Embryology 5 | Placenta and Fetal Membranes
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
36 Terms
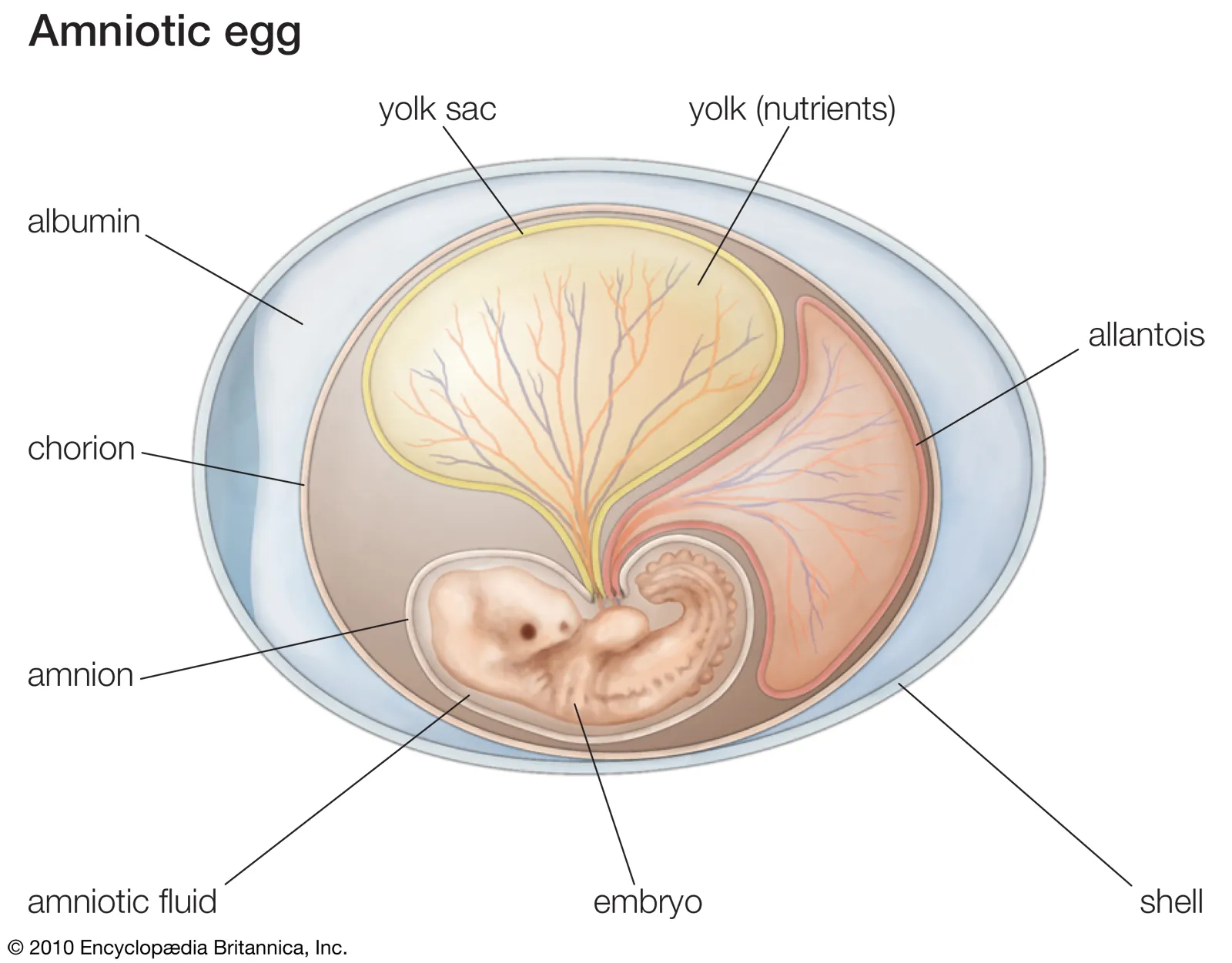
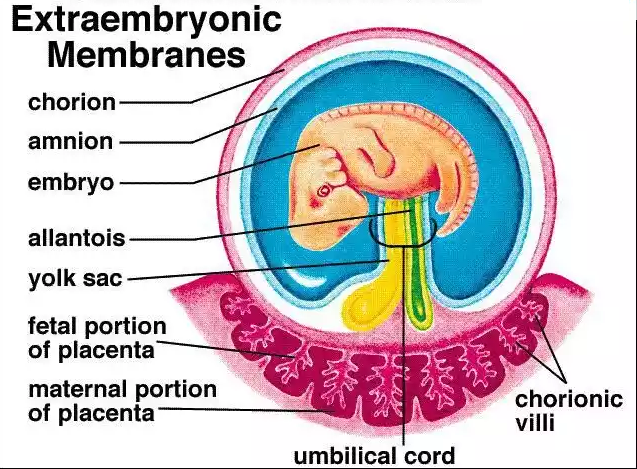
What are the fetal membranes and what is their fate?
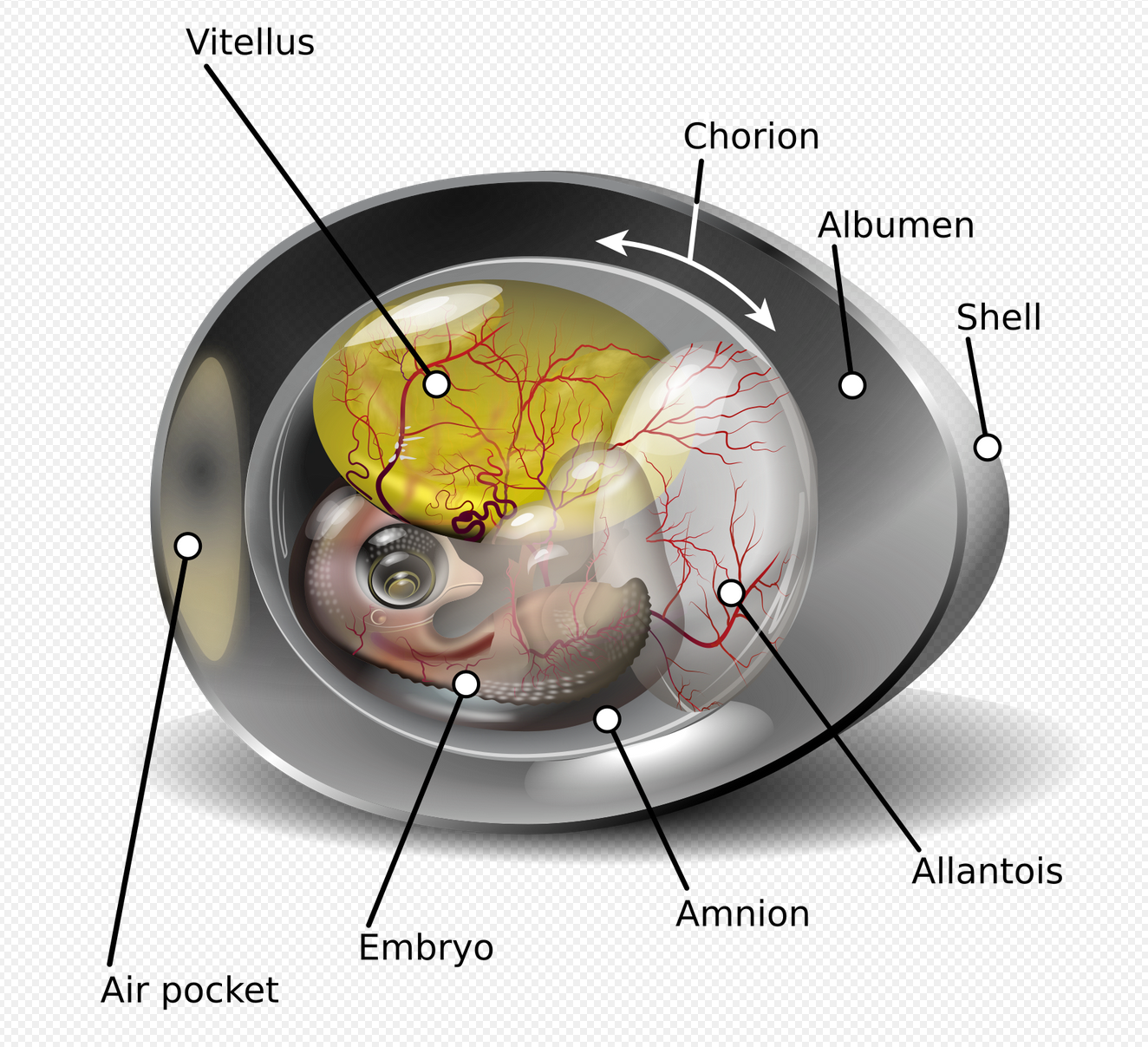
The chorion, yolk sac, amnion, and allantois are fetal membranes formed from the embryo, but they do not become significant parts of the fetus.
What is the placenta and what is its main function?
the primary site of exchange between mother and fetus.
What portions make up the placenta?
both maternal and fetal components.
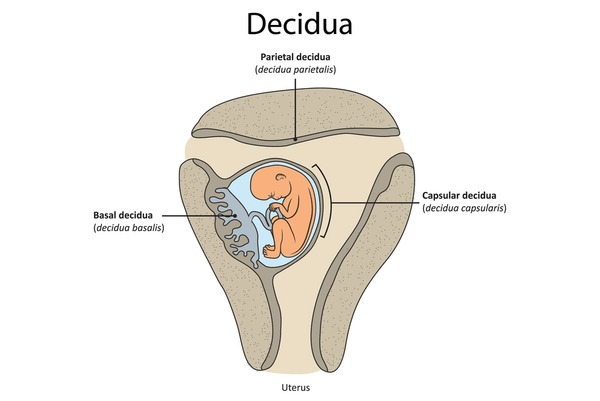
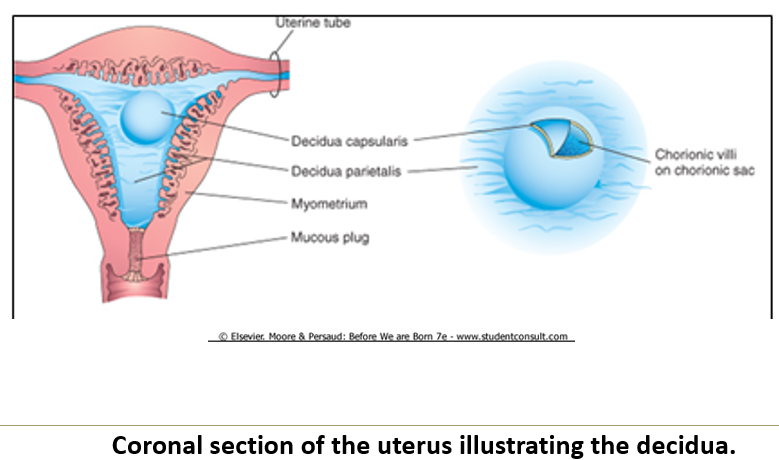
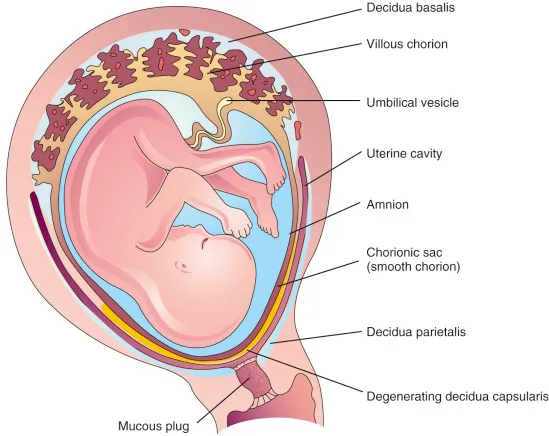
What is the decidua and when is it shed?
The functional layer of the gravid uterine lining, and it is shed after birth.
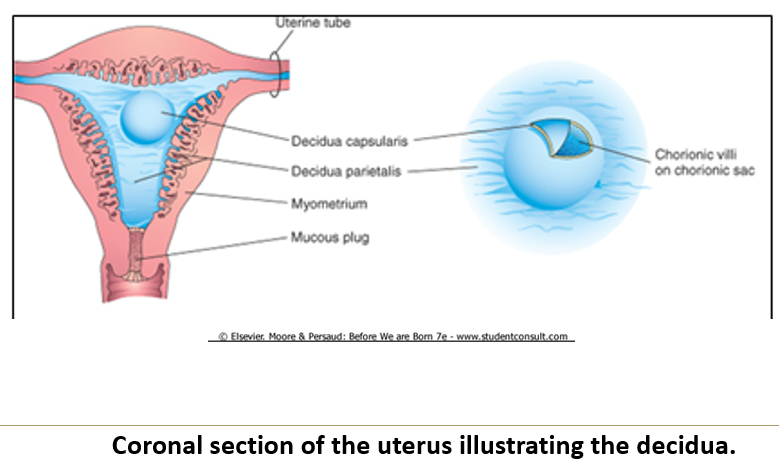
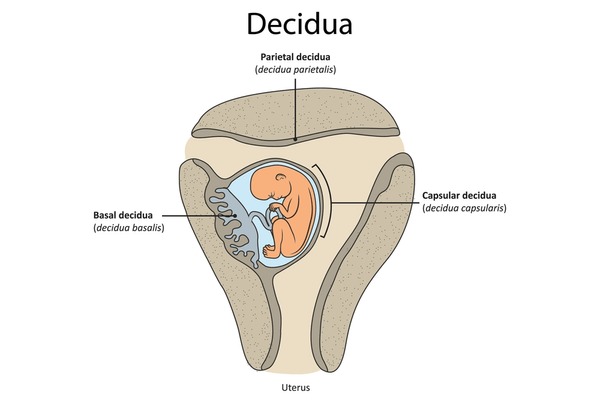
What is the role of the decidua basalis?
It lies under the embryo and attaches to the chorionic villi, forming the maternal portion of the placenta.
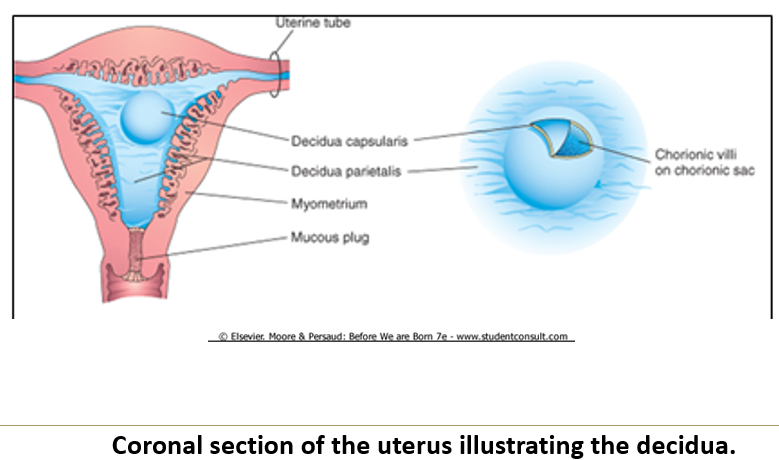
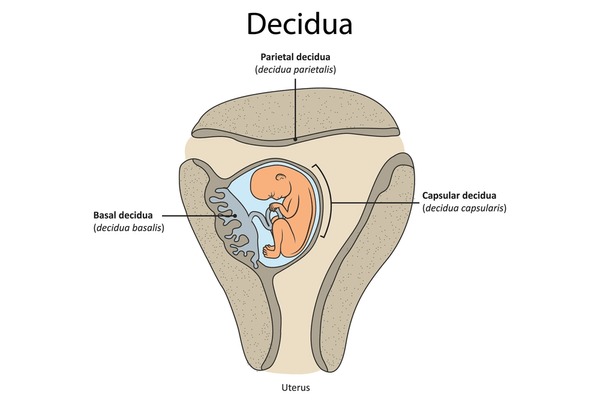
What happens to the decidua capsularis?
It covers the embryo
It becomes stretched, and degenerates when compressed between the chorion and decidua parietalis.
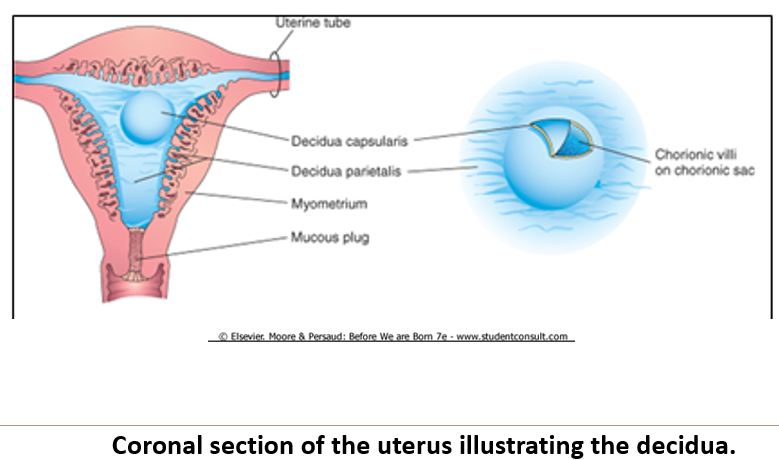
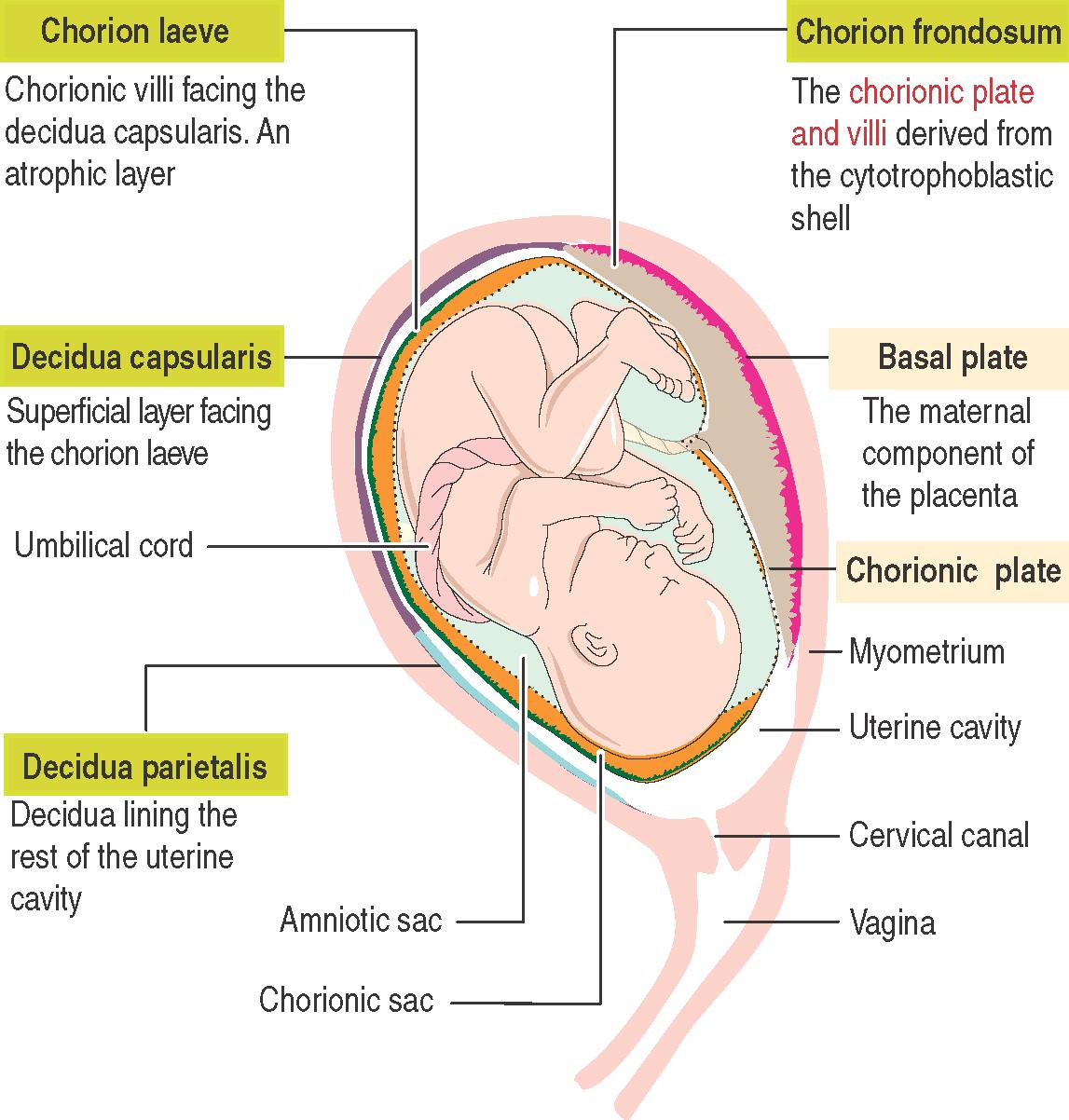
What is the decidua parietalis?
It includes all remaining parts of the decidua
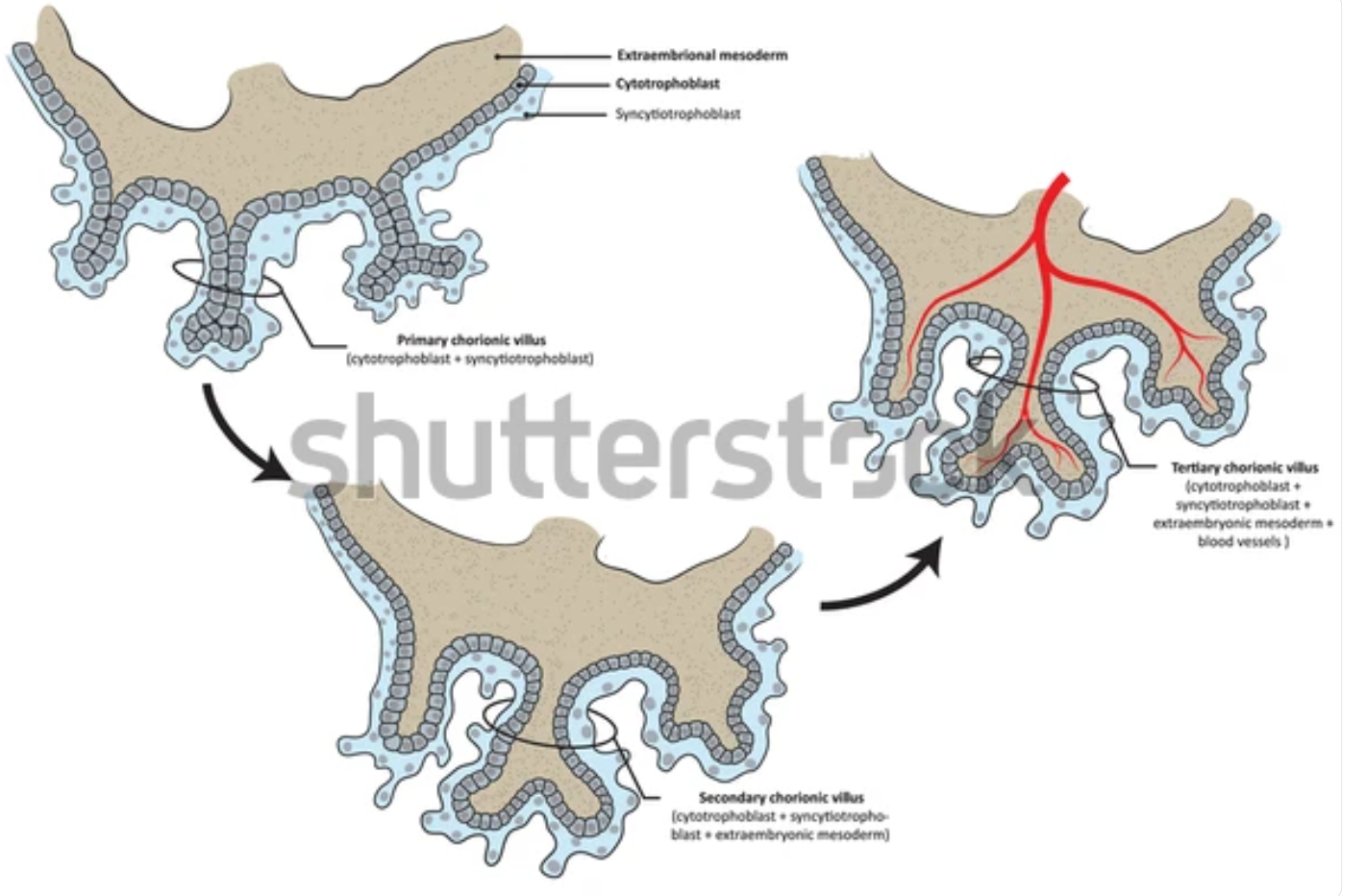
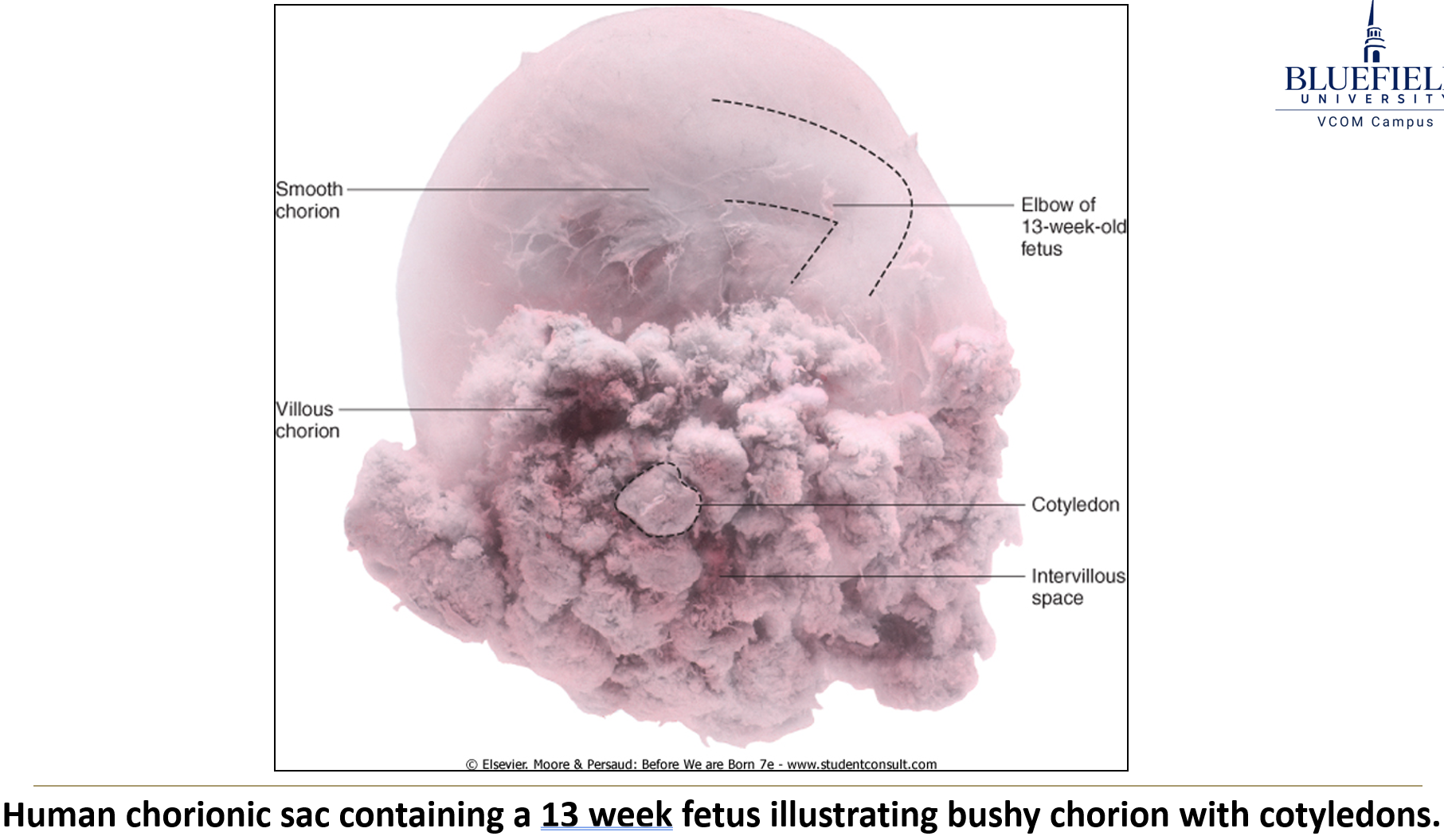
When do tertiary villi cover the entire surface of the chorionic sac?
By the beginning of week 8, tertiary villi cover the entire surface of the chorionic sac.
What is the difference between smooth and bushy chorion?
Villous chorion or “bushy chorion”: area with chorionic villi; becomes the placenta.
Smooth chorion: part where villi degenerate. It degenerates because the areas of the chorion not in contact with the decidua basalis receive poor vascular support, leading to villous atrophy and the formation of the smooth chorion
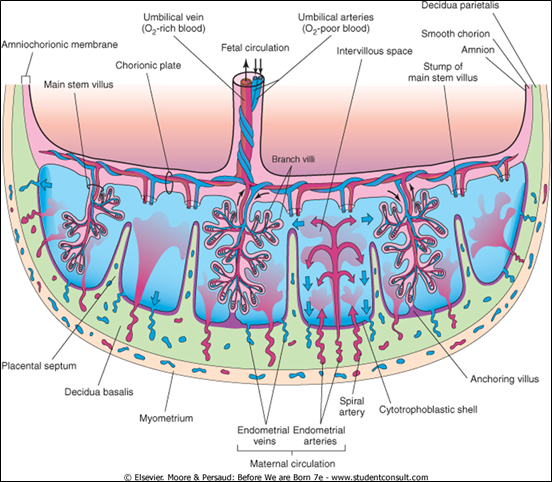
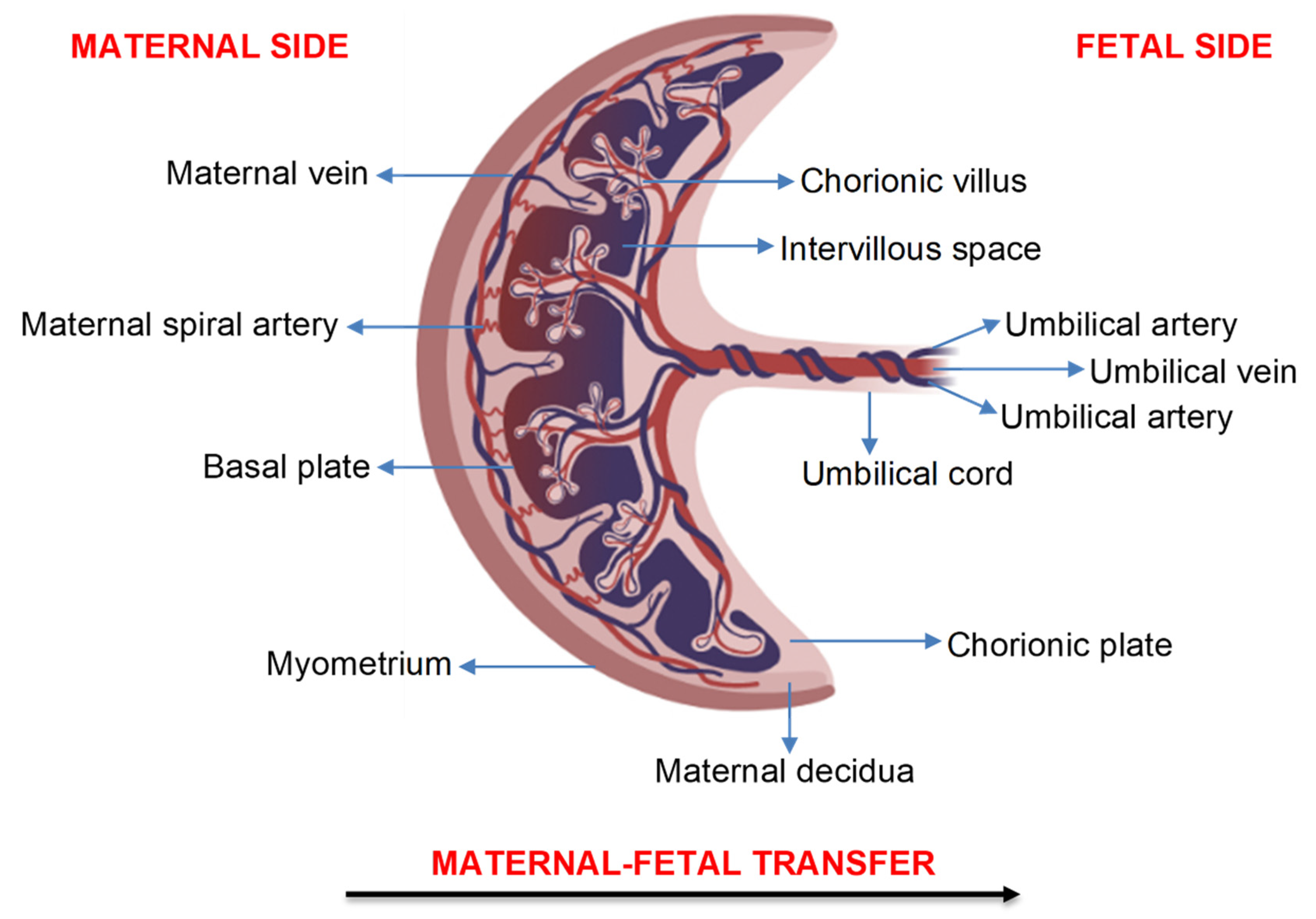
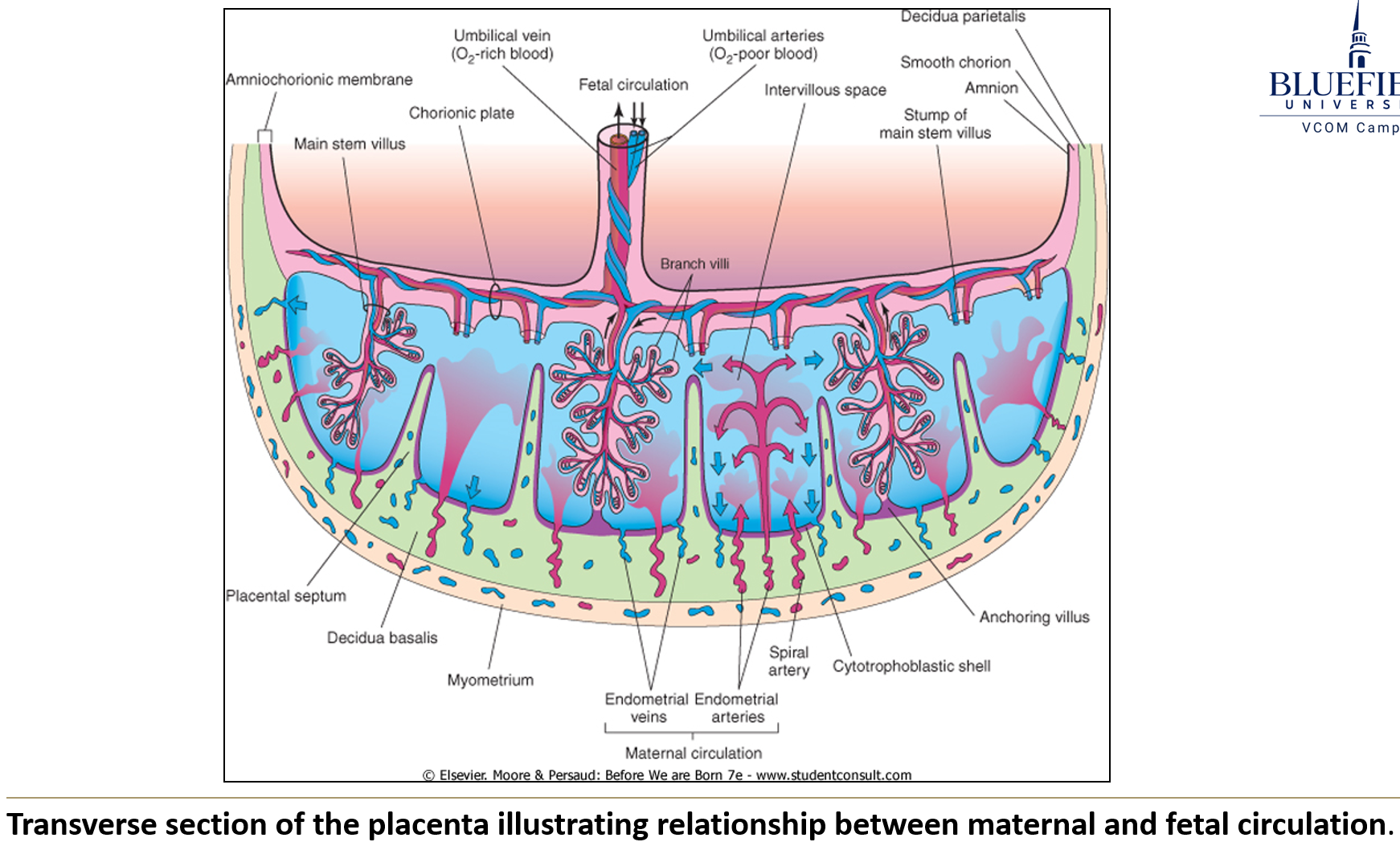
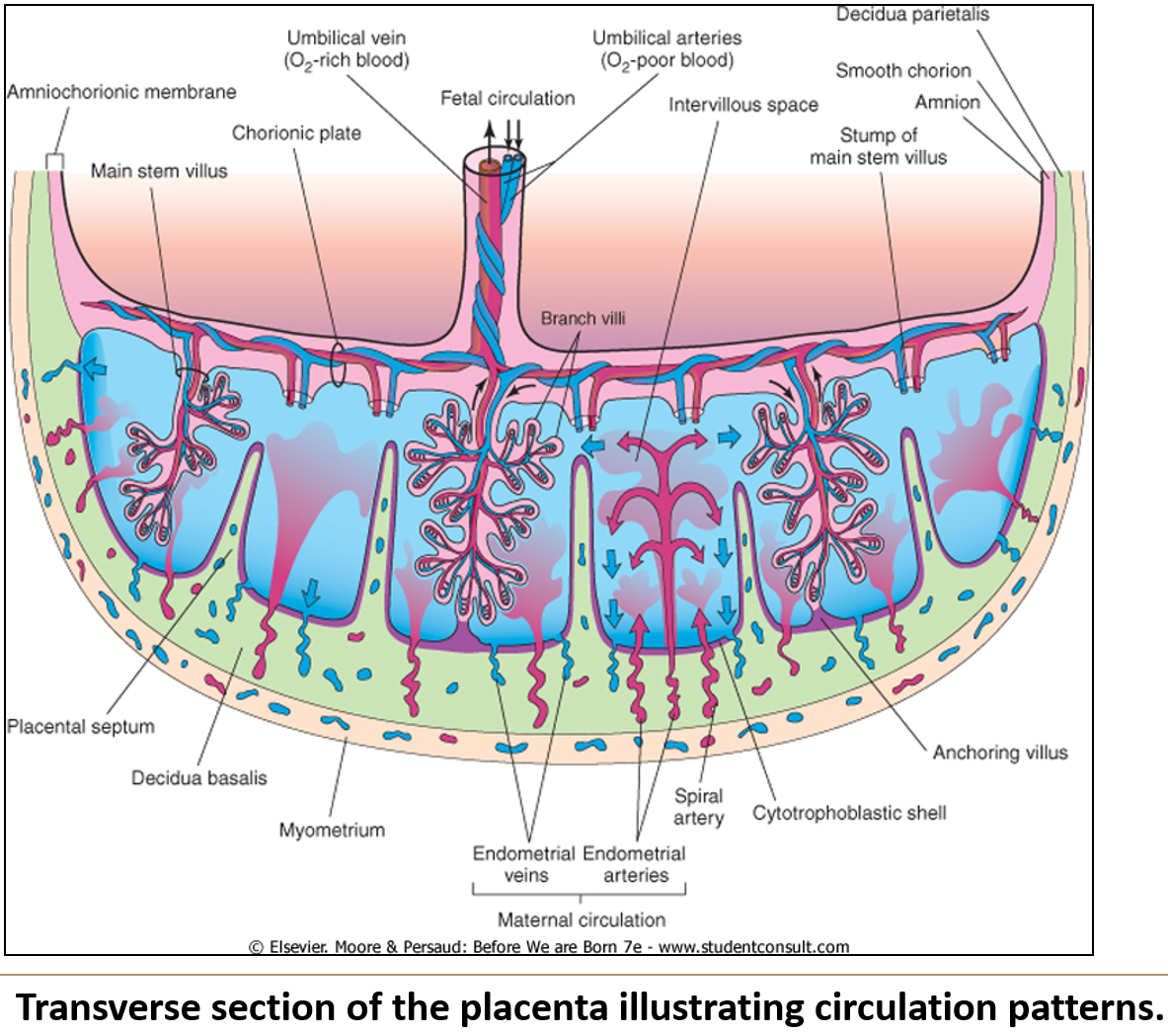
How do lacunar or intervillus spaces form during week 3?
The cytotrophoblast forms a shell separating the embryo from uterine tissue.
The syncytiotrophoblast degenerates, creating maternal blood sinuses.
Uterine blood vessels penetrate the cytotrophoblast, and maternal blood empties into intervillous spaces.
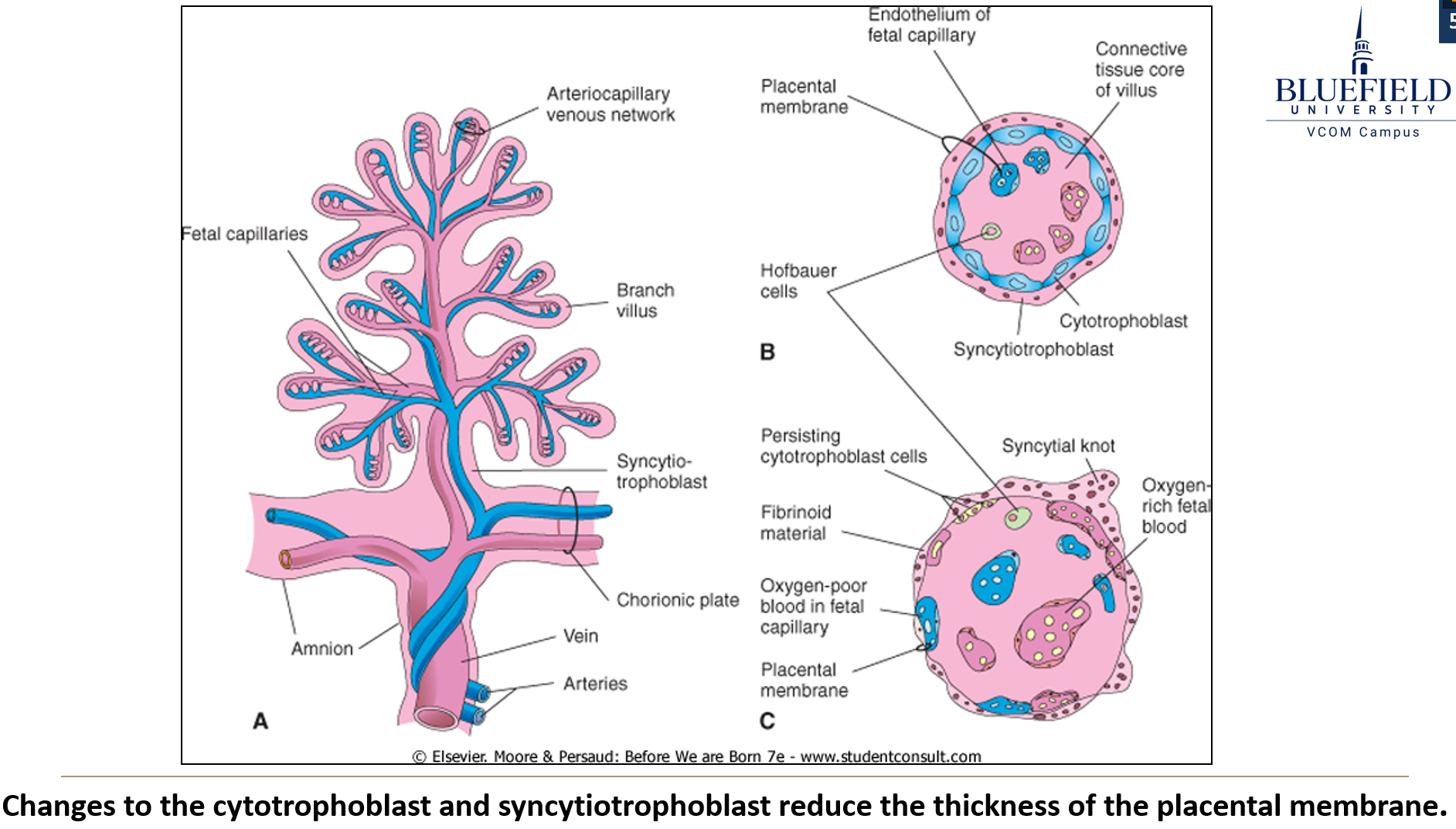
What changes affect the villi after week 8?
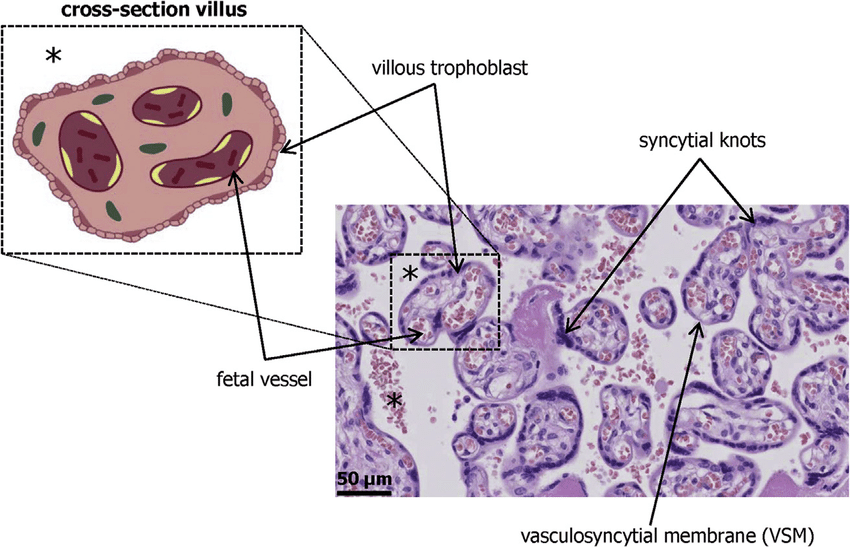
Cytotrophoblast around villi thins, becomes connective tissue, and largely disappears.
The syncytiotrophoblast fragments, with parts falling into intervillous blood as syncytial knots, which degrade without issues.
Fetal blood vessels are now in closer contact with maternal blood.
Growth of villi and decidua leads to placental septum formation and cotyledons.
What are syncytial knots and their clinical significance?
Fragments of syncytiotrophoblast that enter maternal circulation and degenerate safely; they are being explored for noninvasive fetal DNA testing.
What types of substances cross the placenta?
Wastes – urea, ammonia, CO₂
Antibodies – especially maternal IgG
Nutrients – all nutrients and oxygen
Teratogens
Microorganisms – many viruses, tuberculosis, syphilis, Toxoplasma gondii
Hormones
Drugs – illicit, prescription, and OTC drugs
Mnemonic: want my hot dog (Wastes, Antibodies, Nutrients, Teratogens, Microorganisms, Hormones, Drugs)
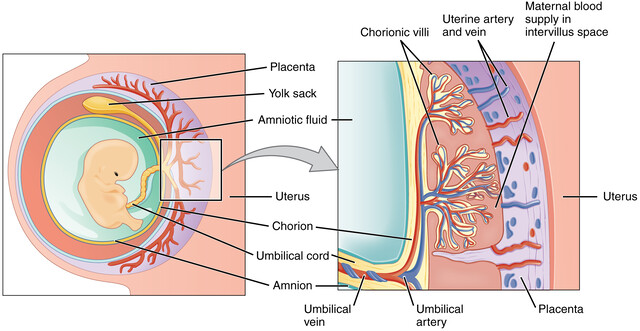
How does circulation in the placenta work?
Low-oxygen blood enters the placenta through umbilical arteries into the chorionic plate.
These arteries exit the plate and branch into capillaries of cotyledons.
Oxygen-rich, nutrient-rich blood then exits the placenta to the fetus via the umbilical vein.
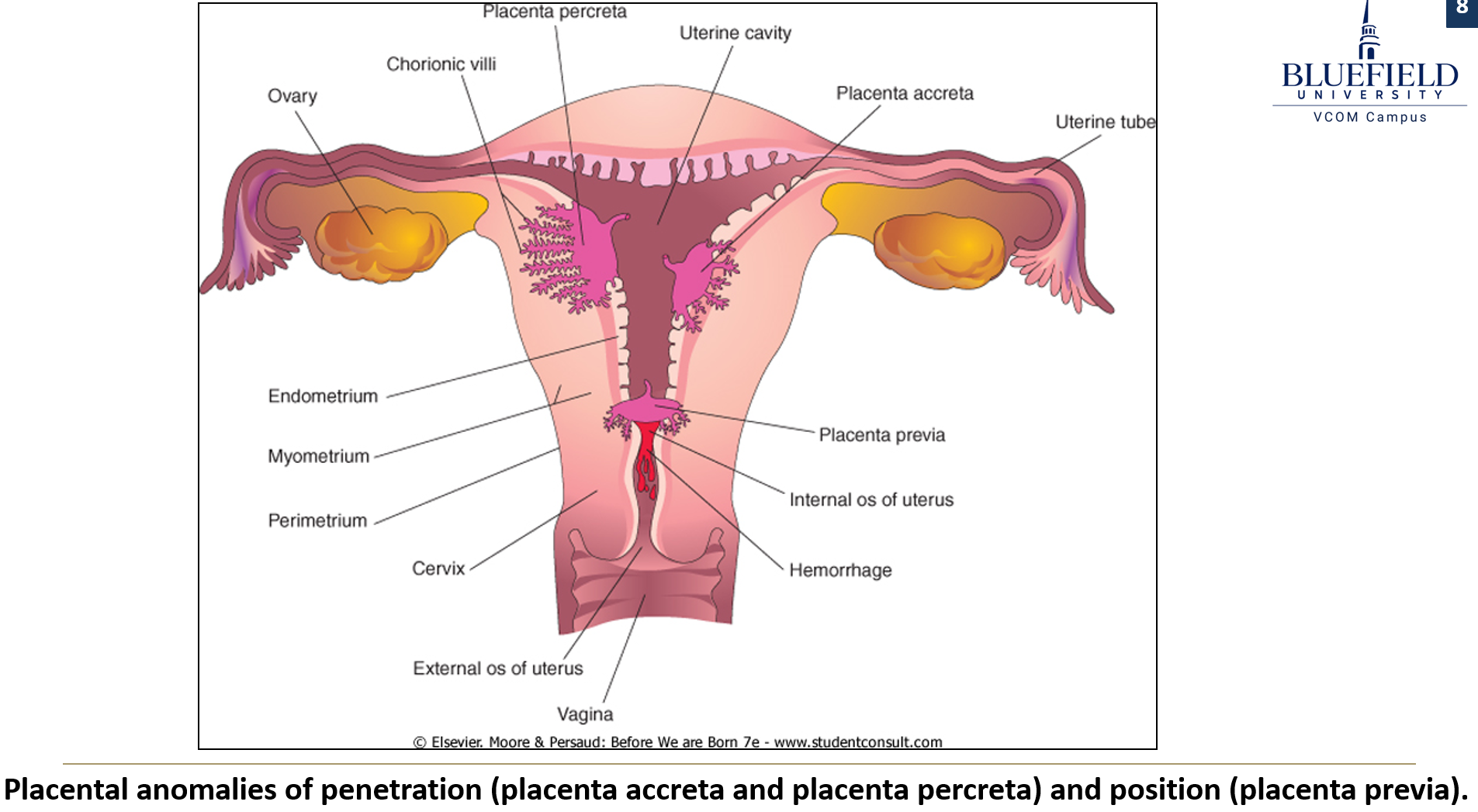
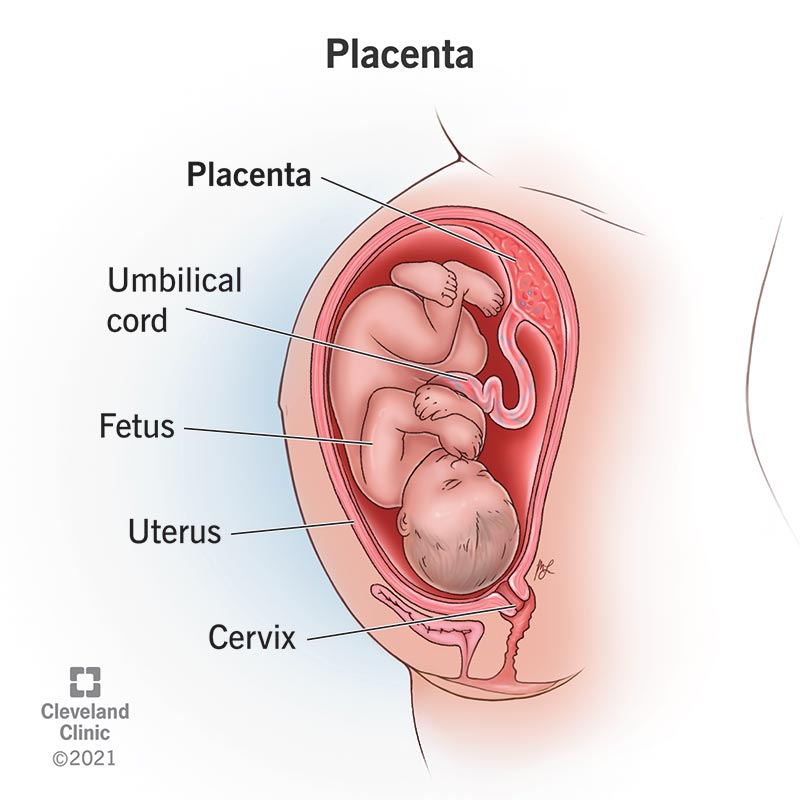
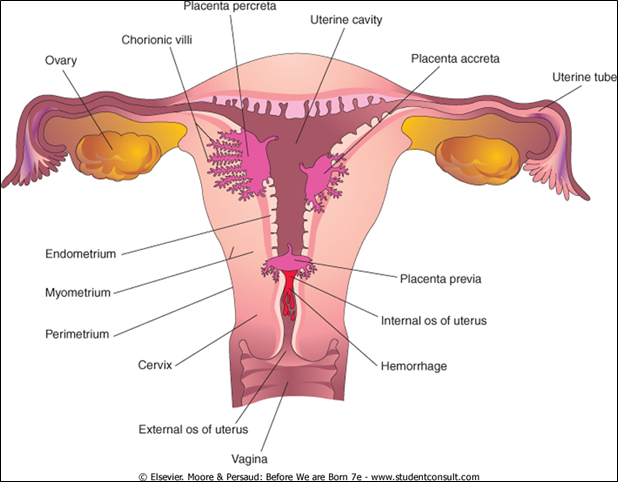
What is placenta accreta and how does it differ from placenta percreta?
Placenta accreta: villi penetrate the myometrium.
Placenta percreta: villi penetrate the entire thickness of the uterine wall.
Both can cause bleeding in the 3rd trimester and hemorrhage if the placenta fails to detach at birth.
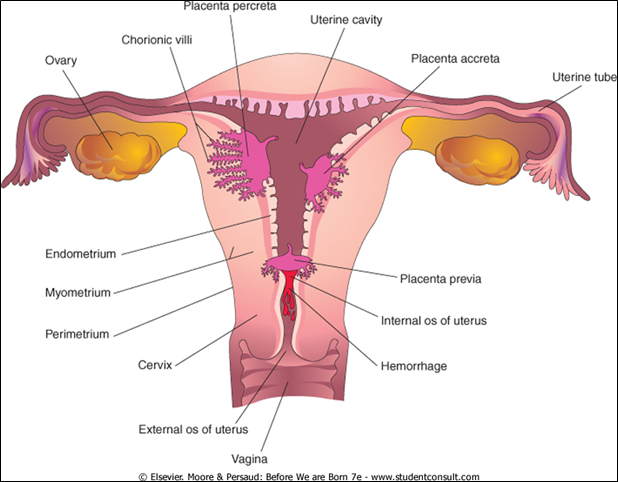
What is placenta previa?
Occurs when the placenta covers the internal cervical os, leading to third-trimester bleeding and often requiring a Cesarean section.
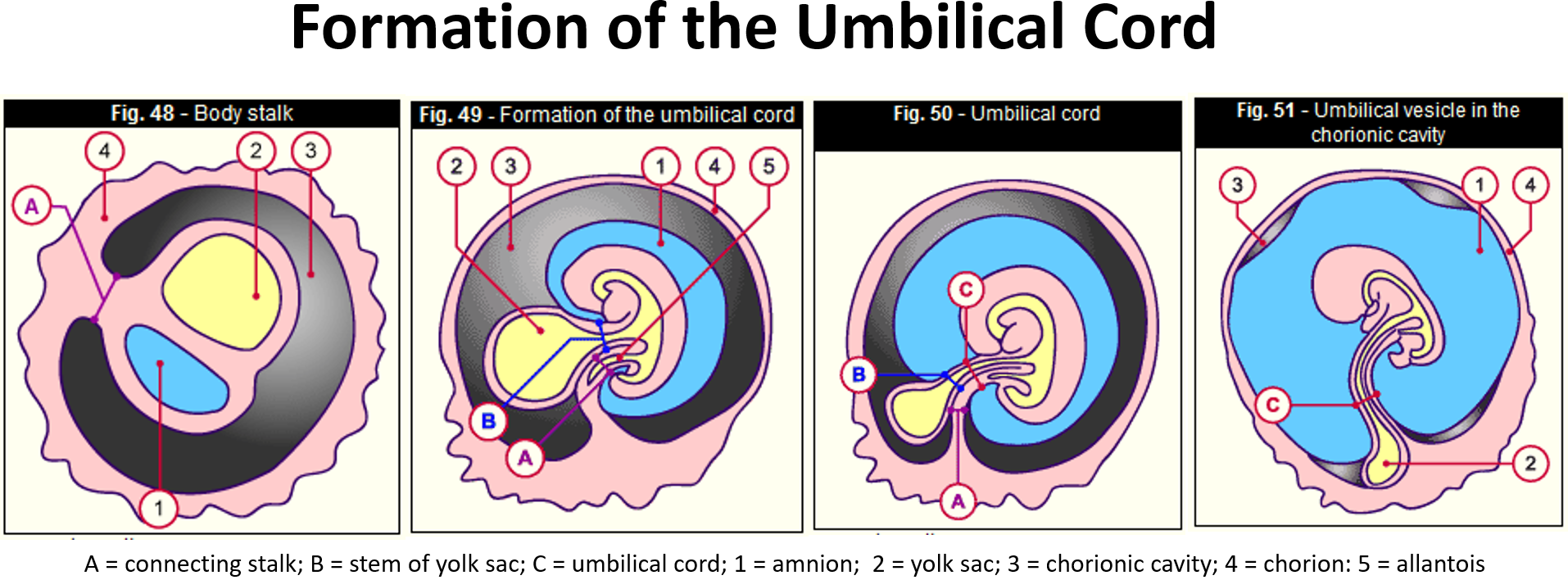
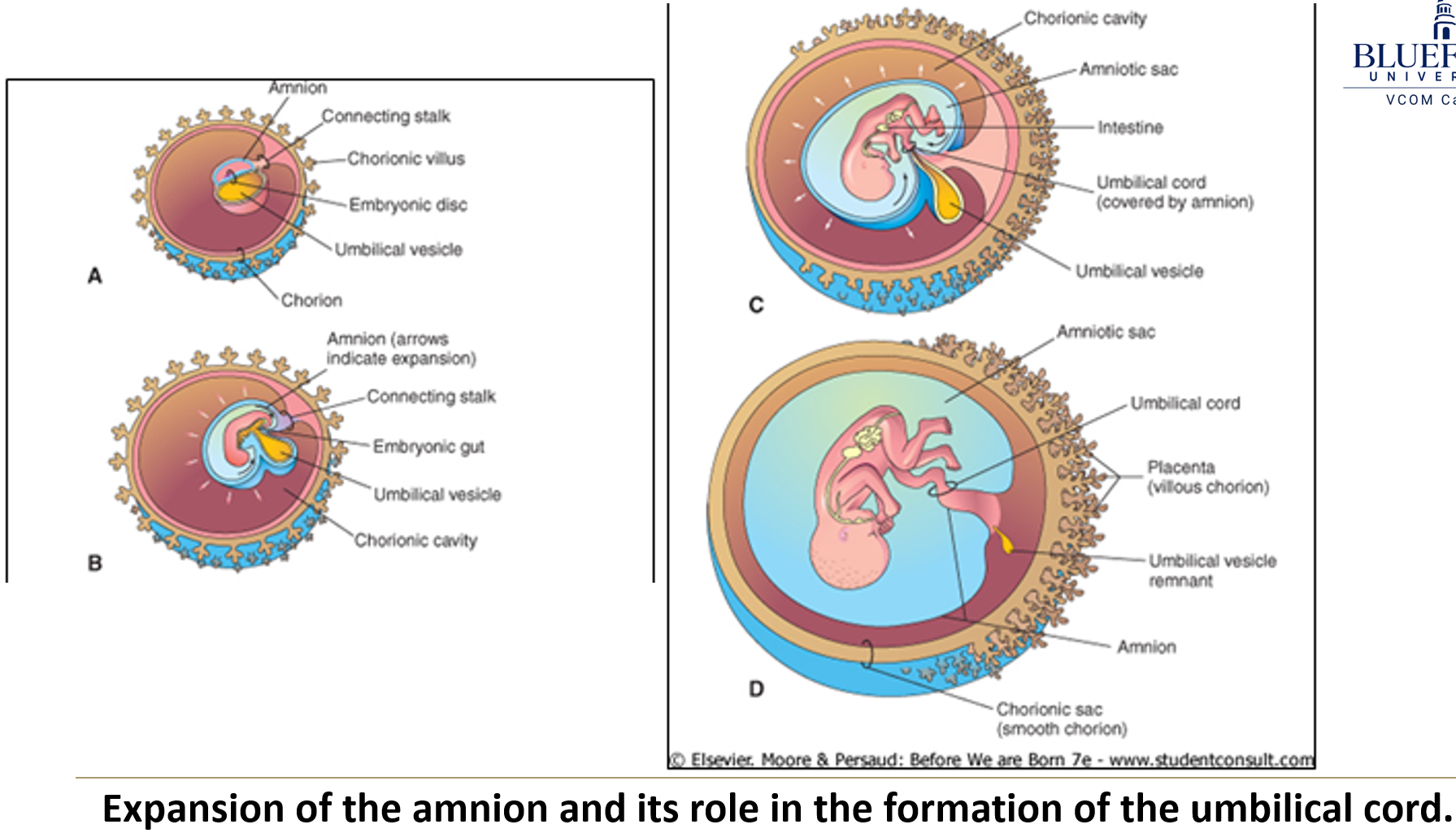
What is the composition of the primitive umbilical ring at week 5?
The connecting stalk, which contains the allantois and umbilical vessels
The vitelline duct with the vitelline artery and vein
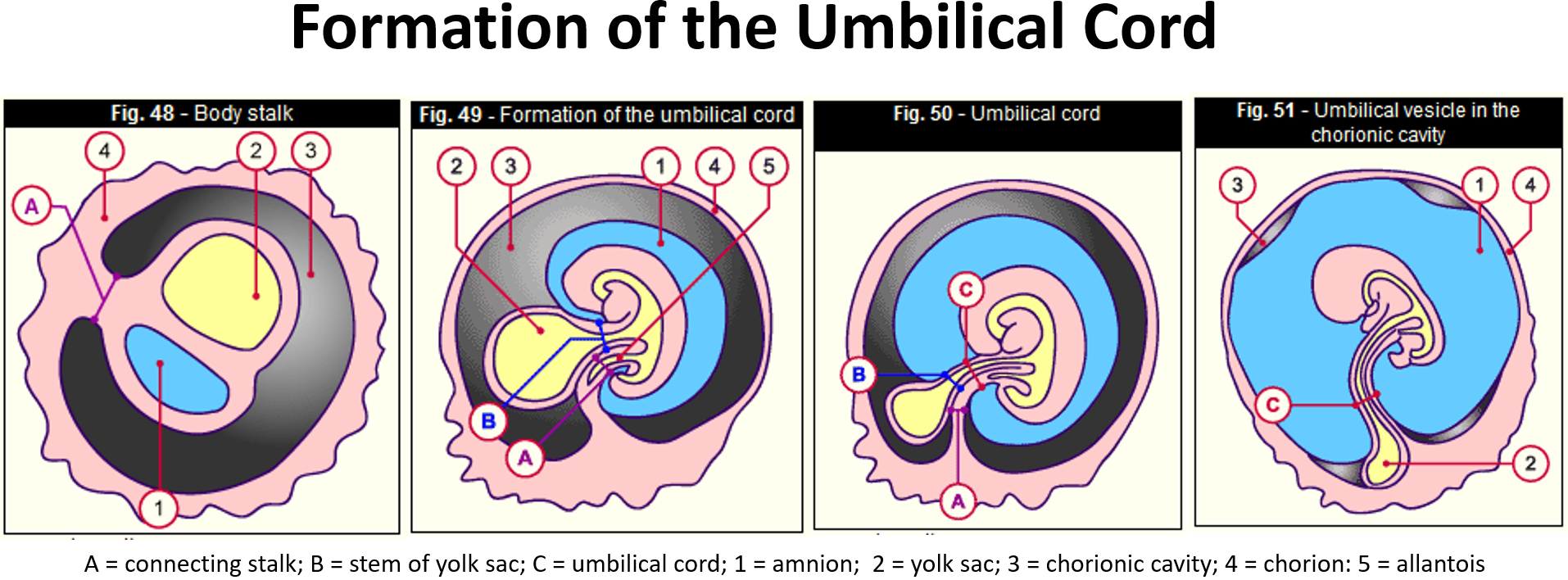
What happens as development of the primitive umbilical cord progresses?
The yolk sac and vitelline duct with associated vessels are obliterated by compression.
What structures are found in the mature umbilical cord?
It contains 2 umbilical arteries and 1 umbilical vein, all embedded in Wharton’s jelly (a primitive connective tissue).
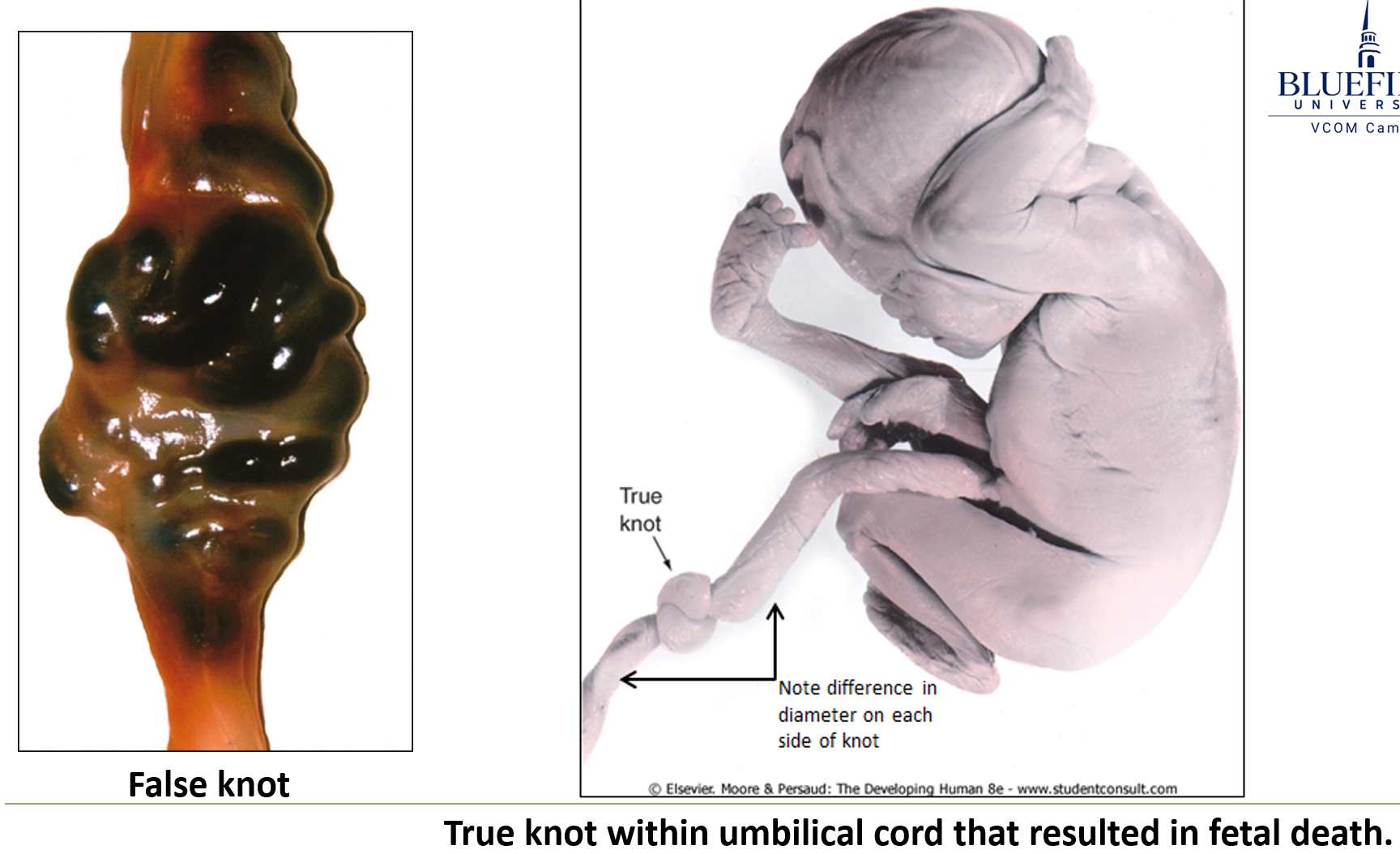
What are false knots in the umbilical cord?
They are caused by vessels being longer than the cord, making it look knotted without actual twisting.
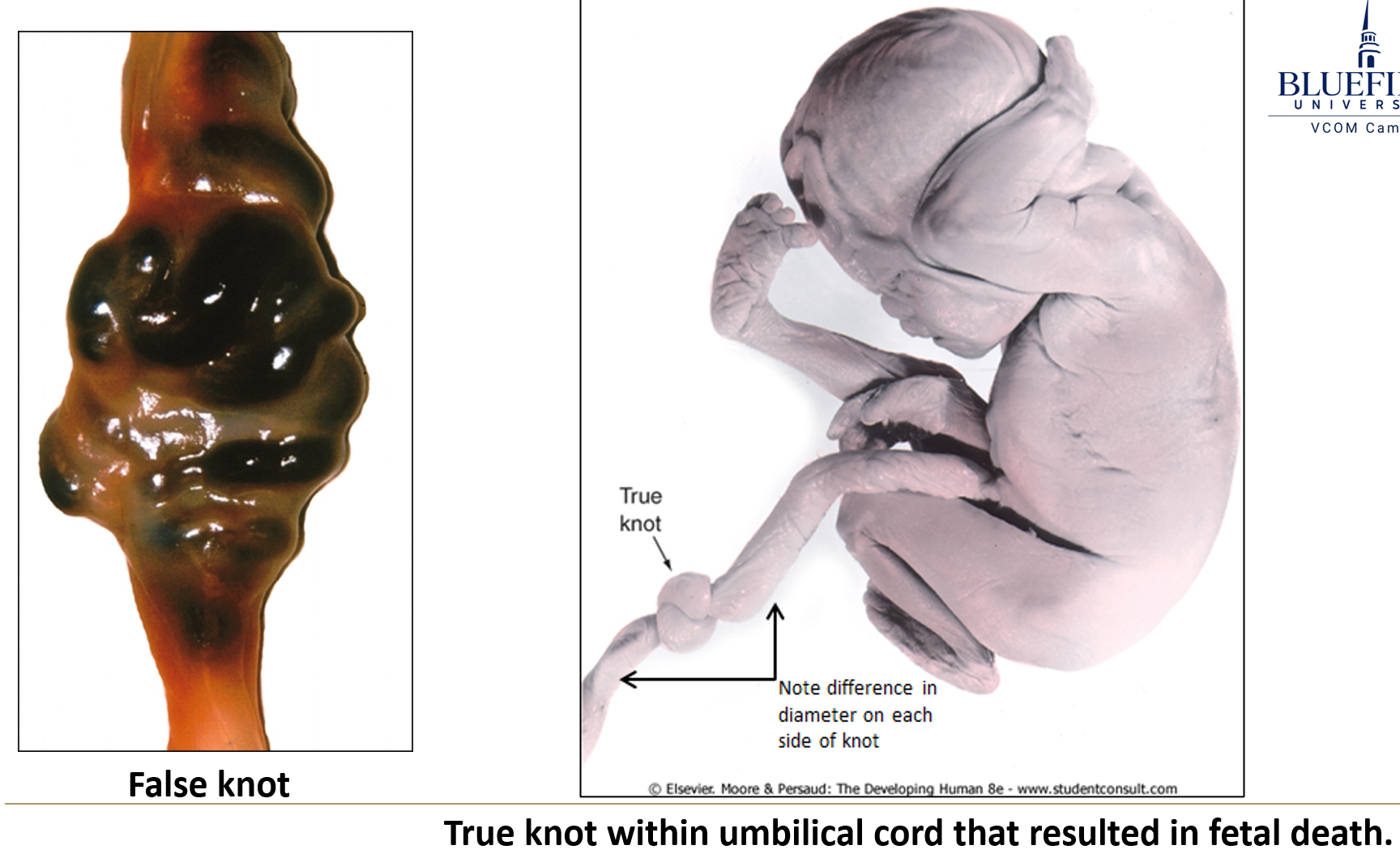
What risks are associated with an abnormal cord length?
If too short, the cord may detach the placenta before birth.
If too long, it may:
Form true knots, diminishing circulation
Wrap tightly around limbs, impairing blood flow and development
Where does the umbilical cord typically insert?
At the center of the placenta.
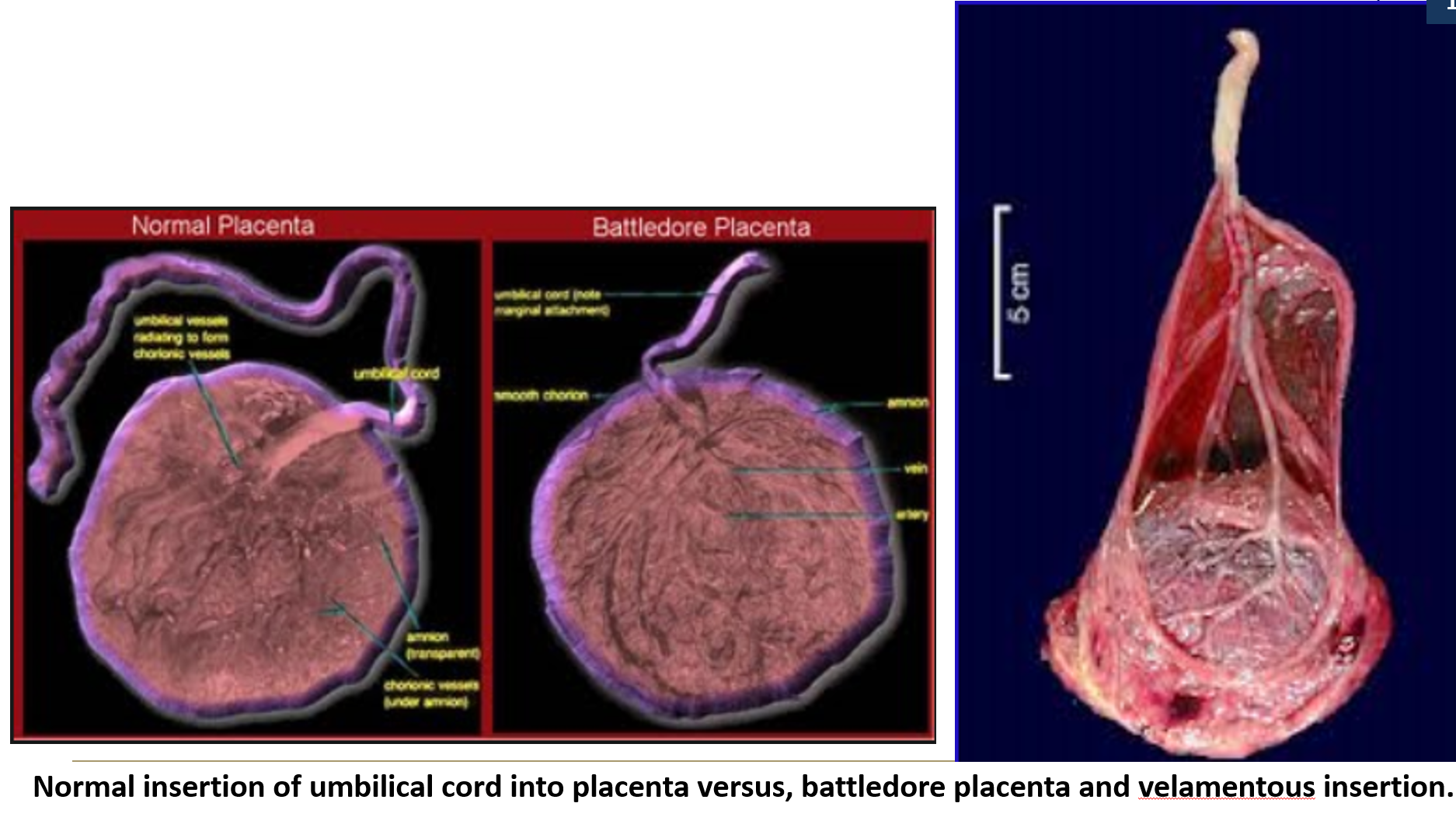
What are abnormal insertion types of the umbilical cord?
Battledore placenta: insertion at the edge of the placenta
Velamentous insertion: insertion into fetal membranes, with vessels exposed between amnion and chorion, making them easily torn.
What is the amnion and what does it form?
The amnion forms the amniotic sac, a fluid-filled cavity that surrounds the fetus.
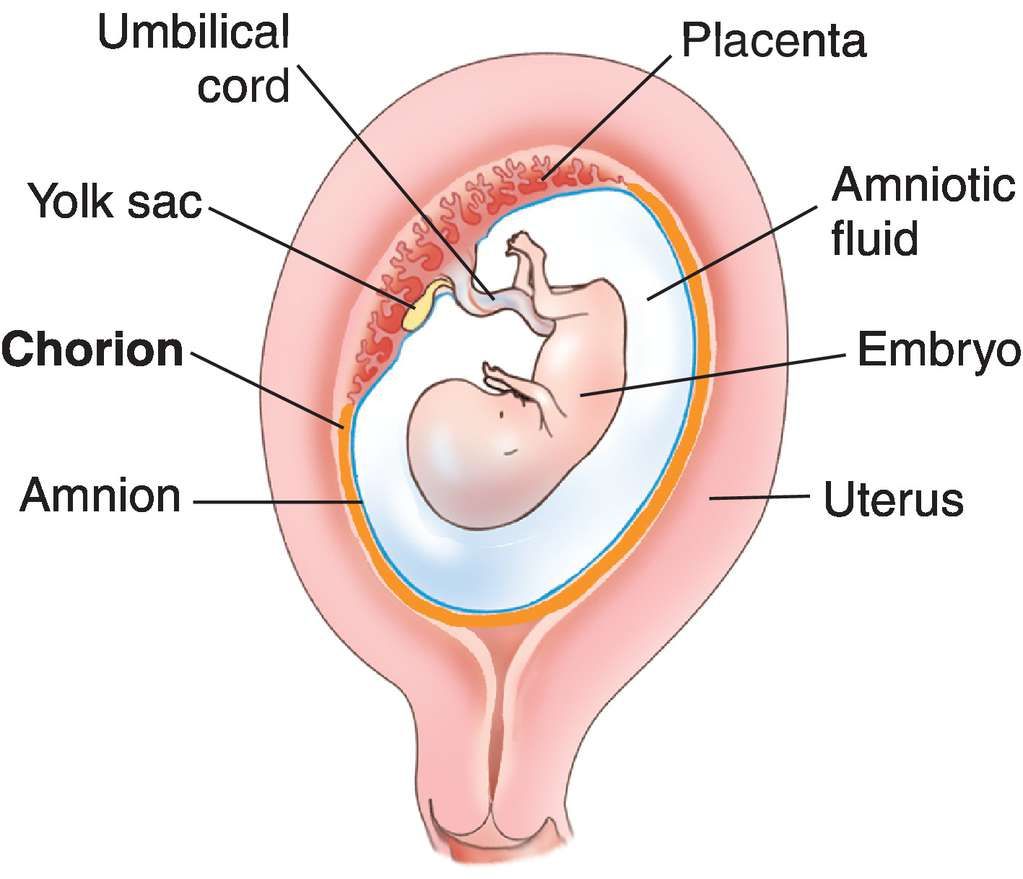
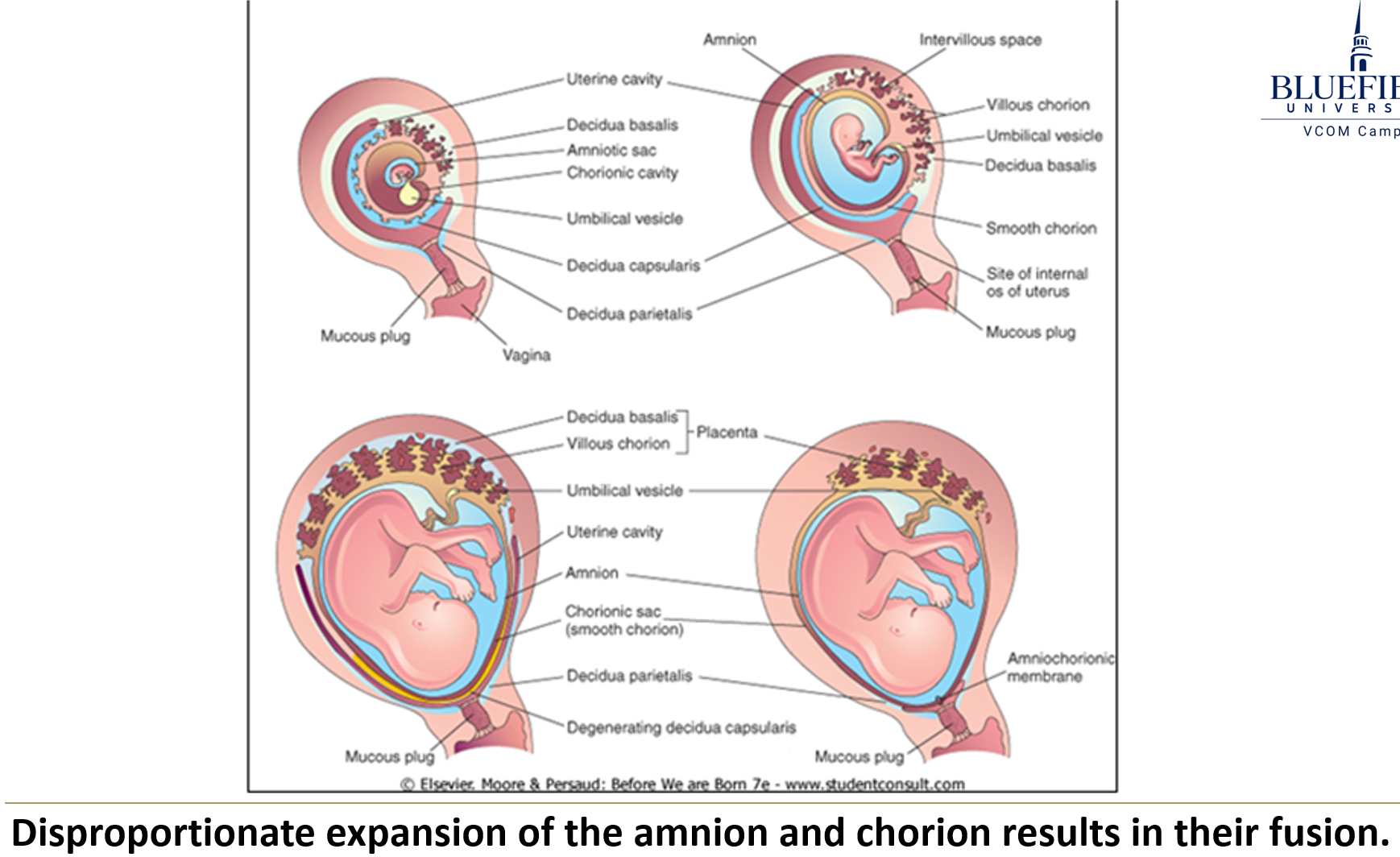
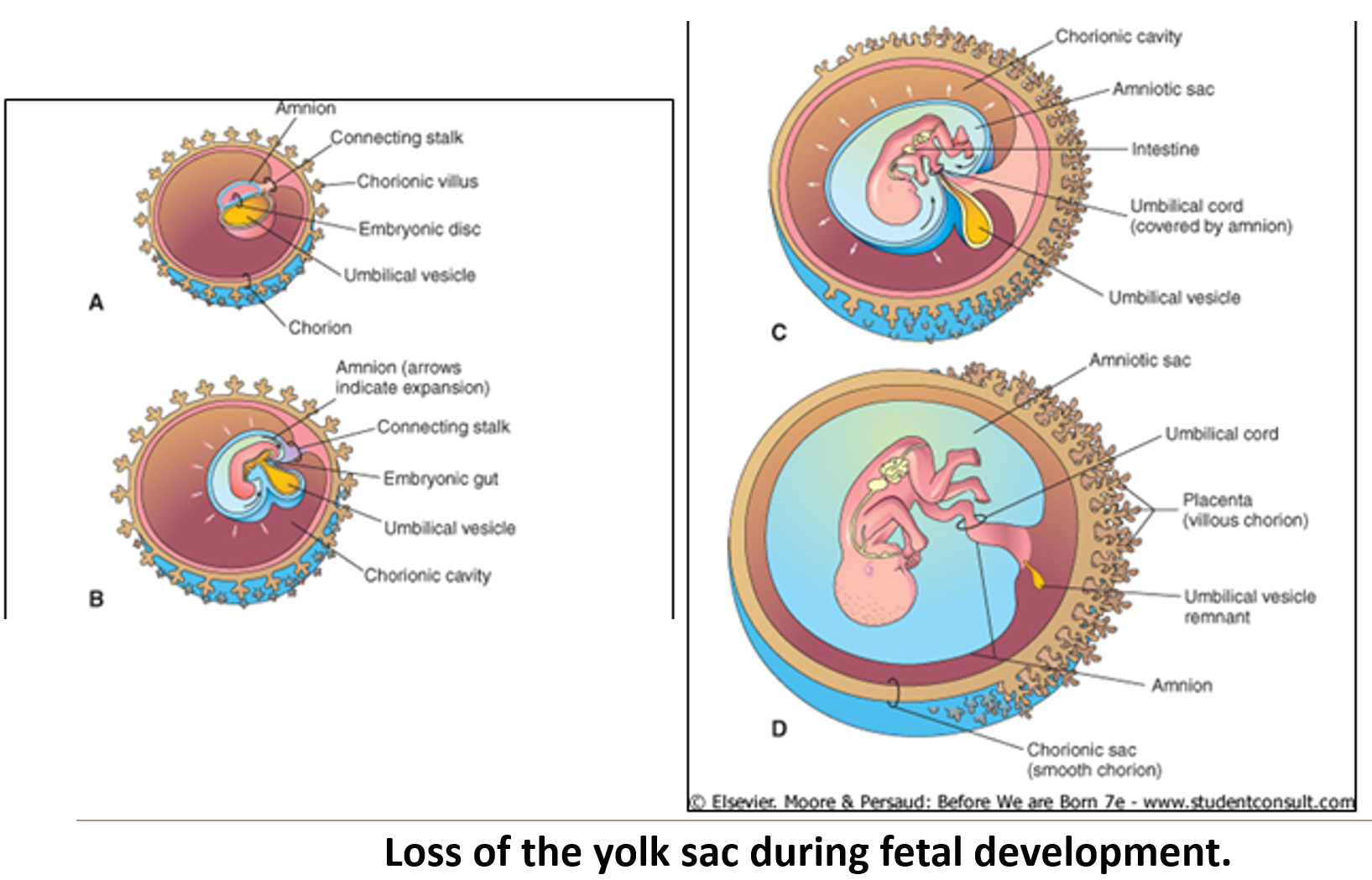
What occurs during the rapid expansion of the amniotic cavity (weeks 10–20)?
It obliterates the yolk sac and chorionic cavity, forming the amniochorionic membrane.
The amniotic membrane also provides the outer epithelial covering of the umbilical cord.
This compression obliterates the vitelline duct and associated vessels.
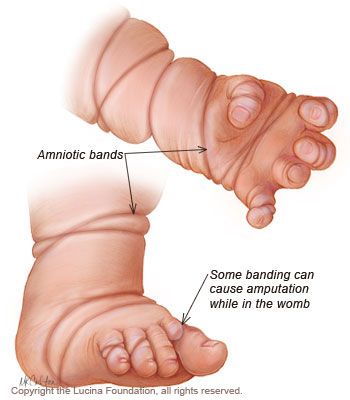
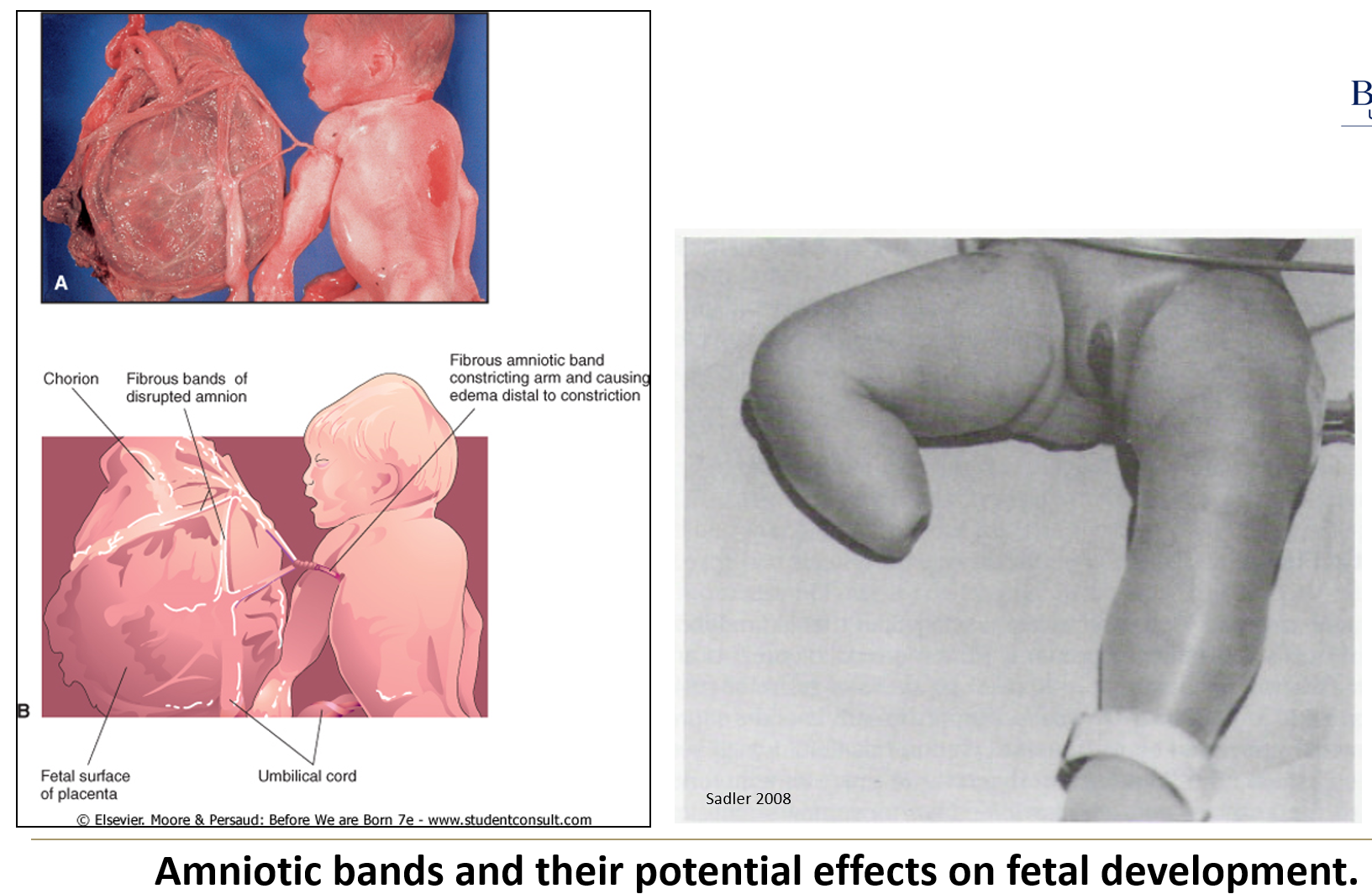
What are amniotic bands and how do they form?
They result from tears in the amnion, often due to infection or toxic insult.
These bands may encircle fetal extremities or head, leading to amputations, ring constrictions, or craniofacial abnormalities.
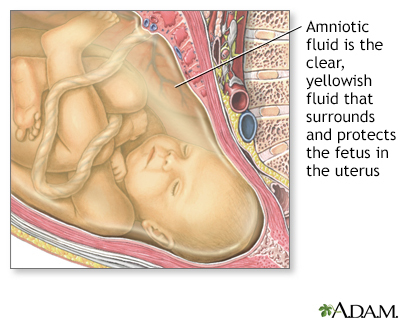
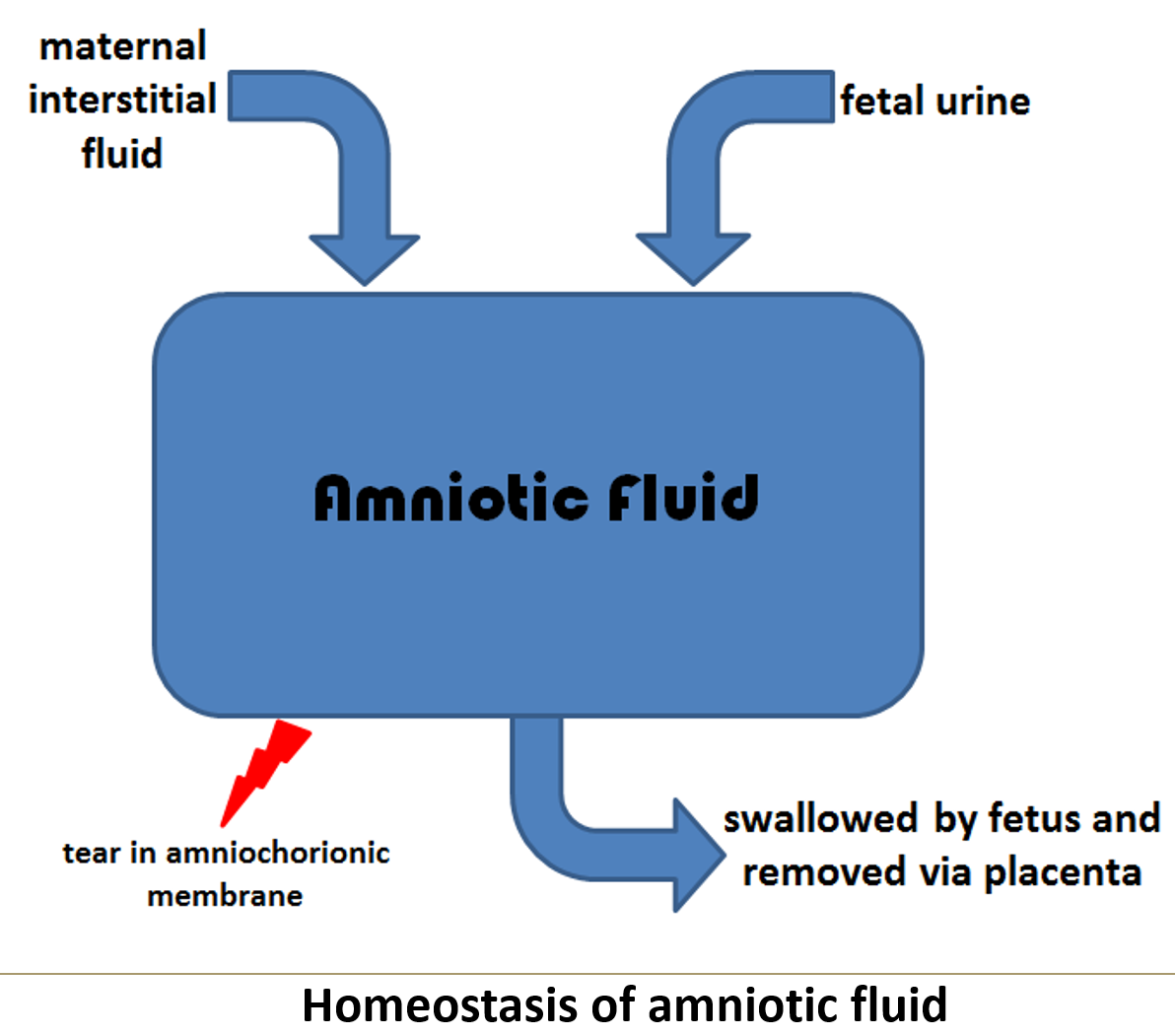
What is amniotic fluid mostly composed of?
Primarily maternal interstitial fluid, with minor contributions from amniotic cells.
What are the early developmental functions of amniotic fluid?
Absorbs shocks
Maintains constant temperature
Allows fetal movement, promoting bone and muscle development
Before skin keratinizes, it exchanges with fetal tissues to balance fetal fluid composition
Provides space for fetal growth
Maintains a sterile environment
What changes occur in the amniotic fluid by the 5th month?
The fetus starts to urinate into the amniotic fluid, which is normal. The urine is mostly water, and waste products are removed by the placenta into the mother's bloodstream.
The fetus also swallows the amniotic fluid, which helps with the development of its digestive system and allows some waste products to be reabsorbed and transferred to the mother.

What is meconium?
Fetal excrement found in amniotic fluid, typically present in very late pregnancy.
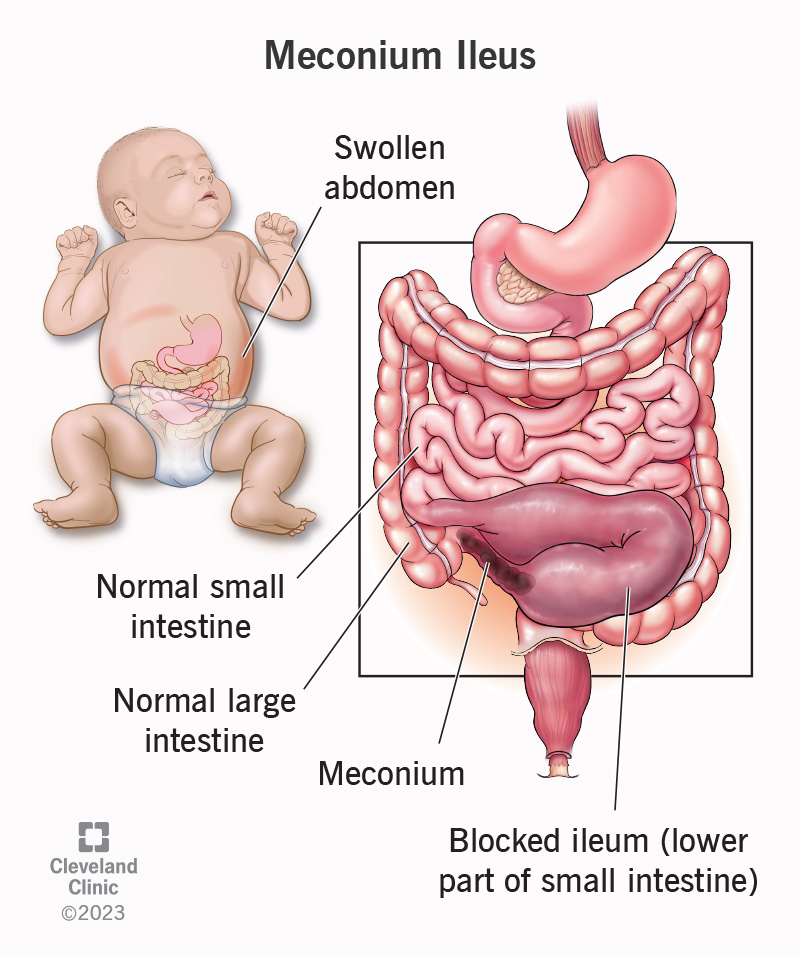
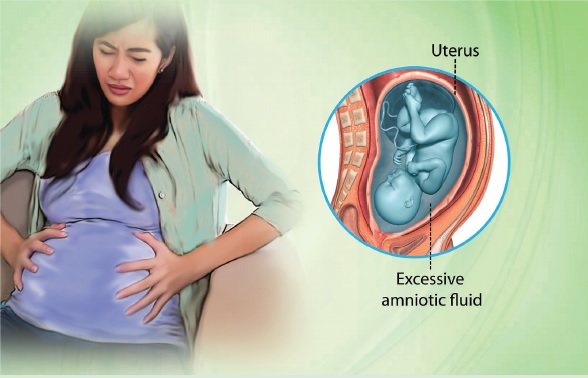
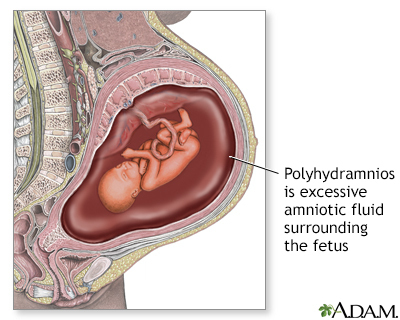
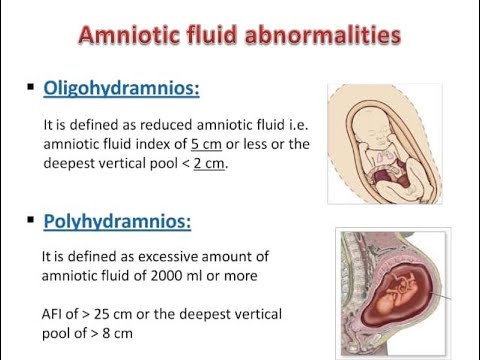
What is polyhydramnios and what causes it?
Polyhydramnios is excessive amniotic fluid, commonly caused by:
Birth defects involving the GI or CNS that impair fetal swallowing (most common)
Maternal diabetes
Idiopathic causes
What is oligohydramnios and what causes it?
Oligohydramnios is too little amniotic fluid, caused by:
Placental insufficiency, lack of fetal urine, or rupture of the amniochorionic membrane
It may lead to fetal compression (causing developmental problems) or compression of the umbilical cord.
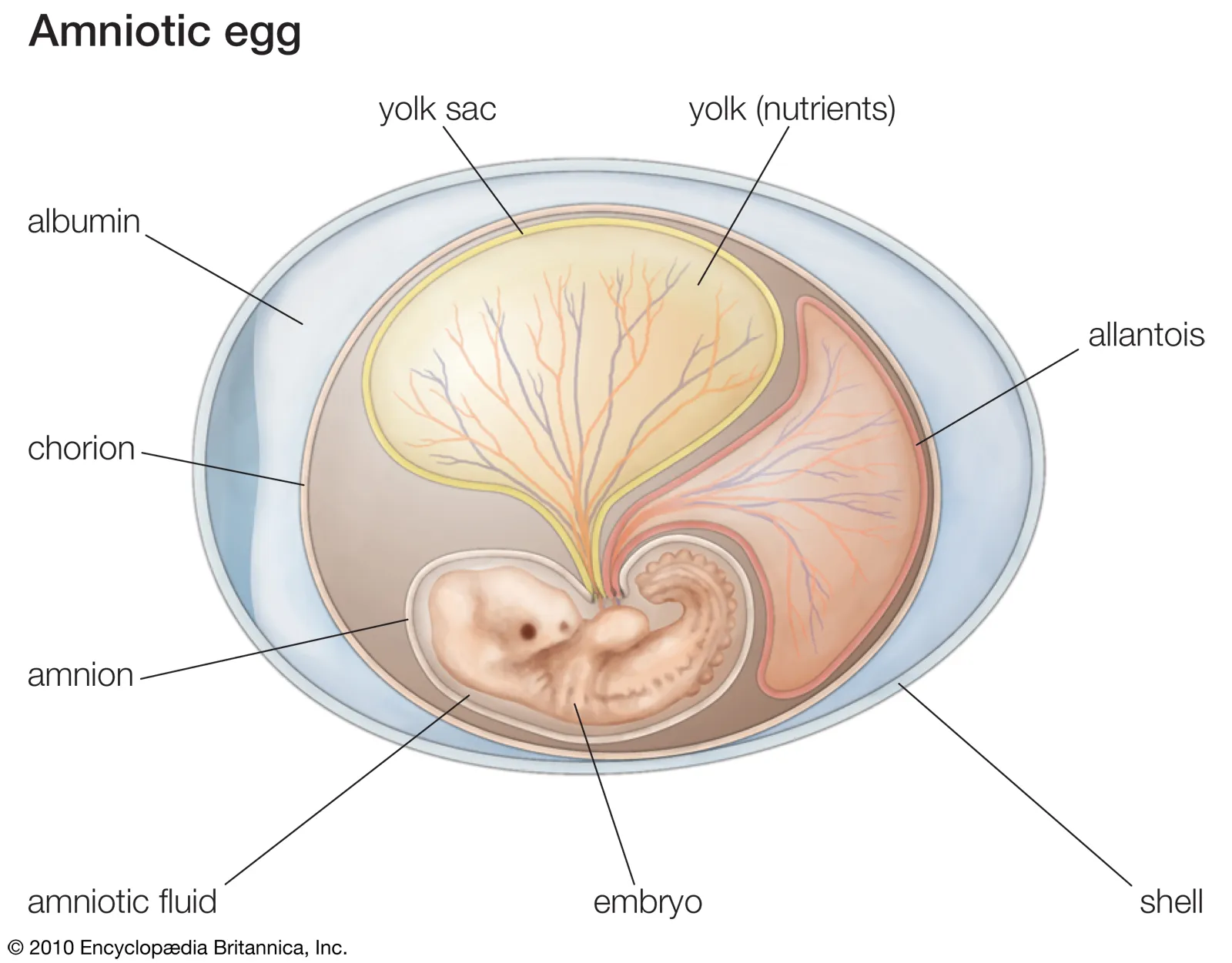
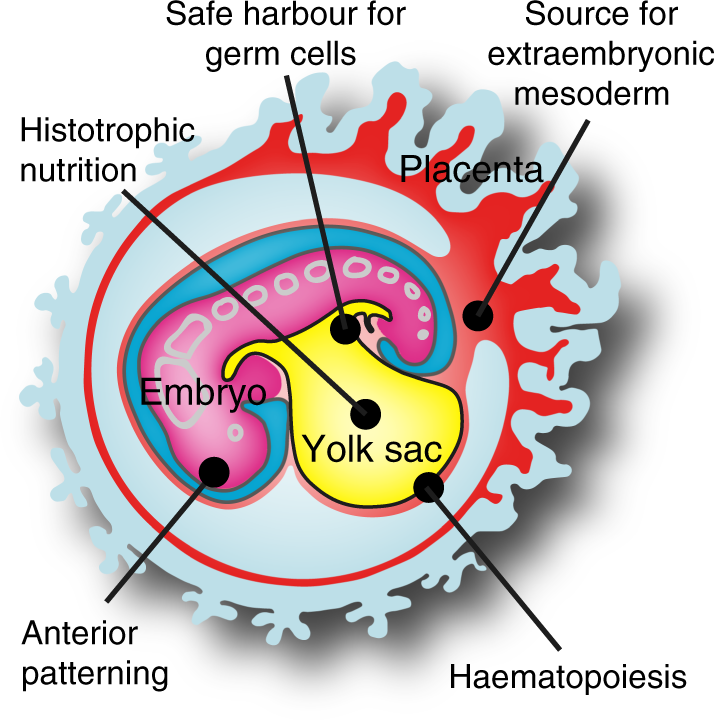
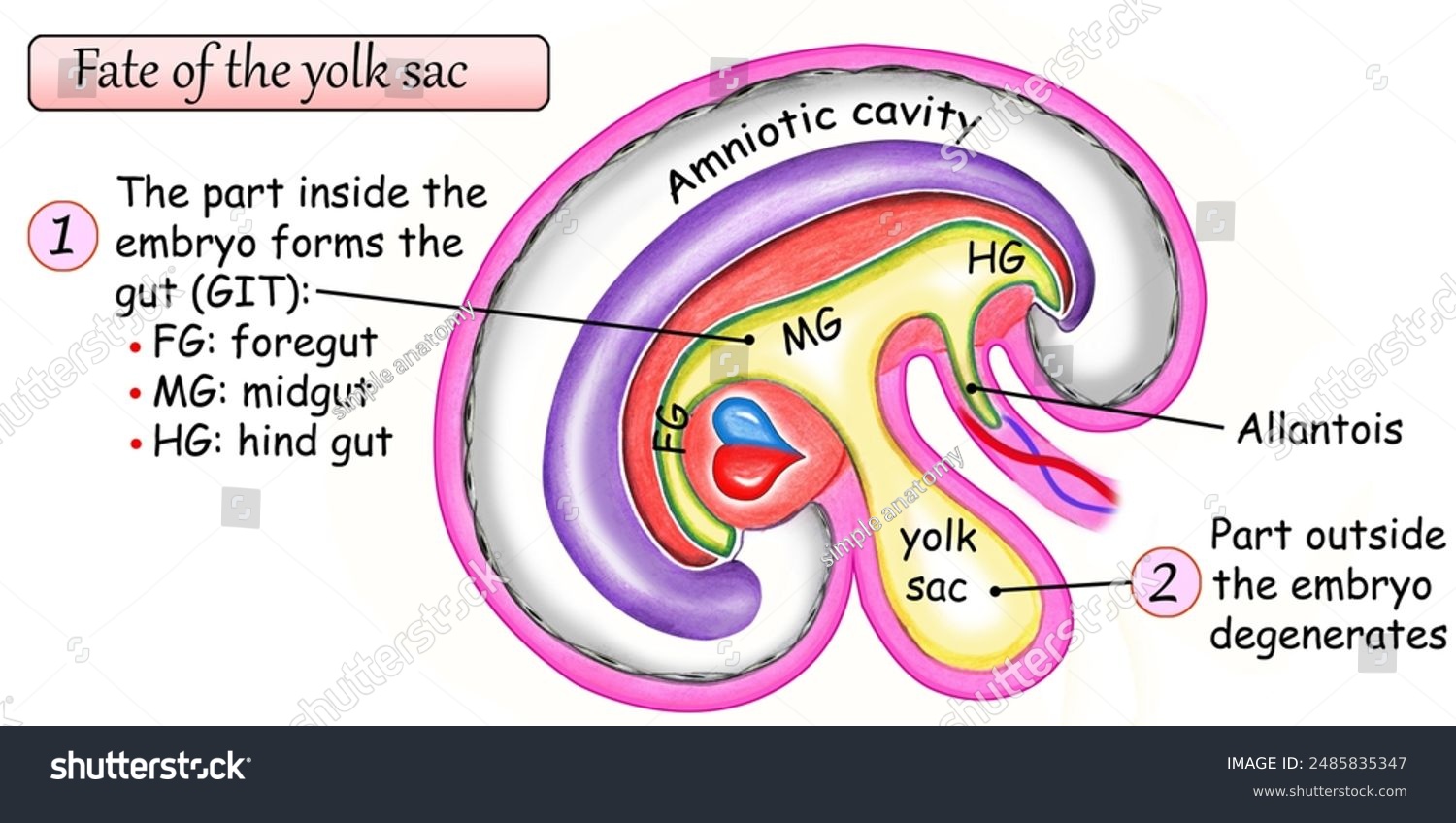
What is the yolk sac and where is it located?
The largest component of the conceptus in early development.
It lies between the amnion and chorion, and is later obliterated by the expanding amnion, leaving nonfunctional remnants.
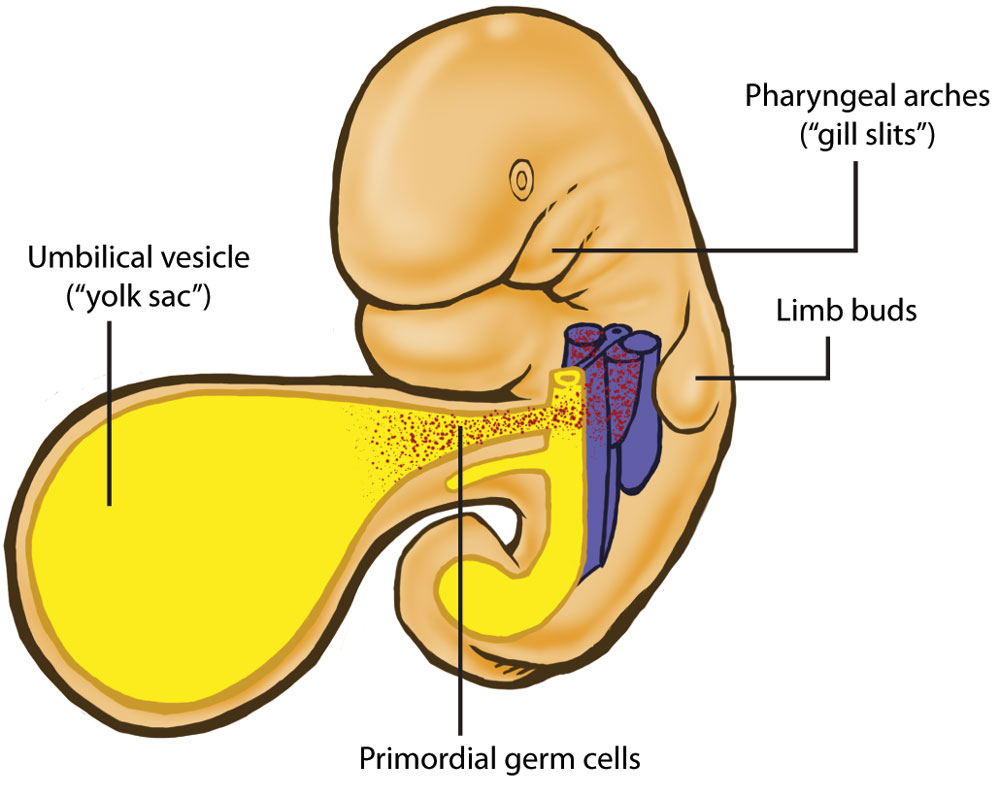
What are the main functions of the yolk sac?
Nutritional source during weeks 3–4
First site of hemopoiesis (blood cell formation)
Becomes part of the midgut in week 4; its endoderm gives rise to respiratory and digestive epithelia
Site of primordial germ cell development
What is the allantois and how does it develop?
A diverticulum (small pouch) off the yolk sac, extending into the connecting stalk.
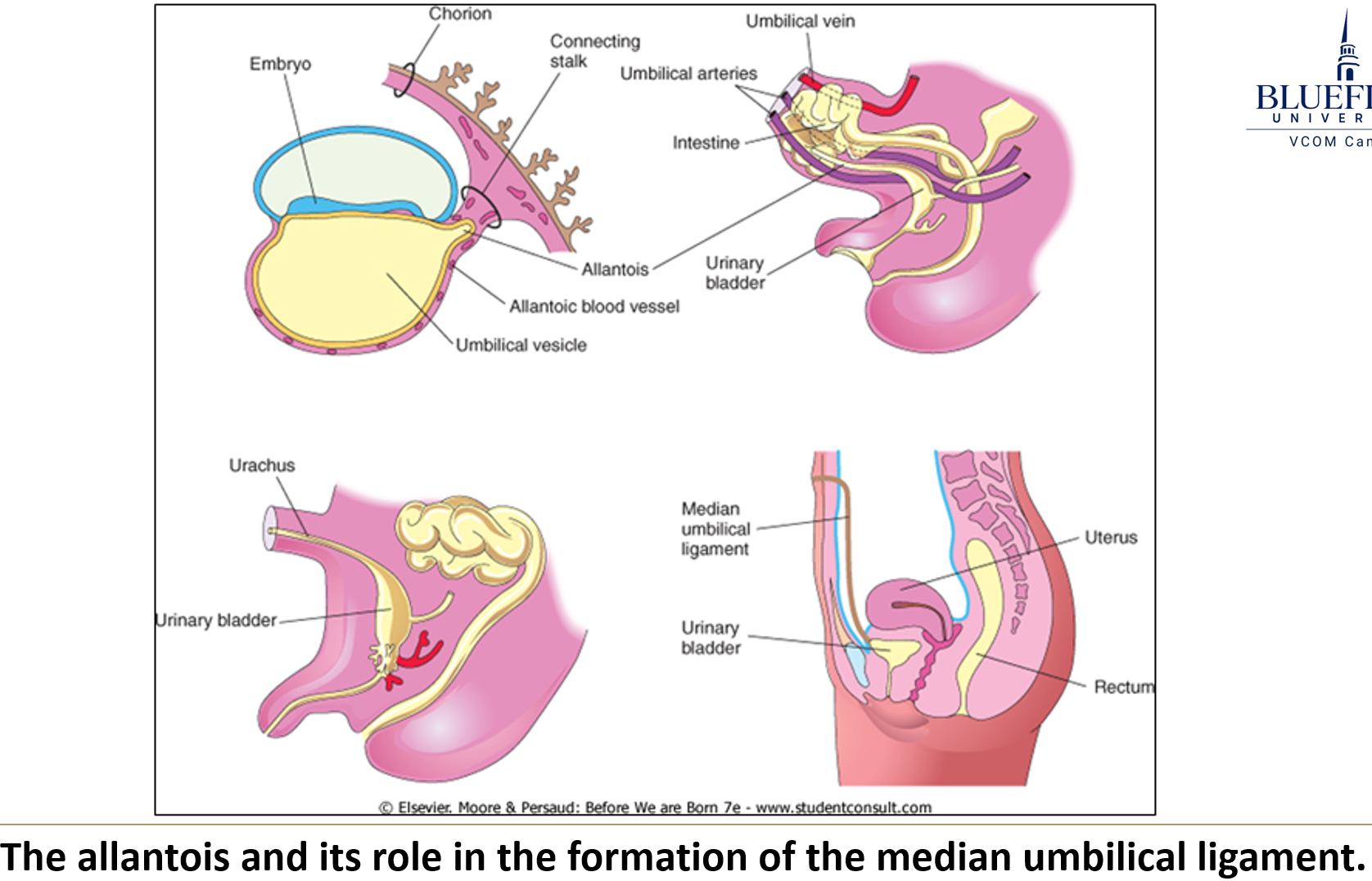
What are the functions of the allantois?
Its blood vessels form the umbilical vessels
Enhances exchange through the placental membrane
A portion becomes the urachus, which forms the median umbilical ligament after birth.