Respiratory
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
49 Terms
Respiration
exchange of O2 and CO2 between atmosphere, blood, and cells
Pulmonary ventilation
gas exchange between atmosphere and lungs
External respiration
gas exchange between lungs and blood
Internal respiration
gas exchange between blood and cells
components of respiratory system
Structurally:
upper respiratory
nasal cavity
pharynx
vocal cords
larynx
lower respiratory
lungs
bronchi
trachea
Functionally:
conducting zone
allows air to enter/exit to alveoli
respiratory zone
gas exchange
bronchioles to alveolar sacs
nose
Function
primary entrance/exit for respiration
moistens and warms air
resonating chamber for speech
olfactory receptors
External nose
bony framework: ethmoid and vomer make septum; nasal bone, maxilla, lacrimal, palatine
cartilage: septal, alar, lateral
nares (naris - sing) = nostrils
internal nose
nasal cavity - superior and middle nasal conchae (ethmoid), inferior nasal conchae
nasal vestibule - can close w closing cartilage
internal naris opens to pharynx
olfactory mucosa - olfactory epithelium
respiratory mucosa
pseudostratified ciliated columnar epithelium
lysozyme and defensins in mucous and serous secretion
inspired air is warmed by plexuses of capillaries and veins
sensory nerve ending - sneezing
patentcy
open; clear of obstruction
change in pressure allows breathing to take place
pharynx
Functions
muscular tube from internal nares to C6
connects nasal cavity to larynx and esophagus
composed of smooth muscle
passageway for air and and food
resonating chamber for speech
houses tonsils
nasopharynx
internal naris to oral cavity
oropharynx
behind oral cavity
fauces: posterior opening between tongue and uvula
laryngopharynx
behind epiglottis
larynx
connects pharynx and trachea
cartilage: thyroid, arytenoid (vocal cords attached), cricoid
epiglottis: root attaches to inside cricoid cartilage; when swallow, will cover opening to trachea
trachea
extends larynx to primary bronchi
tracheal cartilage - C shaped
carina - trachea divides into R and L main bronchi
branching of bronchial tree
conduction zone —>
trachea
main bronchi
lobar bronchi
segmental bronchi
bronchioles
terminal bronchioles
respiration zone —>
respiratory bronchioles
alveolar ducts
alveolar sac
alveoli
23 generations of divisions
main bronchi
R is wider and shorter, more vertical
more likely to have food stuck
L bends more due to cardiac notch
lungs
apex at point superiorly, base flatter at inferior
L lung has 2 lobes - superior and inferior sep by oblique fissure
R has 3 lobes - superior lobe, inferior lobe, oblique fissure and middle lobe w horizontal fissure
pleura - each lung in own
parietal pleura lines thoracic cavity
visceral pleura lines lungs directly
between is pleural cavity w fluid
surface tension for lungs to stick to rib cage
reduces friction
medial view
hilum: where blood vessels enter and exit, bronchus, nerves
pulmonary ventilation
atmosphere to lungs
alternating pressure differences created by contraction and relaxation of respiratory muscles cause air to flow in and out of lungs
boyle’s law
volume of a gas varies inversely with its pressure
the pump in respiration
chest wall
respiratory muscles that increase or decrease size of thoracic cage
nerves and control areas of the brain
normal inhalation/expiration
500 mL
250 oxygen entering and 250 CO2 exiting
6-8 Lpm
12-18 breaths per minute
anatomical dead spaces
air remains in spaces not designated for air exchange/conductive zone (nose, pharynx, larynx, trachea, bronchi)
~150 mL
alveolar dead space
when some alveoli cease to act in gas exchange (collapse, obstruction)
control of breathing
medulla oblongata establishes rhythmic pattern
cerebrum provides voluntary override
pons regulate inspiration and expiration
intrapulmonary (intralveolar pressure)
pressure within the alveoli
muscles cause pulmonary ventilation by alternatively compressing and distending the lungs, causing pressure in alveoli to rise and fall
needs to equal atmosphere pressure (will cause air to rush in or rush out)
inspiration = -1 mmHg
expiration = +1 mmHg
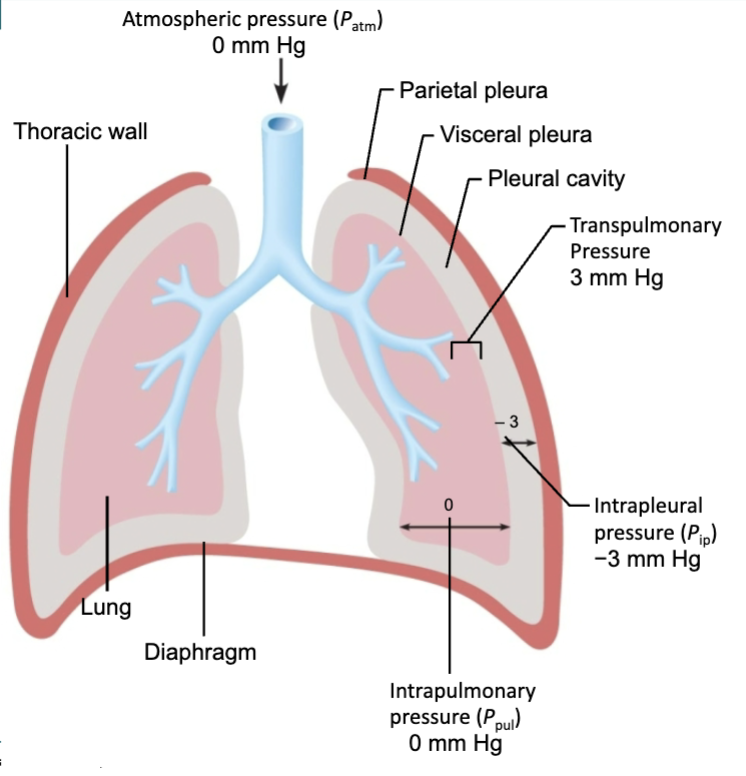
intrapleural pressure
pressure between lungs and thoracic wall
lungs have cont. capacity to collapse and recoil away from wall (caused by elastic fibers and surface tension)
intramolecular pressure between the alveoli will collapse the whole lung; recoil tendency of the lungs can be measured by negative pressure in intrapleural spaces
eupnea
normal quiet breathing
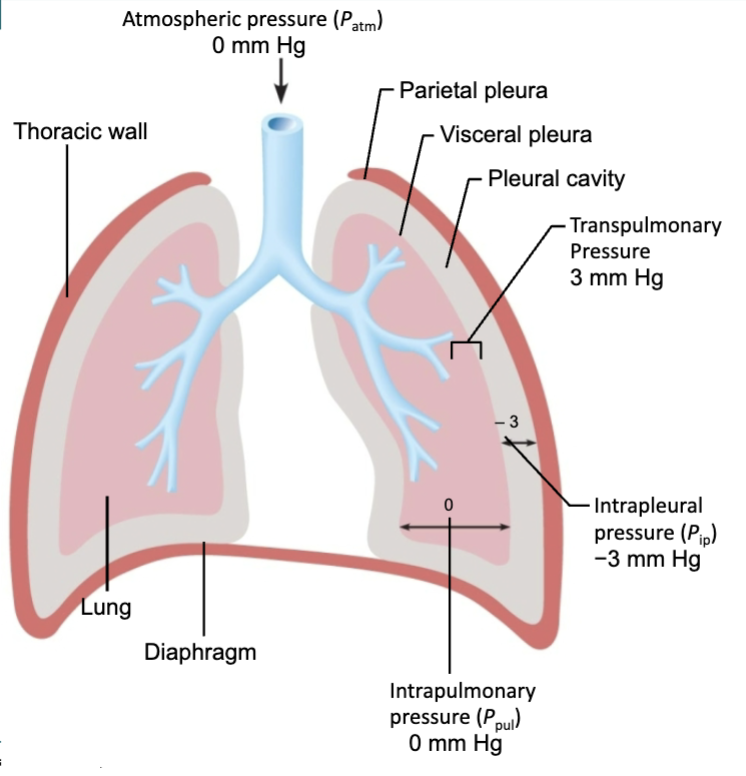
inspiration
enlargement of the thoracic cavity
contraction of diaphragm (down and flat)
contraction of external intercostals (rib cage up and outward)
decrease in alveolar pressure drives air inward
deep inspirations
neck and chest muscles also contract
sternocleidomastoid. pec minor, scalenes
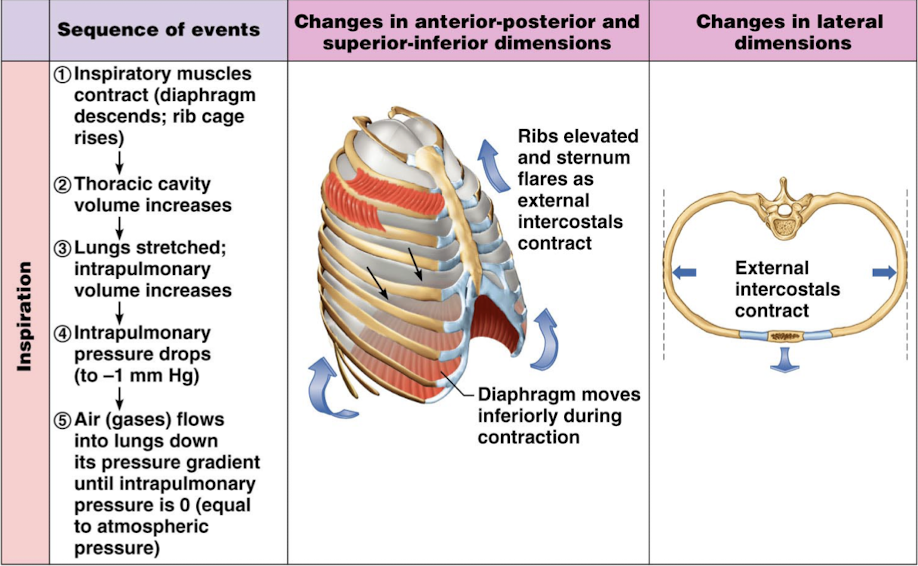
expiration
requires no actual contractions: passive
relaxation of muscles increases lung pressure, allowing air to move into atmosphere
forced expiration
internal intercostals contract, decreasing intrathoracic volume = forced
abdominal muscles can drive viscera into diaphragm
spirometry
lung volume changes that occur during respiration can be measured using spirogram
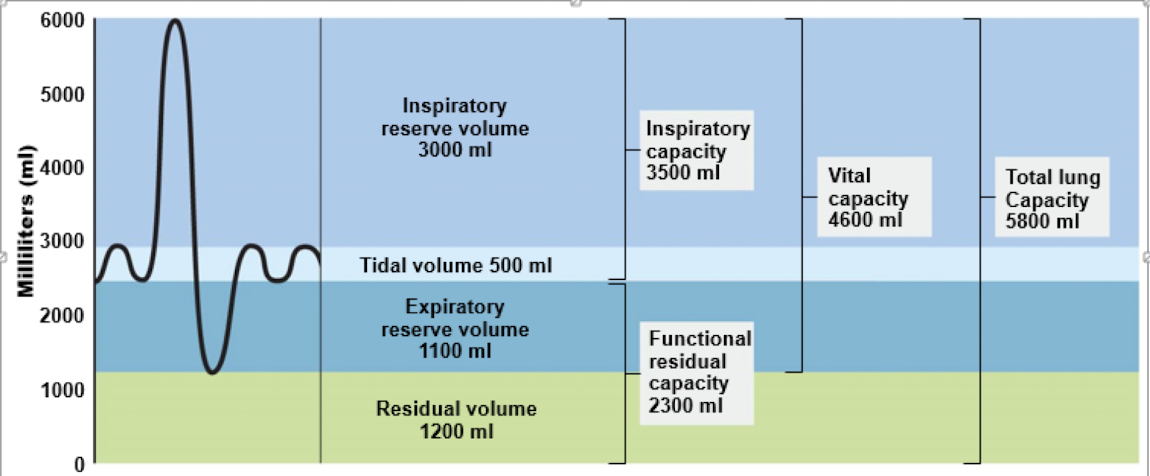
tidal volume (TV)
amount of air moved through the lungs during a normal respiratory cycle
500 mL
about 10-20% of vital capacity
inspiratory reserve volume (IRV)
amount of air that can be forcefully and maximally inspired into the lungs after a normal expiration
1900-3000 mL
60-70% VC
expiratory reserve volume (ERV)
air that can be maximally and forcefully exhaled after normal expiration
700-1200 mL
25% of VC
residual volume (RV)
air you cannot move out of the lung after forced expiration
1100-1200 mL
air is not stale; mixes w new air during each breath
maximum inspiratory flow rate or maximum expiratory flow rate
maximum rate of air movement during inhalation or exhalation
inspiratory capacity (IC)
maximum amount of air that can be inspired by an individual
IC = TV + IRV
2400-3500 mL
expiratory capacity (EC)
maximum amount of air that can be expired
EC = TV + ERV
1200-1700 mL
vital capacity (VC)
maximum volume of gas that can be inspired after maximum expiration
measured to determine strength of respiratory muscles and other aspects of pulmonary function
3-5 L (3100-4800 mL)
VC = TV + IRV + ERV
timed vital capacity (TVC)
fraction of vital capacity that is expired in one second
functional residual capacity (FRC)
amount of air that is remaining in lungs at the end of tidal expiration
FRC = ERV + RV
1800-2300 mL
total lung capacity (TLC)
total amount of air which occupies the lung after a maximum respiratory effect
TPC = TV + IRV + ERV + RV
4200-5800 mL
forced vital capacity (FVC)
amount of air that can be forcefully expelled from the lungs by expiring as forcibly as possible after a maximum inspiration
reduced in those with restrictive pulmonary disease
forced expiratory volume (FEV)
portion of VC that is expelled during specific intervals of time
in one sec = FEV1 (75-85% of VC)
in two sec = FEV2 (94%)
in three sec = FEV3 (97%)
obstructive disease will not have normal FEV values
minute resipiratory volume (MRV)
amount of new air moved into respiratory passages each minute
MRV = TV x RR
alveolar ventilation rate (AVR)
flow of gases into and out of alveoli during specific time (minute)
(TV - anatomical dead space)(ml/breath) x RR (breaths per min) = AVR (ml/min)
effect of exercise on lung volumes
TV and RR will increase bc more oxygen is required by skeletal muscles of body
hyperpnea
TV will erode the IRV but other volumes will remain consist including IC
breath period will decrease as RR increases
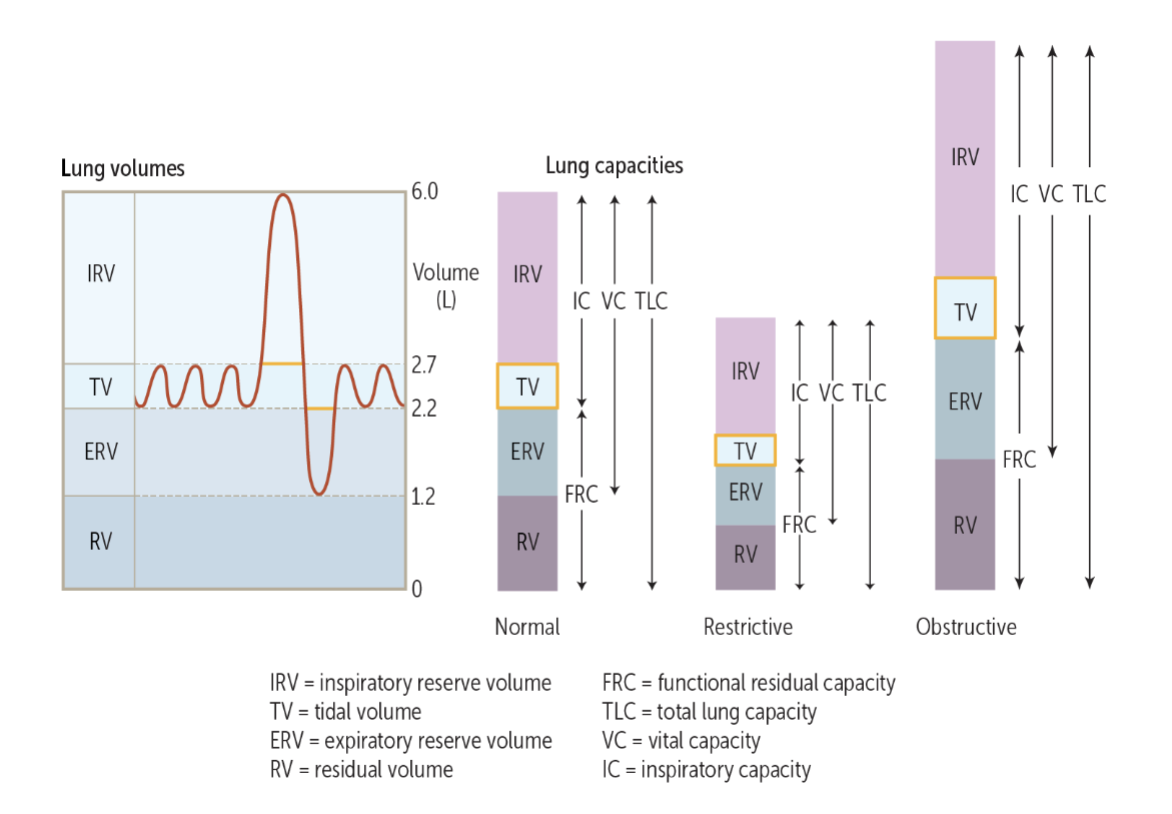
obstructive lung diseases
airflow in and out of the lungs is reduced bc expiration is more difficult due to the reduced size of the airways
asthma, chronic bronchitis, emphysema
difficulty exhaling all air in lungs
closing tendency of airways increased by positive pressure in chest during expiration
inhalation not as bad bc the negative pressure allows air to enter more freely
reductions in rate of forced expiration due to resistance to airflow and reduced airway diameter (all FEV values decrease)
VC not affected
Residual volumes may increase
dyspnea (difficult breathing) can occur
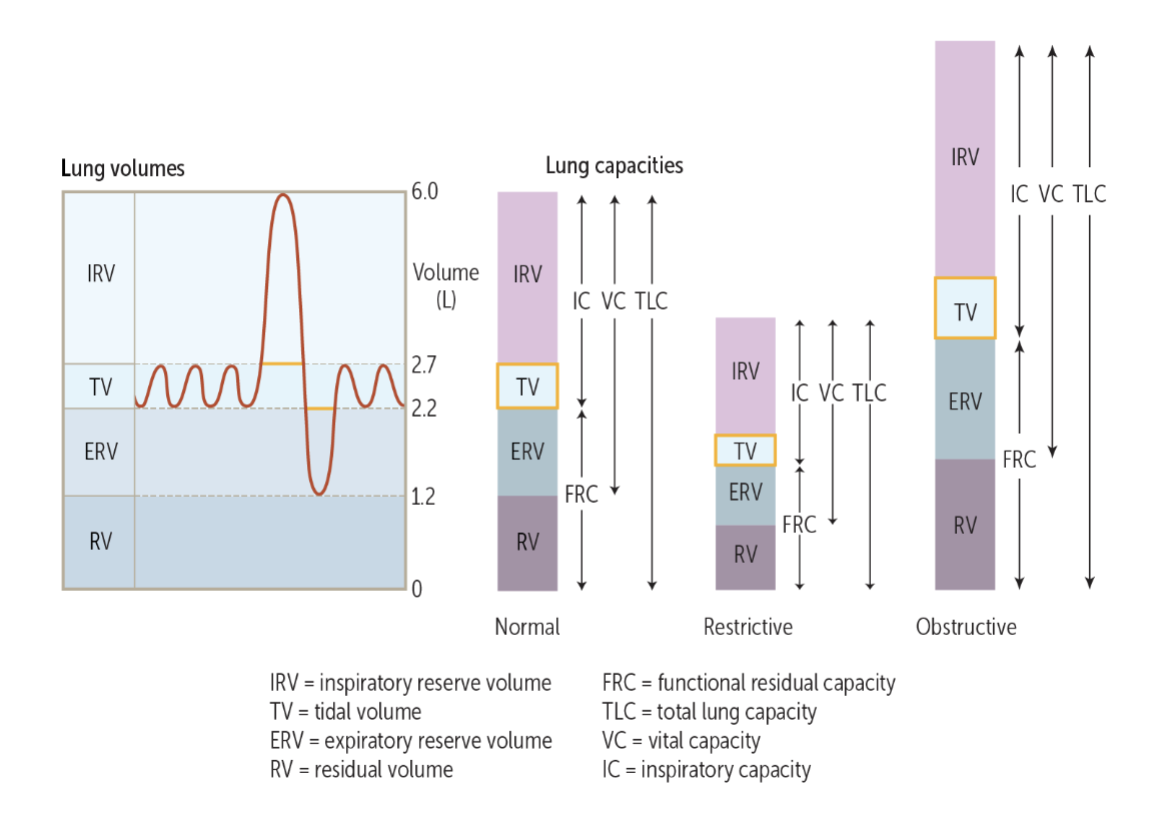
restrictive lung disease
ability to inflate and deflate the lungs is reduced bc of damage to the alveoli (or less surfactant or other things in the way like enlarged liver or spinal curvatures) which restricts a person’s ability to inhale
alveolar tissue may be damaged (tuberculosis, pneumonia, bronchiogenic carcinoma)
can also result from stiffness of chest wall, weak muscles, or damaged nerves inhibiting lung expansion
difficulty fully expanding lungs during inhalation
hypoventilation
some lung capacities and volumes will be decreased
VC reduced bc of reductions in inspiratory and expiratory reserve volumes
rate that VC can be expelled may remain normal
FVC would be reduced
surface tension
inwardly directed force in alveoli which must be overcome to expand lungs during each inspiration
water will cause alveoli to collapse
surfactants help break surface tension
elastic recoil
ability to return to resting volume when stretching force is released
compliance
ability to stretch
high compliance stretches easily
low compliance requires more force to stretch
restrictive lung disease
fibrotic lung diseases
inadequate surfactant production
breath period
duration of each breathing cycle recorded as breaths per second
FEV1/FVC
proportion of vital capacity that is expired in one second
