Pharmacologic Management of Gastric Acidity and Prokinetics
1/26
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
27 Terms
What are the Proton Pump Inhibitors?
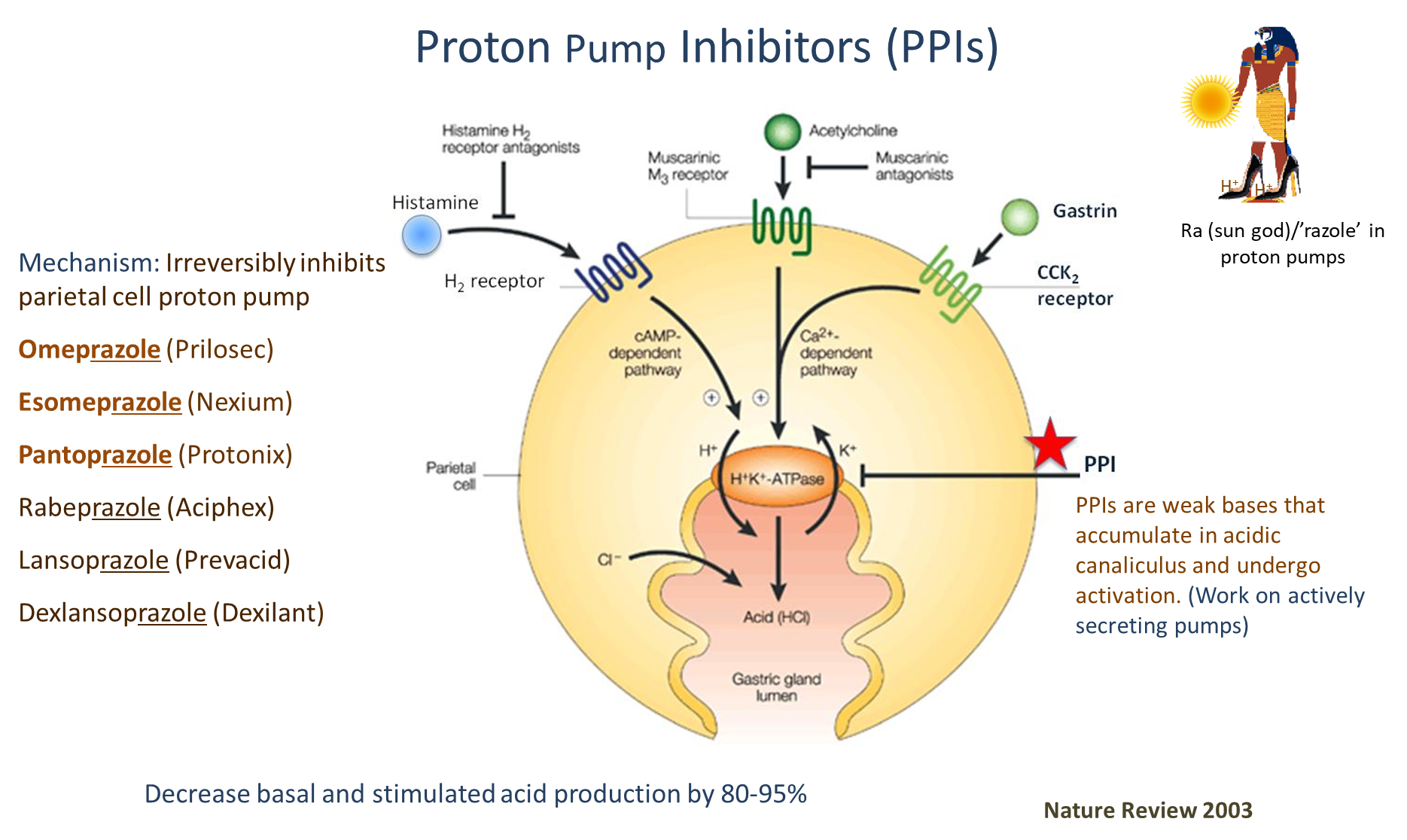
Proton Pump Inhibitors are drugs that irreversibly inhibit the parietal cell Hydrogen Potassium ATPase. The drugs in this category all end with the suffix -prazole
1) These drugs are weak bases and tend to accumulate in the acidic canaliculus of parietal cells. These drugs only work on actively secreting pumps
→ Omeprazole
→ Esomeprazole
→ Pantoprazole
How are Proton Pump Inhibitors activated?
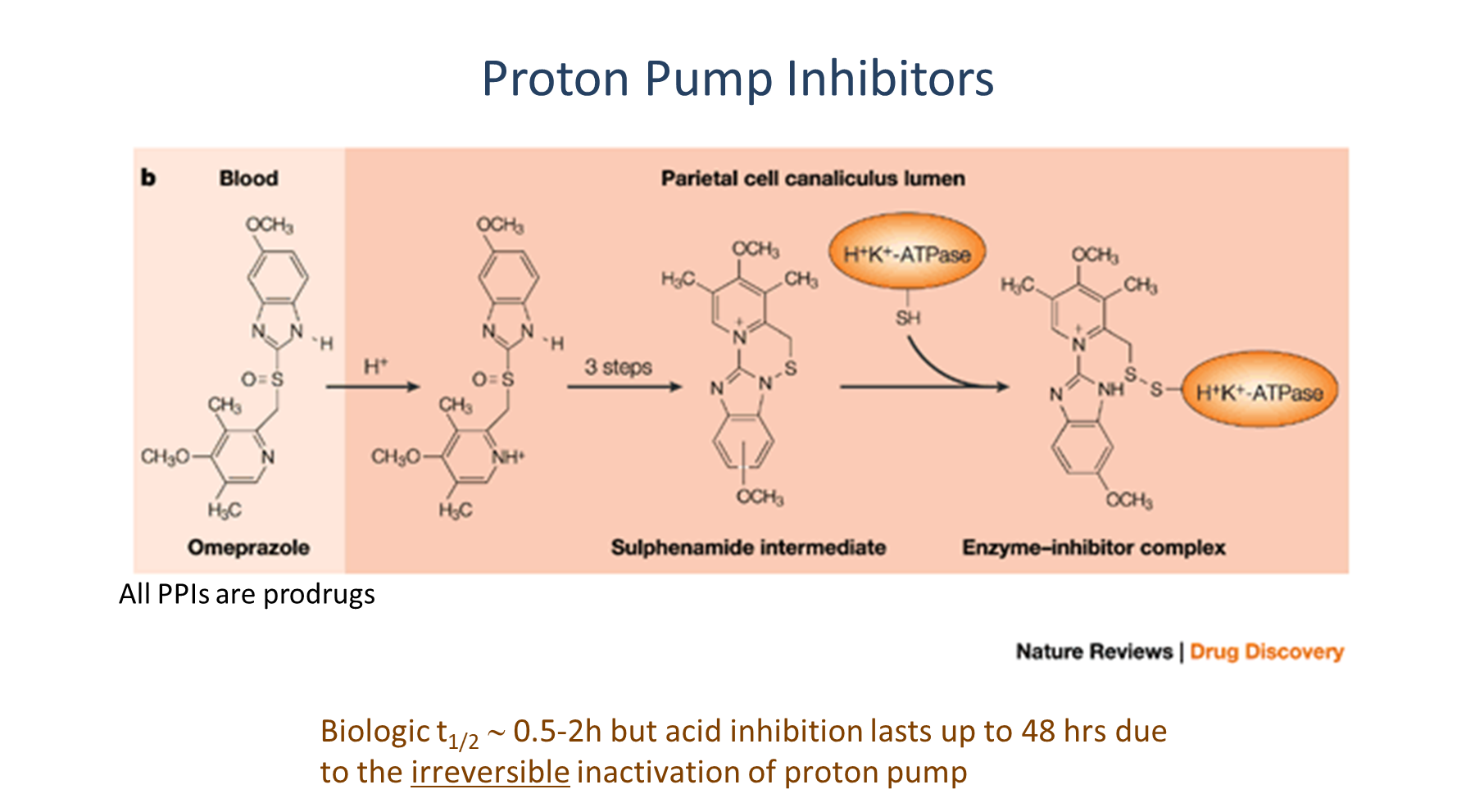
1) PPIs like Omeprazole are weak bases that can be taken up into the acidic parietal cell canaliculus
→ acid will convert the PPI to a sulphenamide intermediate which interacts with sulfhydryl groups located on the ATPase covalently
→ this causes irreversibly binding of the PPI
2) Because of its irreversibility, even if the half life of the drug is relatively short (0.5-2 hours) they can last for long periods of time
When are Proton Pump Inhibitors indicated? (6)
Peptic Ulcer Disease
GERD
Gastrinomas (Zollinger Ellison Syndrome)
Treatment of NSAID associated ulcers
Prevention of stress-related mucosal bleeding
Dyspepsia (discomfort in the upper abdomen after eating)
How are Proton Pump Inhibitors administered and why? How long does it take for the PPI to
PPIs are administered 30 minutes prior to a meal so that they can be used at max pump activity
→ its important to remember that these drugs can only bind to an actively secreting pump
→ these drugs take 3-4 days to reach maximum activity
What are the four common adverse effects associated with PPIs
1) B12 and magnesium deficiency
→ Magnesium requires a certain acidity level in order to be absorbed, and B12 needs acid in order to be freed from R-protein
→ B12 deficiency can present as anemia
→ Magnesium - cramps, spasms, fatigue
2) recurrent enteric infections, especially with C. diff
3) Patients may have gastric acid hypersecretion following cessation of the therapy
4) hypergastrinemia or elevated gastrin levels during usage
What are the major drug interactions associated with Proton Pump Inhibitors?
Proton Pump Inhibitors exhibit what is known as a Class Effect
→ because we decrease the amount of acid being produced, this will affect the absorption and bioavailability of drugs that require low pH in order to be activated such as antiviral proteases
Most PPIs will also inhibit CYP2C19 which is necessary for clopidogrel activation (antiplatelet drug)
What is the Potassium Competitive Acid Blockers?
Vonoprazan
→ drug that competes with potassium for binding to H+/K ATPase and reversibly inhibits activity
→ does not require activation like Proton Pump Inhibitors
What are the two histamine receptor 2 (H2 receptor) antagonists? (mechanism, benefits, and limitations)
Famotidine and Cimetidine
1) these drugs act at the H2 receptor on parietal cells, which couple to the cAMP pathway that activate the H+/K+ ATPase
→ administered at night as they are most effective at decreasing nocturnal acid secretion
2) less effective than PPIs but have extremely rapid onset
→ tolerance can develop after 2-6 weeks
When would you use the two H2 Antagonists?
Famotidine and Cimetidine
→ GERD
→ Uncomplicated Peptic Ulcers
→ Dyspepsia (upper abdominal discomfort after eating)
→ Prevention of Stress Related Gastritis
What are the adverse effects and drug interactions associated with H2 antagonists?
Famotidine and Cimetidine
→ while generally well tolerated, these drugs are known to worsen CNS symptoms in the cognitively impaired
→ Cimetidine can also cause endocrine adverse effects (interfering with androgen binding and decreases estrogen metabolism)
these drugs also have lots of drug interactions
1) Cimetidine inhibits multiple CYP enzymes
2) drugs can also inhibit the absorption of drugs that require low pH activation
What are the two Cytoprotective Agents?
Misoprostol and Bismuth subsalicylate
What is the function of Misoprostol? (use and mechanism)
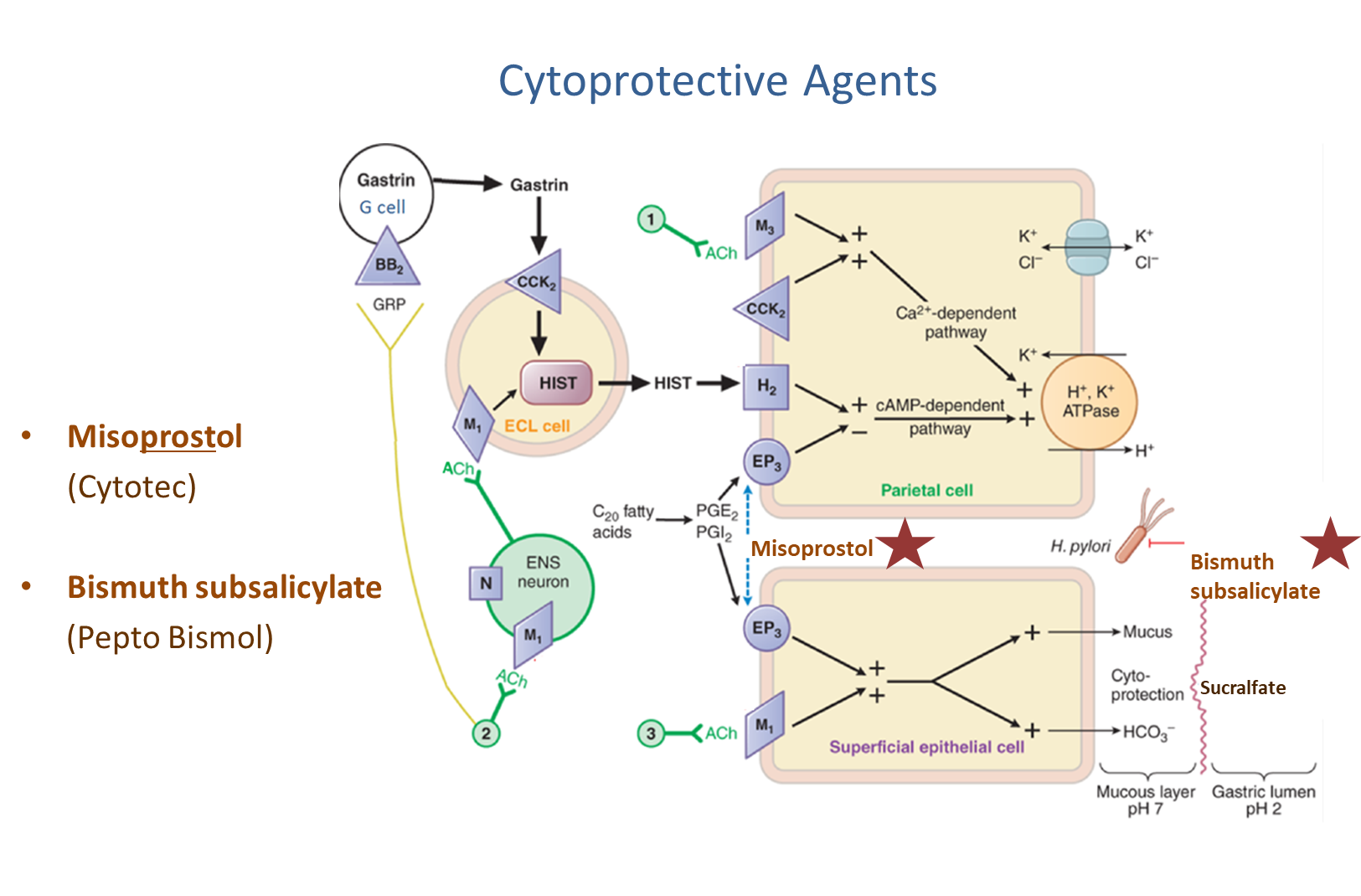
Misoprostol is a Prostaglandin PGE1 analog for the treatment of NSAID induced gastric ulcers and inducing labor contractions/cervical ripening
1) used in decreasing acid secretion at the parietal cell via the cAMP pathway, decreasing cAMP levels and inhibiting the H+/K+ ATPase
→ also stimulates mucus and bicarbonate secretion from superficial epithelial cells via the EP3 receptors
What are the adverse effects associated with Misoprostol?
Misoprostol, a PGE1 analog causes abdominal pain, cramping, and diarrhea
→ it is a uterine stimulating drug so it is a abortifacient
→ teratogenic and cause uterine rupture
What is Bismuth Salicylate (mechanism and 3 uses)
Bismuth Salicylate also known as Pepto Bismol
1) Bismuth has antimicrobial properties against both bacterial and viral GI pathogens, including helicobacter
→ bismuth will bind to the base of an ulcer and promote mucin and bicarbonate secretion
→ bismuth will also bind to enterotoxins
2) Bismuth is an antisecretory
→ increases both fluid and electrolyte absorption, and the salicylate metabolite will decrease formation of motility stimulating prostaglandins
3) used in diarrhea, dyspepsia, and treatment of H. pylori
What are the adverse effects of Bismuth Subsalicylate?
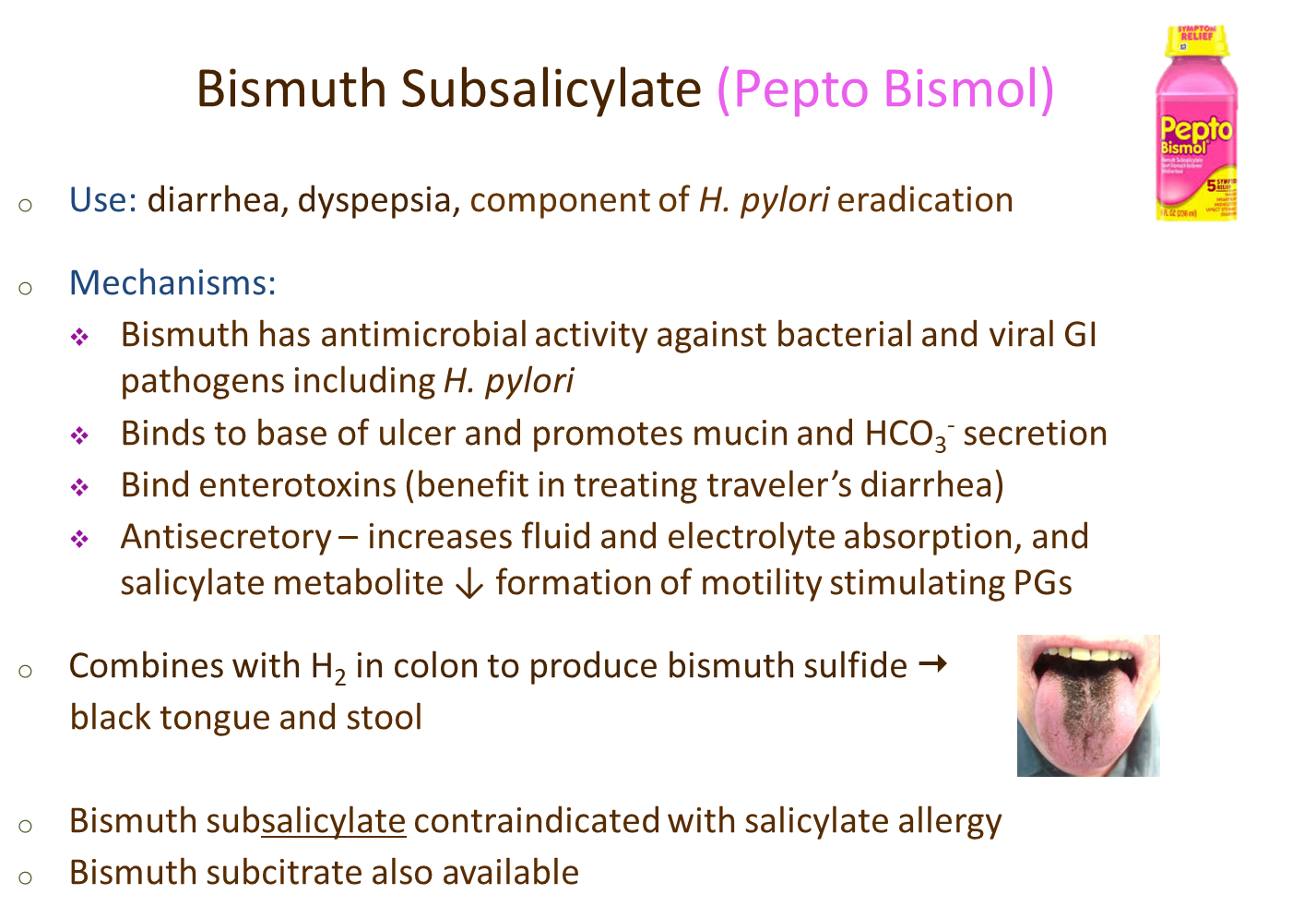
Pepto Bismol will combine with H2S (hydrogen sulfide) in the colon in order to produce bismuth sulfide causing black tongue and stool
→ bismuth subsalicylate is contraindicated in patients with a salicylate allergy, so bismuth subcitrate can be used
What is the first line therapy for helicobacter pylori eradication?
Quadruple Therapy
→ PPI, metronidazole, bismuth, and tetracycline
What are the four antacids and how do they function?
Sodium Bicarbonate, Calcium Carbonate, Magnesium Hydroxide, and Aluminum Hydroxide
→ works by neutralizing gastric acid
What are the adverse effects of sodium bicarbonate and calcium carbonate
The two drugs below are antacids
1) Sodium Bicarbonate
→ risks of metabolic alkalosis and hypernatremia
→ there is a small increased risk of cardiac or renal failure
2) Calcium Carbonate - reacts slower than sodium bicarbonate
→ hypercalcemia in patients with chronic kidney disease or milk alkali syndrome
→ Milk Alkali Syndrome is where excessive doses of calcium in milk along with alkali can cause hypercalcemia
What are Magnesium and Aluminum Hydroxide? What are their adverse effects
These two drugs are antacids - can be used in combination or alone
→ combining the two (magnesium is rapid and aluminum is slow) allows for sustained neutralizing capacity.
1) Adverse Effects - both cause renal impairment
→ magnesium causes diarrhea
→ aluminum causes constipation
Because of this, the two are often administered together in order to prevent adverse effects
What are the major drug interactions associated with antacids?
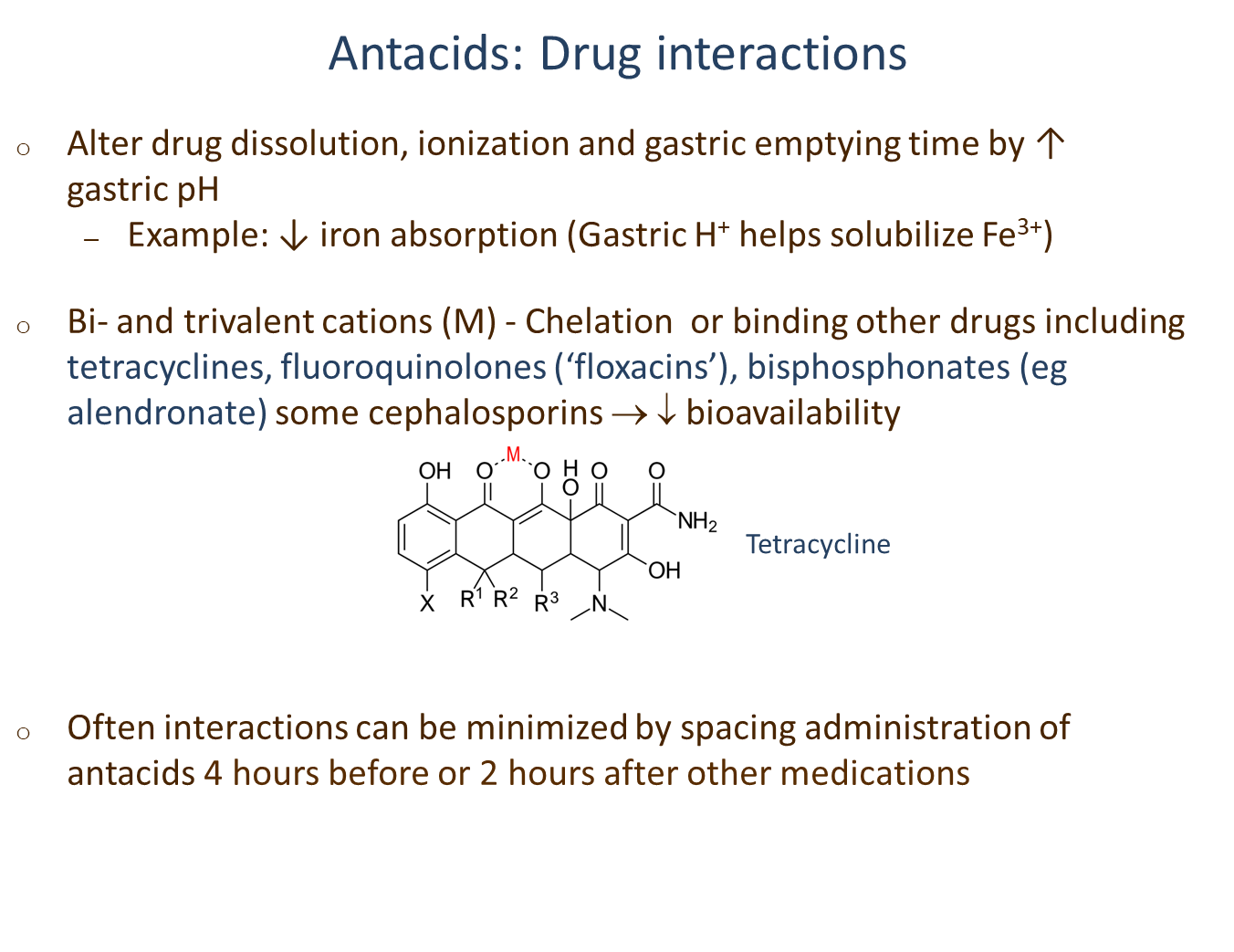
Antacids will alter drug dissolution, ionization, and gastric emptying time by increasing gastric pH
1) because these drugs are bi and trivalent cations - can chelate or bind other drugs decreasing their absorption by forming insoluble complexes
What are the four classes of Prokinetics? Which of these causes a prolonged QT interval?
Drugs that allow for improved gastric motility
Dopamine Receptor Antagonists
→ Metoclopramide
→ Domperidone - causes a prolonged QT interval
Serotonin Type 4 Receptor Agonists
→ Cisapride - causes a prolonged QT interval
Macrolide Antibiotic
→ Erythromycin and Azithromycin
Muscarinic Agonist
→ Bethanechol
What is Metoclopramide mechanism of action and uses
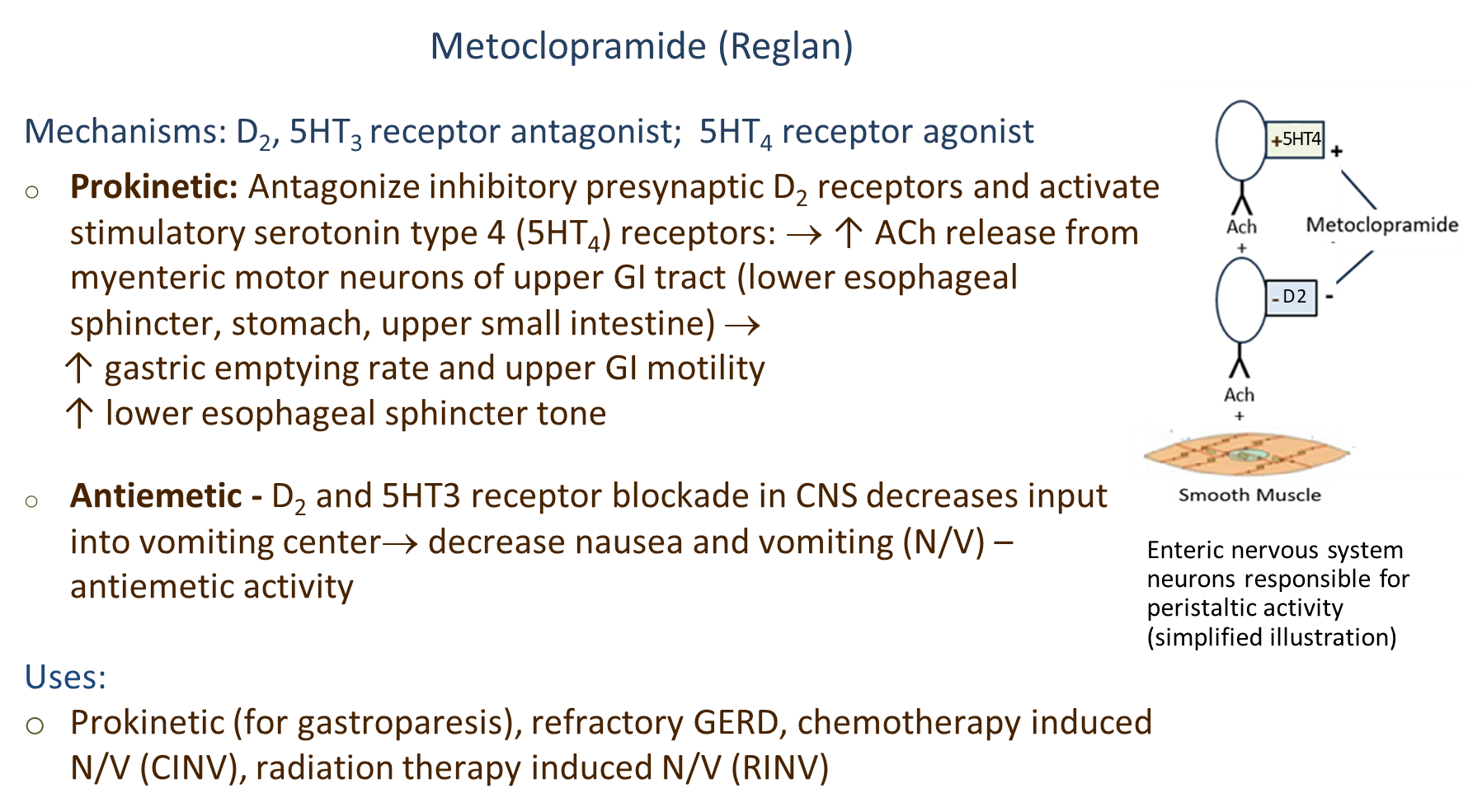
Metoclopramide is a D2 Antagonist, Serotonin Three Antagonist, and Serotonin Four Agonist
1) Functions as a Prokinetic
→ blocks D2 receptors and binds to Serotonin Four Receptors (5HT4), increasing acetylcholine release
→ this increase in acetylcholine will bind to smooth muscle cells of the upper GI tract increasing gastric emptying and upper GI motility
→ this also increases lower esophageal sphincter tone preventing reflux
2) Functions as an Antiemetic
→ blocking the D2 and Serotonin 3 Receptors (5HT3) will decrease input to the vomiting center
→ decreases nausea and vomiting
What are the effects of D2 antagonism in the CNS?
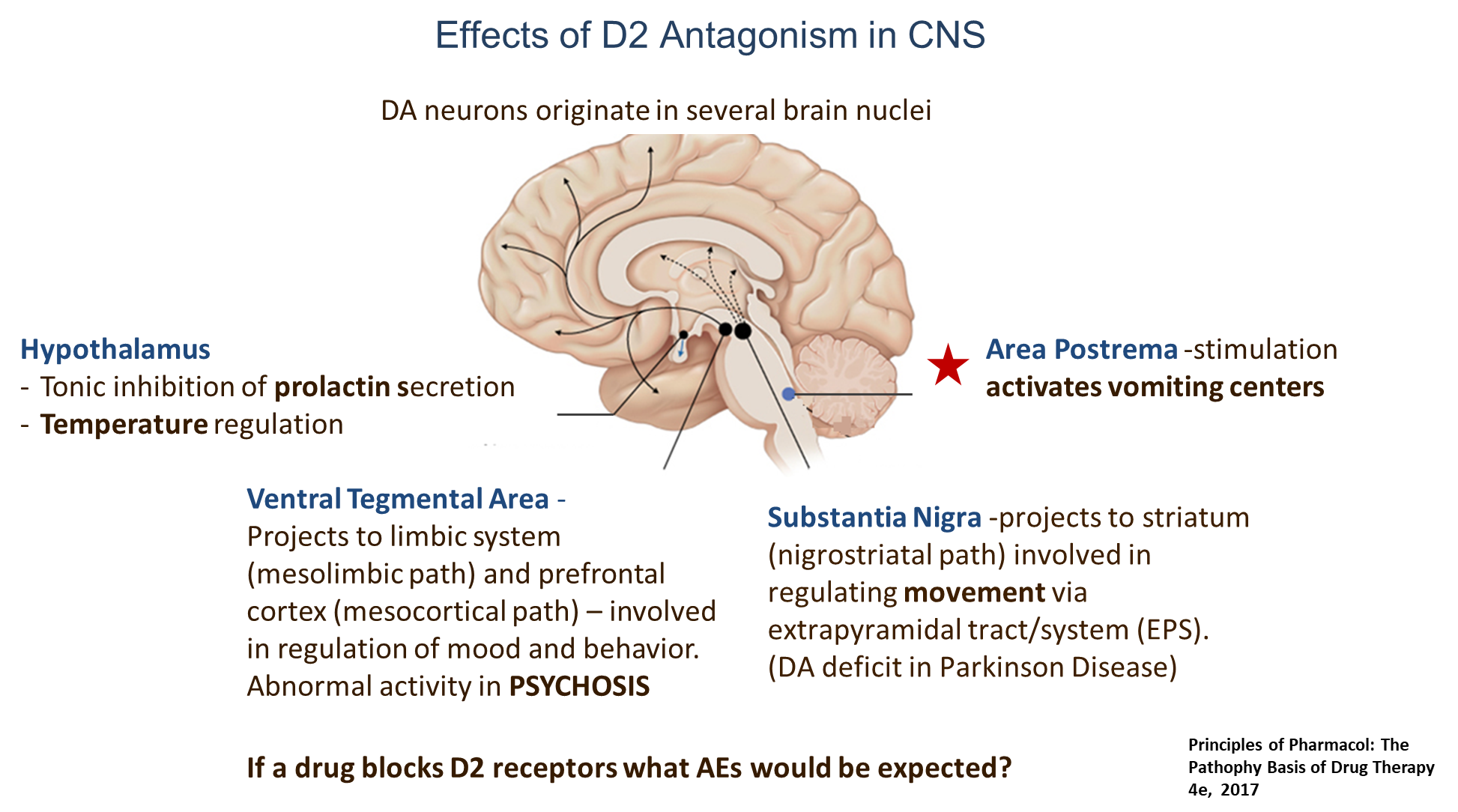
Drugs like Domperidone and Metoclopramide
1) Area Postrema/Chemoreceptor Trigger Zone
→ D2 receptors will activate the vomiting centers
2) Substantia Nigra
→ projects into the striatum and is involved in regulating movement by the extrapyramidal system
→ blockage of dopamine receptors can also cause movement disorders such as in Parkinsons
3) Ventral Tegmental Areas
→ involved in regulation in mood and behavior
→ D2 antagonism can be used to treat psychosis
4) Hypothalamus
→ D2 inhibition here can cause increase prolactin secretion
→ also involved in temperature regulation
What are the extrapyramidal side effects of metoclopramide
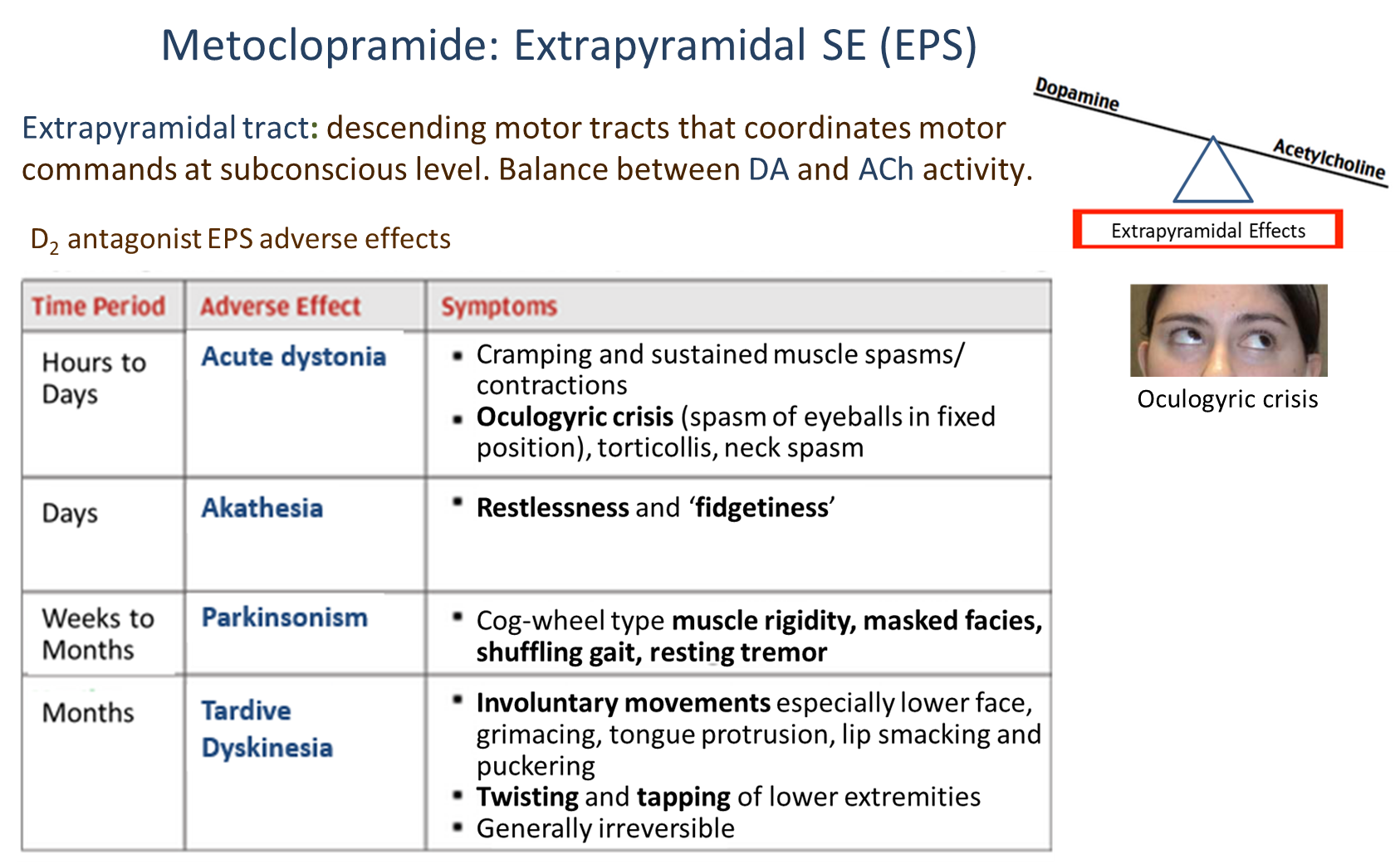
Metoclopramide blocks D2 receptors at the substantia nigra, impairing motor coordination by creating an imbalance between dopamine and acetylcholine
→ the adverse effects will progress over time and can be seen above
What are the two serotonin receptors found in the GI tract and what do they do?
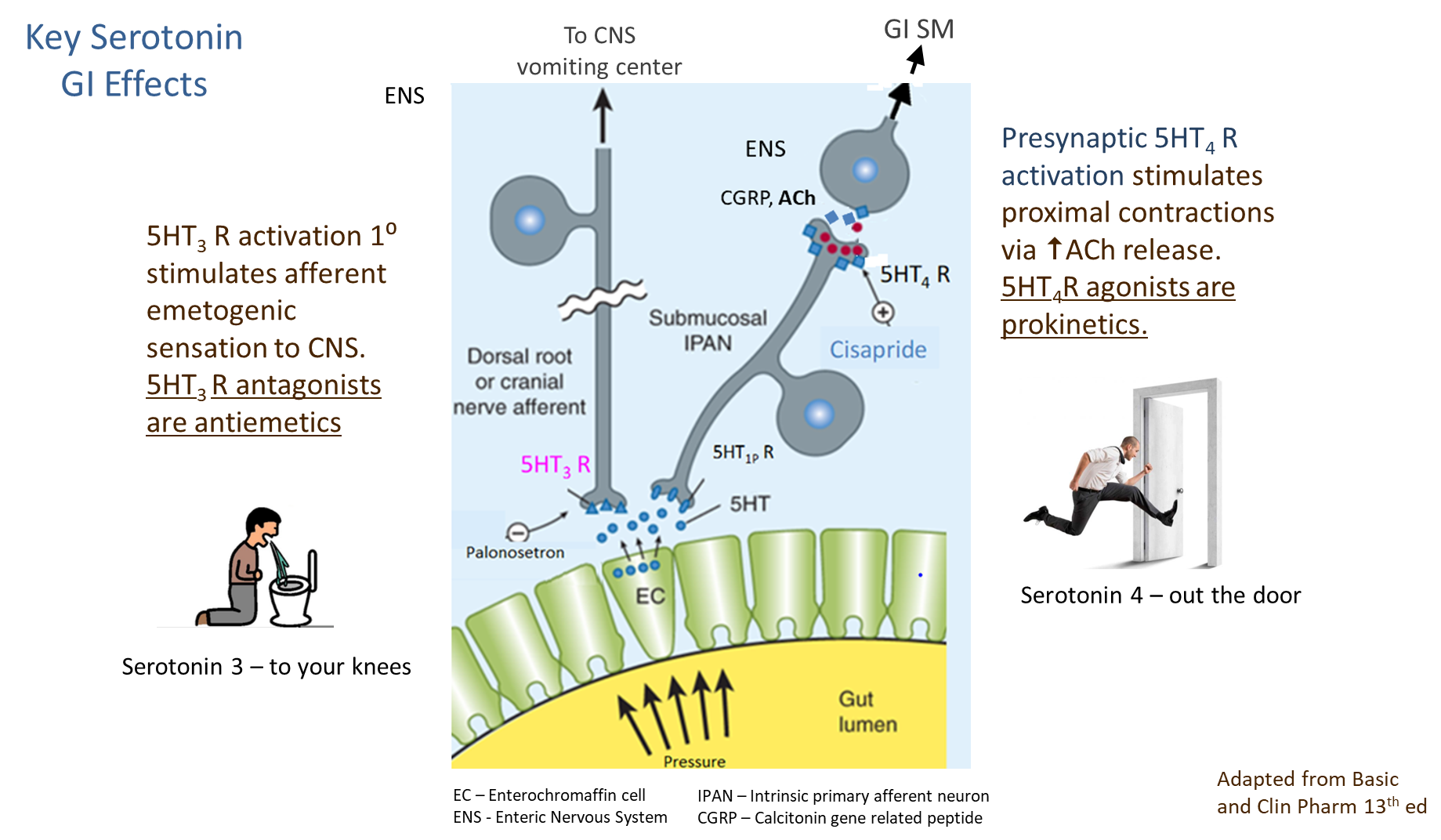
Serotonin receptors in the GI tract control various effects
1) Serotonin 3 Receptors (5HT3)
→ stimulation of these receptors send afferent emetogenic sensation to the CNS
→ antagonists to this receptor are antiemetics
2) Presynaptic Serotonin 4 Receptors (5HT4)
→ stimulates GI contractions as well as increasing acetylcholine
→ agonists of this receptor are prokinetics
What is Cisapride?
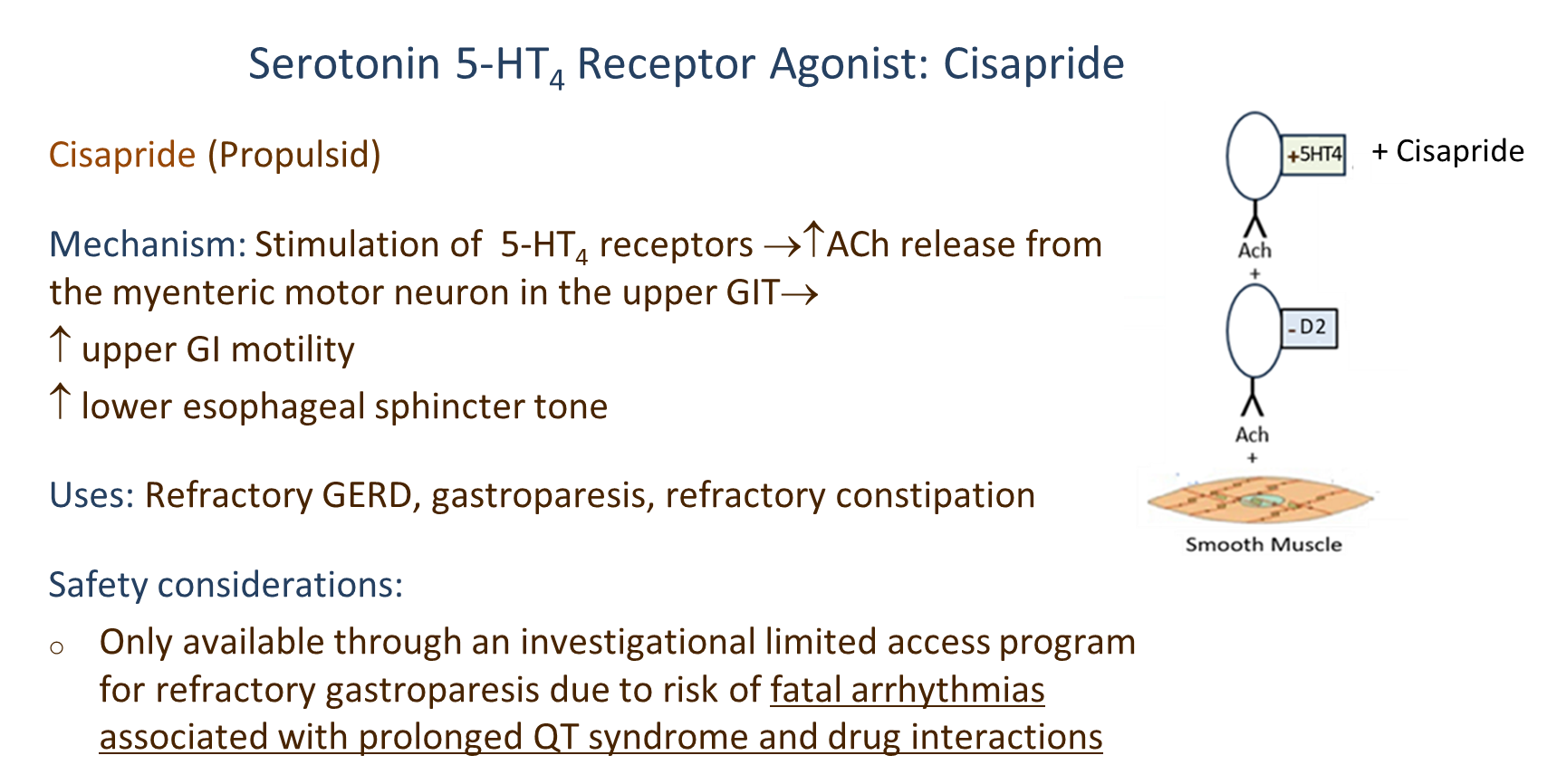
Cisapride is a Serotonin 4 Receptor Agonist (5HT4 Agonist)
→ stimulates the 5-HT4 receptors increasing acetylcholine release from myenteric motor neurons
→ increases upper GI motility and lowers esophageal sphincter tone
→ has a high risk of prolonged QT syndrome and arrhythmias
What are Motilides?
Erythromycin and Azithryomycin are Motilides - a form of prokinetic
1) mimic motilin, allowing for increased migrating motor complexes
→ allows for increased upper GI contractility and lower esophageal pressure