
Responsible for blue – yellow color detection
Largely unknown function
Modulators
Sleep/awake states
Burst firing during sleep, tonic firing while awake
Attention to attended vs unattended stimulus (harder to study and prove)
Motor planning
Likely involved in saccadic suppression
Although LGN cells are activated by single eye, there is evidence that contralateral eye may have influence
Binocular rivalry: presenting each eye with one image, the brain will alternate the two
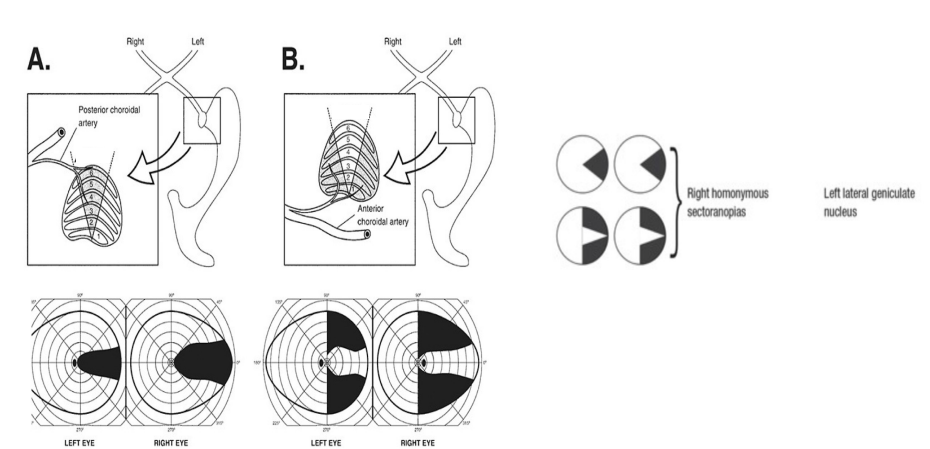
LGN– Blood Supply
The anterior choroidal artery (peripheral)
The posterior choroidal branches of the posterior cerebral artery (dorsal/ hilum wedge for the macula)
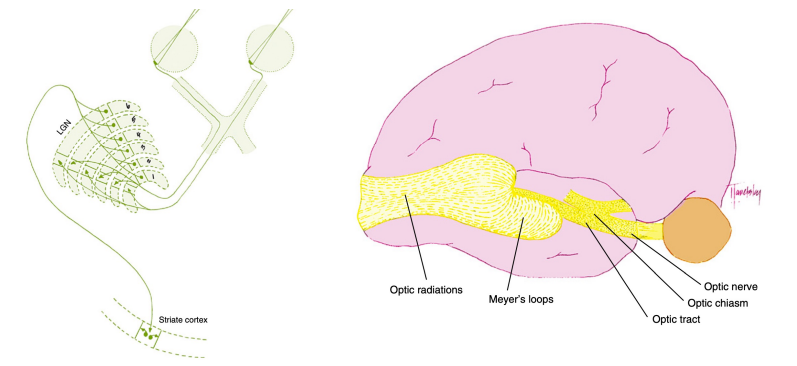
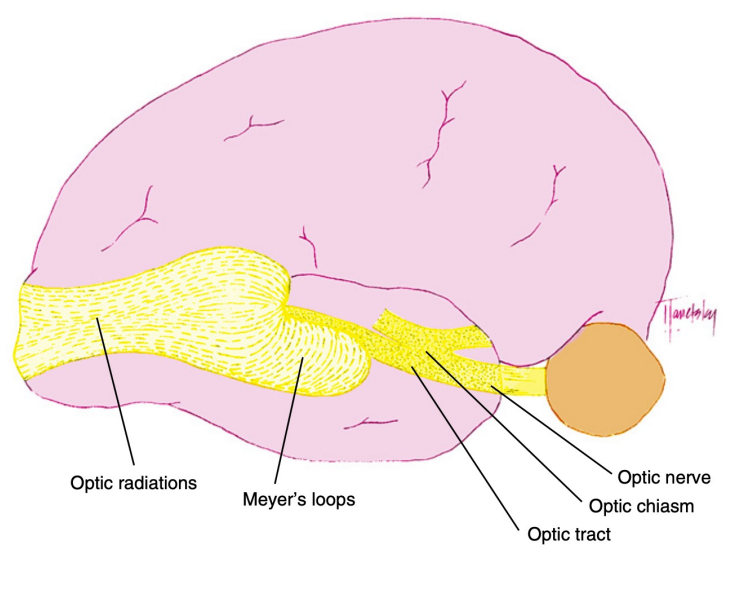
Optic Radiations
Optic radiations spread out fanwise sweeping laterally and inferiorly around the anterior tip of the temporal horn of the lateral ventricle
May loop in the temporal lobe or pass within the parietal lobe on their way to the occipital lobe.
Fibers leaving the lateral aspect of the LGN representing inferior retina follow an indirect route to the occipital lobe. They pass into the temporal lobe and loop around the tip of the temporal horn of the lateral ventricle forming Meyer Loops (inferior radiations)
Fibers from the medial aspect of the LGN representing superior retina lie superiorly as the pass through the parietal lobe.
The fibers from the macula are generally situated between the superior and inferior fibers
Optic Radiations - Blood Supply
The optic radiations can be divided into three sections:
Anterior radiations
Pass laterally over the inferior horn of the ventricle
Supplied by the anterior choroidal artery and the middle cerebral artery.
Middle Radiations
Passing lateral to the ventricle
Supplied by the deep optic branch of the middle cerebral artery
Posterior radiations
Supplied by branches of the posterior cerebral artery, including the calcarine branch
Branches from the middle cerebral artery also contribute
Striate Complex (Primary Visual Cortex)
2 main types of cells; both glutamate containing
Pyramidal 80%
Available in all layers
Stellate 20%
Mainly in layer IV
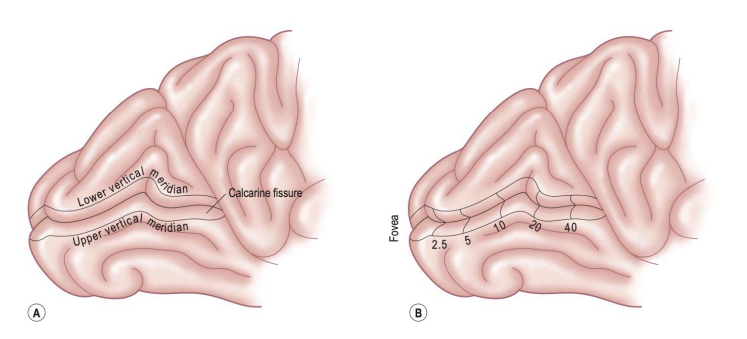
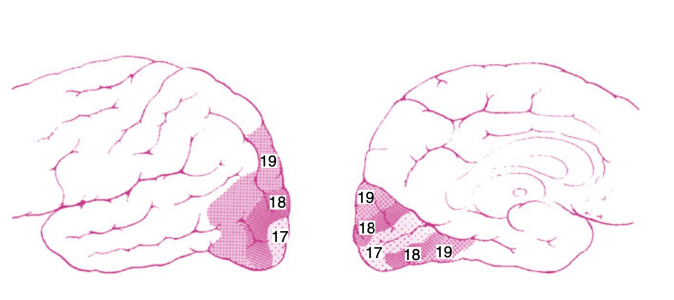
Primary Visual Cortex
Primary visual cortex (Brodmann area 17, V1)
Medial surface of the occipital lobe
Just a small portion (1 cm) extends around the posterior pole onto the lateral surface
Called striate cortex: white myelinated fiber layer called the white stria of Gennari
Calcarine fissure extends from the parieto-occipital sulcus to the posterior pole dividing the visual cortex into an upper portion (cuneus) gyrus and lower (lingual) gyrus
The fovea is represented in the occipital pole and the far periphery is represented in the anterior margin of the calcarine fissure
Upper visual field mapped on the lower lingual gyrus
Lower visual field mapped on upper cuneus gyrus
Primary Visual Cortex- Organization
2 mm thick and 1400-3400 mm²
Organized into horizontal layers and vertical columns
Organization:
Input: Fibers from thalamus ends up in middle layers IVC of V1.
Output: superficial layers above IVC send information to other cortical areas.
Output: Layers below IVC send signals to subcortical targets.
Ocular dominance columns: Left and right eye segregation of axons from the M and P LGN layers endings in layer IVC of V1
K LGN synapse on layers IVA, III, and I
Vertical organization:
Alternating parallel ocular dominance columns according to the eye of origin
Primary Visual Cortex- 6 Layers
Layer 1 most superficial, few scattered neurons
Layer 2 neurons that send axons only to the deeper cortical layers
Layer 3 neurons the communicate with both near and far cortical locations
Layer 4 stria of Gennari
subdivided into strata (receiving from either M or P cells)
Sends axons to more superficial visual cortex as well as other visual cortical areas
Layer 5 sends axons to superior colliculus and brainstem
Layer 6 send projections back to the LGN
Extrastraite Visual cortex
Information transmitted to extrastraite cortex (higher visual association areas) provide further interpretation
These areas surround V1 located on the lateral aspects of the occipital cortex
V2-V5; previously Brodmann 18-19
Visual and visual association areas in one hemisphere are connected to the corresponding areas in the other hemisphere through the posterior portion of the corpus callosum
Information about stimulus orientation, movement direction, binocularity are all constructed in V1
Primary Visual Cortex- Two hierarchies
Object – what something is “what pathway”
Also called the ventral stream
Consists of pathways going from V1 through V4 to the temporal cortex
Spatial - where something is “where pathway”
Also called the dorsal stream
Pathway from V2 through MT to the parietal cortex
Primary Visual Cortex - other outputs
Superior colliculus
Complete retinotopic map of the contralateral field of vision
Controls saccadic eye movements with input from the frontal eye fields
Frontal eye fields
Frontal lobe
Receives fibers from the V1 controlling conjugate eye movements
Voluntary and reflex ocular movements
Pupillary responses to near objects
Primary Visual Cortex / V1 - Blood Supply
The calcarine branch of the posterior cerebral artery is the major blood supply for the striate cortex
Supplemented by
The posterior temporal or parietooccipital branch of the posterior cerebral artery
The occipital branch of the middle cerebral artery
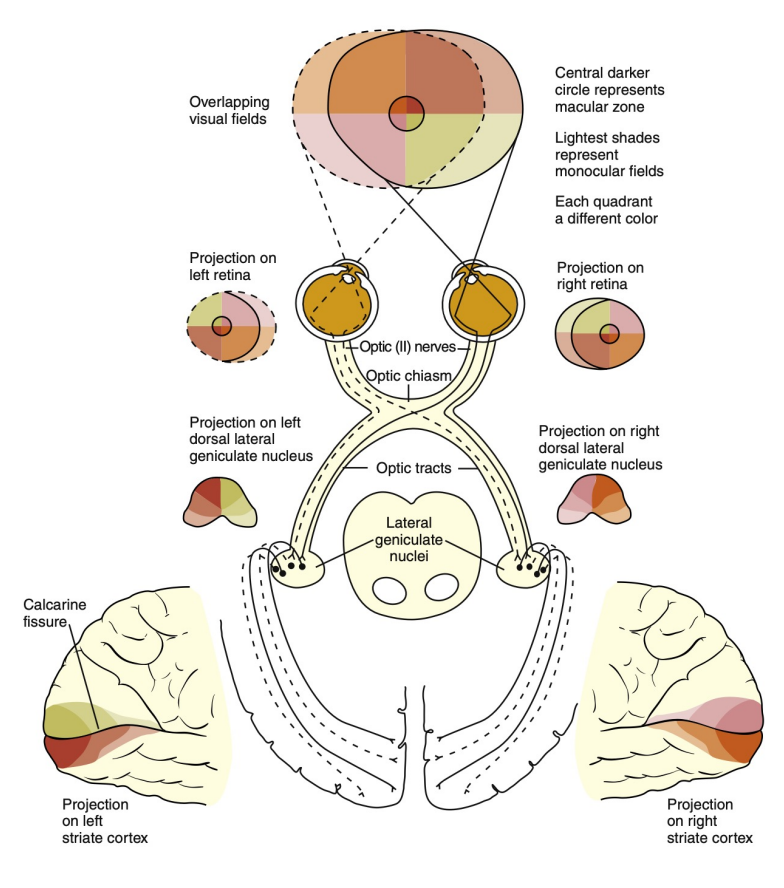
Visual Field
The entire visible area is termed the visual field.
Information taken in by the retina is processed through the visual sensory pathway reaching the visual cortex and extrastraite cortex.
Damage along the pathway causes defects in the visual field.
Knowledge of the fiber patterns can help in identifying the location of the lesion causing the defect.
Visual Field - Basic
The visual field is divided into 4 different quadrants split by a horizontal and a vertical midline.
The optics of the eye cause an inversion and reversal of the field
Superior field is imaged on inferior retina
Inferior field is imaged on superior retina
Nasal field is imaged on temporal retina
Temporal field is imaged on nasal retina
The point of fixation is seen by the fovea (central point)
Temporal field
Temporal field is larger than nasal field
Temporal crescent:
Far temporal periphery
Only imaged by the nasal fibers of the ipsilateral eye and not on the temporal retina of the contralateral eye
Secondary to the depth of the orbit and prominence of the nose
Physiologic Blind spot:
Correlated to the location of the optic nerve head
Secondary to a lack of photoreceptors at the optic disc.
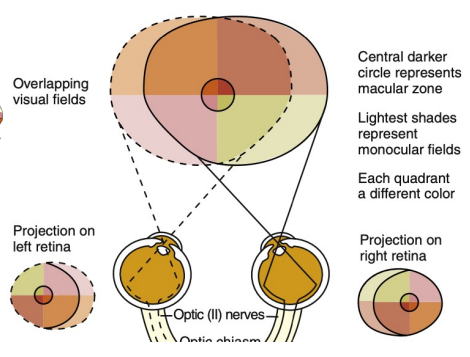
Retina
Superior and inferior temporal fibers are separated by the horizontal retinal raphe and arch around the macular area to reach the optic disc. These fibers are called the superior and inferior arcuate, respectively.
The fibers from the macular area to the optic disc are called the papillomacular bundle
The nasal fibers travel directly to the optic disc and are described as radiating thus labeled as nasal radial bundle.
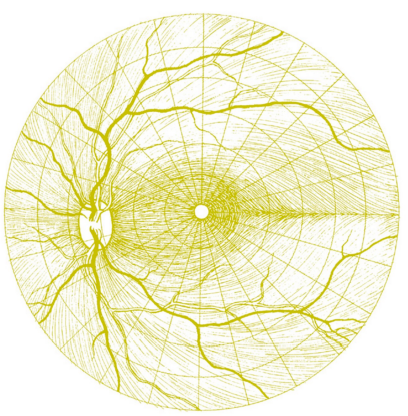

Retina → Optic Disc → Optic Nerve
Nasal fibers radiate directly to the nasal side of the disc.
Papillomacular bundle course to the temporal side of the disc.
Fibers from the superior arcuate arch around the papillomacular bundle to enter the superior pole of the disc. The same with the inferior to enter the inferior pole.
Macular fibers take up one third of the disc, despite the macular area being only one twentieth of the total retinal area.
The temporal fibers take up another third, and lastly the nasal fibers take up the last third.
Boundaries between each set of fibers are not always clear-cut.
Fibers from the peripheral retinal are more superficial than those coming from central locations
Macular fibers move to the center of the nerve.
The rest all line up in their respective logical location (e.g., superior temporal in the superior temporal portion of the nerve).
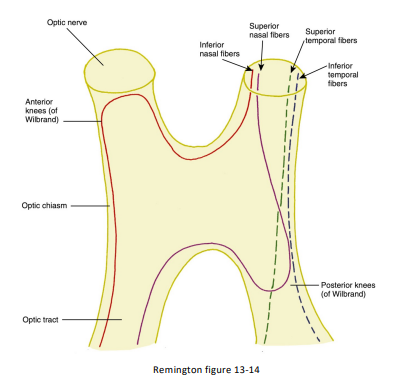
Optic Nerve → Optic Chiasm
Temporal fibers remain ipsilateral while nasal fibers cross (decussate).
The ratio of the crossed to uncrossed fibers in the chiasm is 53 to 47
Inferior nasal fibers cross inferiorly in the anterior chiasm and terminate part of the opposite optic nerve before turning back to the chiasm and into the contralateral optic tract. This is called the anterior knee of Wilbrand.
Superior nasal fibers cross superiorly in the posterior chiasm. These fibers loop posteriorly into the ipsilateral optic tract of the before crossing over. This is called the posterior knee of Wilbrand.
Small number of fibers exit the posterior chiasm and enter the suprachiasmatic nucleus in the hypothalamus and work on synchronizing the circadian rhythm.
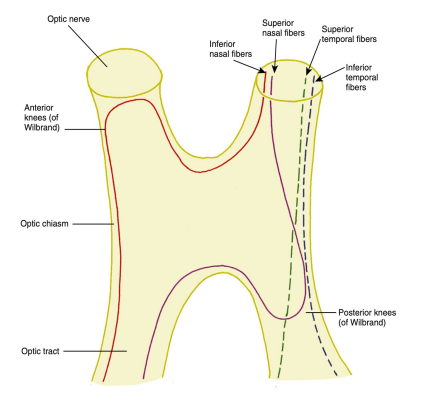
Optic Chiasm → Optic Tract
As the fibers leave the chiasm in the optic tract, the crossed and uncrossed fibers intermingle
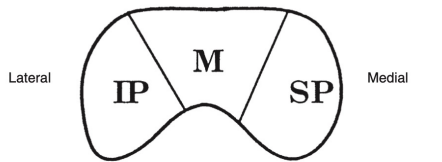
The superior fibers (the fibers from both the ipsilateral superior temporal retina and the contralateral superior nasal retina) move to the medial side of the tract.
The fibers from the inferior retina (ipsilateral inferior temporal retinal fibers and contralateral inferior nasal retinal fibers) occupy the lateral area of the tract.
The macular fibers remain in the middle of the groups
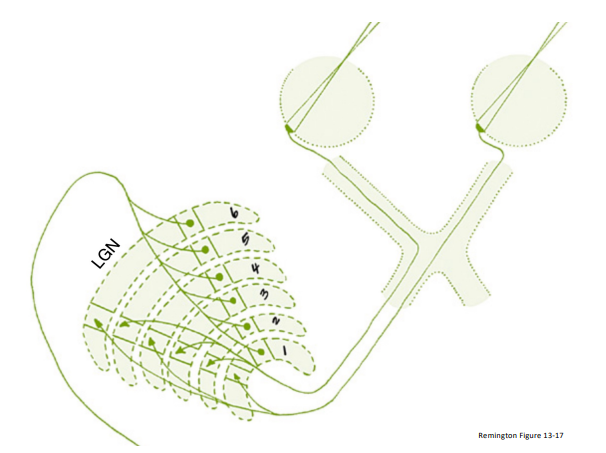
Optic Tract → LGN
Superior fibers from the optic tract terminate in the medial aspect of the LGN
Inferior fibers terminate in the lateral aspect of the LGN
A dorsal wedge composing 2/3 to 3/4 of the LGN is dedicated to the macula
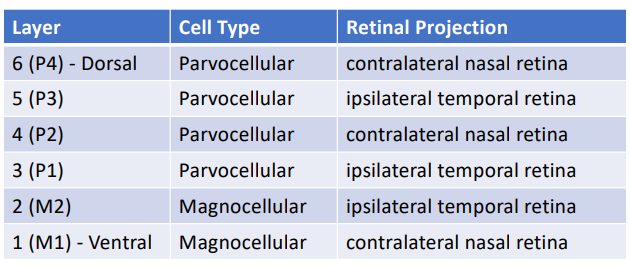
Layers 1, 4 and 6 receive input from the contralateral nasal retina
Layers 2, 3, and 5 receive ipsilateral temporal retina
Each layer of the LGN contains a retinotopic map or representation of the contralateral hemifield of vision.
A retinotopic map is a “point-to-point localization” of the retina.
Line of projection
A line passing through all six layers perpendicular to the surface
All the intercepted cells would be carrying information about the same point in the visual field.
This alignment is so precise that there is a gap in each contralateral layer along the line of projection that corresponds to the location of the optic disc.
LGN → Optic Radiations
Inferior retinal fibers leave the LGN from the lateral aspect, pass into the temporal lobe and loop around the tip of the temporal horn of the lateral ventricle. This is caller Meyer’s Loop. • Superior retinal fibers leave the LGN from the medial aspect and lie superiorly as they pass through the parietal lobe. • Macular fibers are situated between superior and inferior fibers.
Optic Radiations → Striate Complex (Primary visual cortex)
Inferior radiations terminate in the region below the calcarine sulcus called the lingual gyrus • Superior radiations terminate in the region above the calcarine sulcus called the cuneus gyrus • Fibers from the macular area terminate posteriorly in the visual cortex • Fibers from the nasal periphery terminate in the most anterior part of the visual cortex near the parietal lobe. This corresponds to the temporal crescent in the visual field seen by only the contralateral eye • Mapping of the visual cortex demonstrated that the central portion of the visual field occupies the majority of the striate cortex
Visual Field Territories
Territory 1: choroid and outer retina
Territory 2: inner retina and optic nerve
Territory 3: optic chiasm
Territory 4: Post-chiasmal
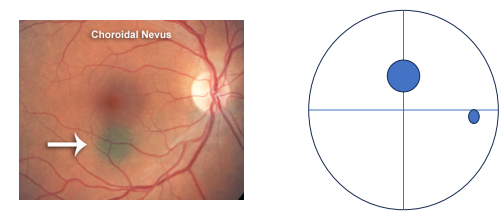
Visual Field - Territory 1
Defects in the choroid and outer retina will cause a field defect that is similar in shape to the lesion and located in the corresponding location of the field (e.g., a lesion in the superior nasal retina should be found in the inferior temporal field)
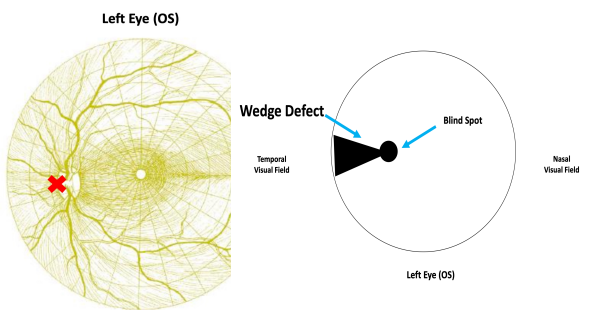
Visual Field - Territory 2
Damage to the superior, inferior and papillomacular nerve fiber bundles causes a field defect corresponding to the location and configuration of the affected nerve fiber layer.
These defects respect the horizontal midline
If the nasal radial bundle is affected, a wedge shape defect emanates from the blind spot.
Terminology for Visual Field Loss
“Anopia” or “Anopsia”- defines loss of a portion of the visual field
Hemianopsia – loss of half a visual field
Quadrantanopia OR quadranopsia – loss of one-quarter of a visual field
Sectoranopia – loss of a sector of a visual field
Heteronymous – two eyes have non-overlapping field losses
Homonymous – visual field loss is on the same side of the vertical line of both eyes
Congruity:
A judgment of how similar an incomplete homonymous hemianopic defect is
A characteristic of post-chiasmal VF loss only
It is secondary to the fact that nerve fibers from corresponding points lie adjacent to one another
Cannot judge congruity if the VF defect is total/complete (all points in the whole hemifield) and absolute (no sensitivity at all)
Congruity increases the more posterior the lesion is in territory 4
Visual Field - Territory 3
The location of the lesion in comparison to the optic chiasm determines the location of the defect
If the lesion is directly below the chiasm, the resulting defect is a bitemporal field defect.
If a lesion affects the anterior or the posterior portion of the chiasm as it connects to the optic nerve or optic tract, respectively, it may result with an anterior junctional scotoma or a posterior junctional scotoma
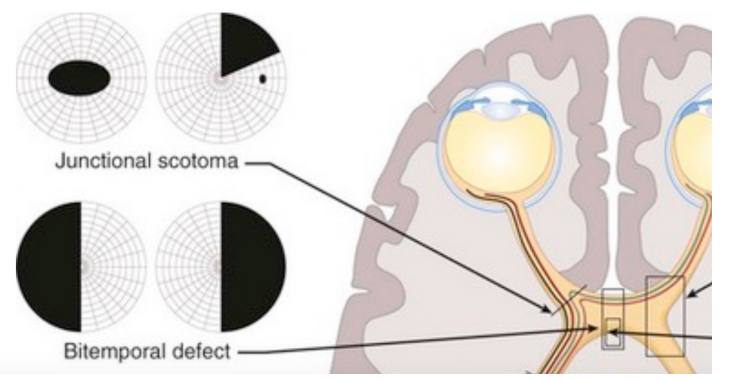
Visual Field - Territory 4
The postchiasmal pathway (ipsilateral temporal fibers and contralateral nasal fibers) carries information from the contralateral visual field (e.g., right pathway from left field) thus postchiasmal lesions cause a homonymous field defect.
Optic tract: relatively small in cross section so often a single lesion will damage the majority of fibers and causes a full homonymous field defect, if patrial may be incongruent. (affect one side more than other)
Can cause optic nerve atrophy and/or pupillary defects
LGN lesions cause a defect in the contralateral field
Can cause optic atrophy, but no pupillary defects.
Optic radiations running through the temporal lobe cause superior defects, while those running in the parietal lobe causes inferior defects.
Cannot cause optic atrophy or pupillary defects.
Occipital lobe: congruous hemianopsia, quadranopsia, possible macular sparing
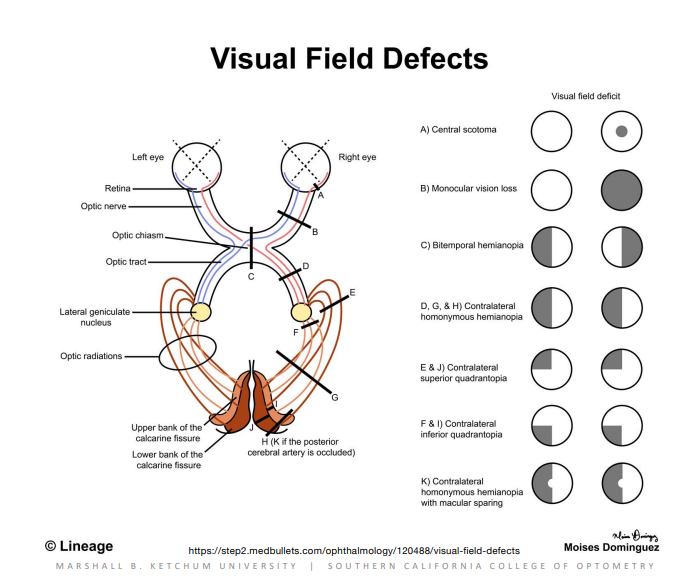
Visual Field Defects
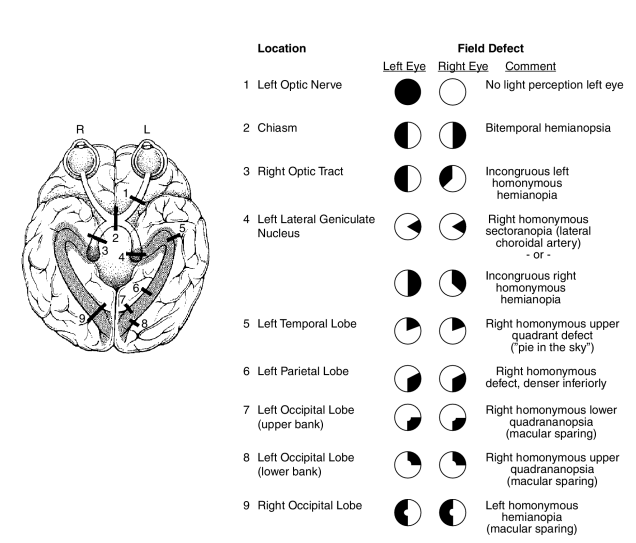
Visual Field Defects - LGN