Session 2: Toxins
1/66
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
67 Terms
Toxigenesis
Ability to produce toxins
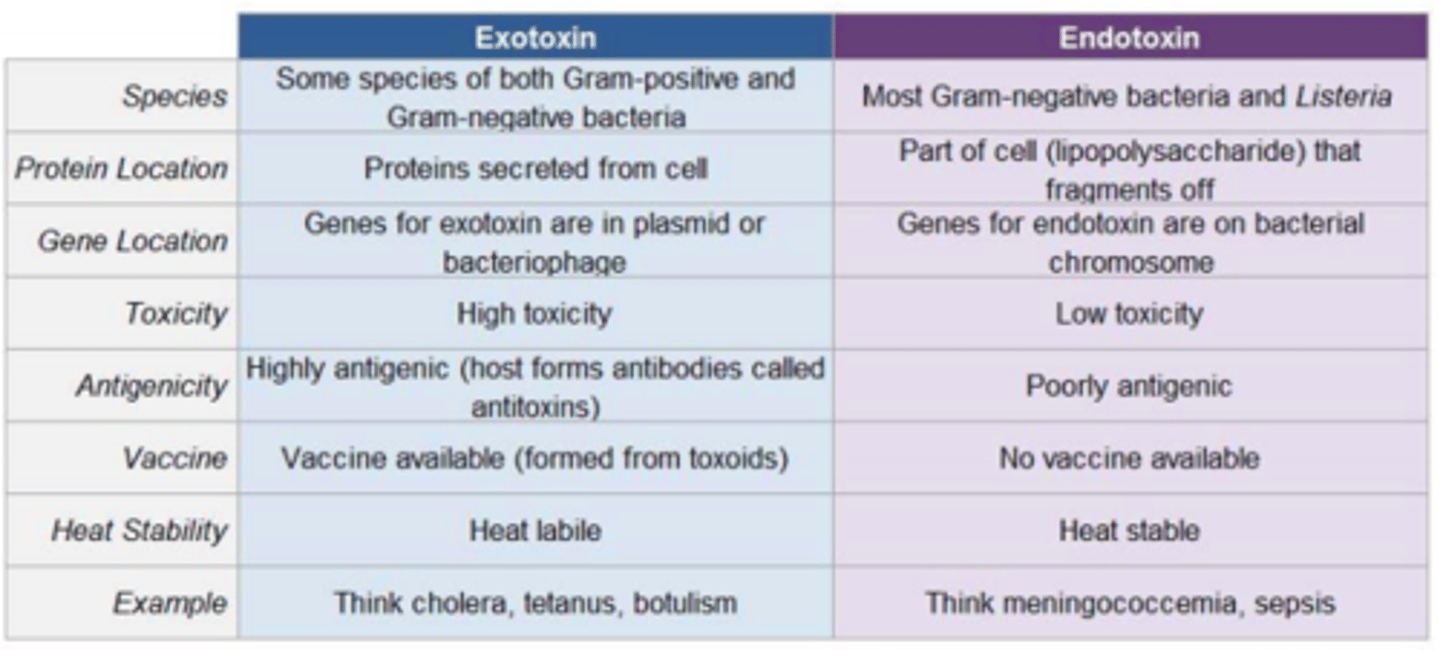
Bacteria can produce two types of toxins, what are they?
1) Exotoxins = released from bacterial cells and may act at tissue sites removed from the site of bacterial growth
2) Endotoxins = cell-associated substance
Difference between Gram positive and Gram negative bacteria
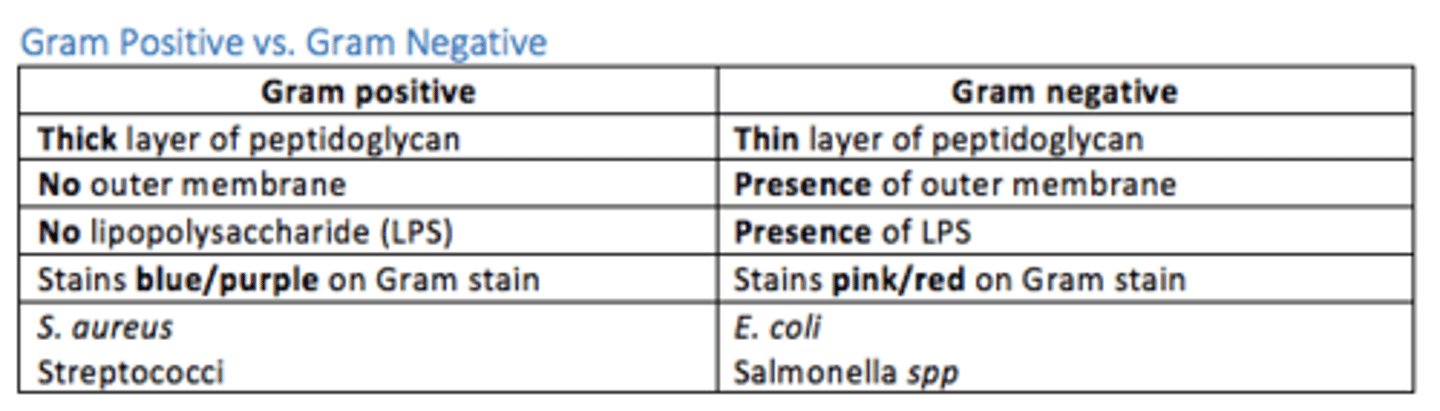
Example of an endotoxin
Lipopolysaccharide (LPS) in Gram negative bacteria
When are LPS endotoxin released from Gram negative bacteria?
LPS are released after destruction of the bacterial outer membrane or secreted in bacterial vesicles
How does LPS produce an inflammatory response?
Lipid A (the toxic component of endotoxins) stimulates TLR4 expressed on myeloid cells (macrophages, monocytes).
TLR-4 stimulation leads to production of pro-inflammatory cytokines such as IL-1, IL-6, IL-8, TNF and platelet-activating factor and also stimulate production of prostaglandins.
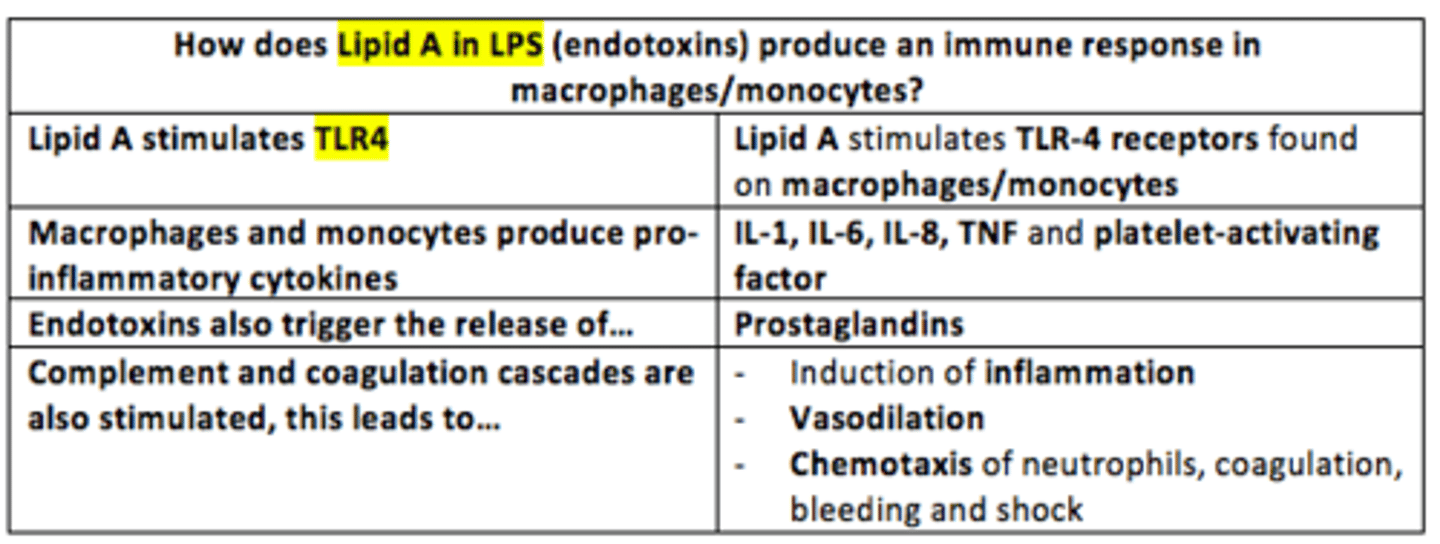
LPS endotoxin stimulates the ___ and ___ cascades, inducing inflammation, vasodilation, chemotaxis of neutrophils, coagulation, bleeding and shock
LPS endotoxin stimulates the complement and coagulation cascades, inducing inflammation, vasodilation, chemotaxis of neutrophils, coagulation, bleeding and shock
Gram ___ bacteria are the leading cause of sepsis
Gram negative bacteria are the leading cause of sepsis
E.g., Pseudomonas aeruginosa, Escherichia coli
An example of an endotoxin-mediated disease state of heightened inflammation leading to massive production of proinflammatory cytokines such as TNF-alpha, leading to inflammatory tissue injuries and multi-organ failure
Sepsis
What bacteria causes meningococcal disease
Neisseria meningitidis
Aerobic, Gram negative diplococcus which colonises the nasal cavity
Symptoms of meningococcal meningitis
- Fever
- Headache
- Nausea/vomiting
- Petechial rash

Neisseria meningitidis release ___ which triggers the inflammatory response, resulting in small-vessel thrombosis and skin necrosis
Neisseria meningitidis release endotoxin which triggers the inflammatory response, resulting in small-vessel thrombosis and skin necrosis
If left untreated and severe, meningococcal meningitis may progress rapidly to what complications?
- Septic shock
- Hypotension
- Acidosis
- Disseminated intravascular coagulation
Exotoxin
Group of soluble proteins secreted by a bacterium which can destroy cells directly or disrupt normal cellular metabolism
Examples of exotoxins
Botulinum toxin
Tetanospasmin toxin
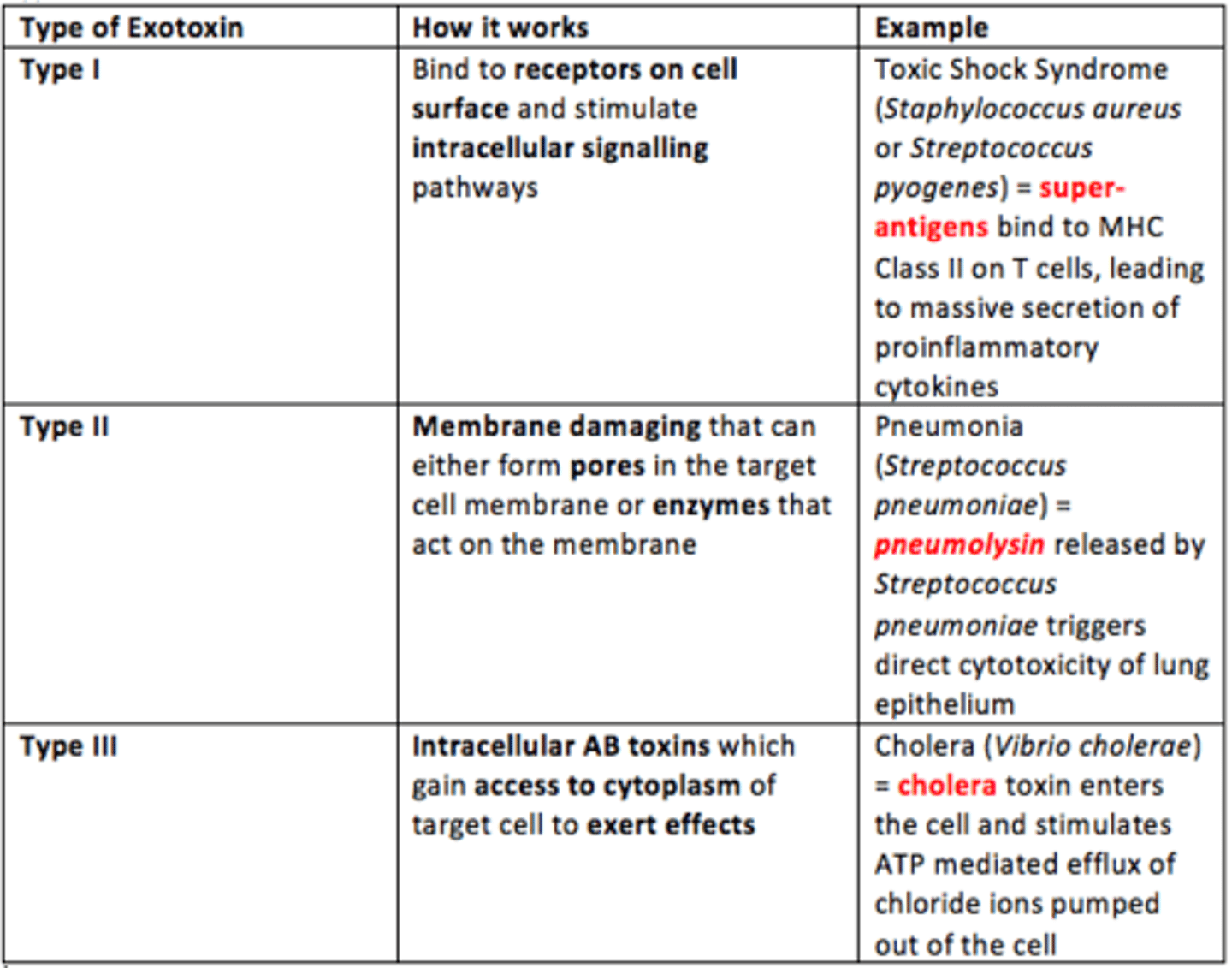
How many different types of exotoxin are there?
Three
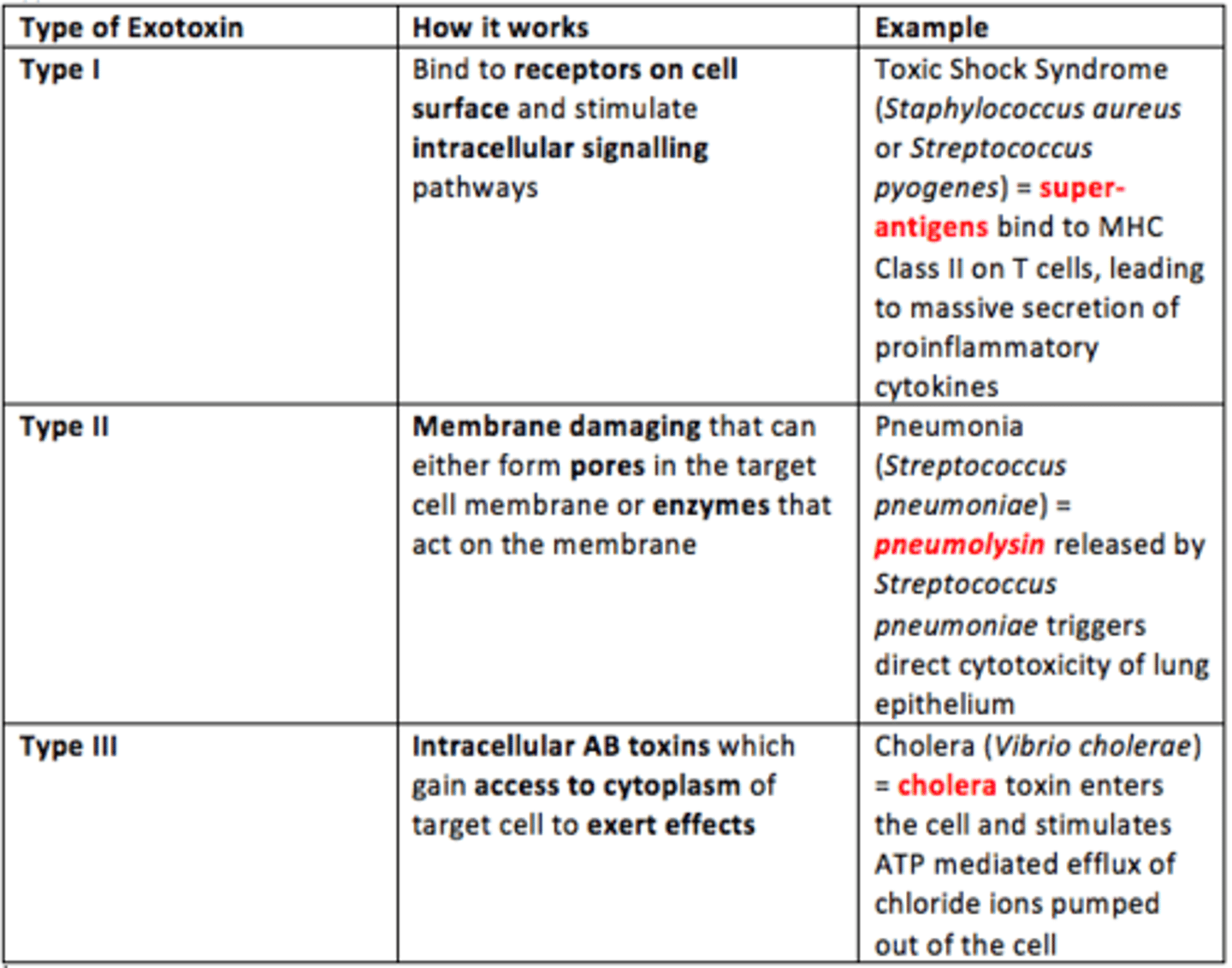
Type I exotoxin
Bind to receptors on the cell surface and stimulate intracellular signalling pathway
Example = Toxic Shock Syndrome
Superantigens bind to MHC Class II on T cells, leading to a massive secretion of proinflammatory cytokines
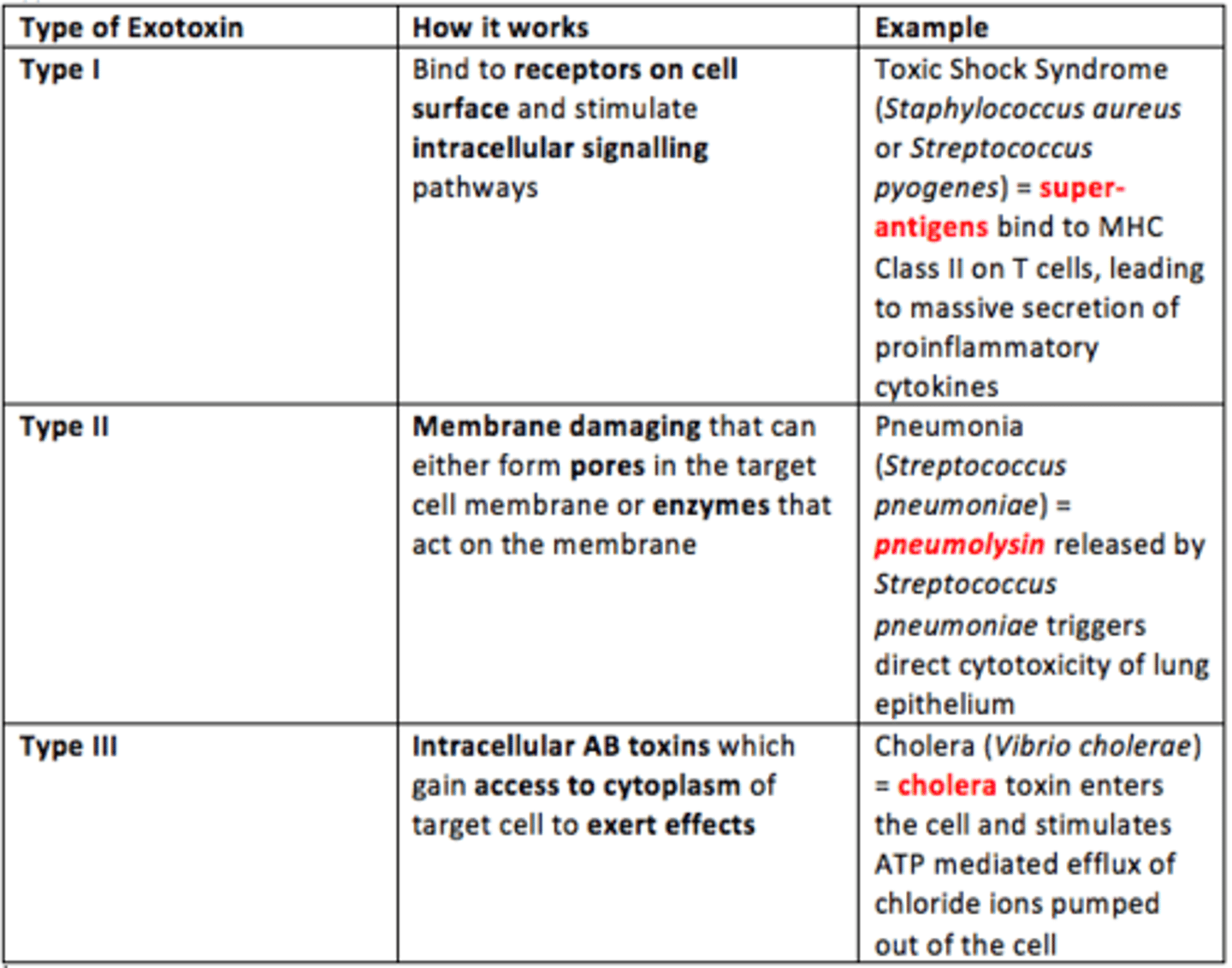
Type II exotoxin
Membrane damaging which form pores in cell membrane or enzymes that act on the membrane
Example = Pneumonia
Pneumolysin enzyme released by Streptococcus pneumoniae triggers direct cytotoxicity of lung epithelium, nasal tracheobronchial epithelium
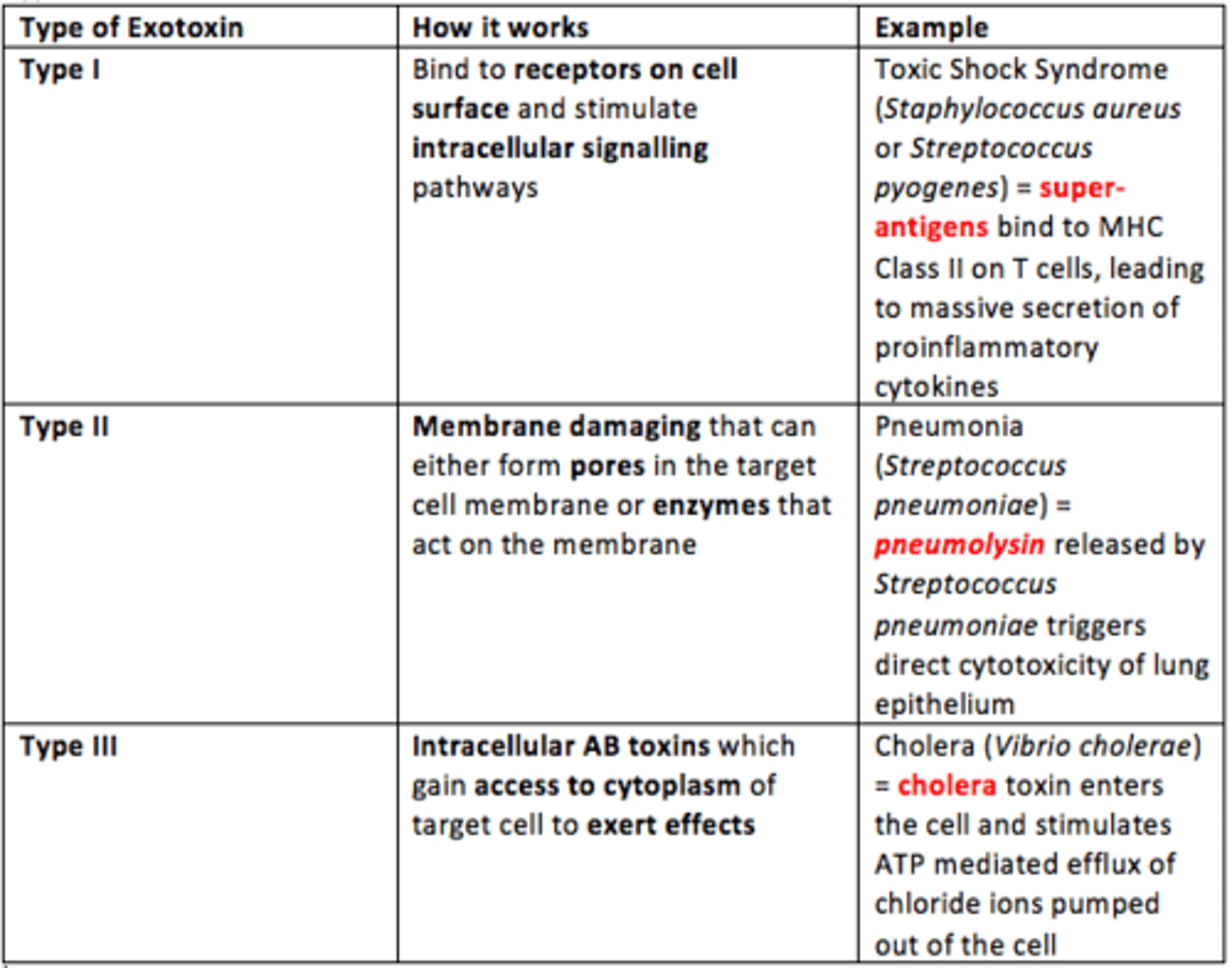
Type III exotoxin
Intracellular toxins which gain access to cytoplasm of target cell to exert effects
Example = Cholera
Cholera toxin enters cell and stimulates ATP mediated efflux of chloride ions pumped out of the cell
Enterotoxin
Exotoxins that act on GI tract to cause diarrhoea e.g., cholera toxin
Neurotoxins
Exotoxins that act on the nerves or the neuromuscular junctions to cause paralysis or spasms e.g., botulinum toxin or tetanospasmin toxin
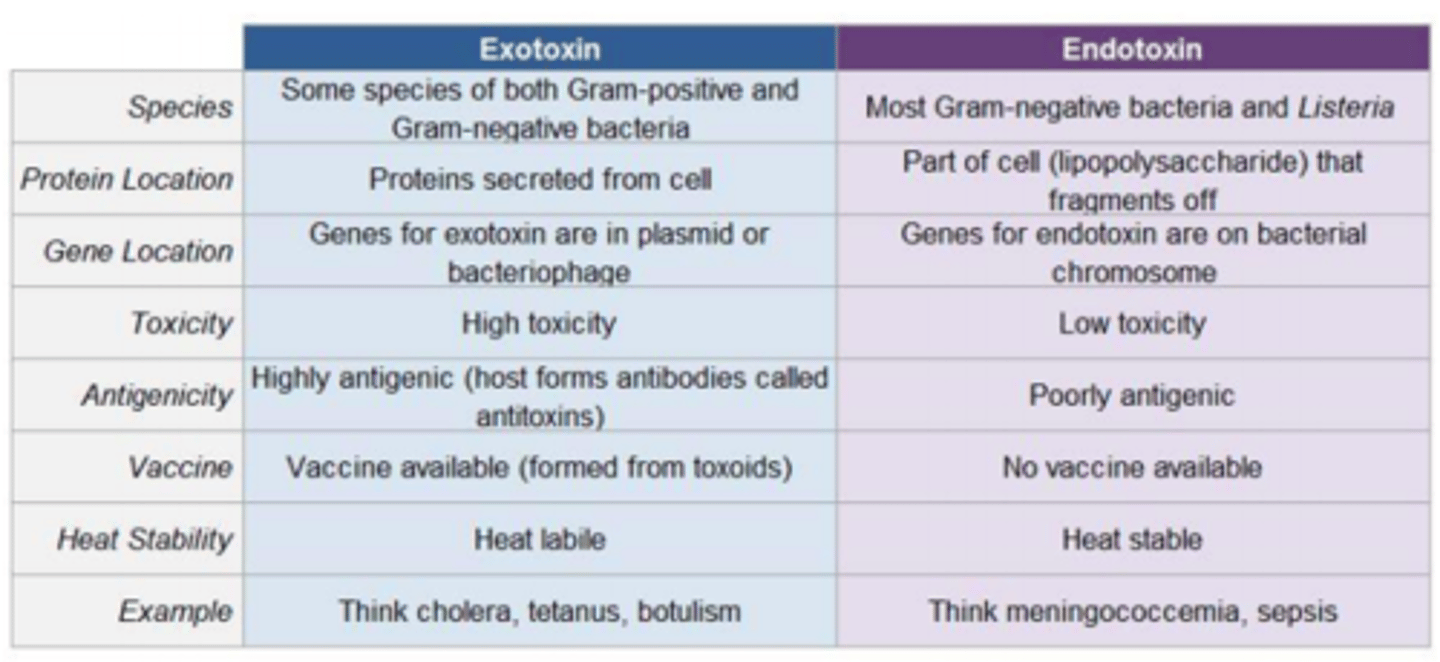
Differences between exotoxins and endotoxins
Clostridium botulinum
Gram positive, rod-shaped, anaerobic, spore-forming bacteria that produces neurotoxins associated with botulism
Sources of Clostridium botulinum
Foodborne botulism = ingestion of toxin in improper canned foot
Infant botulism = intestinal infection e.g., consumption of honey
Wound botulism = infection of a wound, IV drug use
Adult intestinal botulism

Symptoms of Botulism
Weakness
Slurred speech
Blurred vision
Fatigue
Descending paralysis
Muscle weakness
Facial muscle paralysis
Effects on ANS: dry mouth, postural hypotension

Severe cases of Botulism lead to...
Reduced movement of respiratory muscles
Dyspnea
Respiratory failure
Risk factors for developing Botulism
- Foodborne botulism = tinned foods
- Infant botulism = infant age group
- Wound botulism = IV drug use
- Travelling to the USA (more cases there)
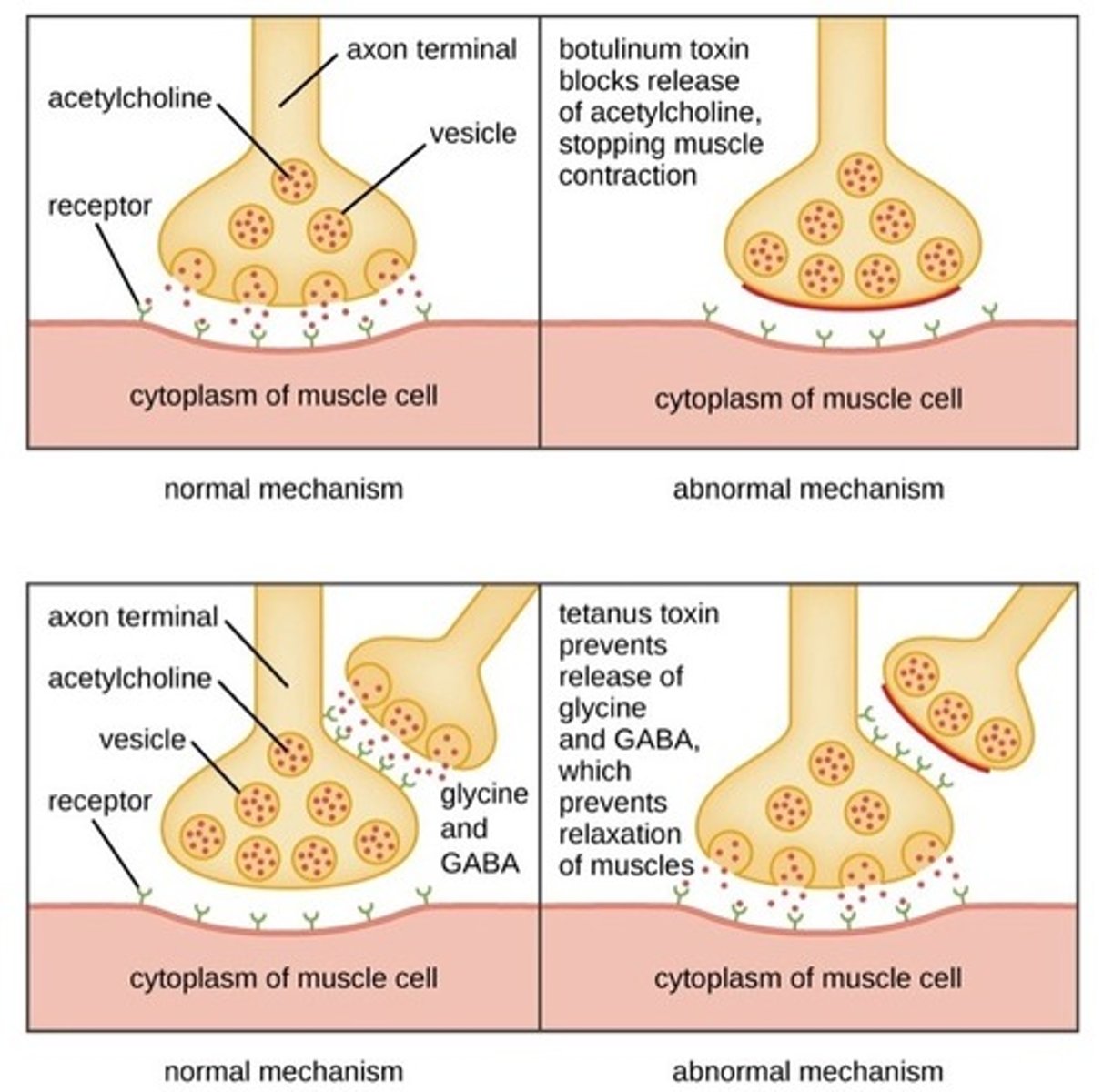
How does Botulinum neurotoxins (BoNT) work?
Block acetylcholine neurotransmitter signal transduction in peripheral α-motor neurons. This results in symptoms of slurred speech, peripheral muscle weakness and paralysis.
Differential diagnosis of botulism
Exclusion of...
- Guillain Barre syndrome
- Myasthenia gravis
- Stroke
Diagnosis of botulism
Botulinum toxin detection in blood, faeces or vomit
Treatment of botulism
Use of botulinum antitoxin which consists of antibodies A, B and E
- Supportive care
- Monitor respiratory function
- Mechanical ventilation
- Surgical treatment of any wounds
Antitoxin
Antibody with the ability to neutralise a specific toxin. These are used to treat or prevent diseases. Usually administered by injection.
Antitoxins are an example of ___ immunity
Passive
Clostridium tetani
Soil bacterium
Rod-shaped, spore-forming, Gram positive, motile (flagella) bacterium which is anaerobic
Causes tetanus

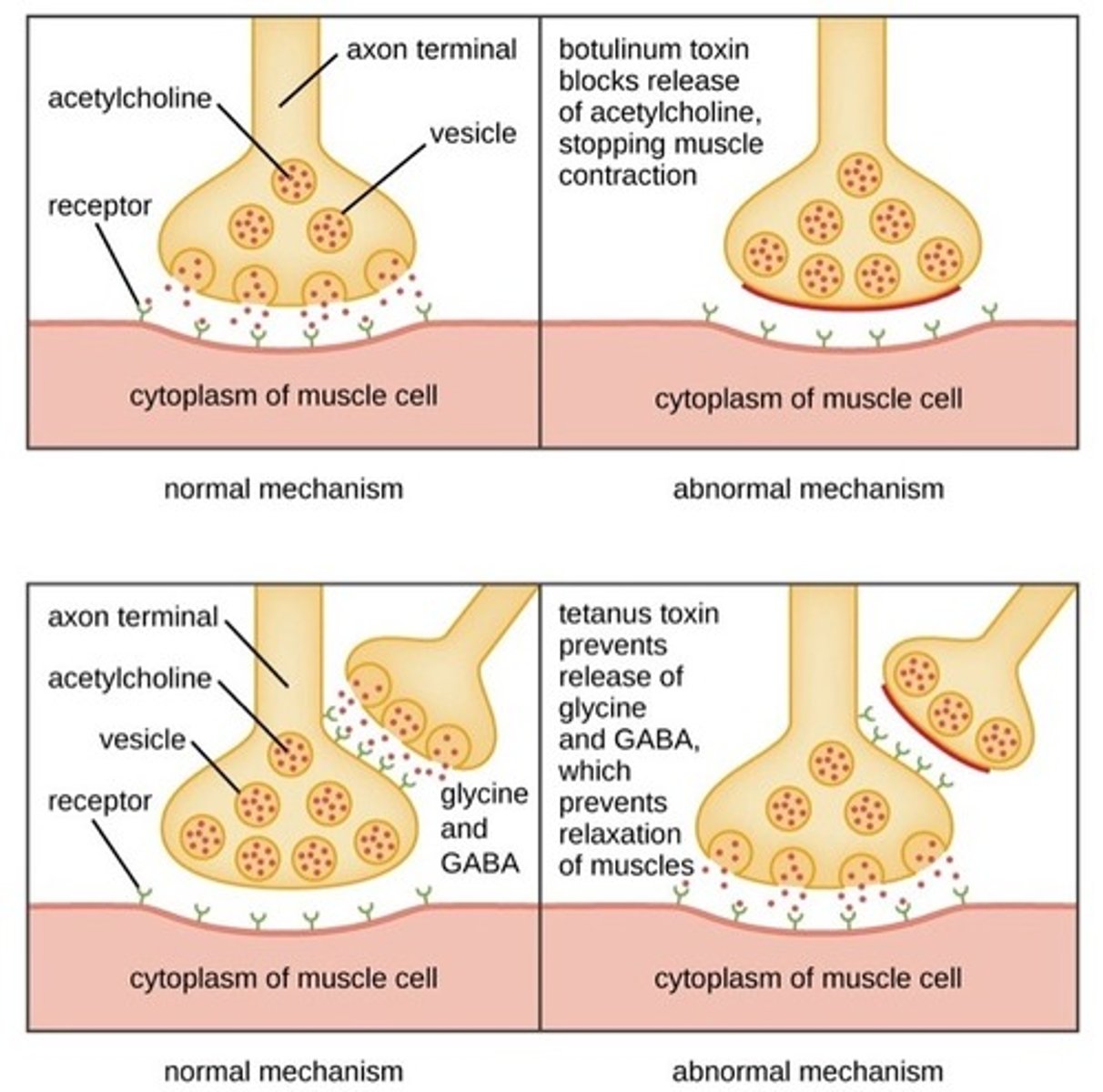
Tetanus pathogenesis
Tetanospasmin toxin travels from wound site to the neuromuscular junction (NMJ).
Here, it binds to presynaptic membranes of motor neurons and is taken up via vesicles into the axon.
It interferes with the release of neurotransmitters such as GABA and Glycine
If GABA cannot inhibit α-motor neurons, the firing rate increases, producing unopposed muscle contraction and spasms (opisthotonus and risus sardonicus)
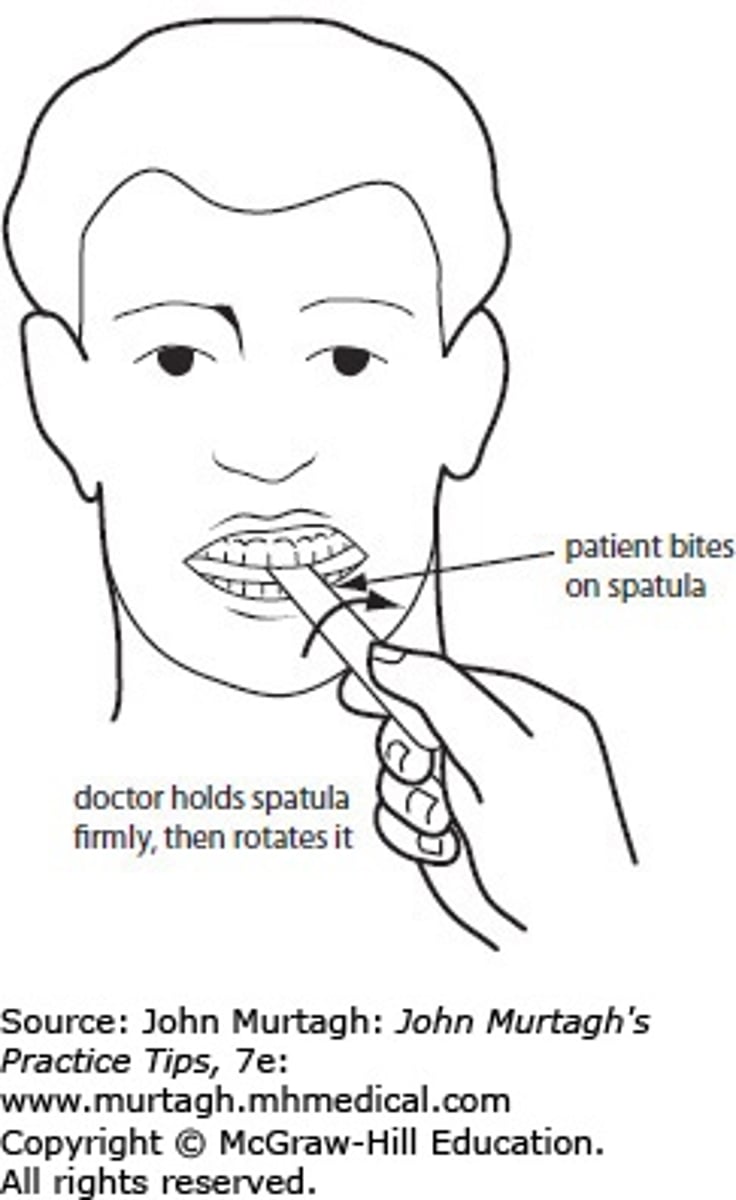
How is tetanus diagnosed?
- Diagnosis is based on presentation of tetanus symptoms
- Positive spatula test = touch posterior pharyngeal wall with soft-tipped instrument. If positive, patient will involuntarily bite down on the spatula (involuntary contraction of jaw muscles).
Treatment of tetanus
- Tetanus antitoxin (IV/IM)
- Antibiotic therapy: metronidazole
- Benzodiazepine e.g., diazepam to control muscle spasms
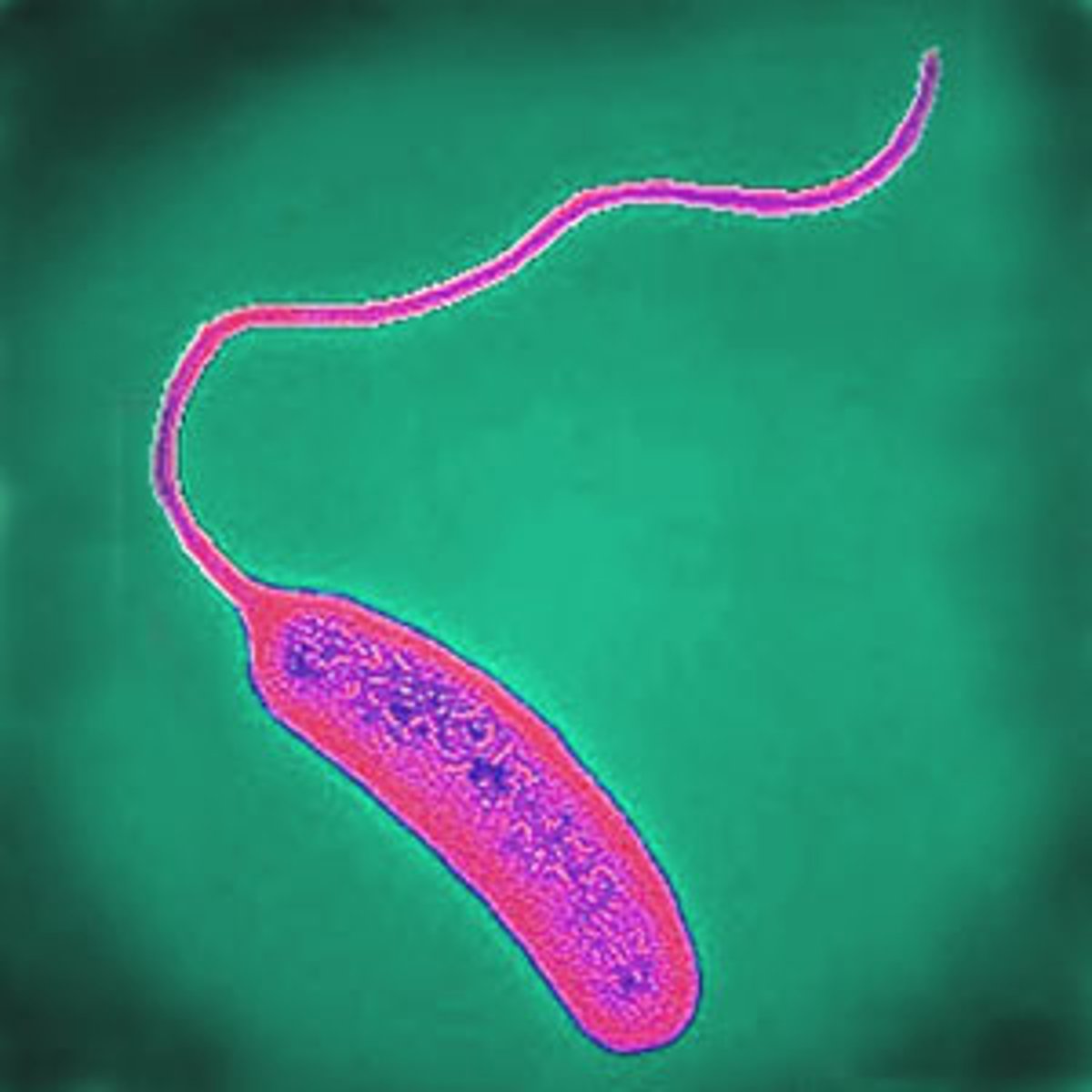
Vibrio cholerae
Comma-shaped, highly motile (flagellum), Gram negative bacteria
Responsible for cholera infections via ingestion of contaminated water
Symptoms of cholera
- Diarrhoea (looks like rice water) 20L/day
- Vomiting clear fluid
- Blue-grey skin from loss of fluids
- Wrinkled skin
- Kussmaul breathing
How is cholera spread
Contaminated water or food
Risk factors for cholera
Poor sanitation = lack of clean water access
Returning travellers from Asia/Africa
Pathogenesis of cholera
- Cholera toxin gains entry to the cell via ganglioside receptor on host intestinal epithelial cells
- Activates G protein, leading to increased adenylate cyclase activity
- ATP → c-AMP → activation of protein kinase
- ATP-mediated (ACTIVE) efflux of chloride ions via CFTR proteins, leading to loss of chloride ions
- Massive fluid secretion in small intestine
- Inhibition of NaCl absorption inhibits the large intestine from reabsorbing fluid, resulting in severe and water diarrhoea
Diagnosis of cholera
Rapid dipstick test
Stool or swab samples (lab)
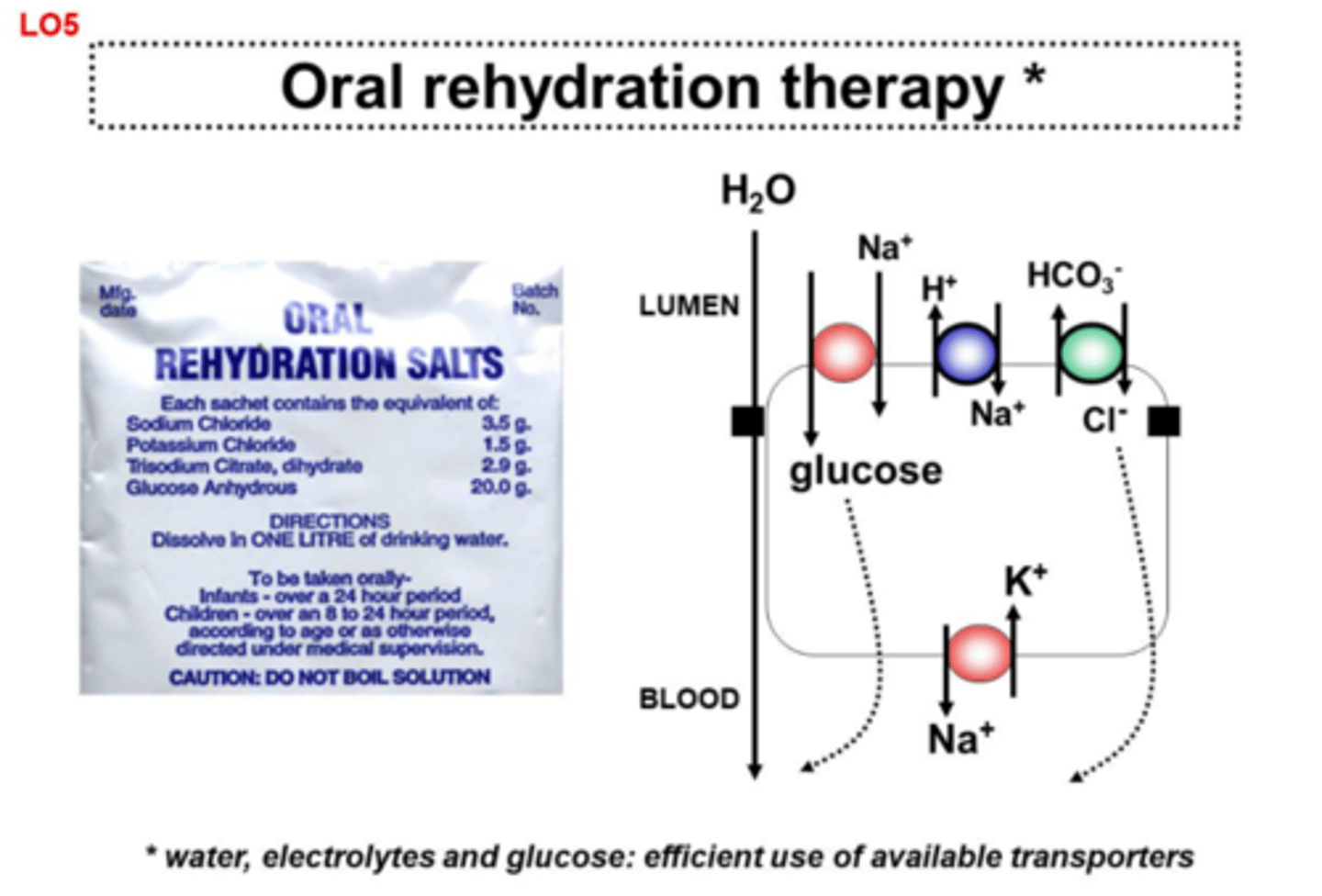
Treatment of cholera
Oral rehydration therapy
IV rehydration with Ringer's lactate
Antibiotic therapy = doxycycline
Prevention of cholera
Water and sanitation measures
Oral vaccines available for endemic/high-risk areas
Necrotising fasciitis
Flesh eating disease caused by bacterial infection, often from Staphylococcus aureus or Streptococcus pyogenes

Symptoms of necrotising fasciitis
- Fever
- Swelling
- Excessive pain
- Red/purple skin from thrombosis
- Reduced sensation in the skin
- Most often seen in extremities and genitals (Fournier's gangrene)
Risk factors for necrotising fasciitis
- Immunosuppression
- Diabetes mellitus
- Alcoholism
- Trauma
- Surgery
- IV drug use
- Herpes zoster (shingles)
Toxins involved in necrotising fasciitis
- M-protein = superantigen which is produced by Streptococcus pyogenes = prevents phagocytosis
- Alpha-toxin = produced by Clostridium perfringens (anaerobe) = causes excess platelet aggregation to block blood vessels and therefore lack oxygen supply to tissues (which causes bacteria to thrive)
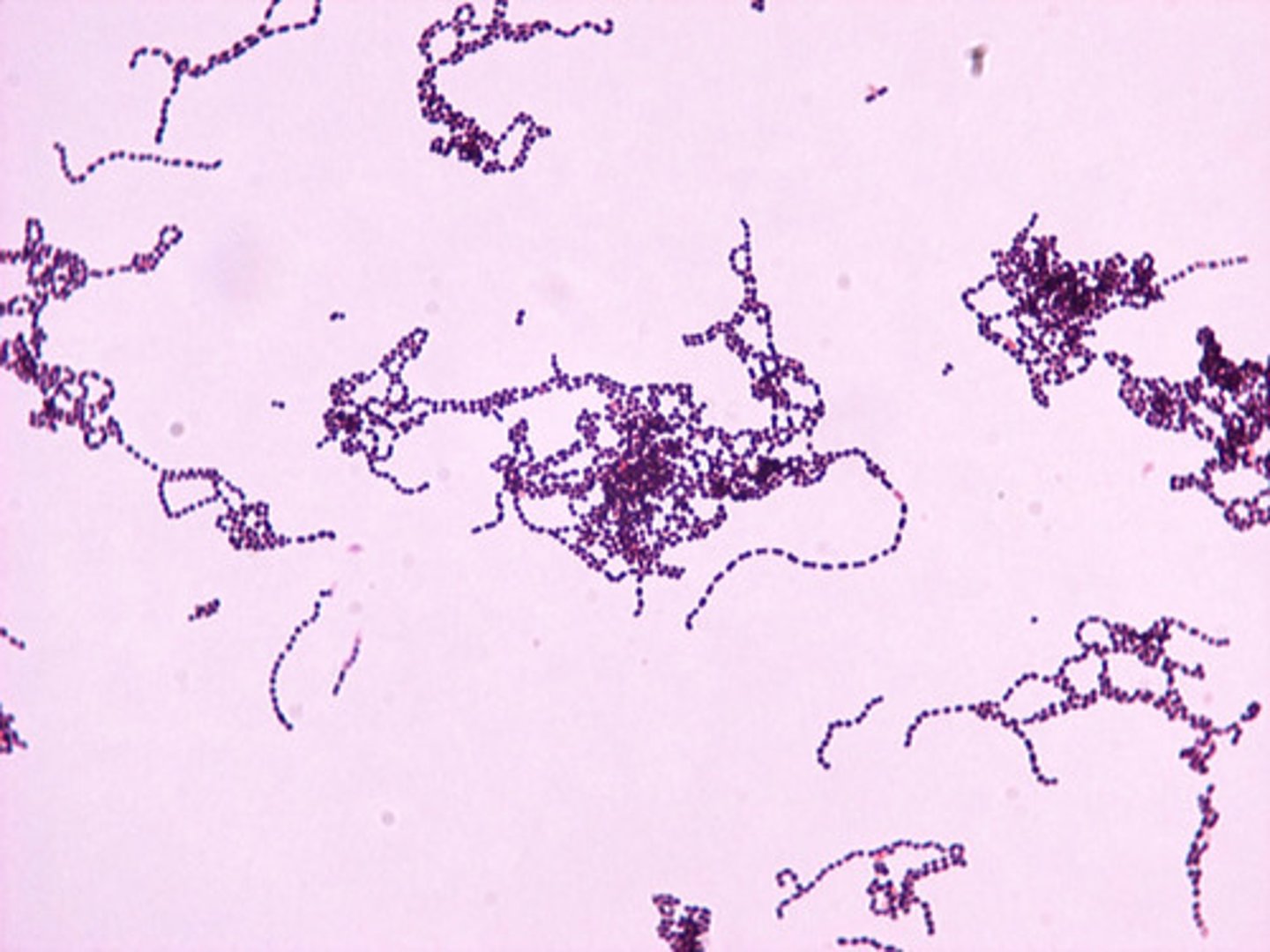
Streptococcus pyogenes
Gram positive cocci that grow in chains
Also known as Group A Streptococcus
Diagnosis of necrotising fasciitis
Elevated WBC
Serum sodium < 135 mmol/L
Raised CRP
Haemoglobin < 11 g/dL
Surgical exploration
Treatment of necrotising fasciitis
Surgical wound debridement of necrotic tissue
Empirical antibiotics = broad spectrum to cover Gram positive, Gram negative and anaerobes
Major virulence determinant of Streptococcus pyogenes and how it exerts its virulence
M protein
- Activates coagulation and thrombosis
- Induce production of IL-6, IL-1β and TNF-α in monocytes via Toll-like receptors (TLRs)
Endotoxin diseases (LPS)
Sepsis
Meningococcal disease
Exotoxin diseases
Botulism (BoNT)
Tetanus (Tetanus neurotoxin)
Cholera (CT)
Which of the following is NOT a risk factor for toxic shock syndrome?
a) Diabetes
b) Alcoholism
c) Caesarean delivery
d) Single use tampons
e) HIV +ive
e) HIV +ive
What is the most likely origin of a tetanus infection?
Soil
Which pathogen can cause necrotising fasciitis from the release of superantigen?
a) Staphylococcus aureus
b) Clostridium tetani
c) Streptococcus pyogenes (group A)
d) Neisseria meningitidis
c) Streptococcus pyogenes (group A)
Which toxin blocks the fusion of vesicles containing acetylcholine with the pre-synaptic membrane at the neuromuscular junction?
a) Clostridium botulinum
b) Clostridium tetani
c) Vibrio cholerae
d) Neisseria meningitidis
e) Streptococcus pyogenes (Group A streptococcus)
a) Clostridium botulinum
Give an example of a neurotoxin and which bacteria it is produced by
An example of a neurotoxin is the botulinum toxin. It is produced by the bacteria Clostridium botulinum.
Another example of a neurotoxin is the tetanospasmin toxin. This toxin is produced by the bacteria Clostridium tetani.
Explain how botulinum toxin produces the symptoms seen in botulism
Botulinum toxin acts by blocking acetylcholine neurotransmission signal transduction in peripheral alpha-motor neurons.
This leads to symptoms such as slurred speech, peripheral muscle weakness and paralysis which slowly progresses downwards (DESCENDING PARALYSIS).
Explain how tetanospasmin toxin produces the symptoms seen in tetanus
Tetanospamsin toxin acts by binding to presynaptic membrane of motor neurons and is taken up by the vesicles into the axon, where it interferes with the release of GABA.
GABA cannot inhibit the alpha-motor neurons – this leads the firing rate to increase and produce unopposed muscle contractions and spasms (risus sardonicus, opisthotonus).
Botulism and tetanus both affect the muscles. Explain how these diseases differ due to the toxins produced.
While botulism is characterised by flaccid paralysis, tetanus consists of spastic paralysis.
The botulinum toxin blocks the release of acetylcholine – this stops muscle contraction
The tetanospasmin toxin prevents the release of glycine and GABA, which prevents the relaxation of muscles – leading to uncontrolled muscle contractions and spasms.
What are the main symptoms of cholera and their causes?
Cholera symptoms include excess diarrhoea (which looks like rice water), vomiting clear fluid, blue-grey skin from loss of fluid (dehydration), wrinkled skin from dehydration and kussmaul breathing.
Causes of diarrhoea in cholera pathogenesis is due to cholera exotoxin. The cholera toxin enters cell via ganglioside receptors on the intestinal epithelial cells. Here it activates G proteins, activating adenylate cyclase activity – which produces c-AMP. The activation of various protein kinases leads to the ATP-mediated efflux of chloride ions via CFTR proteins. This leads to massive fluid secretion in the small intestine. Inhibition of NaCl absorption inhibits the ability of the large intestine to reabsorb fluid – resulting in heavy and watery diarrhoea and subsequent dehydration.
What is the antitoxin and how is it used to treat certain diseases?
An antitoxin is an antibody with the ability to neutralise a specific toxin.
These can be used to treat or prevent a disease.
These are usually administered via injection.
Antitoxins are an example of passive immunity.
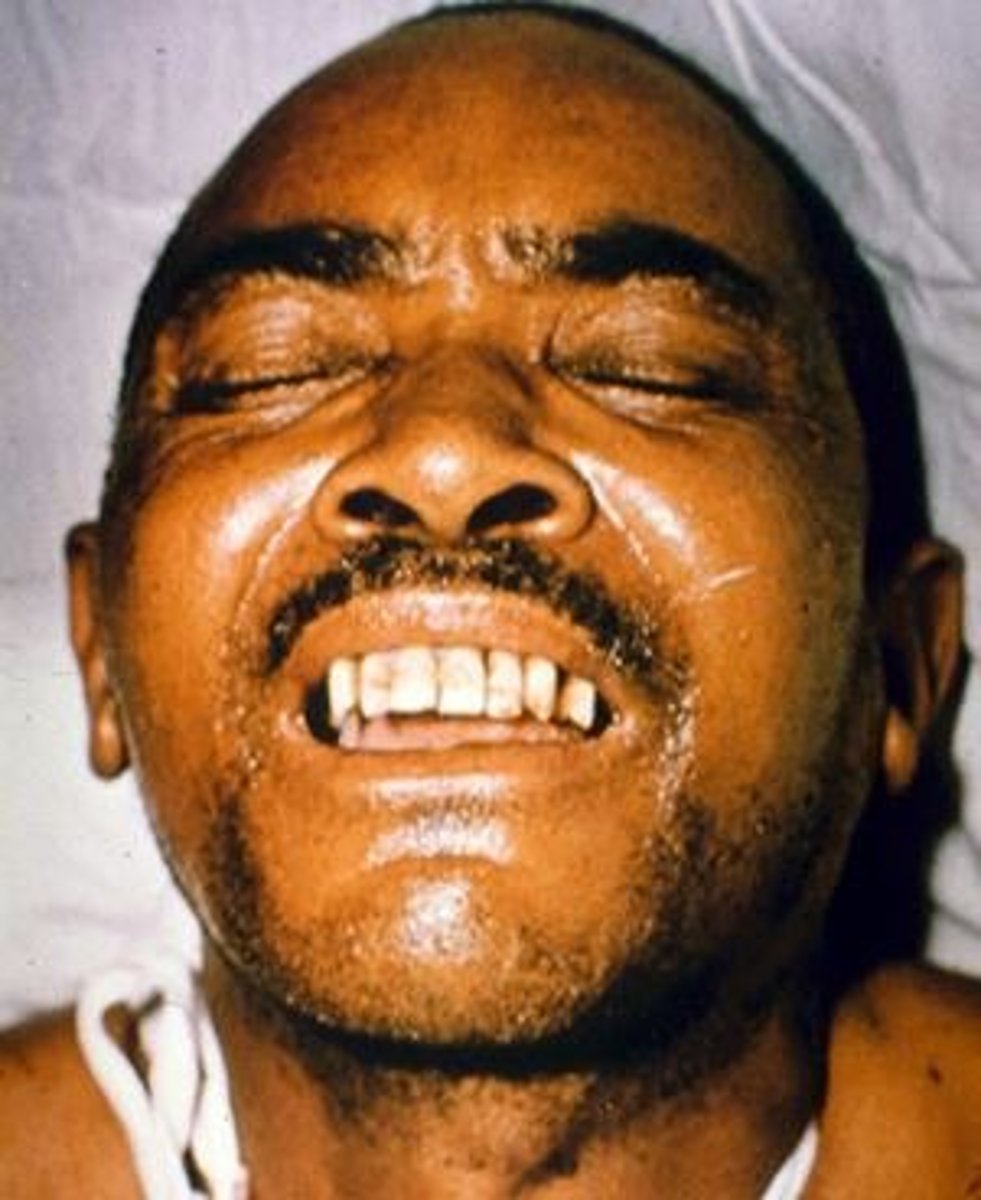
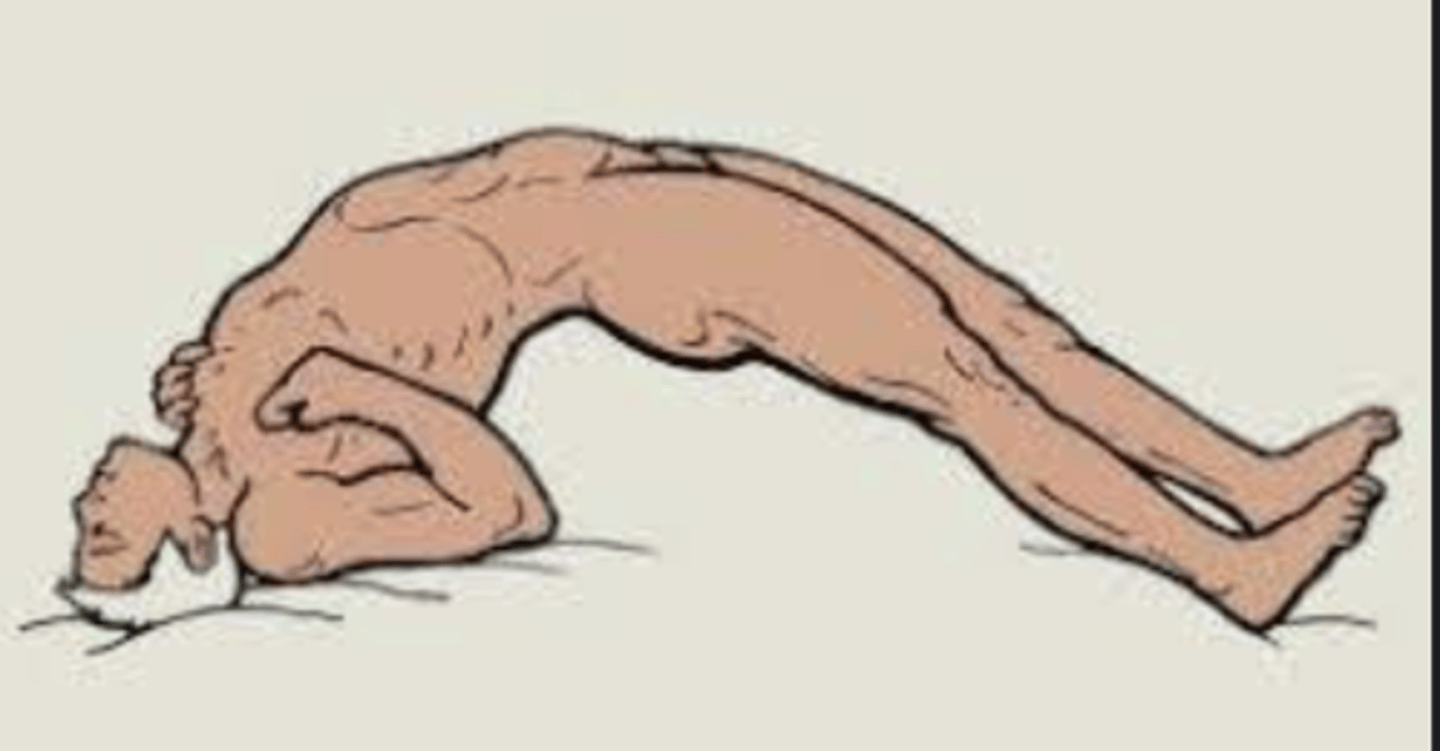
Opisthotonus (tetanus)
The back is rigid and arching, and the head is thrown backward.
Spasm of tetanus
Risus sardonicus (tetanus)
A highly characteristic, abnormal, sustained spasm of the facial muscles that appears to produce grinning
Spasm of tetanus