Scrotum
1/50
Earn XP
Description and Tags
Chapter 23 pg 708 - DONE
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
51 Terms
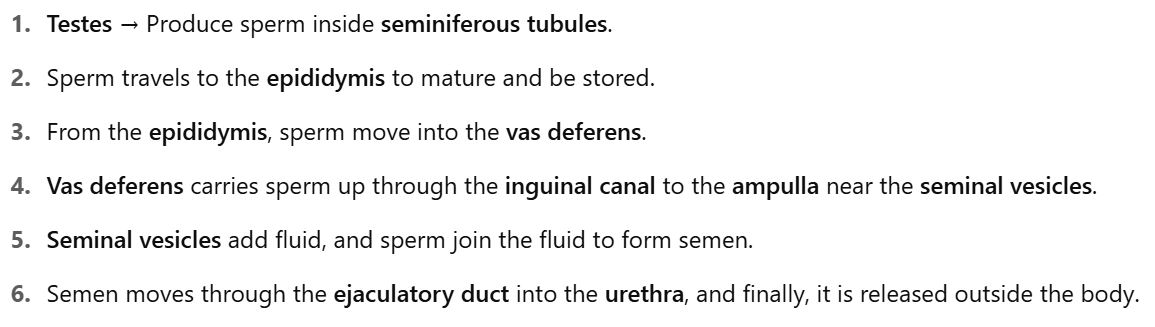
Testes 🧪 →
Epididymis 📍 →
Vas Deferens 🚶♂ →
Ampulla of the Deferens 🏁 →
Seminal Vesicles 🍇 →
Ejaculatory Duct 🚰 →
Urethra ⛲ →
Exit the body 🚪
Flow Map: Sperm Transport 🚗💨
Shape: Symmetrical, oval-shaped glands
Size: ~3-5 cm long, 2-4 cm wide, ~3 cm high 📏.
Structure: 250-400 lobules with seminiferous tubules 🧬.
Converge to form rete testis in the mediastinum 🔗.
Ultrasound appearance: Smooth, medium-gray, fine echotexture 🎨
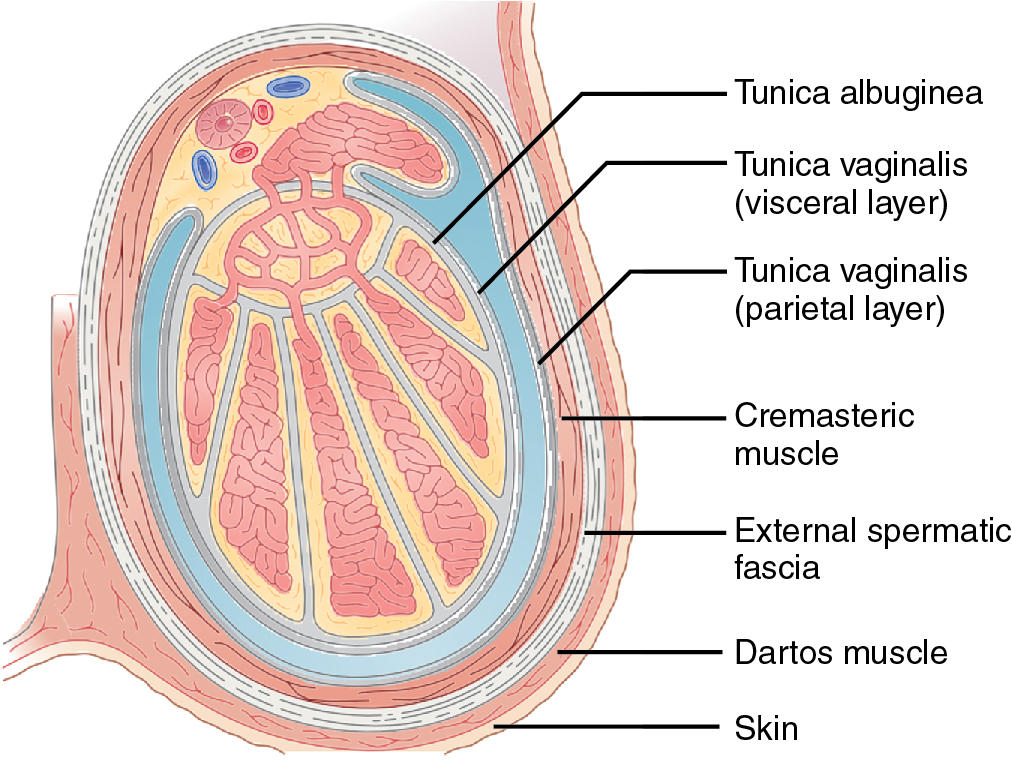
Covering:
Surrounded by the tunica albuginea, a dense, fibrous layer.
Mediastinum testis forms from the tunica albuginea, creating a vertical septum that supports blood vessels and ducts.
Ultrasound Appearance: Smooth, medium-gray with a fine echotexture.
Testes 🧪
What It Is: The fibrous outer covering of the testis.
Main Job: Gives shape to the testis and protects it.
Special Feature: It forms a structure inside the testis called the mediastinum testis, which supports blood vessels and ducts.
Ultrasound: Bright, white line that divides the testis into lobules.
The Tunica Albuginea 🏰
Testes produce what?
Main Job: ___________ .
Structure: Inside each testis, there are many tiny structures called seminiferous tubules that help make sperm.
Outer Layer: Covered by a tough membrane called the tunica albuginea.
Sperm and testosterone
Length: 6-7 cm, located superior and posterolateral to the testis.
Parts:
Head: Largest part (6-15 mm wide), superior to the upper pole of the testis 🧠.
Body: Smaller, hard to see on ultrasound 👀.
Tail: Slightly larger, posterior to the lower pole of the testis 🦰.
Appendix Epididymis: Small protuberance from the head (found in 34% unilaterally, 12% bilaterally) 🧶.
Ultrasound appearance: Isoechoic or hypoechoic, coarse texture 🔳.
Epididymis 📍
The Epididymis does what?
What It Is: A tube-like structure attached to each testis.
Main Job: _______________ .
Parts:
Head: Located at the top of the testis.
Body: The middle part of the epididymis.
Tail: Located at the bottom of the testis, connected to the vas deferens.
Relationship with Testes: It’s located just behind the testis.
Appearance: It’s a little coarser on ultrasound, compared to the smooth testis.
Stores sperm and helps them mature
What It Is: A small, extra structure that may be attached to the testis.
Where It Is: Between the testis and epididymis, at the top of the testis. (upper pole)
Common: Present in 92% of men unilaterally and 69% bilaterally.
Appearance: Small, oval, and may appear hypoechoic or isoechoic on ultrasound.
Appendix Testis 🍏
Small protuberance from the head of the epididymis.
Found in 34% of testes unilaterally, 12% bilaterally.
Ultrasound Appearance: Isoechoic or hypoechoic.
Appendix Epididymis 🧶
What It Is: A two-layered sac that surrounds each testis and epididymis.
Main Job: Provides a lubricated space for the testes to move within the scrotum.
Parts:
Parietal layer: Lines the inside of the scrotum.
Visceral layer: Covers the testis and epididymis.
Space Between Layers: This is where hydroceles (fluid collections) can form.
The Tunica Vaginalis 💧
What It Is: The tube that carries sperm from the epididymis to the urethra.
Connection: Starts from the tail of the epididymis and moves upward into the inguinal canal, eventually reaching the ampulla (enlarged portion near the seminal vesicles).
Connection with Seminal Vesicles: It joins with the seminal vesicles to form the ejaculatory duct, which empties into the urethra.
Vas Deferens 🚶♂
What It Is: The bundle of structures that suspends the testis in the scrotum.
Contents: Includes the vas deferens, blood vessels (arteries and veins), nerves, and lymphatics.
Connection: It connects the testis to the abdomen via the inguinal canal.
The Spermatic Cord 🔗
Tunica vaginalis has two layers:
Visceral layer: touches the testis and epididymis.
Parietal layer: lines the inside of the scrotal wall.
The space between these two layers is where fluid can build up → forming a ___________________???
Hydrocele
Layers of the Testes
Abdominal Aorta
⬇
Right & Left Testicular Arteries
⬇ (enter spermatic cord via deep inguinal ring)
Posterior Testis → Pierces Tunica Albuginea
⬇
Capsular Arteries (run along surface)
⬇
Centripetal Arteries (toward mediastinum)
⬇
Recurrent Rami (Centrifugal Arteries) (curve back outward)
⬇
Arterioles → Capillaries
➕ Optional Branch:
Transmediastinal Artery
↘ Coursing through mediastinum
⬇
Forms additional capsular branches (opposite side)
➕ Collateral Arterial Supply:
Cremasteric Artery (from inferior epigastric → external iliac)
Deferential Artery (from vesicle artery → internal iliac)
↘ Both can anastomose with testicular artery
Testicular Blood Flow – Arterial Supply
Pampiniform Plexus
⬇
Drains into 3 Sets of Veins:
Testicular Vein
- Right → Inferior Vena Cava
- Left → Left Renal VeinDeferential Vein → Pelvic Veins
Cremasteric Vein → Epigastric & Deep Pudendal Veins
🔼 Venous Drainage of Testes
✅ Preparation:
• No prep required.🛏 Position:
• Supine
• Penis placed on abdomen, covered with towel
• Legs together or towel under scrotum for support
• Valsalva Maneuver or Upright if varicocele is suspected🌡 Warm Gel:
• Generously apply to scrotum
• Use extra gel mound or stand-off pad if needed for near-field imaging
📍 Before Scanning – Ask the Patient
🗣 “Why are you here today?”
• Pain? Lump? Swelling? Trauma?
• Can they point to a lump?
• Any history (e.g., vasectomy)?
📝 Document: Location, duration, trauma history, symptoms
📷 Transducer Selection
🔍 Use 8–12 MHz linear probe
• Preferably high-resolution for best images
• Use Color Doppler & Spectral Doppler when needed
🔎 Step-by-Step Scanning Protocol 1⃣ Start with a Brief Survey Scan
🩻 Scan both testes from superior to inferior
🔄 Compare both sides:
• 🔸 Size
• 🔸 Shape
• 🔸 Echogenicity
• 🔸 Structure
❓ Ask yourself:
• Homogeneous or heterogeneous?
• Solid or cystic mass?
• Intra- or extratesticular?
• Is there swelling or shrinkage?
• Epididymis normal?
• Skin thickened?
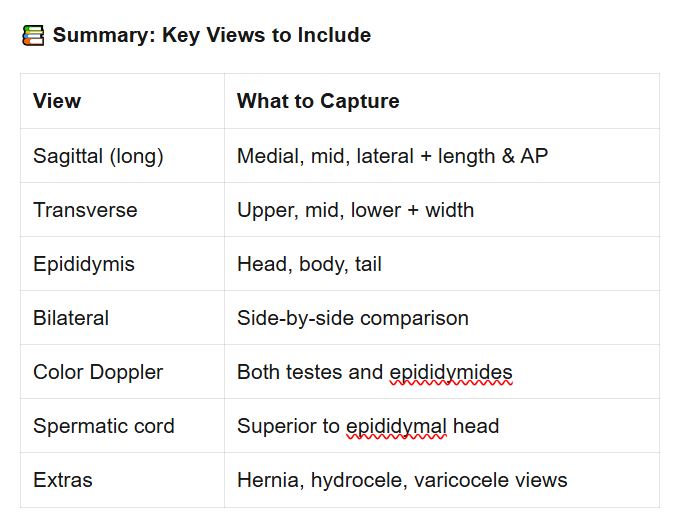
🖼 Required Images 🔹 Gray Scale Imaging
• Long axis (sagittal): Medial, mid, and lateral
• Length & AP measurements of testes and epididymis
• Transverse (axial): Upper, mid, and lower testes
• Width measurement at mid-transverse
• Transverse head of epididymis
• 📸 Split screen view for side-by-side comparison
• 🫧 Check for: Hydrocele, hernia, spermatoceles, tunica cysts
🧲 Color & Spectral Doppler
• Evaluate blood flow in both testes and epididymides
• 💓 Look for:
🔵 Normal flow
🔴 Absence of flow (possible torsion)
🟠 Increased flow (possible inflammation)
💡 Optimize for slow flow:
• Lower PRF/scale
• Decrease wall filters
• Increase gain/power
🧍♂ Special Maneuvers for Varicocele
• Upright position
• Valsalva maneuver
→ Look for dilation of veins in spermatic cord
💬 Tips for Success
✨ Ask the patient questions to guide the exam
🧊 Use gel generously for best contact
🧍 Always scan both sides, even if only one is symptomatic
🧠 Think critically as you scan – compare sides
📸 Take extra views if abnormalities are seen
🧍♂ Patient Positioning & Prep
1⃣ Problem: Large swelling → hard to see everything with regular view
⬇
2⃣ Solution: Use tools to expand the view or enhance image quality
⬇
3⃣ Tools/Techniques:
- Panoramic view 🖼
- Curved-array probe 🔄
- Advanced imaging features ⚙
- Doppler (Color, Power, Spectral) 🌈
⬇
4⃣ Tweak Settings to Get Best View 🎛
🎯 Goal: Improve Scrotal Ultrasound Imaging, Especially When There’s Swelling (like hydroceles, hematomas)
✅ Panoramic Tool 🧷
Moves with the probe and stitches a long image 🧵
Good when testicle is enlarged/swollen (like a big hydrocele)
✅ Image Stitching 🧩
Take one image ➡ move probe ➡ take second, matching edges
✅ Curved-Array Transducer 🌀
Frequency: 5–7.5 MHz
Use it temporarily to get whole scrotum in view, then go back to high-frequency linear probe for detai
🔍 Seeing More in One Image
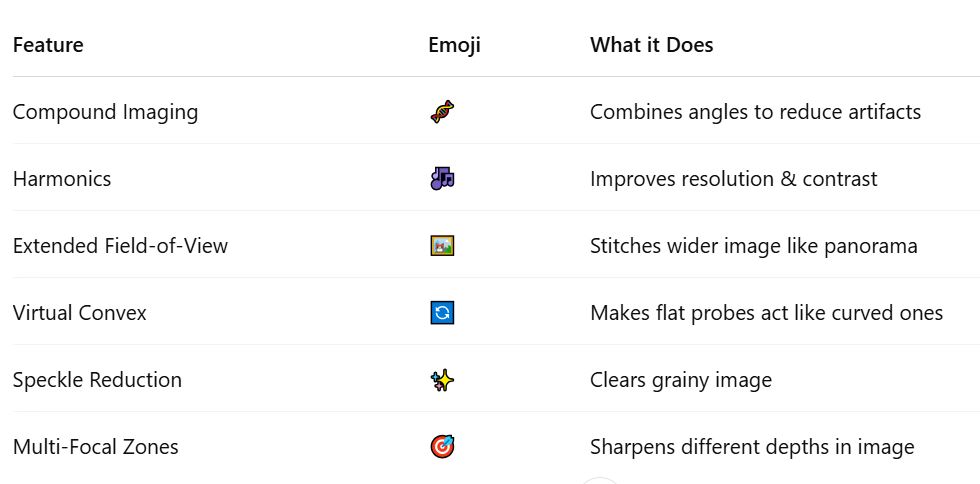
⚙ Advanced Imaging Features
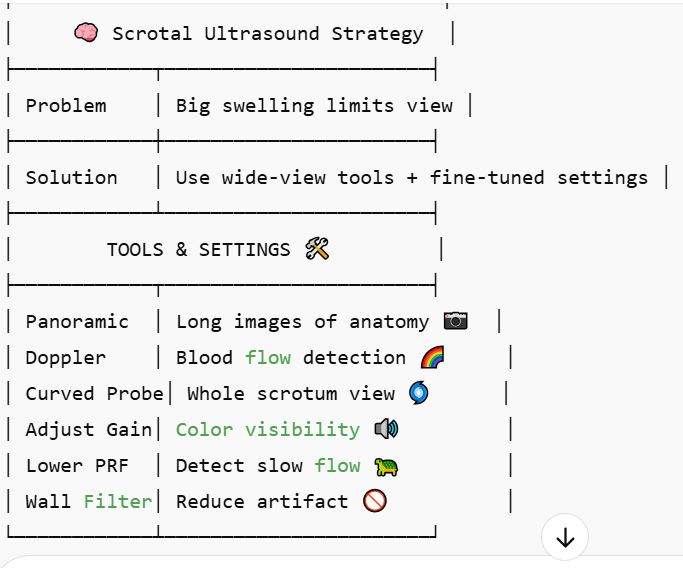
Color Doppler = Direction & speed of flow 🧭
Spectral Doppler = Velocity waveform 📈
Power Doppler = Shows presence of flow, not direction ➡ More sensitive to slow flow 🐢
🌈 Using Doppler for Blood Flow Types
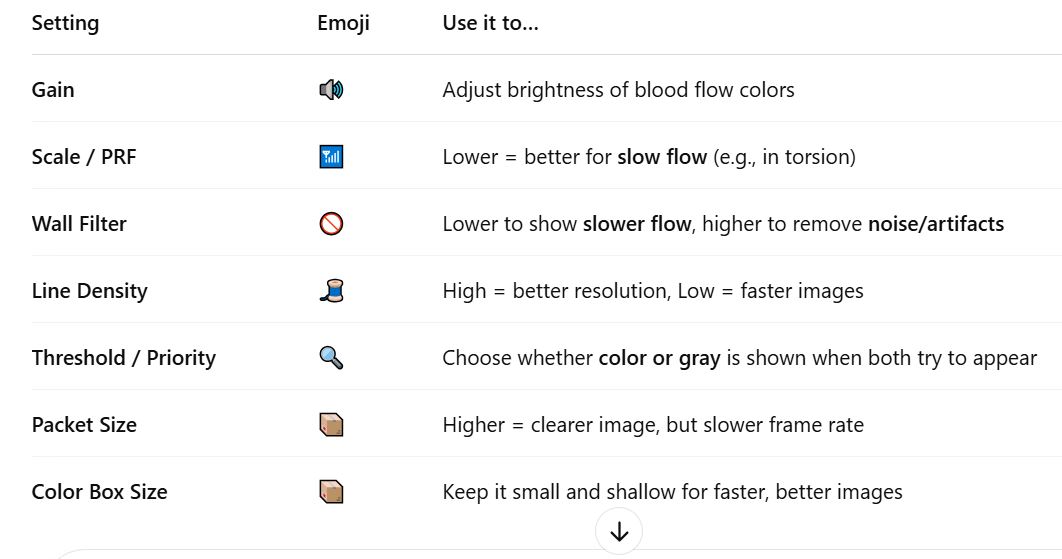
🎛 Doppler Settings to Tweak for Best View
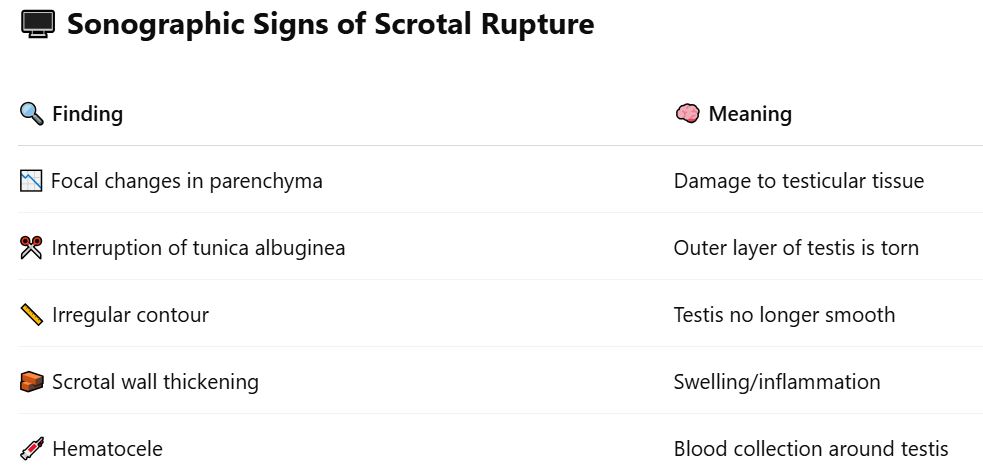
🚨 – Scrotal Trauma
Common Causes of Scrotal Trauma
🚗 Car accidents
🏃 Sports injuries
🥋 Direct blows
🚴 Straddle injuries
🧪 Main Goal of Ultrasound :
🔎 Determine if testicular rupture has occurred — it’s a surgical emergency!
✅ If treated within 72 hrs → 90% testis salvage
❌ After 72 hrs → Only 45% salvage
Acute Scrotum
Time After Injury | Sonographic Appearance |
|---|---|
⏱ Acute (Early) | Echogenic with moving echoes |
🕓 Chronic (Later) | Low-level echoes, septations, fluid level |
💉 Hematoceles (Blood in Scrotum)
Heterogeneous on ultrasound
May displace the testis
Can become cystic as they evolve
🧊 AVASCULAR – use color Doppler to check for absence of flow
🩸 Hematomas
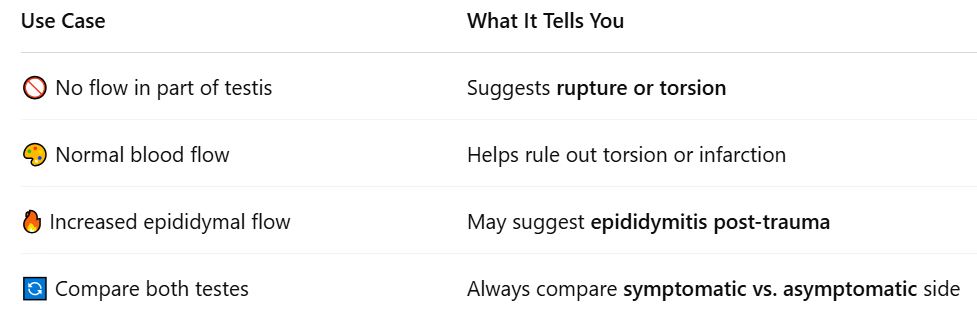
🎯 Use of Color Doppler in Trauma
🧍♂ Clinical Signs & Symptoms of
🩺 Finding | 🔎 Explanation |
|---|---|
😣 Painful, swollen scrotum | Most common and early complaint |
🛑 Sudden onset of pain | Often reported after trauma |
🤕 History of trauma | Key factor — from MVA, sports, straddle injury |
🧊 Tenderness to touch | Suggestive of inflammation, hemorrhage, or rupture |
📉 Reduced or absent blood flow (Doppler) | Suggests torsion or infarction (not visible externally) |
🔥 Increased vascularity (Doppler) | Suggests infection (epididymitis/orchitis) if trauma is secondary |
⚠ Signs of systemic infection (e.g., fever) | May be seen if infection accompanies trauma or occurs secondarily |
🔻 Displacement of testis | Due to large hematoma pushing it aside |
💧 Hydrocele or hematocele formation | May cause visible or palpable scrotal enlargement/swelling |
Scrotal Trauma (Acute Scrotum)
🦠 Infection of the epididymis and sometimes the testis (orchitis)
🔍 Causes
⚠ Common | 🧪 Less Common |
|---|---|
🔽 Spread from UTI (via spermatic cord) | 🧫 Mumps, syphilis, TB, viruses |
💉 Trauma (rare) | 🧪 Chemical causes |
🧍♂ Clinical Signs & Symptoms
🔎 Symptom | 🧠 Explanation |
|---|---|
😣 Increasing scrotal pain | Develops over 1–2 days |
🧊 Pain may be mild or severe | Variable, depending on severity |
🌡 Fever | Suggests systemic infection |
💧 Urethral discharge | Common with bacterial/UTI source |
💻 Sonographic Findings (Gray-Scale & Doppler) 🦠 Epididymitis
🔍 Enlarged, hypoechoic epididymis
✨ Hyperemic flow on color Doppler (increased blood flow)
⚪ Focal hyperechoic spots if hemorrhage is present
📊 Low resistance Doppler waveform (↑ systole & diastole)
🦠 Orchitis (when it spreads to testis)
📏 Enlarged testis (focal or diffuse)
🎨 Hypoechoic or heterogeneous appearance
🔥 Hyperemic flow if infected
🧊 Scrotal wall thickening
💧 May be associated with hydrocele (fluid around testis)
🧪 Severe Complications
🧠 Condition | 🩺 Sonographic Clues |
|---|---|
🧪 Testicular infarction | ⚠ Absent or decreased flow, high resistance waveform, reversed diastolic flow |
💥 Pyocele (pus collection) | Complex hydrocele with septations, debris, and loculations |
🔥 Epididymo-Orchitis
Torsion = twisting of the spermatic cord → cuts off blood supply 🚫🩸
A surgical emergency that needs immediate diagnosis!
⚠ Clinical Signs & Symptoms
❗ Symptom/Sign | 📘 Notes |
|---|---|
⚡ Sudden onset of scrotal pain | Classic hallmark |
😖 Severe pain | Usually intense, unilateral |
🧊 Swelling | Affected side, scrotal wall thickening |
🤢 Nausea & vomiting | Common with severe pain |
🔁 Prior episodes of pain | May suggest intermittent torsion |
📈 Peak incidence at age 14 | Most common in adolescents, but can happen at any age |
🎯 Undescended testis = 10× risk | Very high-risk group |
⏳ Timing Matters
🕐 Time Since Torsion | 🔧 Testis Salvage Rate |
|---|---|
Within 5–6 hours | 80%–100% 🌟 |
6–12 hours | ~70% ⚠ |
>12 hours | ~20% or less 🔥 |
🧬 Cause
📍 Bell Clapper Deformity: abnormal tunica vaginalis ➡ allows free rotation
Often bilateral anatomic anomaly
Starts with venous obstruction, then arterial occlusion → ischemia/infarction
💻 Sonographic Findings 📊 Gray-Scale Imaging
⏱ Time Frame | 🧪 Sonographic Features |
|---|---|
<4 hours | Testis may appear normal |
4–6 hours | Enlarged, hypoechoic testis; lobes visible due to edema |
>24 hours | Heterogeneous texture (due to necrosis, hemorrhage, infarction) |
⬆ Epididymis | Enlarged, ↓ echogenicity or heterogeneous |
⚫ Twisted Cord | Seen as round/oval extratesticular mass |
💧 Reactive hydrocele & scrotal wall thickening | May be present |
🎨 Color Doppler
🔍 Feature | 📘 What It Shows |
|---|---|
❌ Absent flow | Diagnostic of torsion |
✅ Normal flow in opposite testis | Used as comparison |
⚠ Adjust PRF & wall filter | Important for detecting slow flow |
↔ Spontaneous detorsion | May show hyperemia or minimal flow → mimics infection |
📍 Appendix torsion | Small hypoechoic mass near epididymis/testis; increased flow around it |
🔄 Testicular Torsion
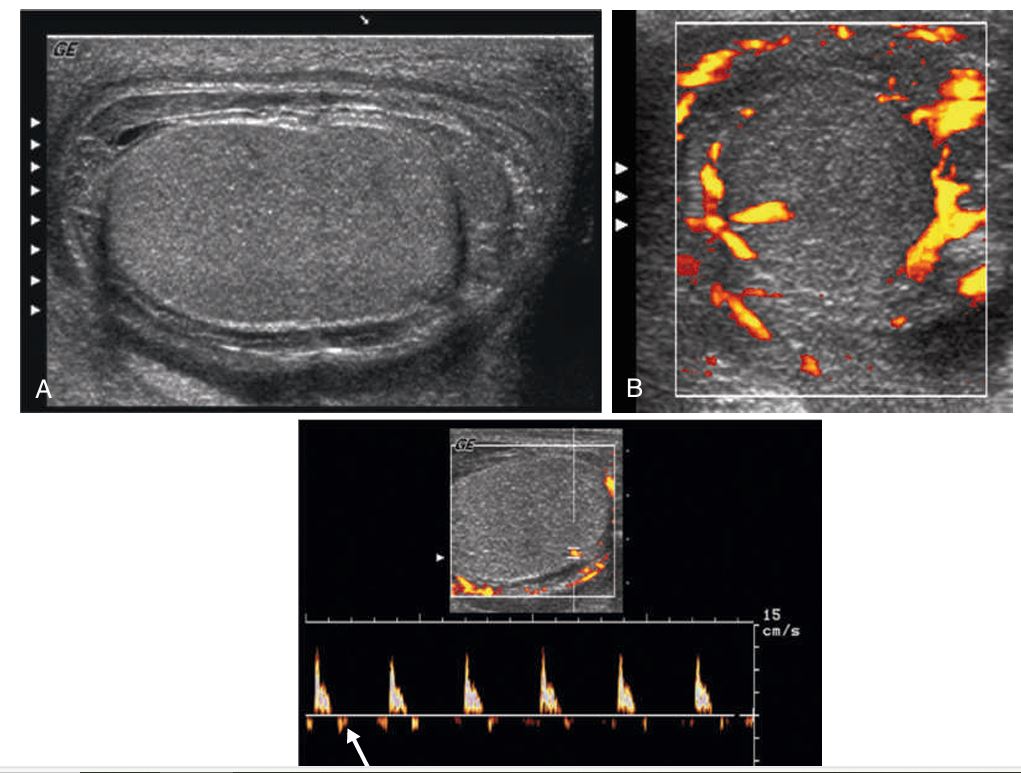
(A) Severe _________ in patient with scrotal pain, swelling, and edema.
The testis is swollen against a rigid tunica albuginea. Scrotal skin thickening is evident.
(B) Power Doppler shows hyperemic perfusion surrounding the testis but little intratesticular flow, despite the use of sensitive Doppler settings.
(C) Spectral Doppler waveform of an intratesticular artery demonstrates a high- resistance waveform. Reversed flow is seen in diastole (arrow). This is a serious finding, indicating threatened infarction.
Epididymo-orchitis
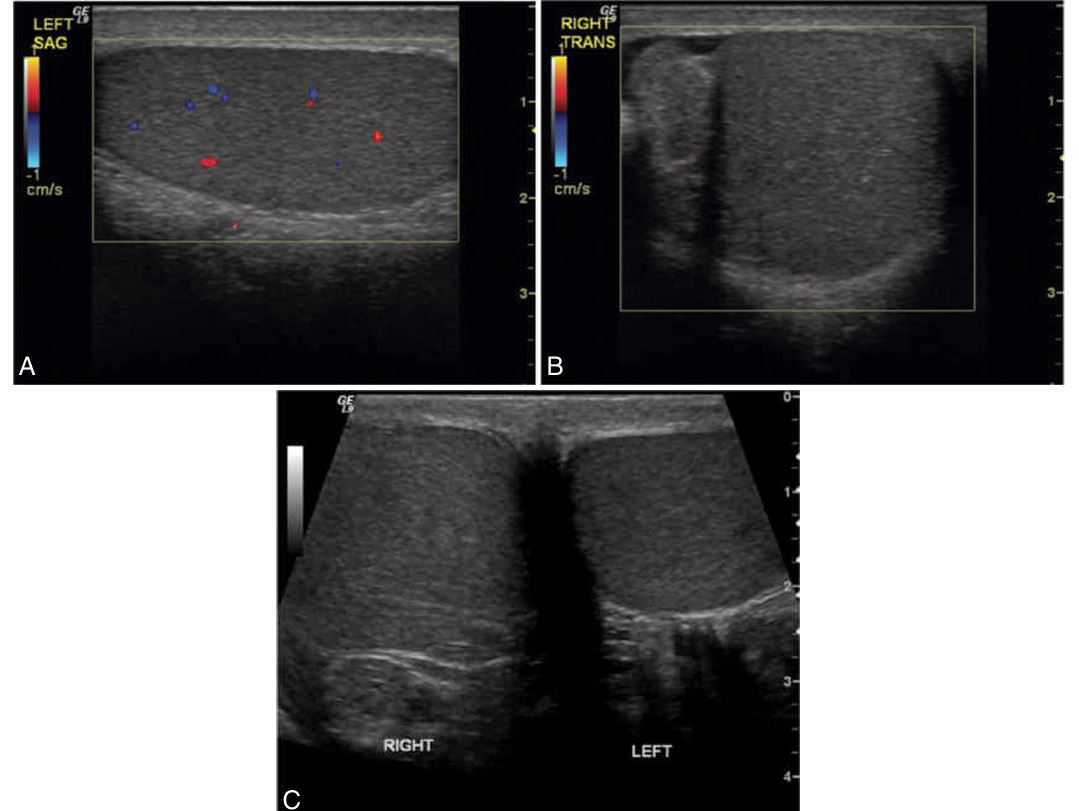
Testicular __________ in an adolescent patient with sudden onset of right testicular pain, accompanied by nausea and vomiting.
(A) Color Doppler shows normal flow within the parenchyma of the left testis.
(B) The right testis and epididymis are avascular with color Doppler imaging, with the same settings used to show flow on the asymptomatic side.
(C) Transverse ultrasound image showing both testes in right testicular torsion. The right testis is swollen and hyperechoic compared with the normal left testis.
Torsion
Definition & Location:
Cystic dilation of the efferent ductules of the epididymis
Always located in the epididymal head
Contents:
Filled with proteinaceous fluid and spermatozoa
Causes / Associations:
May occur more frequently after vasectomy
Symptoms:
Usually asymptomatic
May be palpable and cause patient concern
Sonographic Appearance:
Seen as simple cysts or multiloculated cystic collections
May contain internal echoes
Shows posterior acoustic enhancement
🧪 Spermatocele
Definition & Location:
Small, clear cysts that contain serous fluid
Found anywhere within the epididymis
Symptoms:
Generally asymptomatic
May be palpable
Sonographic Appearance:
Simple, fluid-filled structures
Thin walls
Posterior acoustic enhancement
Note:
Ultrasound cannot reliably differentiate between spermatocele and epididymal cyst
🧫 Epididymal Cyst
Definition & Location:
Found in the tunica albuginea (lining around the testis)
Extratesticular, typically near the testicular surface
Symptoms:
Generally asymptomatic
Can become large enough to displace or distort the testis
Sonographic Appearance:
Usually small, anechoic, thin-walled
May cause distortion of the testis, unlike hydroceles
Shows posterior acoustic enhancement
🩸 Tunica Albuginea Cyst
🔍 Definition & Location
Abnormal dilation of the veins in the pampiniform plexus, located within the spermatic cord.
📌 Types
Primary Varicocele
Caused by incompetent venous valves in the spermatic vein
More common on the left side
Anatomical reason:
The left spermatic vein drains at a steep angle into the left renal vein
Compression of the left renal vein between the aorta and superior mesenteric artery can occur
Secondary Varicocele
Due to increased pressure on the spermatic vein
Can result from:
Renal hydronephrosis
Abdominal mass
Liver cirrhosis
Retroperitoneal malignancy (e.g. invading the left renal vein → noncompressible varicocele)
⚠ In men >40 years old, a noncompressible varicocele warrants evaluation for a retroperitoneal mass
🧬 Clinical Significance
Associated with male infertility
More common in infertile men
Treatment may improve sperm count in ~53% of cases (though it's still debated)
Intratesticular varicocele may occur (near the mediastinum)
Clinical significance unknown, but potentially impacts fertility like extratesticular types
💡 Sonographic Findings Extratesticular Varicocele
Numerous tortuous tubes of varying sizes near epididymal head
May show moving echoes → indicates slow venous flow
>2 mm diameter
Enlarges with Valsalva or upright position
Color Doppler:
Confirms venous flow
Shows retrograde filling with Valsalva
Requires sensitive settings for slow flow (low PRF & wall filter)
⚠ Flash artifact may occur — instruct patient to hold still
Intratesticular Varicocele
Appears as straight or serpiginous channels from mediastinum into testis
Can mimic tubular ectasia of the rete testis on gray-scale
Key difference:
Color Doppler shows venous flow in varicocele
Tubular ectasia shows no flow
💢 Varicocele
🔍 Definition
Occurs when bowel, omentum, or other abdominal structures herniate into the scrotum.
🧪 Clinical Evaluation
Often clinically diagnosed, but ultrasound is used when the diagnosis is unclear or equivocal.
📊 Most Common Contents
Bowel — most common
Omentum
💡 Sonographic Findings
✅ Confirmatory Sign
Peristalsis of bowel loops on real-time imaging → confirms diagnosis
Can be documented with cine clips or video recording
📺 Appearance Based on Contents
Fluid-filled bowel
Easy to recognize on ultrasound
Air-filled bowel
Shows bright echoes with:
Dirty acoustic shadow
Ring artifact
Solid stool-filled loops
Harder to detect
Omental hernia
Appears brightly echogenic due to omental fat
Clinical Findings
Scrotal mass or swelling
→ This is often palpable and may extend from the inguinal canal into the scrotum.Soft, reducible mass
→ The hernia may be pushed back into the abdomen manually, especially when the patient is lying down.Changes with position or straining
→ The swelling increases with standing or Valsalva (straining, coughing, etc.)May be painful or painless
Painless in many cases.
Pain or discomfort may occur with prolonged standing, heavy lifting, or if the hernia becomes incarcerated (trapped).
Bowel sounds in the scrotum (very suggestive!)
→ Clinicians may even auscultate (listen) and hear gurgling—which strongly suggests bowel content.Incarceration or strangulation signs (emergency):
Severe pain
Redness or firmness
Signs of bowel obstruction (nausea, vomiting, no bowel movements)
Scrotal Hernia
These fluid collections form in the potential space between the visceral and parietal layers of the tunica vaginalis.
💧 Hydrocele, Hematocele, Pyocele
🌊📖 Definition
Serous fluid collection
Most common cause of painless scrotal swelling
⚠ Causes
Idiopathic (unknown origin)
Associated with:
Epididymo-orchitis
Testicular torsion
Trauma
Neoplasm (tend to have smaller hydroceles)
🧪 Sonographic Findings
Fluid-filled area outside the anterolateral aspect of the testis
Typically anechoic, but may show low-level echoes (cellular debris)
More internal echoes seen in infectious cases
Better visualization of debris with:
High-frequency transducers
Harmonic imaging
May appear more anechoic with:
Frequencies < 7 MHz
Low dynamic range
Clinical Findings
Painless scrotal swelling
→ This is the key clinical feature of a hydrocele.May be palpable by the patient or physician.
Typically not tender, unless associated with infection, trauma, or torsion.
Hydrocele
🧫 📖 Definition
Pus collection in the tunica vaginalis
Caused by:
Untreated infection
Ruptured abscess
🧪 Sonographic Findings
Indistinguishable from hematoceles on ultrasound
Internal echoes
Thick septations
Loculations
Presence of air = confirms abscess (but not always present)
Clinical Findings
Occurs due to untreated infection or abscess rupture
Painful and tender scrotum
May present with:
Redness
Fever
Systemic signs of infection (chills, malaise)
→ These aren't directly listed but can be inferred based on the pus and infectious nature.
Pyocele
📖 Definition
Blood collection in the tunica vaginalis
Caused by:
Trauma
Surgery
Neoplasm
Torsion
🧪 Sonographic Findings
Same appearance as pyocele:
Internal echoes
Thick septations
Loculations
Cannot be definitively differentiated from pyocele by ultrasound alone
Clinical Findings
Usually occurs after trauma, surgery, torsion, or neoplasm
Painful scrotal swelling (especially if acute)
Tenderness is likely due to blood accumulation
May present with bruising or discoloration of the scrotum (not always noted in the text but commonly known)
🩸 Hematocele
✅ Definition / Cause:
A chronic inflammatory reaction to extravasation of spermatozoa (sperm leakage into surrounding tissue).
Most commonly seen in patients with a history of vasectomy.
👨⚕ Clinical Findings:
Frequently painful (helps distinguish from epididymal tumors, which are usually painless).
Usually found in post-vasectomy patients.
May be palpable.
Can be located anywhere within the epididymis or vas deferens.
📸 Sonographic Findings:
Appears as a well-defined solid mass.
Echotexture: Hypoechoic or isoechoic relative to the epididymis.
Often heterogeneous in appearance.
Calcifications are not commonly present.
Color Doppler: May show increased flow if inflammation is present.
🔍 Key Diagnostic Notes:
Ultrasound’s main role: Determine if the mass is intratesticular or extratesticular:
Extratesticular masses (like sperm granulomas) are much less likely malignant than intratesticular ones.
Cannot be reliably distinguished from epididymal tumors on ultrasound alone.
Patient history (e.g., vasectomy) is essential in narrowing the differential.
Strongly associated with vasectomy history.
Can occur at the site of vas deferens ligation.
Sperm Granuloma
🧵✅ Definition:
Uncommon, benign condition.
Involves dilation of the rete testis tubules (located at the mediastinum testis, the hilum area).
Clinical Findings:
Typically affects men ≥45 years old.
Associated with epididymal obstruction on the same side.
Often seen with:
Spermatoceles
Epididymal/testicular cysts
📸 Sonographic Findings:
Hypoechoic tubular structures near the echogenic mediastinum.
Avascular on Doppler.
Must be differentiated from intratesticular varicocele:
Tubular ectasia = no flow
Intratesticular varicocele = slow venous flow
(requires low PRF & Valsalva)
Tubular Ectasia of the Rete Testis
💧 ✅ Definition:
Simple fluid-filled cysts located within the testis, near the mediastinum.
Clinical Notes:
More common in men >40 years.
Often incidental and do not require treatment.
Associated with extratesticular spermatoceles.
📸 Sonographic Findings:
Anechoic lesion
Smooth borders
Posterior acoustic enhancement
Intratesticular Cysts
🟡 ✅ Definition:
Tiny intratesticular calcifications
(<3 mm, usually multiple).May be associated with malignancy, but the relationship is unclear.
Clinical Notes:
Usually bilateral
May also be associated with:
Cryptorchidism
Klinefelter syndrome
Infertility
Varicocele
Testicular atrophy
Male pseudohermaphroditism
Annual ultrasound follow-up may be recommended
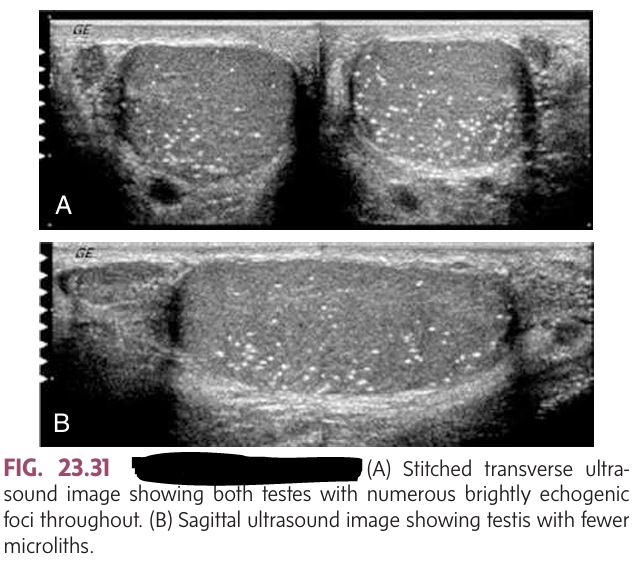
📸 Sonographic Findings:
Multiple bright, non-shadowing echogenic foci scattered in testis
Not considered abnormal unless >5 seen on one image
Testicular Microlithiasis
✅ Overview:
Most common malignancy in men aged 15–35
Peak: Ages 20–34
95% of testicular tumors are germ cell type
Highly malignant
Most often painless, presenting as:
A lump
Testicular enlargement
Vague scrotal discomfort
⚠ Risk Factors:
Undescended testicles (cryptorchidism): 2.5–8x more likely
More common in white men
🧪 Labs:
↑ hCG
↑ Alpha-fetoprotein (AFP)
CLINCAL FINDING:
Most patients:
Painless lump
Testicular enlargement
Vague discomfort in the scrotum
Germ Cell Tumors
✅ Overview:
Rare
Usually occurs later in life
Often bilateral, with multiple lesions
⚠ Primary Tumors May Originate From:
Prostate
Kidney
Lung, pancreas, bladder, colon, thyroid, melanoma (less common)
📸 Sonographic Appearance:
Solid hypoechoic mass
May also appear hyperechoic or mixed
❌ No specific clinical findings mentioned
Metastasis to the Testicle
✅ Overview:
Lymphoma:
1–7% of all testicular tumors
Most common secondary testicular malignancy in men >60
Leukemia:
Most common in children
Seen in ~8% of kids with leukemia
Clinical Findings:
Weight loss
Anorexia
Weakness
Unilateral or bilateral testicular enlargement
📸 Sonographic Appearance:
Homogeneous hypoechoic testis
Or multiple focal hypoechoic areas
Increased vascularity with Doppler
Chronic lymphocytic leukemia may show anechoic mass with through-transmission
Lymphoma & Leukemia
✅ Overview:
Testes fail to descend into the scrotum
Most common location: Inguinal canal
More common in preterm babies
Bilateral in 10–25%
⚠ Complications if untreated:
Infertility
↑ Risk of testicular cancer
↑ Risk of torsion
📸 Sonographic Appearance:
Smaller, less echogenic testis
Oval, homogeneous
Mediastinum rarely seen
Clinical findings:
❌ Not described with classic clinical symptoms — but text says:
May be palpable in the inguinal canal
Can lead to infertility, cancer, and torsion if untreated
Scrotum may appear empty
Cryptorchidism (Undescended Testis)
✅ Overview:
Very rare
Testicle located outside normal descent path
Most common location: Superficial inguinal pouch
❌ No clinical findings explicitly listed
Testicular Ectopia
✅ Overview:
Unilateral in ~4% of nonpalpable testes (more common on left)
Bilateral anorchia is rare (0.6–1%)
Patients have XY genotype
Associated with:
Hypoplastic scrotum
Micropenis
Delayed puberty
Clinical Findings:
Empty, hypoplastic scrotum
Micropenis
Delayed puberty due to hormonal imbalance
Anorchia (Absent Testis)
✅ Overview:
Extremely rare (~80 cases reported)
Left side more common (75%)
Bilateral in 5%
Testes may be in scrotum, inguinal canal, or retroperitoneum
⚠ Associated Risks:
↑ Malignancy
↑ Cryptorchidism
↑ Inguinal hernia
↑ Torsion
📸 Imaging Clue:
Duplicated testis is often small, and no efferent duct system
🔹 Clinical Findings:
❌ No direct clinical symptoms listed
But associated risks include malignancy, cryptorchidism, hernia, and torsion
Polyorchidism (Testicular Duplication)
1. Normal Anatomy & Physiology
Testes:
Symmetric, oval-shaped glands in the scrotum.
Sonographic appearance: smooth, medium-gray with fine echotexture.
Epididymis:
6–7 cm tubular structure.
Begins superiorly, courses posterolaterally to the testis.
Blood Supply:
Arteries: Right and left testicular arteries arise from the abdominal aorta (just below renal arteries).
Veins: Venous drainage via pampiniform plexus.
Tunica Vaginalis:
Contains a potential space between visceral and parietal layers.
Site where hydrocele, pyocele, or hematocele may develop.
2. Sonographic Pathologies A. Trauma
Scrotal rupture:
Focal alteration of parenchymal pattern
Interruption of tunica albuginea
Irregular contour, wall thickening, hematocele
B. Infection/Inflammation
Epididymo-orchitis:
Infection of epididymis and testis
Often from lower urinary tract infection
Pyocele:
Pus collection
Results from untreated infection or ruptured abscess
Sperm granuloma:
Chronic inflammatory reaction to sperm leakage
Common post-vasectomy
3. Vascular & Structural Abnormalities
Torsion of the spermatic cord:
Due to abnormal testicular mobility
Often caused by bell clapper deformity
Varicocele:
Dilated veins of pampiniform plexus
Caused by incompetent venous valves
Hernia:
Bowel, omentum, or other structures herniate into scrotum
4. Cysts and Benign Conditions
Scrotal Cysts:
Usually extratesticular
Benign fluid collections
Hydrocele:
Serous fluid in tunica vaginalis
Most common cause of painless scrotal swelling
May be idiopathic or associated with epididymo-orchitis/torsion
Tubular ectasia of rete testis:
Benign, uncommon
Associated with spermatocele or epididymal obstruction
5. Testicular Tumors
General Notes:
Extratesticular masses = usually benign
Intratesticular masses = more likely malignant
Tumors classified as germ cell or non–germ cell
Germ Cell Tumors:
Elevated hCG and AFP
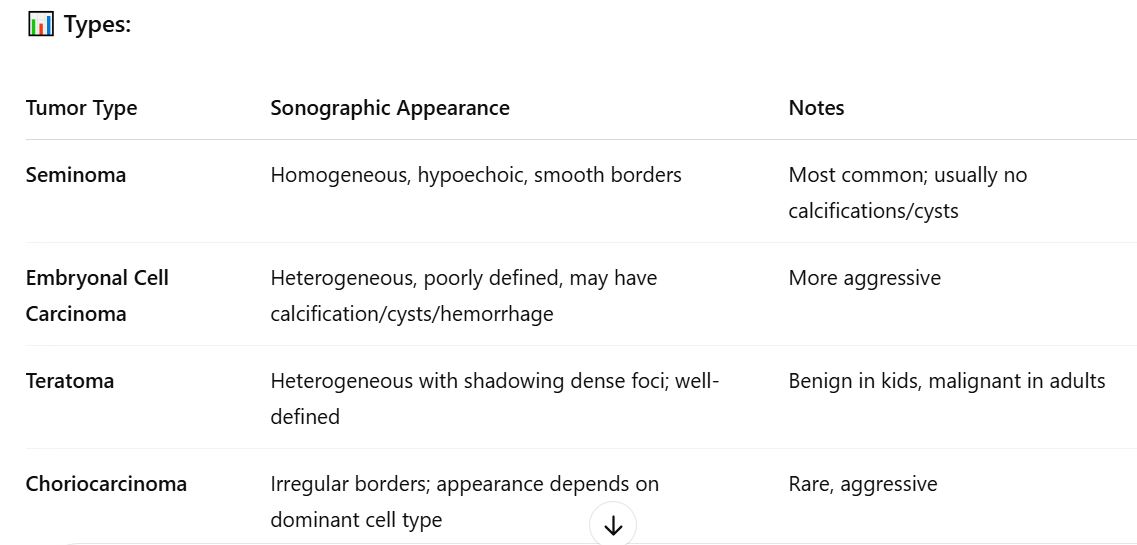
Seminoma: Homogeneous, hypoechoic, smooth border
Embryonal carcinoma: Heterogeneous, less defined, calcifications, hemorrhage, cysts
Teratoma: Heterogeneous, well-defined, may have acoustic shadowing
Lymphoma:
1–7% of testicular tumors
Most common bilateral secondary neoplasm in men >60
6. Congenital Anomalies
Undescended testis (cryptorchidism):
Testis not in scrotum, can't be manipulated into place
Orchiopexy:
Surgical correction by placing testis in scrotum
KEY PEARLS