Addiction pathophysiology
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
30 Terms
What is addiction
ØDrug addiction is a progressive and often fatal behavioural syndrome characterized by compulsive drug seeking and consumption despite serious negative consequences.
Ø
ØCharacterized by:
⁃Overwhelming involvement with the use of a drug (compulsive use)
⁃The securing of its supply (compulsive drug-seeking)
⁃A high tendency to relapse after withdrawal
Drugs of abuse

Drugs abused - ocycotin
Addictive drugs take a horrific toll on humanity

can change their physical appearance
can have health affects
social consequences - increased abuse and violence
drug overdoses
economical and social damage
Recreational drug use

Drugs tend to be used for recreational use.
But what are the risk factors for addiction?
•Heritability
⁃Genetic variation
⁃
•Personality
⁃Not everyone who takes a drug once gets addicted to it!
⁃
•Environment
⁃Peer pressure
⁃Family environment (parental influence?)
Genetics and addiction
Some polymorphism that either predispose to or protect from drug addiction
Specific alleles for the genes encode alcohol dehydrogenase ADH1B and acetaldehyde dehydrogenase ALDH 2 (enzymes involved in metabolism of alcohol) are reportedly protective against alcoholism. When we do not have breakdown of alcohol and get accumulation of acetal aldehyde it can lead to aversive effects stopping the individual from wanting to use alcohol.
Polymorphism of the neuropeptide Y gene has been correlated with increased alcohol consumption
Single nucleotide polymorphisms of the gene encoding the mu-opioid receptor correlates with an increased likelihood of heroin abuse
Environmental factors
Environmental factors that have been consistently associated with the propensity to self- administer drugs include:
Structural factors: (low socioeconomic status,)
Proximal factors: parental drug use and dependence, poor quality of parenting, parental depression, sibling and peer influence, licensing laws)
Distal factors: drug availability, school, neighbourhood characteristics, advertising and the media.
Stress might be a common feature in a wide variety of environmental factors that increase the risk for drug abuse.
Stages
of addiction
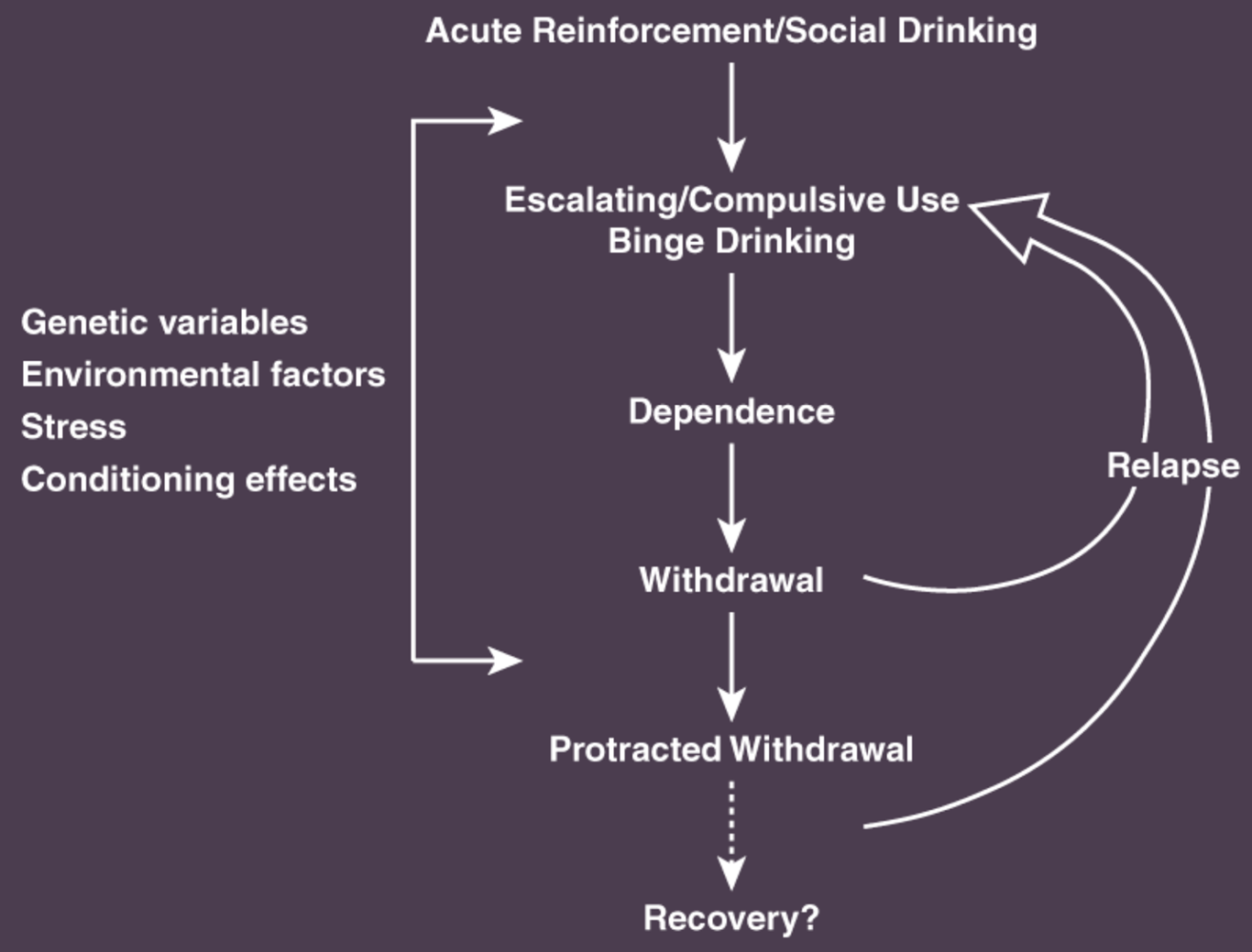
Acute enforcement in our brain - feels good when taking the drug. Brain remembers this pleasurable experience which leads to compulsive use of drug/alcohol. Withdrawal of drugs leads to withdrawal symptoms - makes them addicted.
Symptoms can be acute and last anywhere between 5 to 30 days. Another set called protracted withdrawal symptoms last longer - chance of recovery is much lower.
Genetic/environmental variables can play a part in the first initial transition from social to compulsive drug use or play a part in how the individual deals with withdrawal symptoms
“Drug addiction" -Both impulse control disorders and compulsive disorder
From a psychiatric perspective, drug addiction has aspects of both impulse control and compulsive disorders.
•Impulse control disorders are characterized by three factors:
1.an increasing sense of tension or arousal before committing an impulsive act.
2.pleasure, gratification, or relief at the time of committing the act.
3.regret, self-reproach, or guilt following the act.
•In contrast, compulsive disorders are characterized by two factors:
1.anxiety and stress before committing a compulsive repetitive behaviour.
2.relief from the stress by performing the compulsive behaviour.
Learning from pleasurable experiences (reward!)
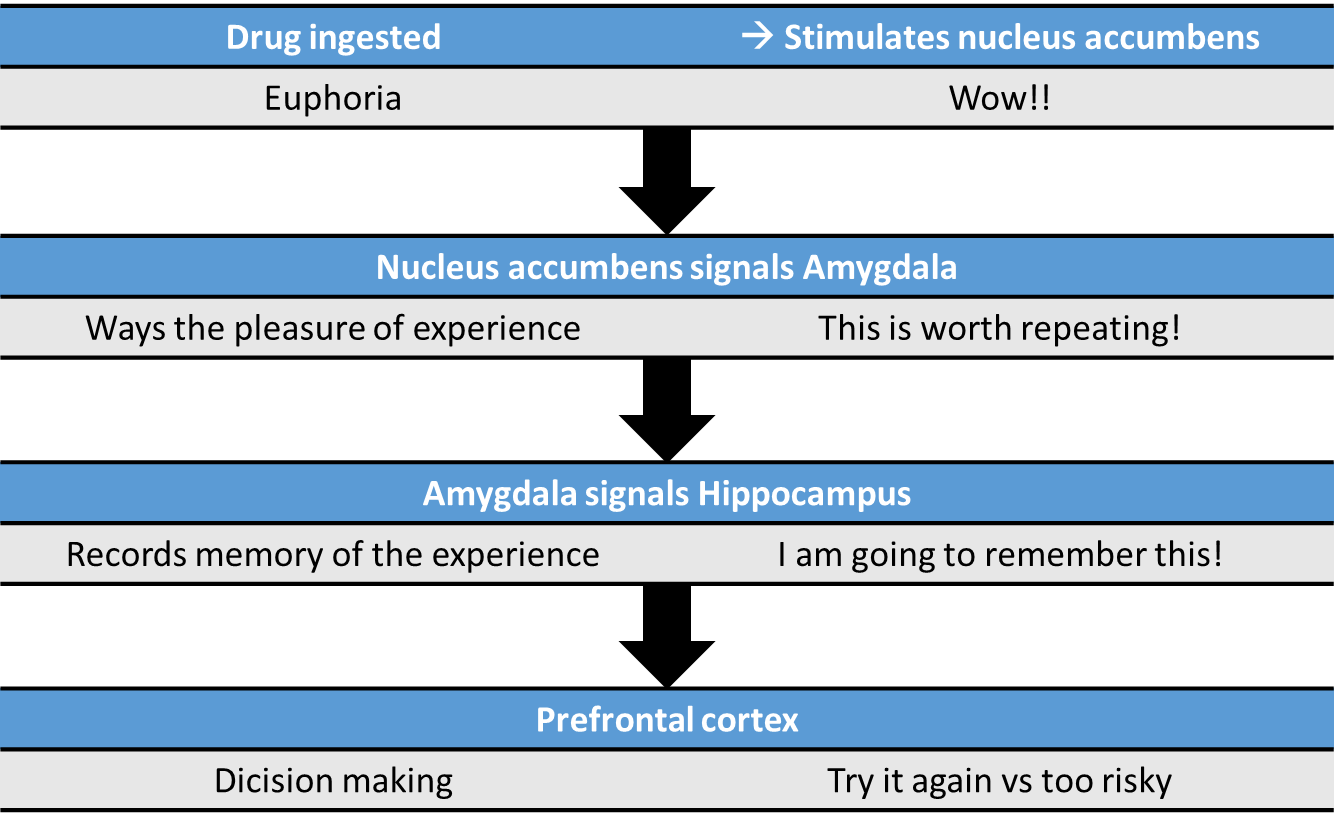
-. reward pathway
Neuronal circuits involved in addiction
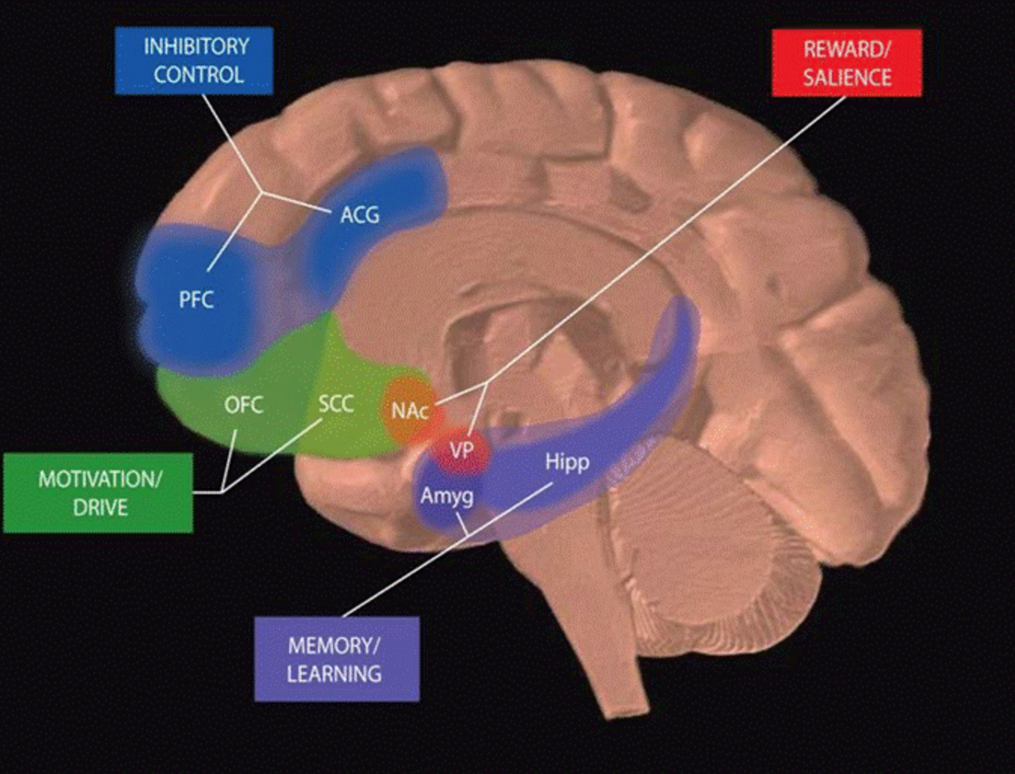
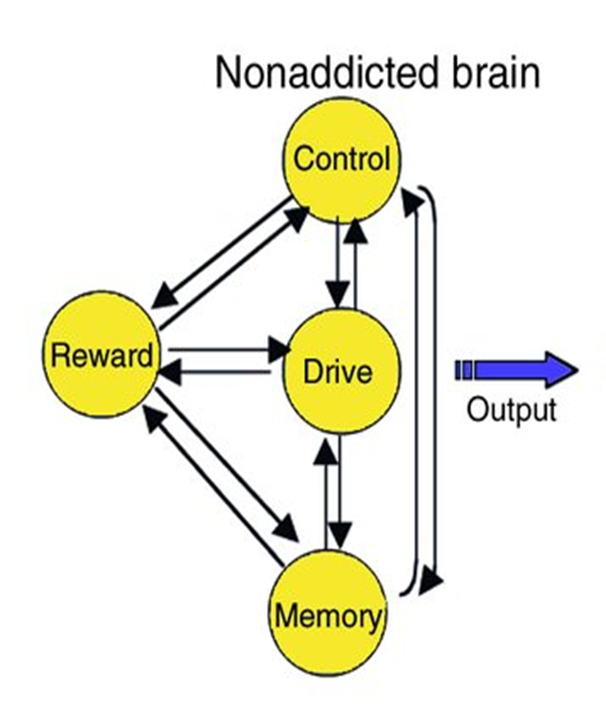
Normally in a non - addictive brain there is a perfect balance between the communication of all these different brain regions which leads to normal behaviour
PFC: prefrontal cortex; ACG: anterior cingulate cortex; OFC: orbitofrontal cortex; SCC: subcallosal cortex
NAc: nucleus accambens; VP: ventral pallidum; Amyg: amygdala; Hipp: hippocampus
The reward pathway (mesolimbic pathway)
•Mainly located in the limbic system and functions to monitor internal homeostasis, mediate memory, mediate learning and experience emotion
•
•
•Main structures include Includes the hypothalamus, amygdala, hippocampus, nucleus accumbens (NA), the ventral tegmental area (VTA), locus coeruleus and the prefrontal cortex
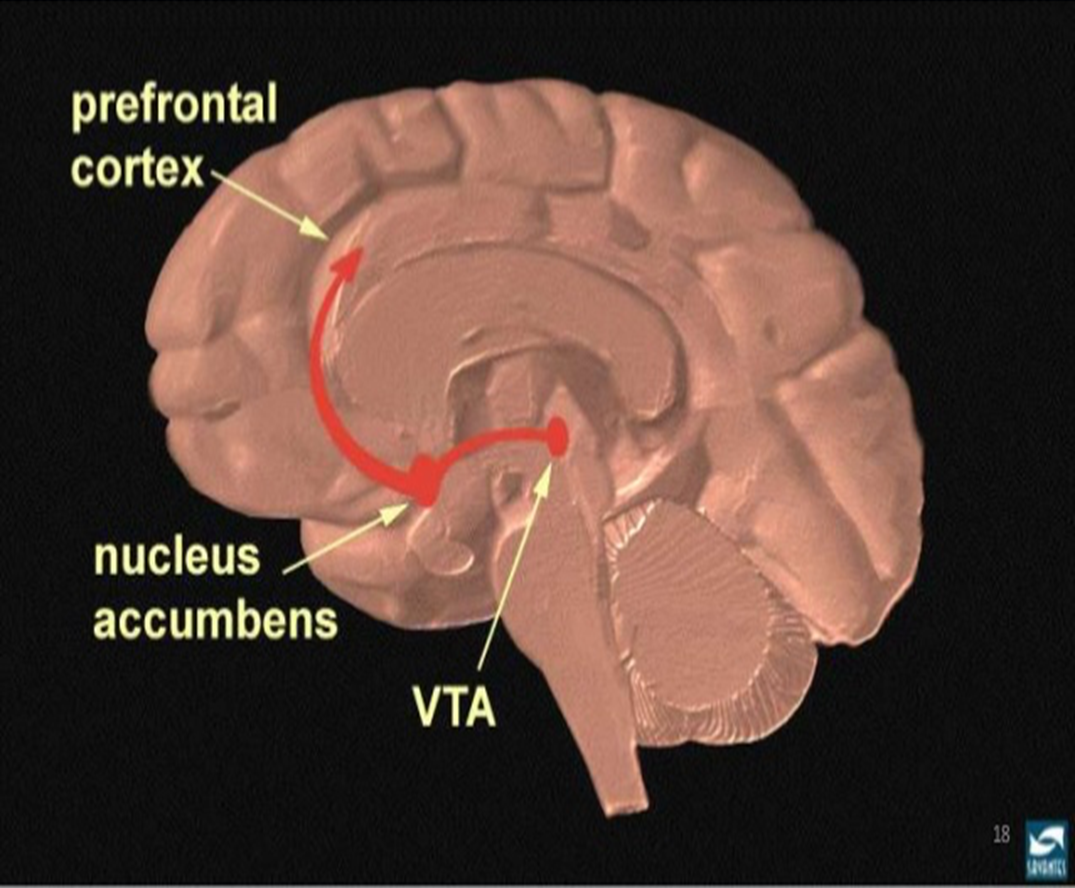
When exposed to rewarding stimuli the VTA gets activated and releases dopamine onto nucleus acumbens neurons which signal the pre frontal cortex leading to the feeling of being high and reward
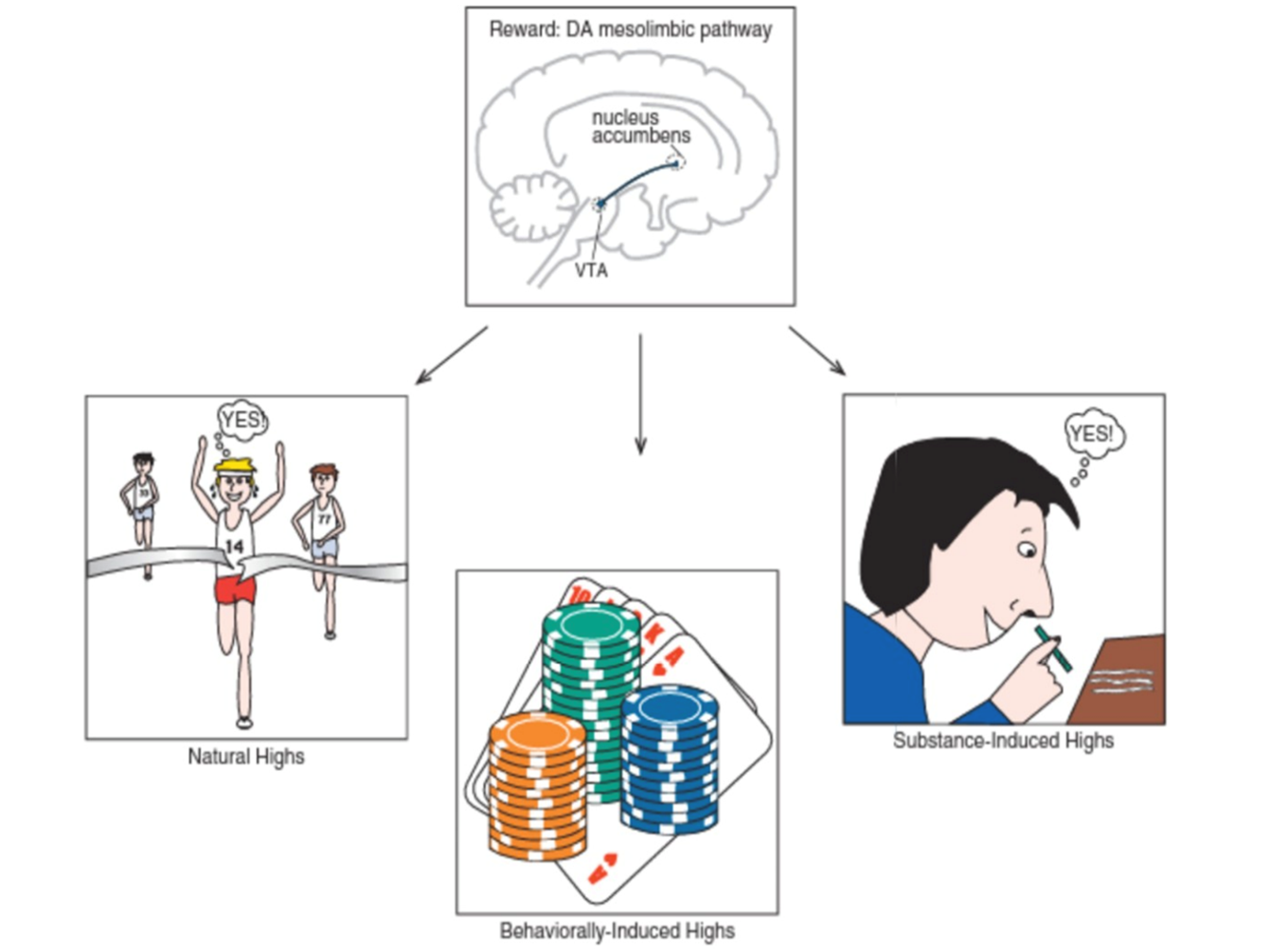
Reward pathway is stimulated by
ØNATURAL : Food, Sex, drinks
Ø
ØBEHAVIORS : e.g. gambling.
Ø
ØDRUGS : drugs of abuse (hyperactivity of reward pathway)
Ø
ØDISEASES : e.g. psychosis, schizophrenia
Rewards elevate dopamine levels in the brain
Dopamine is released by neurons in the VTC
Dopamine and the reward pathway
•Dopamine is the primary neurotransmitter of the reward pathway
•
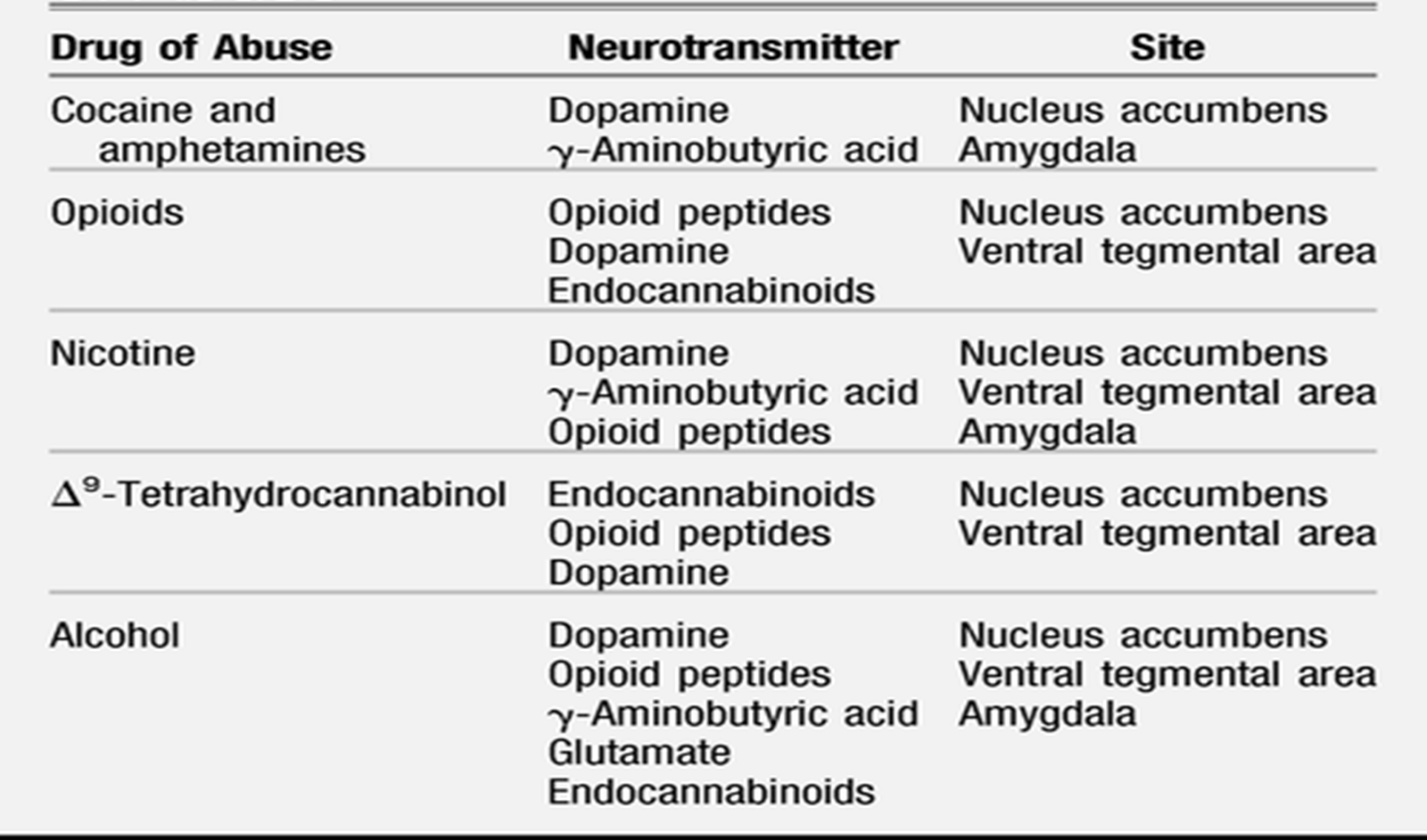
•All drugs of abuse increase dopamine levels in the brain reward pathway although they often act through separate mechanisms
•
•Drugs that are not abused have no effect on dopamine concentrations in the reward pathway
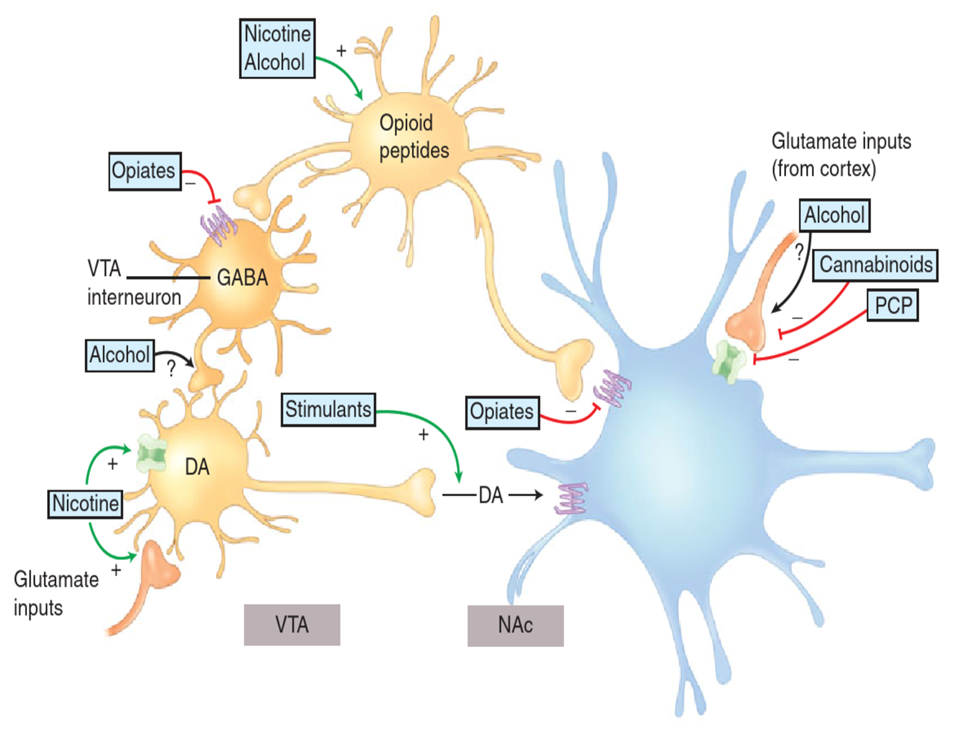
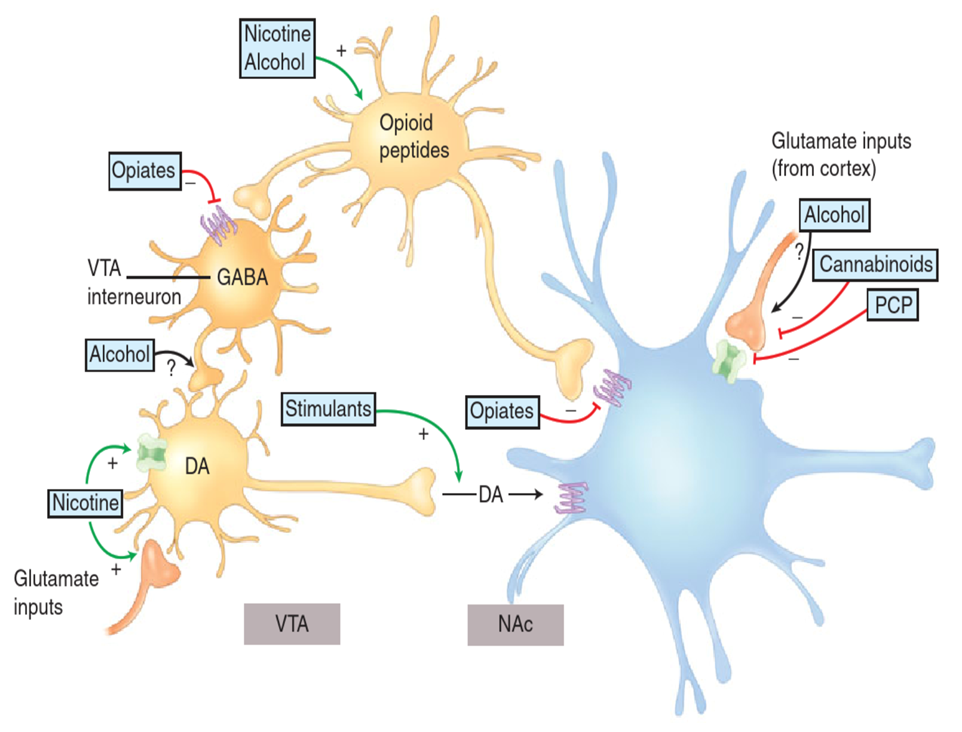
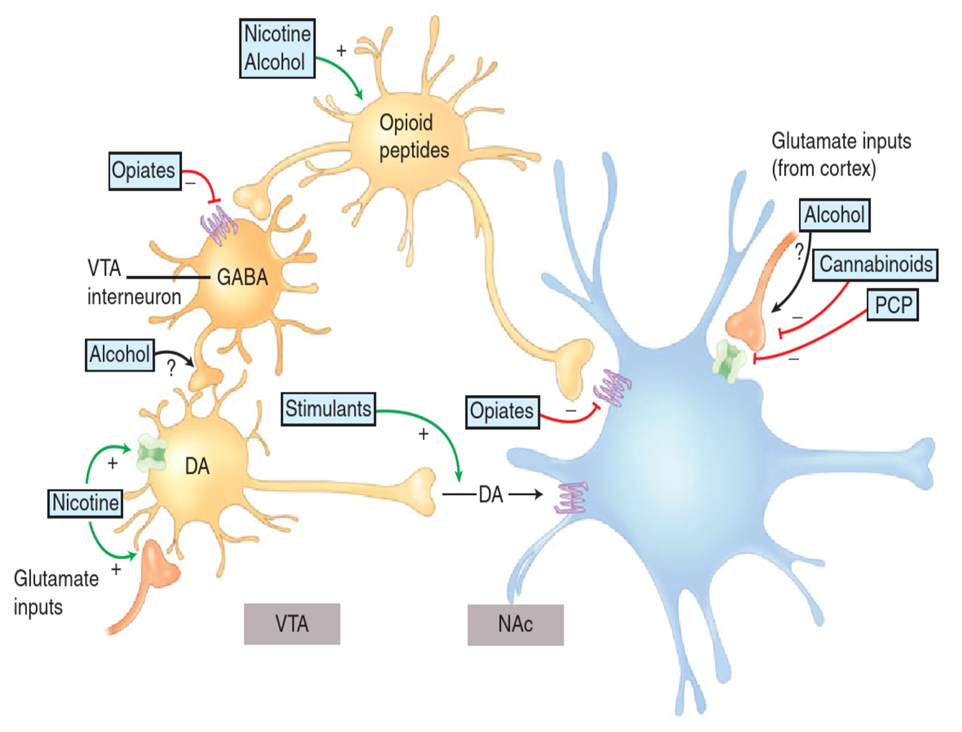
Neurochemicals involved in reward and addiction
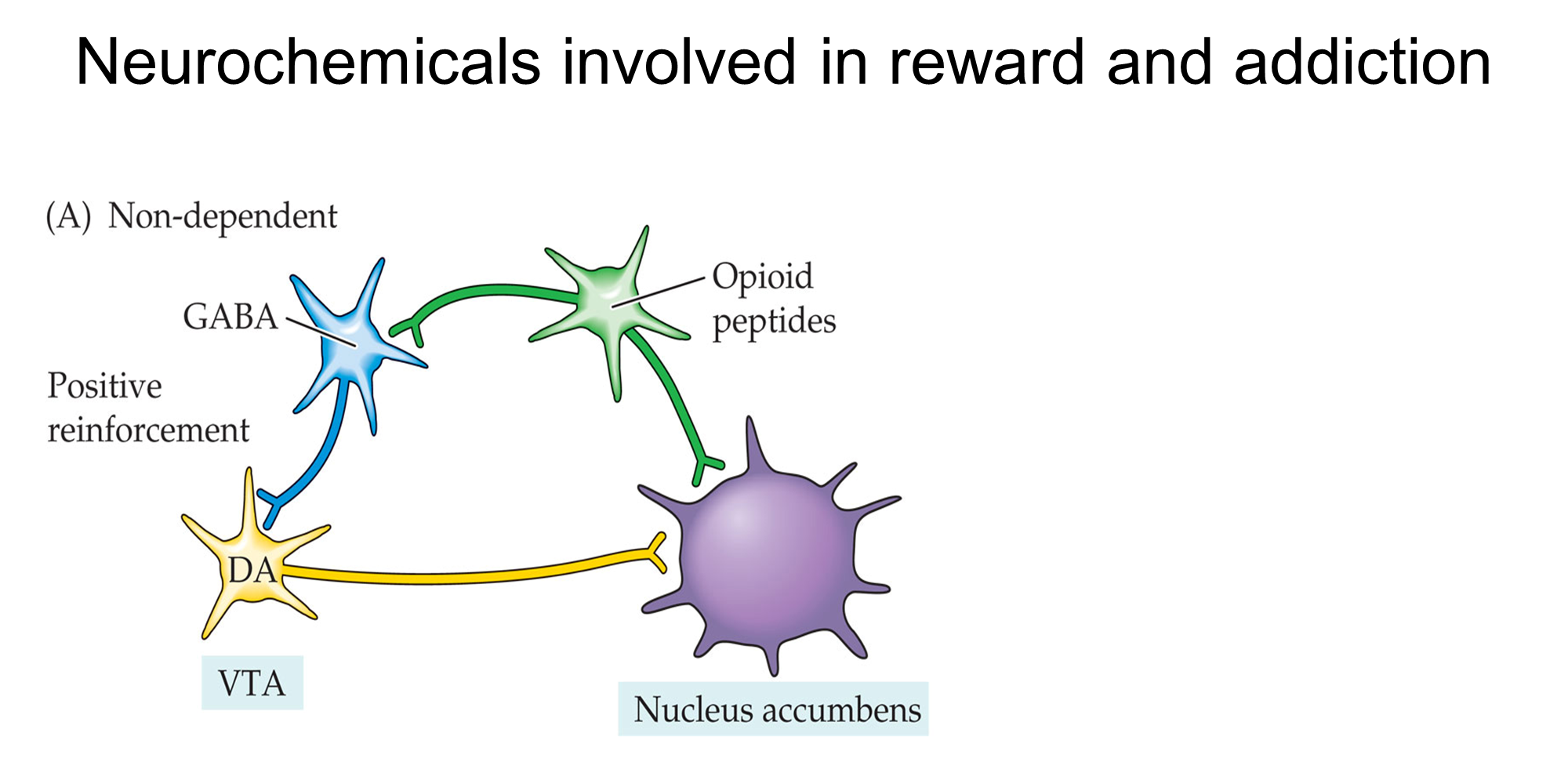
Addictive drugs include:
1.Substances that increase activity of opioid and DA neurons
●
2.Substances that decrease activity of GABAergic interneurons
How drugs of abuse activate the reward system
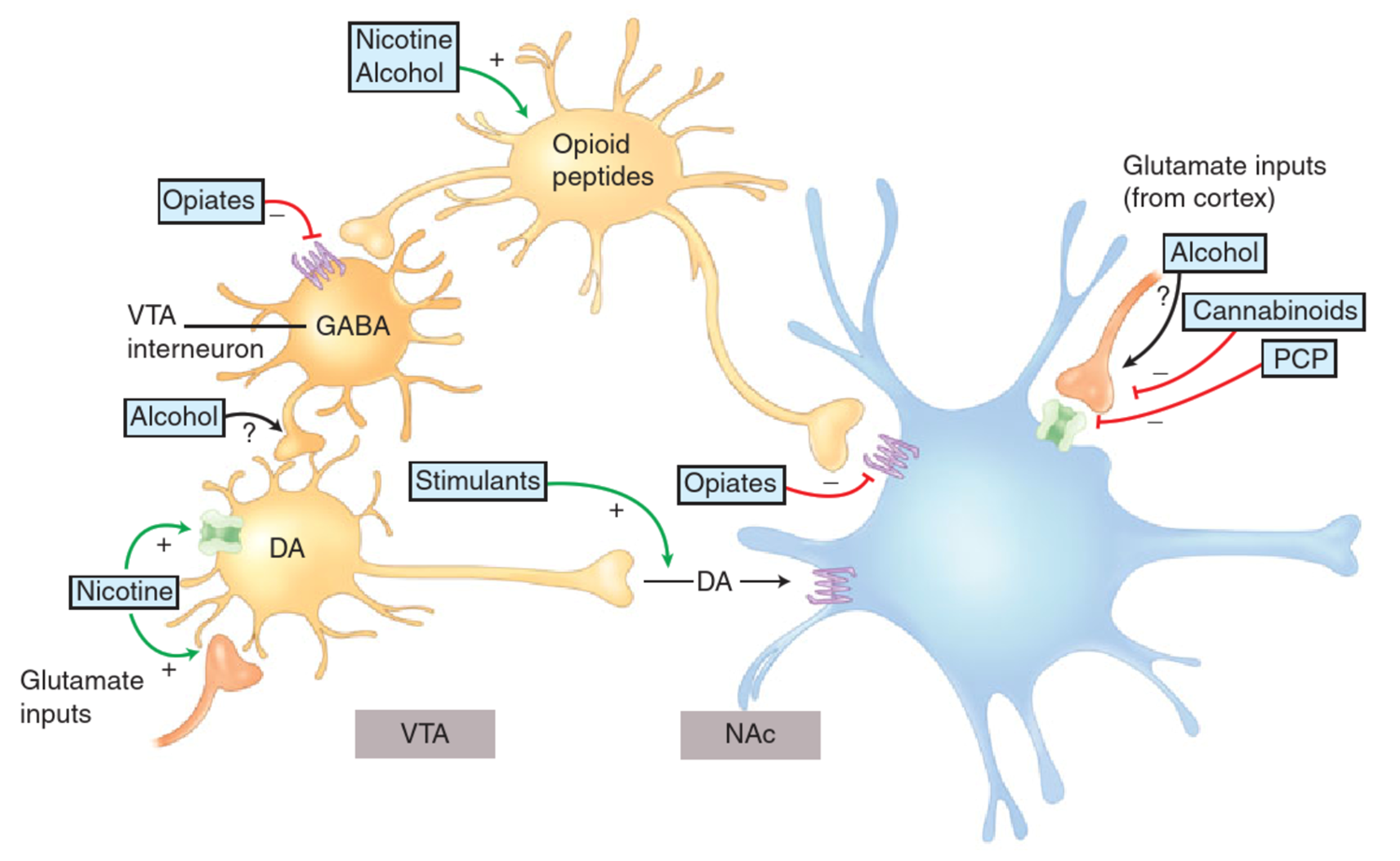
Opioids can act on GABAergic neurons and inhibit the activity of this which stimulates this pathway or they can directly inhibit the activity of nucleus accumbens neurons.
Nicotine can increase the activity of the opioid peptide producing neurones or increases the activity of dopaminergic neurones. Both of these will lead to the inhibition of nucleus accumbens neurones and stimulation of the reward pathway.
It is proposed that alcohol has inhibitory effect in glutamate being released into the nucleus accumbens from the cortex.
Same with cannabinoids and PCP, PCP also blocks NMDA receptors as well. NMDA receptors in glutamate are excitatory so they inhibit the reward pathway.
Cocaine can increase levels of dopamine in synapses.
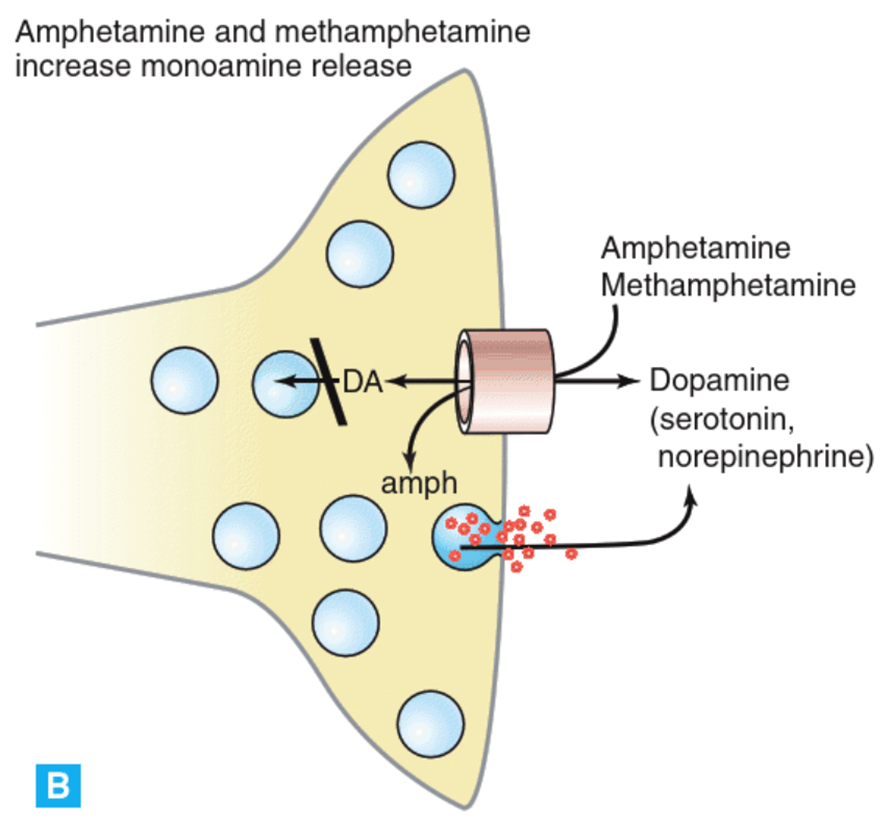
Psychostimulants increase monoaminergic transmission in the brain
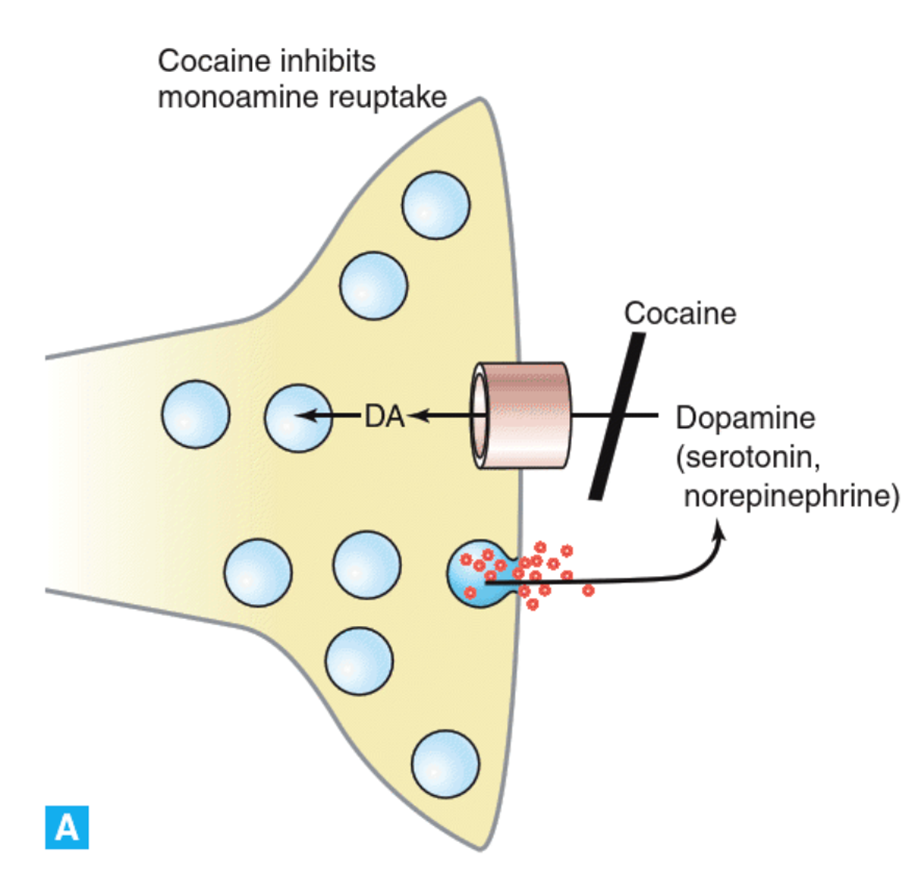
→ Cocaine inhibits the activity of these transporters which means the neurotransmitters are being released but they are not taken back up so they accumulate in the synapse and you get much more dopamine present here
→ increase monoaminergic transmission
Similar structure to monoaminergic molecules and as a result are taken up by transporters and packaged into vesicles instead of dopamine due to similar structure. As a result the neurone will start pumping them out leading to more dopamine being released.
Neurological substrates for the acute reinforcement of drug abuse
Altered neural integration in addiction
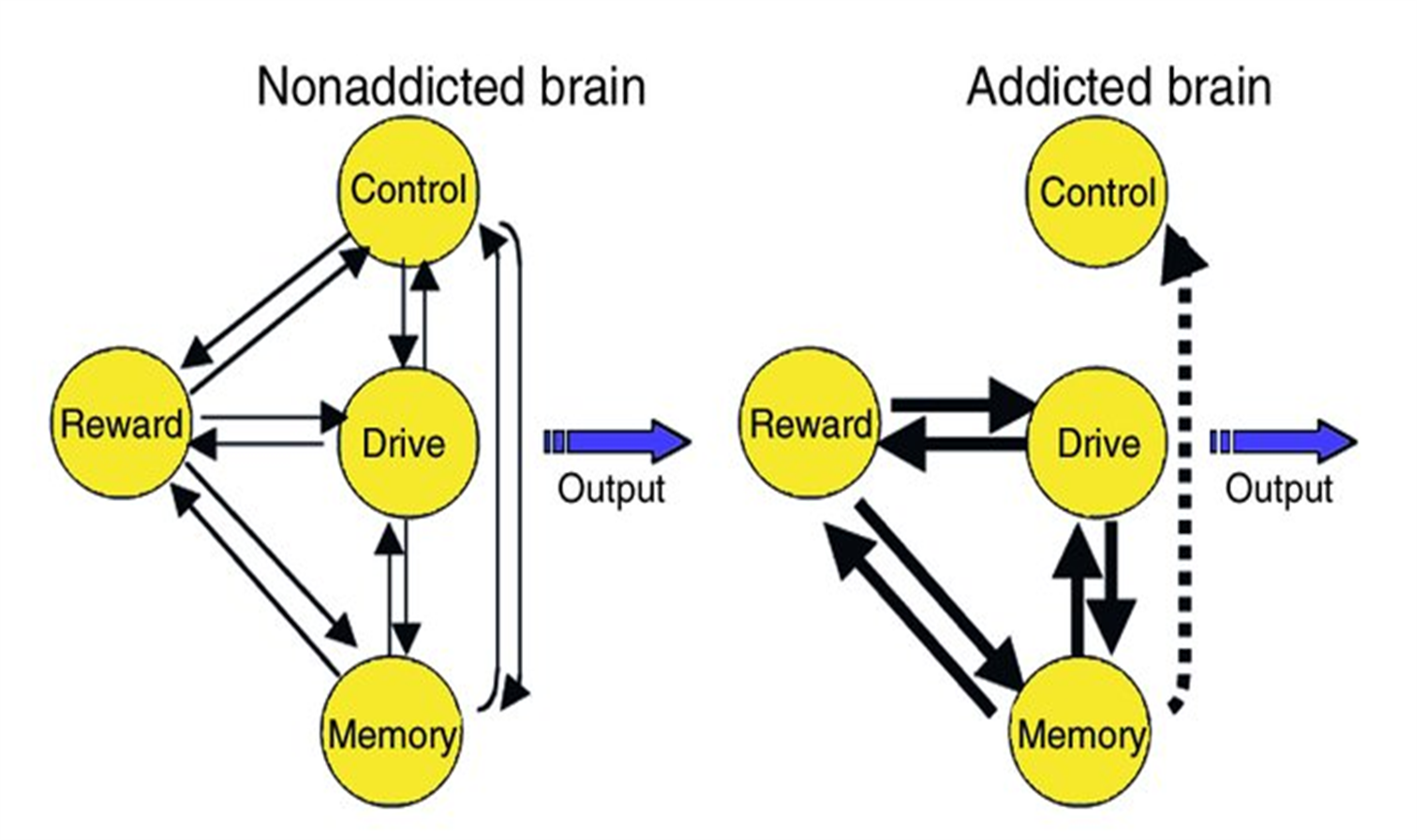
In addicted brain there is a stronger communication between the reward, drive and memory pathway which means the individual has to drive to feel the reward of the drug. The more they do this the more it strengthens the memory of having the motivation to find the drug and use it. → now the inhibitory pathway is much weaker
How drugs alter our brain and behaviour?
1.Acute reinforcement of the reward pathway
●
2.Repeated drug use → Compulsion to seek and take drugs
●
3.Loss of control in limiting intake due to withdrawal symptoms
●
4.Development of tolerance → more drugs required to produce high
Compulsion to seek & take the drug
Natural rewards - release of DA
→
DA binds to receptors on post synaptic neuron on nucleus accumbens, stimulating the reward pathway
→
Reward and high
→
DA transporter pumps DA back into the cell (cocaine prevents it)
→
DA levels in the synapse increased → receiving neuron stimulated constantly - EUPHORIA {alteration of brain circuits – natural rewards no longer produce high}
→
Use of drug becomes obligatory
Loss of control in limiting intake
After cocaine use – DA levels fall below normal
→
Low mood
→
To alleviate – uses drug again
Tolerance
Chronic use of cocaine
→
Continuous above normal levels of DA
→
Reduction in no. of DA receptors
→
Larger amount of drug needed to get same HIGH
Incentive sensitization theory of addiction
1. Hypersensitization
Compulsive seeking of drugs derives from a progressive and persistent hypersensitization of dopamine neural systems.
-Neural sensitization = increasing ability of a drug to stimulate specific neurobehavioral systems.
-Even intermittent use of drugs leads to this sensitization.
-
2. Increased wanting
The neural systems involved lead to a motivational increase in incentive salience or, more simply, 'wanting.'
-This is not 'liking' or pleasure, which is an outcome, but a driver of the addictive action
-It may have pleasurable associations, perhaps of anticipated pleasure.
3. Repetition
Repetition of the addictive behaviour, typically taking drugs, leads to increased sensitization.
Addicts thus want the drugs more even if they know the harmful effects and would like to stop.
4. Conscious desire
The preconscious neural wanting becomes conscious desire.
This translation process can lead to us seeking something without really knowing why.
Negative reinforcement and withdrawal symptoms (role of noradrenaline)
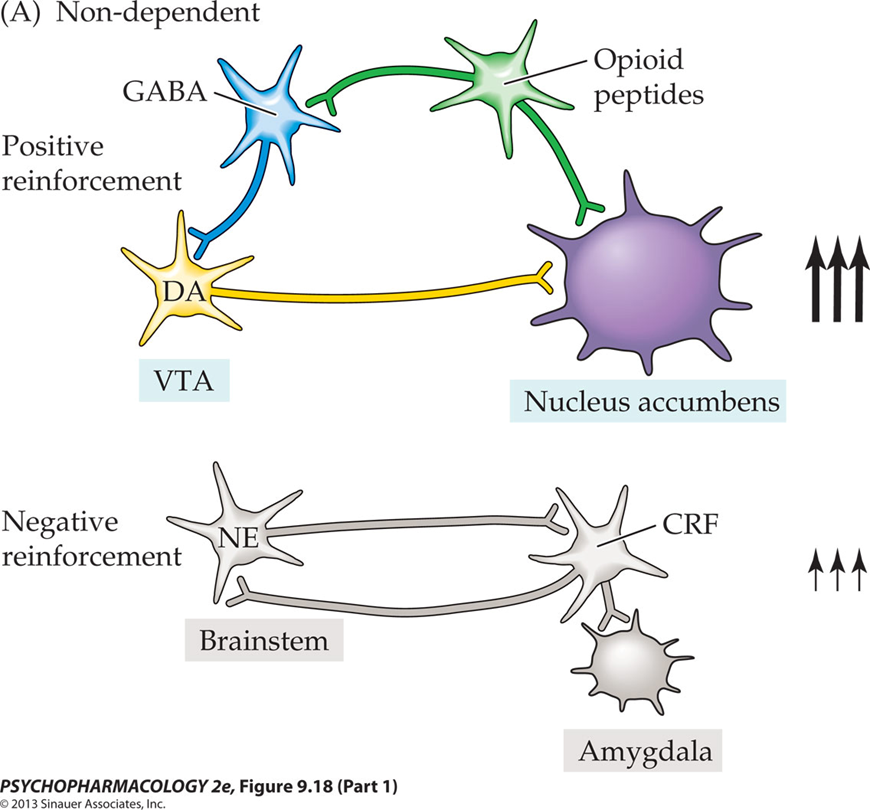
Negative re - enforcement pathway - includes the hypothalamus, amygdala and locus cerelius. Normally this is not stimulated, however when becoming dependant on drugs you get dysfunction of the reward pathway and increase in activity of the negative reinforcement pathway.
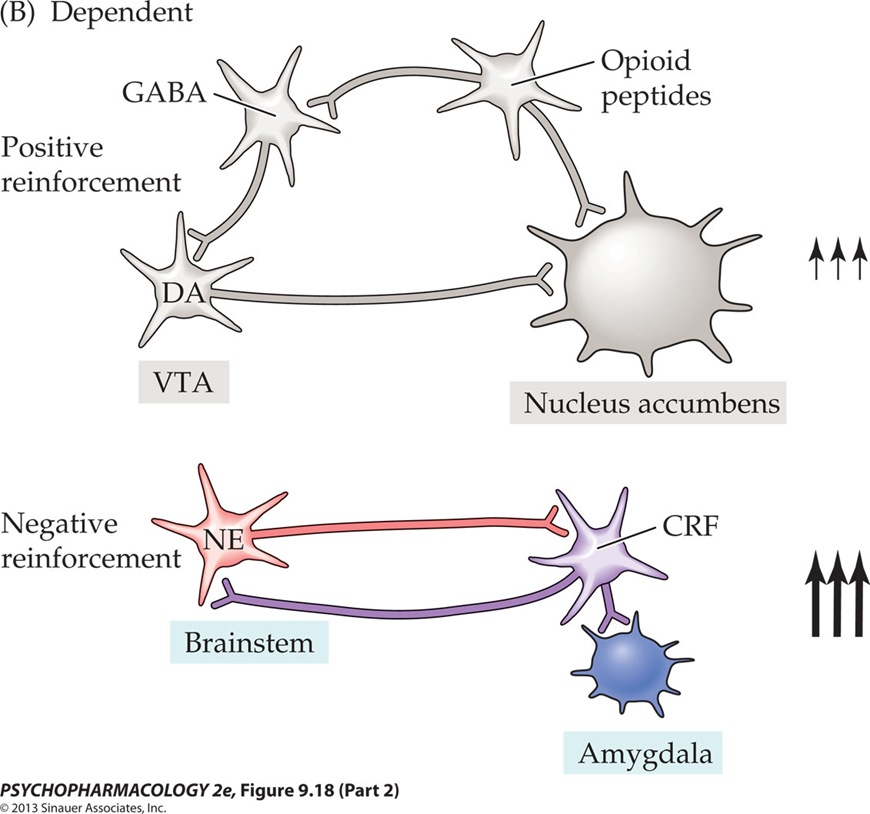
→ CRF which is a neurotransmitter being released from the hypothalamic neurones which works on the amygdala and the brain stem, and the overall effect of this pathway is a lot of noradrenaline being released → seems to be culprit of withdrawal symptoms.
Primary pathways through which stress, drugs of abuse, and drug-associated stimuli are hypothesized to trigger relapse of drug-seeking behaviour
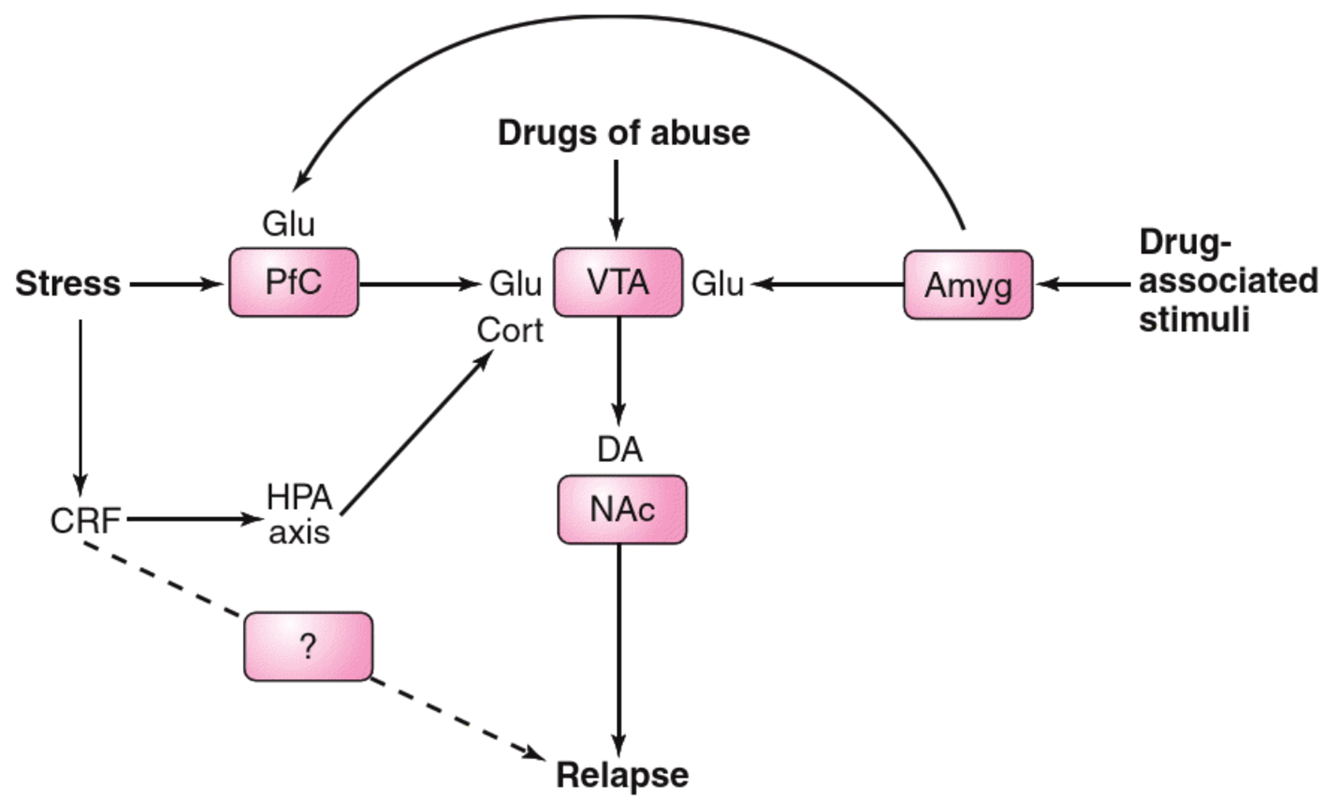
drugs of abuse and drug associated stimuli can trigger a relapse of drug seeking behaviour as a result of drug withdrawal.
drug abuse activates VTA which releases dopamine onto the nucleus accumbens neurones giving the feeling of high and euphoria.
drug associated stimuli can activate the amygdala which releases glutamate onto VTA neurones activating them and causing release of dopamine → want to take drugs again
Stress does the same thing but it can also release CRF and stimulate hypothalamic pituitary axis leading to release of glucocorticoid which can again activate VTA neurones.
Treatment of ethanol dependence
ØAlcohol dependence ‘alcoholism’ (4-5% of population)
Ø
ØAcute abstinence syndrome: Benzodiazepines, clonidine (alpha2 adrenergic agonist → blocks release of noradrenaline) and propranolol (beta adrenergic blocker - stops affect of noradrenaline)
Ø
ØTo reduce alcohol consumption and block the reward system: Disulfiram (inhibits aldehyde dehydrogenase responsible for braking down alcohol) and naltrexone (opioid antagonist - inhibit activity of opioid receptors, stopping effect of opioids on the reward pathway)
Ø
ØTo reduce craving: Acamprosate (Thought to interact with neuronal NMDA receptors and calcium channels on NAc neurons)
Treatment of psychostimulant addiction
ØTreatment of psychostimulant addiction (e.g. cocaine) generally unsatisfactory
Ø
ØBased on findings that dopamine system is down regulated, dopamine agonist (bromocriptine and amantadine) have been tried (little clinical benefit) -
Ø
ØAntidepressant drugs have been used to help with depression-like symptoms
Ø
ØCurrently, cognitive-behavioural therapies seems the most effective therapy to prevent relapse
Treatment of opioid addiction
Treatment of opiate addiction is twofold:
•Detoxification (to minimize physical withdrawal symptoms)
⁃Methadone and clonidine can be used
•Treatment of emotional-motivational symptoms to maintain abstinence, more difficult
⁃Some success with a combination of naloxone and buprenorphine (a partial μ-opioid receptor agonist)