Chapter 15- Disorders of Motor Function
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
20 Terms

During a late night study session, a pathophysiology student reaches out to turn the page of her textbook. Which of the following components of her nervous system contains the highest level of control of her arm and hand action?
A) Cerebellum
B) Thalamus
C) Basal ganglia
D) Frontal lobe
D) Frontal lobe
Feedback: While intentional movement involves input from various components of the nervous system including the cerebellum, thalamus, and basal ganglia, primary control and coordination are controlled by the motor cortex in the frontal lobe.

A patient is asked to stand with feet together, eyes open, and hands by the sides. Then the patient is asked to close his eyes while the nurse observes for a full minute. What assessment is the nurse performing?
A) Segmental reflex
B) Posture
C) Proprioception
D) Crossed-extensor reflex
C) Proprioception
Information from the sensory afferents is relayed to the cerebellum and cerebral cortex and is experienced as proprioception or the sense of body movement and position independent of vision. The knee-jerk reflex is a form of stretch reflex. The crossed-extensor reflex serves to integrate motor movements, so they function in a coordinated manner.

A clinician is conducting an assessment of a male client suspected of having a disorder of motor function. Which of the following assessment findings would suggest a possible upper motor neuron (UMN) lesion?
A) The client has decreased deep tendon reflexes.
B) The client displays increased muscle tone.
C) The client's muscles appear atrophied.
D) The client displays weakness in the distal portions of his limbs.
B) The client displays increased muscle tone.
Feedback: UMNs typically produce increased muscle tone, while hyporeflexia, muscle atrophy, and weakness in the distal portion of limbs are more commonly indicative of LMN lesions.
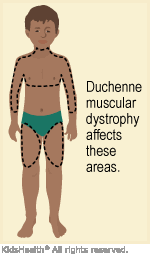
The parents of a 3-year-old boy have brought him to a pediatrician for assessment of the boy's late ambulation and frequent falls. Subsequent muscle biopsy has confirmed a diagnosis of Duchenne muscular dystrophy. Which of the following teaching points should the physician include when explaining the child's diagnosis to his parents?
A) “Your son's muscular dystrophy is a result of faulty connections between muscles and the nerves that normally control them.”
B) “He'll require intensive physical therapy as he grows up, and there's a good chance that he will outgrow this problem as he develops.”
C) “Your son will be prone to heart problems and decreased lung function because of this.”
D) “His muscles will weaken and will visibly decrease in size relative to his body size throughout his childhood.”
C) “Your son will be prone to heart problems and decreased lung function because of this.”
Feedback: Muscular dystrophy is associated with cardiac and respiratory complications. It does not involve the nervous system, and the problem will not dissipate with time. While muscles become weakened, pseudohypertrophy means that their size does not decrease.

The unique clinical presentation of a 3-month-old infant in the emergency department leads the care team to suspect botulism. Which of the following assessment questions posed to the parents is likely to be most useful in the differential diagnosis?
A) “Have you ever given your child any honey or honey-containing products?”
B) “Is there any family history of neuromuscular diseases?”
C) “Has your baby ever been directly exposed to any chemical cleaning products?”
D) “Is there any mold in your home that you know of?”
A) “Have you ever given your child any honey or honey-containing products?”
Feedback: Botulism in infants is frequently attributable to honey. Family history is not a relevant consideration given the bacterial etiology, and mold and chemical cleaning products are not known to predispose to botulism toxicity.

A 22-year-old female college student is shocked to receive a diagnosis of myasthenia gravis. What are the etiology and most likely treatment for her health problem?
A) Autoimmune destruction of skeletal muscle cells; treatment with intensive physical therapy and anabolic steroids
B) A decline in functioning acetylcholine receptors; treatment with corticosteroids and intravenous immunoglobulins
C) Cerebellar lesions; surgical and immunosuppressive treatment
D) Excess acetylcholinesterase production; treatment with thymectomy
B) A decline in functioning acetylcholine receptors; treatment with corticosteroids and intravenous immunoglobulins
Feedback: The etiology of myasthenia gravis involves a deficiency of acetylcholine receptors at neuromuscular junctions. Treatment can include corticosteroid therapy and intravenous immunoglobulins. Destruction of skeletal muscle cells, cerebellar lesions, and excess acetylcholinesterase are not noted to underlie the disease.

A toddler is displaying signs and symptoms of weakness and muscle atrophy. The pediatric neurologist suspects it may be a lower motor neuron disease called spinal muscular atrophy (SMA). The patient's family asks how he got this. The nurse will respond
A) “This could result from playing in soil and then ingesting bacteria that are now attacking his motor neurons.”
B) “No one really knows how this disease is formed. We just know that in time, he may grow out of it.”
C) “This is a degenerative disorder that tends to be inherited as an autosomal recessive trait.”
D) “This is a segmental demyelination disorder that affects all nerve roots and eventually all muscle groups as well.”
C) “This is a degenerative disorder that tends to be inherited as an autosomal recessive trait.”
Feedback: SMA is a distinctive group of degenerative disorders involving LMNs that begins in childhood. Answer choice A relates to botulism. It is known which gene is involved in SMA. Answerchoice D does not describe SMA.

Which of the following individuals is likely to have the best prognosis for recovery from his or her insult to the peripheral nervous system? An adult
A) who developed rhabdomyolysis and ischemic injury after a tourniquet application.
B) who suffered a bone-depth laceration to the shoulder during a knife attack.
C) who had his forearm partially crushed by gears during an industrial accident.
D) who had nerves transected during surgery to remove a tumor from the mandible.
C) who had his forearm partially crushed by gears during an industrial accident.
Feedback: Crushing-type injuries carry a higher possibility of nerve function recovery than do lacerations and insults resulting from ischemia.
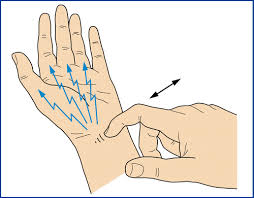
A nurse working in a busy orthopedic clinic is asked to perform the Tinel sign on a patient having problems in his hand/wrist. In order to test Tinel sign, the nurse should give the patient which of the following directions?
A) “Stand tall, arms at your side, shut your eyes; place the tip of your index finger to your nose.”
B) “Hold your wrist in complete flexion; keep it in this position for 60 seconds; how does your hand feel after placing it in a neutral position?”
C) “I'm going to tap (percuss) over the median nerve in your wrist; tell me what sensation you feel while I am doing this. Does the sensation stay in the wrist or go anywhere else?”
D) “I'm going to tap this tuning fork and place it on the side of your thumb; then tell me what you are feeling in your hand and wrist.”
C) “I'm going to tap (percuss) over the median nerve in your wrist; tell me what sensation you feel while I am doing this. Does the sensation stay in the wrist or go anywhere else?”
Feedback: A positive Tinel sign will help diagnose carpal tunnel syndrome. The patient will have a tingling sensation radiating into the palm of the hand when lightly percussed over the median nerve at the wrist. Answer choice B relates to Phalen sign, which is also a test to help diagnose carpel tunnel syndrome. Answer choice D is not the medical test for carpal tunnel syndrome

During a flu shot clinic, one of the questions the student nurse asks relates to whether the patient has had Guillain-Barré syndrome in his medical history. The patient asks, “What is that?” How should the nursing student reply?
A) “A type of paralysis that affects movement on both sides of the body that may even involve the respiratory muscles”
B) “Swelling of your arm where you got your flu shot, and maybe your eyes and lips had some swelling as well”
C) “A degenerative disease where you have trouble walking without the help of a cane or walker”
D) “Influenza-like illness where you had fever and chills for 2 to 3 days after your last flu shot”
A) “A type of paralysis that affects movement on both sides of the body that may even involve the respiratory muscles”
Feedback: Guillain-Barré syndrome is an acute immune-mediated polyneuropathy. The majority of people report having had an acute, influenza-like illness before the onset of symptoms. It progresses along the ascending muscle weakness of the limbs, producing a symmetric flaccid paralysis. The rate of disease progression varies, and there may be disproportionate involvement of the upper or lower extremities. Option B is anaphylaxis following the flu shot. It is not a degenerative disease

A 60-year-old male office worker presents to a clinic complaining of new onset of lower back pain that has been worsening over the last 6 weeks. The nurse knows which of the following components of his physical assessment and history is most indicative of a serious pathological process (like aortic aneurysm or cancer)?
A) His pain is relieved by extended bed rest.
B) When supine, passive rising of his leg to 90 degrees results in hamstring pain.
C) He has needed regular nonsteroidal anti-inflammatory drugs to control the pain in recent weeks.
D) His onset of pain has been gradual, and he has no prior history of lower back problems.
D) His onset of pain has been gradual, and he has no prior history of lower back problems.
Feedback: The gradual onset of back pain unrelated to injury and initial presentation after age 50 are considered red flags for more serious pathologies such as aortic aneurysm, malignancy, or compression fracture. Pain that is aggravated by lying down is a red flag for malignancy or infection. The onset of hamstring pain at 90 degrees of hip flexion is a normal finding. The need for and use of NSAIDs for lower back pain relief are not indicative of a serious pathology in and of itself.

A middle-aged woman is brought to the emergency room after a minor auto accident. Her gait is staggering and unsteady; her speech is slurred; and she displays slight nystagmus. The police officer who brought her in says she has not been drinking. Her blood pressure is very high. Which of the following health problems most likely underlies her present state?
A) Multiple sclerosis
B) Guillain-Barré syndrome
C) Myasthenia crisis
D) Cerebellar damage caused by a cerebrovascular accident
D) Cerebellar damage caused by a cerebrovascular accident
Feedback: Cerebellar damage can resemble the effects of alcohol, because alcohol affects the cerebellum. This woman has not been drinking, but her high blood pressure puts her at risk for cerebrovascular accident.

A 70-year-old male has been diagnosed with a stroke that resulted in an infarct to his cerebellum. Which of the following clinical findings would be most closely associated with cerebellar insult?
A) Flaccid loss of muscle tone
B) Difficulty in starting movement, stopping movement, and maintaining rhythmic movements.
C) Tremor, rigidity, and bradykinesia
D) Unsteady gait and difficulty in speaking and swallowing
D) Unsteady gait and difficulty in speaking and swallowing
Feedback: An unsteady gait characterizes cerebellar ataxia, and both swallowing and speaking are partly the domain of the cerebellum. Flaccid loss of muscle tone is not noted to accompany cerebellar insult, and difficulties with starting movement, stopping movement, and maintaining rhythmic movements are indicative of basal ganglia disorders. Tremor, rigidity, and bradykinesia are associated with Parkinson disease.
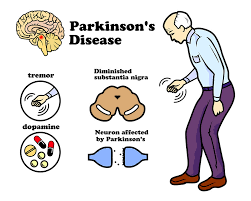
The geriatrician providing care for a 74-year-old man with diagnosis of Parkinson disease has recently changed the client's medication regimen. What is the most likely focus of the pharmacologic treatment of the man's health problem?
A) Maximizing acetylcholine release from synaptic vesicles at neuromuscular junctions
B) Preventing demyelination of the efferent cerebellar pathways
C) Increasing the functional ability of the underactive dopaminergic system
D) Preventing axonal degradation of motor neurons
C) Increasing the functional ability of the underactive dopaminergic system
Feedback: Antiparkinson drugs act by increasing the functional ability of the underactive dopaminergic system. The cerebellar pathways, acetylcholine levels, and axonal degradation are not components of the etiology of Parkinson disease.
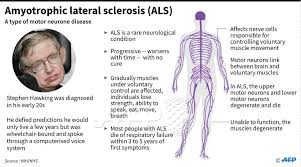
A 47-year-old woman was diagnosed with amyotrophic lateral sclerosis 3 years ago and has experienced a progressive onset and severity of complications. She has been admitted to a palliative care unit due to her poor prognosis? What assessments and interventions should the nursing staff of the unit prioritize in their care?
A) Assessment and documentation of cognitive changes, including confusion and restlessness
B) Regular pain assessment and administration of opioid analgesics as needed
C) Assessment of swallowing ability and respiratory status
D) Cardiac monitoring and administration of inotropic
medications
C) Assessment of swallowing ability and respiratory status
Feedback: The late stages of ALS normally involve deterioration in swallowing and speech and in the respiratory musculature. Cognitive changes are not common complications, and pain and cardiac complications are not noted to be paramount in the course of ALS.
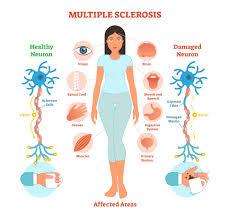
A 41-year-old woman was diagnosed with multiple sclerosis (MS) 7 years ago and is sharing her story with members of an MS support group, many of whom have been diagnosed recently. Which of the following aspects of her health problem should the woman warn others to expect at some point in the progression of the disease? Select all that apply.
A) Debilitating fatigue
B) Progressive loss of visual acuity
C) Gradual development of a resting tremor
D) Loss of mental acuity
E) Shuffling gait
A) Debilitating fatigue
B) Progressive loss of visual acuity
D) Loss of mental acuity
Feedback: Fatigue, visual deficits, and cognitive disturbances are all noted manifestations of MS, while respiratory function and GI function are not normally affected. Shuffling gait is usually associated with Parkinson disease.

The nurse should anticipate she will need to teach the newly diagnosed multiple sclerosis patient how to give injections if he is prescribed which medication to modify the course of the disease by reducing exacerbations?
A) Corticosteroids
B) Plasmapheresis
C) Interferon beta
D) Mitoxantrone
C) Interferon beta
Feedback: Interferon beta helps modify the course of treatment of MS. It may also reduce exacerbations in persons with relapsing–remitting MS. It is a cytokine that acts as an immune enhancer. It is administered by injection. The other medications are prescribed for MS but not given by injection.

After being thrown off the back of a bull, the bull rider can move his arms but has loss of motor function in the lumbar and sacral segments of the spinal cord. This is usually referred to as
A) tetraplegia.
B) quadriplegia.
C) paraplegia.
D) anterior cord
syndrome.
C) paraplegia.
Feedback: Tetraplegia and quadriplegia are loss of motor or sensory function after damage to neural structures in the cervical segments of the spinal cord. Paraplegia refers to loss of motor or sensory function in thoracic, lumbar, or sacral segments. The arms function as normal. Anterior cord syndrome includes loss of motor function provided by the corticospinal tracts and loss of pain and temperature sensation from damage to the lateral spinothalamic tracts.

Several months ago, a 20-year-old male suffered a spinal cord injury brought about by a snowboard trick gone wrong. The lasting effects of his injury include a flaccid bowel and bladder and the inability to obtain an erection. While sensation has been completely preserved in his legs and feet, his motor function is significantly impaired. What type of incomplete spinal cord injury has the man most likely experienced?
A) Anterior cord syndrome
B) Brown-Séquard syndrome
C) Central cord syndrome
D) Conus medullaris syndrome
D) Conus medullaris syndrome
Feedback: Functional deficits resulting from conus medullaris syndrome usually result in flaccid bowel and bladder and altered sexual function. Sacral segments occasionally show preserved reflexes if only the conus is affected. Motor function in the legs and feet may be impaired without significant sensory impairment. Anterior cord syndrome and Brown-Séquard syndrome include a loss of pain and temperature sensation, while central cord syndrome manifests in spastic paralysis and is more common among older adults.
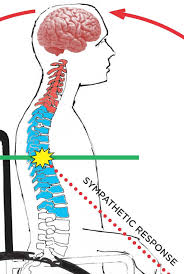
If the nurse suspects a spinal cord injury, the patient has developed autonomic dysreflexia. Which of the following assessments would confirm this complication? Select all that apply.
A) BP 180/98
B) Skin covered with macular rash
C) Pulse rate 49
D) Complains of a pounding headache
E) Cold, cyanotic lower legs
A) BP 180/98
C) Pulse rate 49
D) Complains of a pounding headache
Feedback: Autonomic dysreflexia represents an acute episode of exaggerated sympathetic reflex responses that occur in people with injuries at T6 and above, in which CNS control of spinal reflexes is lost. It is characterized by hypertension (BP 180/98), skin pallor, vagal slowing of the heart rate (pulse 49), and headache ranging from dull to severe and pounding.